Abstract
Background:
Large lumbar or lumbosacral (LS) disc herniations usually expand from the paramedian space to the neuroforamen and compress both the transversing (lower) and the exiting (upper) nerve roots, thus leading to bi-radicular symptoms. Bi-radicular involvement is a statistically significant risk factor for poor outcome in patients presenting with far lateral or foraminal disc herniation after facet preserving microdecompression. There is evidence showing that patients suffering from large lumbar disc herniations treated with interbody fusion have significant superior results in comparison with those who received a simple discectomy. We report our experiences on managing large LS disc herniation with bi-radicular symptoms by transforaminal lumbar interbody fusion (TLIF) using one diagonal fusion cage with unilateral pedicle screw/rod fixation.
Materials and Methods:
Twenty-three patients who suffered from single level lumbar or LS disc herniation with bi-radicular symptoms treated with unilateral decompression and TLIF using one diagonal fusion cage with ipsilateral pedicle screw/rod fixation operated between January 2005 and December 2009, were included in this study. Operation time and blood loss were recorded. The pain and disability status were pre- and postoperatively evaluated by the visual analog score (VAS) and Oswestry Disability Index (ODI). Interbody bony fusion was detected by routine radiographs and computed tomography scan. Adjacent segment degeneration was detected by routine radiographs and magnetic resonance imaging examination. Overall outcomes were categorized according to modified Macnab classification.
Results:
The patients were followed up for an average of 44.7 months. Pain relief in the VAS and improvement of the ODI were significant after surgery and at final followup. No severe complications occurred during hospital stay. Interbody bony fusion was achieved in every case. No cage retropulsion was observed, while 3 cases experienced cage subsidence. Adjacent segment degeneration occurred at 3 discs cephalic to the fusion segment at followup. No patients underwent revised surgery. Overall outcome was excellent in 5 patients (21.7%), good in 13 (56.5%), fine in 4 (17.5%), and poor in 1 (4.3%).
Conclusions:
TLIF using one cage with ipsilateral pedicle screw/rod fixation is an effective treatment option for massive lumbar or LS disc herniation with bi-radicular involvement.
Keywords: Bi-radicular involvement, large disc herniation, unilateral pedicle screw fixation, lumbar disc, transforaminal interbody fusion
MeSh terms: Spinal column, bone screws, disc, herniation, arthrodesis, spine
INTRODUCTION
Large lumbar or lumbosacral (LS) disc herniations usually expand from the paramedian space to the neuroforamen and compress both the transversing (lower) and the exiting (upper) nerve roots, thus leading to bi-radicular symptoms. Therefore, some authors designated this relatively rare entity as double herniation, with an approximate incidence of 15–16.8% in all LS disc herniations.1,2
The herniated fragments within the paramedian space and neuroforamen must be totally removed to decompress the transversing and exiting nerve roots. Unfortunately, neither a single traditional interlaminar approach nor a single extraspinal intertransverse approach can achieve this goal because each approach exposes only the paramedian or foraminal portion of the intervertebral disc.3,4 Therefore, a few studies advocated a combined intra-extracanal approach for treatment of large LS disc herniation.5,6
The clinical results of large herniations operatively managed by simple discectomy through the combined approach seemed satisfactory,5,6 some argued that bi-radicular involvement is a statistically significant risk factor for poor outcome in patients presenting with far lateral or foraminal disc herniation after facet preserving microdecompression.2 In addition, there is evidence showing that patients suffering from large lumbar disc herniations treated with interbody fusion have significant superior results in comparison with those who received a simple discectomy.7
We report our experiences on managing large LS disc herniations with bi-radicular symptoms by transforaminal lumbar interbody fusion (TLIF) using one diagonal fusion cage with unilateral pedicle screw/rod fixation and suggest the procedure mentioned above as an alternative method for the treatment of this entity.
MATERIALS AND METHOD
Twenty-three consecutive patients who suffered from single-level lumbar or LS disc herniation with bi-radicular symptoms and had minimal followup of 2-year treated, by TLIF using one diagonal fusion cage with unilateral pedicle screw/rod fixation between January 2005 and December 2009, were included in this study. Patients with recurrent disc herniation, severe lumbar stenosis and spondylolisthesis were excluded. There were 14 males and 9 females in our series and they were 43–68 years old (mean, 56.8 years). All the herniated discs encroached into the paramedian area and neuroforamen, resulting in compression of the lower and upper nerve roots, respectively. The herniation was located at L3–L4 in 7 patients, L4–L5 in 10, and L5–S1 in 6 patients.
All patients had unremitting radicular pain projecting into 2 dermatomes, among them 10 had previously intermittent monoradiculopathy, while the other 13 had an onset of bi-radicular involvement. The radicular pain was graded 6 to 9 (7.30 ± 0.93) on a 0–10 visual analog scale (VAS). Nineteen patients had nonspecific low back pain graded 1–5 (2.43 ± 1.30) before the onset of radiculopathy. Clinical examination showed positive straight leg raising test in 6 patients, positive femoral stretch test in 7, and both positive signs in 10. Motor weakness was detectable in 16 patients and sensory deficits in 19. Ten patients had a weak knee-jerk, 8 had weak ankle reflex. In 16 patients, the duration of subclinical symptoms ranged from 5 months to 7 years and then they got worse for 3–7 months. The other 7 patients had an acute onset, and the symptoms lasted for 3–5 months. Bi-radiculopathy in each patient was confirmed by both elaborative physical examination and computed tomography (CT) and magnetic resonance imaging (MRI) scans. Six patients showed intervertebral instability at the segment of disc herniation on preoperative flexion extension radiography.
Surgery was carried out after failed conservative treatment, which included bed rest and oral nonsteroidal anti-inflammatory drugs.
Operative procedure
A posterior midline skin incision of length 5 cm was made. The paraspinal muscles on the affected side were dissected subperiosteally and retracted laterally until the two adjacent transverse processes were exposed, followed by intraoperative stiffness measurement of the affected segment via gently distracting the upper spinous process using a pair of Lane's towel forceps or manually pushing the very facet joint exposed by the senior surgeon's thumb. When the upper vertebra could be easily distracted dorsally, or looseness of the very facet joint could be felt, instability of the affected segment was considered. If segment instability was confirmed, 2 polyaxial, top-loading pedicle screws were inserted into the upper and lower pedicles. Then, the upper hemilamina, the lower facet joint of the upper vertebra, and partial upper facet joint of the lower vertebra, the ligamentum flavum, and the upper margin of the lower hemilamina were removed. The dura and the descending nerve root were retracted medially and, if necessary, the exiting nerve root was retracted gently cephalic wards. After initial resection of the herniated disc tissues, the endplates were fused without damaging their integrity by gradual distraction applied to the pedicle screws. Segment stability was again manually detected with the trial placed in the interbody space and a parallelogram-shaped cage of appropriate size, packed with cancellous bone previously harvested from lamina and facet joints, was implanted into the disc space. Finally, the intervertebral distraction was released, the 2 nuts were tightened, and the incision was closed.
Postoperative radiographs obtained immediately, at 6-month, 1-year and annual followups were reviewed to evaluate fusion status. X-ray films (anteroposterior and lateral flexion and extension) were used to evaluate fusion status. Bone bridging the disk space without lucency and <4° of angular motion on flexion extension views between the fused segments were considered as solid fusion. Three-dimensional CT scan radiographs were used to more accurately evaluate the fusion status every year postoperatively. Radiographical analysis was measured on a GE Centricity 3.0 (GE Healthcare) viewing station with calibrated linear and angular measurements. All images were independently measured by 2 experienced surgeons.
Radicular pain and low back pain measured using VAS, as well as Oswestry Disability Index (ODI), were assessed before surgery and at followup. The general outcomes were categorized into 4 groups according to modified Macnab classification, i.e., excellent, good, fair, and poor.8
RESULTS
The herniated discs including their migrated fragments were completely removed. The mean operative time was 143 min (range 127-160 min), the mean blood loss was 263 ml (range 190-370 ml). No patient received blood transfusion. No severe surgery related complications such as nerve root damage and spinal infection occurred.
The preoperative radicular pain measured by VAS was 7.30 ± 0.93, it decreased to 1.43 ± 0.84 at 3 months followup, while slightly increased to 1.83 ± 1.11 at 1 year after surgery and 2.39 ± 0.99 at final followup. The VAS value of preoperative low back pain was 2.43 ± 1.30, it decreased to 1.17 ± 0.72 at 3 months followup, while increased to 1.74 ± 0.75 at 1 year after surgery and 2.04 ± 1.19 at final followup. The preoperative ODI score was 68.74 ± 8.99, it declined to 22.35 ± 5.82 at 3 months followup, but rose to 24.17 ± 7.55 at 1 year surgery and 35.83 ± 9.13 at final followup.
All cases achieved solid bony interbody fusion as detected by X-ray and CT scan at 6 or 12 months followup [Figures 1–3]. No cage retropulsion was observed, while 3 cases experienced cage subsidence. X-ray and MRI examination demonstrated 3 out of 7 discs, which were cephalic to the herniated disc and scored preoperatively as grade 3 according to the classification system described by Pfirrmann et al., showing signs of degeneration such as decreased disc space height and/or hypermobility as well as decreased T2 signal intensity.9 Although 1 patient complained recurrent moderate low back pain in these 3 cases, no patients needed revised surgery at the end of this study.
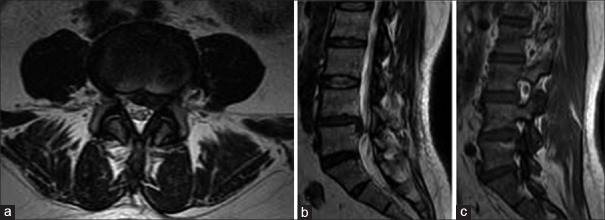
Figure 1.
(a-c) A 54-year old female suffered from left L4 and L5 radiculopathy as well as lower back pain caused by a large L4/L5 disc herniation. The preoperative T2W magnetic resonance imaging axial (a), mid sagittal (b) and parasagittal (c) scans showing large herniation of disc extending from the paramedian space to the left neuroforamen at L4/L5 level
Figure 3.
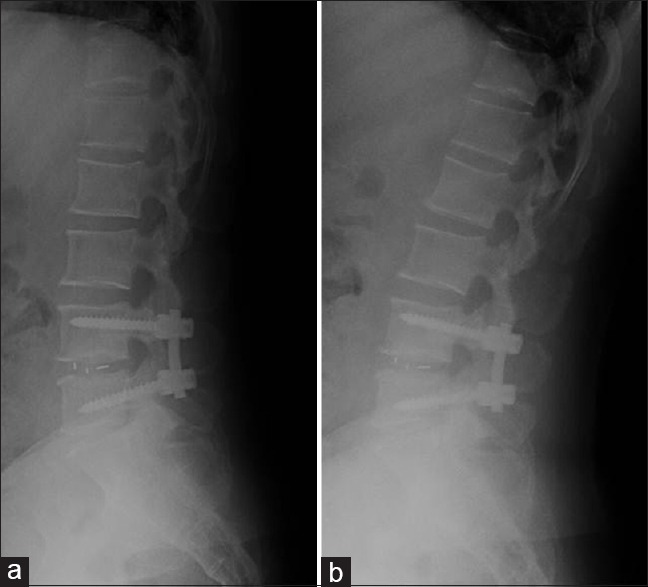
Flexion (a) extension (b) lateral radiographs obtained at 3 years followup showing no obvious instability at L3/L4 and L5/S1, indicating that transforaminal lumbar interbody fusion using one diagonal fusion cage with unilateral pedicle screw fixation does not accelerate adjacent segment degeneration
Figure 2.
Anteroposterior (a) and lateral (b) radiographs as well as sagittal computed tomography (c) reconstruction obtained at 6 months followup showing solid bony fusion of L4/L5 disc space
Overall outcome was excellent in 5 patients (21.7%), good in 13 (56.5%), fair in 4 (17.5%), and poor in 1 (4.3%).8
DISCUSSION
It has been well recognized that spinal fusion is not indicated after routine lumbar discectomy, but some authors maintained that fusion is recommended when conducting operative treatment of lumbar disc herniation as follows: (1) Some patients have long standing low back pain and new onset of radicular pain. (2) Some patients have precocious degenerative changes and preoperative segment instability radiographically. (3) Some patients suffer from recurrent disc herniation and those with large herniation.7,10,11
Some authors define large lumbar or LS disc herniation as a herniated disc with broad mediolateral extension compressing both the upper and lower nerve roots and recommend a combined intra-extracanal approach to simply remove the disc herniation without fusion.5,6 The midterm clinical results of these case series studies seemed satisfactory. Other authors, however, defined large herniation as a complete block on myelogram and observed a significantly superior results on low back pain as well as lower frequency of reoperation in patients who underwent resection of large herniation with fusion than in those without fusion.7 Theoretically, the larger the disc tissues protrude out from the disc space, the more lax the paravertebral ligaments would be, resulting in vertical instability.12 Vertical instability may in turn lead to translational and angular instability which is one of the main sources of low back pain, or foraminal stenosis which is one of the causes of radicular pain. In fact, segment hypermobility was intraoperatively confirmed in all of our patients by gently distracting the upper spinous process using a pair of Lane's towel forceps or manually pushing the very facet joint exposed by the senior surgeon's thumb before decompression of the neural elements, although lumbar instability was observed in only 6 patients on functional X-ray films preoperatively. The reasonable explanation is that pain and muscle spasm limits the flexion and extension of the lumbar spine. Moreover, thoroughly decompressing two nerve roots need facetectomy and, therefore, aggravate segment instability. Thus, we think it is suitable to perform an interbody fusion procedure after resection of a large disc herniation. Moreover, interbody fusion eliminates the possibility of recurrent disc herniation at the identical segment.7
The reasons for why unilateral total facetectomy was done are as follows. First, large herniation causing bi-radicular symptoms is the statistically significant risk factor for unfavorable outcomes in patients who underwent facet preserving microdecompression for far lateral disc herniation or foraminal stenosis, therefore total facetectomy is preferable.2 Second, as compared with posterior lumbar interbody fusion, TLIF is safer because of lower incidence of neural element injury, thus also needing to completely remove the unilateral facet joint.13
It is well known that application of the interbody fusion cage avoids complications related to the donor site. In addition, our previous studies demonstrated that a single diagonal cage enables sufficient anterior support and solid interbody arthrodesis to be achieved.14 Some authors suggested that pedicle screw/rod internal fixation is not required if facet joints can be preserved even in a procedure of repeated discectomy with interbody fusion.15 It is necessary to use instrumentation that complete decompression was performed by unilateral facetectomy, further compromising the segment stability. Since unilateral pedicle screw/rod fixation, as compared with bilateral fixation, provides similar augmentation on the operative segment, while decreasing the stress exerted on the adjacent segments,16 we employed this ipsilateral construct to ensure the immediate stability of the proposed fusion segment. Moreover, application of single fusion cage and unilateral pedicle screw/rod reduces operation time, blood loss, duration of hospitalization, implant costs, and potential complications. By doing these, solid interbody fusion was achieved in all patients, and no recurrent disc herniation or severe low back pain occurred until the end of this study.
The main concern following a lumbar fusion procedure is adjacent segment degeneration. This topic, however, remains controversial. Some authors maintain that there is a causal relationship between spinal fusion and adjacent segment disease, whereas others argue that degeneration at the segment adjacent to fusion is more likely a natural process.17,18,19,20 In our opinion, the relative importance of genetic factors, age, increased stress on the adjacent disc resulting from either fusion itself or injury of the posterior elements in the development of so-called “adjacent level disease” varies in individuals. Because genetic factors, patients’ age, and previous existed disc degeneration adjacent to the proposed fusion segment are out of surgeons’ control, careful manipulation to the spinal elements must be taken to reduce the occurrence of adjacent level disease, if it is really the truth. Some technical tips emphasized in our operations include: (a) Avoiding damage to the capsule of adjacent facet joints as well as supraspinous and interspinous ligaments when detaching the paraspinal muscles, and, if possible, preserving the cephalic margin of upper hemilamina to maintain the attachment of the ligament flava of the above segment;21,22 (b) inserting polyaxial, top-loading pedicle screws as long and thick as possible by Weinstein's method, and using a rod as short as possible to minimize violation of adjacent facet joint while ensure adequate fixation rigidity;23 (c) using a cage with suitable height and large cross-sectional area to provide sufficient anterior support and maintain lumbar lordosis, as well as promote interbody fusion by providing adequate contact surface;24,25 and (d) fixating the screws/rod at neutral position instead of compressed position. All these tips aim to decrease the stress concentration at the adjacent segment. We believe that our patients benefited from these techniques, as shown by our results that only 3 out of 7 adjacent discs with previous degeneration progressed from grade 3 to grade 4. Although no cage retropulsion occurred, we observed 3 cases of cage subsidence. The reason might be the stress concentration on the endplates resulted from the insufficient size of cages in our early cases.
There are 2 main limitations of the current study because of the rareness of this entity. One is that our study involved only a limited number of patients, therefore some factors such as patients’ occupations and compensation state that may affect clinical results might be neglected. The other is that this is a case series study, thus its evidence level is relatively low.
CONCLUSION
TLIF using one diagonal fusion cage with unilateral pedicle screw fixation is effective for treatment of large lumbar or LS disc herniation with bi-radicular involvement. Posterior spinal elements must be carefully protected and lumbar lordosis must be preserved to reduce the potential occurrence of adjacent segment disease in such cases.
Financial support and sponsorship
This study was supported by the National Natural Science Foundation of China (No. 81272038, 81572168), the Industry-Academy-Research cooperation project of Shanghai Science and Technology Committee (STCSM)(No.13DZ1940504,13DZ1940505).
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Abdullah AF, Wolber PG, Warfield JR, Gunadi IK. Surgical management of extreme lateral lumbar disc herniations: Review of 138 cases. Neurosurgery. 1988;22:648–53. doi: 10.1227/00006123-198804000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Chang SB, Lee SH, Ahn Y, Kim JM. Risk factor for unsatisfactory outcome after lumbar foraminal and far lateral microdecompression. Spine (Phila Pa 1976) 2006;31:1163–7. doi: 10.1097/01.brs.0000216431.69359.91. [DOI] [PubMed] [Google Scholar]
- 3.O’Hara LJ, Marshall RW. Far lateral lumbar disc herniation. The key to the intertransverse approach. J Bone Joint Surg Br. 1997;79:943–7. doi: 10.1302/0301-620x.79b6.7876. [DOI] [PubMed] [Google Scholar]
- 4.Wiltse LL, Spencer CW. New uses and refinements of the paraspinal approach to the lumbar spine. Spine (Phila Pa 1976) 1988;13:696–706. [PubMed] [Google Scholar]
- 5.Kutlay M, Topuz K, Colak A, Simsek H, Cetinkal A, Demircan MN. Management of disc herniations with bi-radicular symptoms via combined lateral and interlaminar approach. Neurosurg Rev. 2010;33:97–105. doi: 10.1007/s10143-009-0218-0. [DOI] [PubMed] [Google Scholar]
- 6.Paolini S, Ciappetta P, Raco A, Missori P, Delfini R. Combined intra-extracanal approach to lumbosacral disc herniations with bi-radicular involvement. Technical considerations from a surgical series of 15 cases. Eur Spine J. 2006;15:554–8. doi: 10.1007/s00586-004-0862-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Satoh I, Yonenobu K, Hosono N, Ohwada T, Fuji T, Yoshikawa H. Indication of posterior lumbar interbody fusion for lumbar disc herniation. J Spinal Disord Tech. 2006;19:104–8. doi: 10.1097/01.bsd.0000180991.98751.95. [DOI] [PubMed] [Google Scholar]
- 8.Turner JA, Ersek M, Herron L, Deyo R. Surgery for lumbar spinal stenosis. Attempted meta-analysis of the literature. Spine (Phila Pa 1976) 1992;17:1–8. doi: 10.1097/00007632-199201000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976) 2001;26:1873–8. doi: 10.1097/00007632-200109010-00011. [DOI] [PubMed] [Google Scholar]
- 10.Bambakidis NC, Feiz-Erfan I, Klopfenstein JD, Sonntag VK. Indications for surgical fusion of the cervical and lumbar motion segment. Spine (Phila Pa 1976) 2005;30(16 Supp):S2–6. doi: 10.1097/01.brs.0000174509.31291.26. [DOI] [PubMed] [Google Scholar]
- 11.Esses SI, Huler RJ. Indications for lumbar spine fusion in the adult. Clin Orthop Relat Res. 1992;279:87–100. [PubMed] [Google Scholar]
- 12.Luk KD, Chow DH, Holmes A. Vertical instability in spondylolisthesis: A traction radiographic assessment technique and the principle of management. Spine (Phila Pa 1976) 2003;28:819–27. doi: 10.1097/00007632-200304150-00016. [DOI] [PubMed] [Google Scholar]
- 13.Humphreys SC, Hodges SD, Patwardhan AG, Eck JC, Murphy RB, Covington LA. Comparison of posterior and transforaminal approaches to lumbar interbody fusion. Spine (Phila Pa 1976) 2001;26:567–71. doi: 10.1097/00007632-200103010-00023. [DOI] [PubMed] [Google Scholar]
- 14.Zhao J, Hou T, Wang X, Ma S. Posterior lumbar interbody fusion using one diagonal fusion cage with transpedicular screw/rod fixation. Eur Spine J. 2003;12:173–7. doi: 10.1007/s00586-001-0376-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chitnavis B, Barbagallo G, Selway R, Dardis R, Hussain A, Gullan R. Posterior lumbar interbody fusion for revision disc surgery: Review of 50 cases in which carbon fiber cages were implanted. J Neurosurg. 2001;95(2 Suppl):190–5. doi: 10.3171/spi.2001.95.2.0190. [DOI] [PubMed] [Google Scholar]
- 16.Kabins MB, Weinstein JN, Spratt KF, Found EM, Goel VK, Woody J, et al. Isolated L4-L5 fusions using the variable screw placement system: Unilateral versus bilateral. J Spinal Disord. 1992;5:39–49. doi: 10.1097/00002517-199203000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Anandjiwala J, Seo JY, Ha KY, Oh IS, Shin DC. Adjacent segment degeneration after instrumented posterolateral lumbar fusion: A prospective cohort study with a minimum five-year followup. Eur Spine J. 2011;20:1951–60. doi: 10.1007/s00586-011-1917-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cheh G, Bridwell KH, Lenke LG, Buchowski JM, Daubs MD, Kim Y, et al. Adjacent segment disease followinglumbar/thoracolumbar fusion with pedicle screw instrumentation: A minimum 5-year followup. Spine (Phila Pa 1976) 2007;32:2253–7. doi: 10.1097/BRS.0b013e31814b2d8e. [DOI] [PubMed] [Google Scholar]
- 19.Okuda S, Iwasaki M, Miyauchi A, Aono H, Morita M, Yamamoto T. Risk factors for adjacent segment degeneration after PLIF. Spine (Phila Pa 1976) 2004;29:1535–40. doi: 10.1097/01.brs.0000131417.93637.9d. [DOI] [PubMed] [Google Scholar]
- 20.Wai EK, Santos ER, Morcom RA, Fraser RD. Magnetic resonance imaging 20 years after anterior lumbar interbody fusion. Spine (Phila Pa 1976) 2006;31:1952–6. doi: 10.1097/01.brs.0000228849.37321.a8. [DOI] [PubMed] [Google Scholar]
- 21.Lai PL, Chen LH, Niu CC, Fu TS, Chen WJ. Relation between laminectomy and development of adjacent segment instability after lumbar fusion with pedicle fixation. Spine (Phila Pa 1976) 2004;29:2527–32. doi: 10.1097/01.brs.0000144408.02918.20. [DOI] [PubMed] [Google Scholar]
- 22.Najarian S, Dargahi J, Heidari B. Biomechanical effect of posterior elements and ligamentous tissues of lumbar spine on load sharing. Biomed Mater Eng. 2005;15:145–58. [PubMed] [Google Scholar]
- 23.Chen Z, Zhao J, Xu H, Liu A, Yuan J, Wang C. Technical factors related to the incidence of adjacent superior segment facet joint violation after transpedicular instrumentation in the lumbar spine. Eur Spine J. 2008;17:1476–80. doi: 10.1007/s00586-008-0776-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kumar MN, Baklanov A, Chopin D. Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur Spine J. 2001;10:314–9. doi: 10.1007/s005860000239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lazennec JY, Ramaré S, Arafati N, Laudet CG, Gorin M, Roger B, et al. Sagittal alignment in lumbosacral fusion: Relations between radiological parameters and pain. Eur Spine J. 2000;9:47–55. doi: 10.1007/s005860050008. [DOI] [PMC free article] [PubMed] [Google Scholar]