Abstract
Introduction
Professionals working in intensive and palliative care units, hence caring for patients at the end-of-life, are at risk of developing burnout. Workplace conditions are determinant factors to develop this syndrome among professionals providing end-of-life care.
Objectives
To identify and compare burnout levels between professionals working in intensive and palliative care units; and to assess which workplace experiences are associated with burnout.
Methods
A nationwide, multicentre quantitative comparative survey study was conducted in Portugal using the following instruments: Maslach Burnout Inventory–Human Services Survey, Questionnaire of workplace experiences and ethical decisions, and Questionnaire of socio-demographic and professional characteristics. A total of 355 professionals from 10 intensive care and 9 palliative care units participated in the survey. A series of univariate and multivariate logistic regression analyses were performed; odds ratio sidelong with 95% confidence intervals were calculated.
Results
27% of the professionals exhibited burnout. This was more frequent in intensive care units (OR = 2.525, 95% CI: 1.025–6.221, p = .006). Univariate regression analyses showed that higher burnout levels were significantly associated with conflicts, decisions to withhold/withdraw treatment, and implementing palliative sedation. When controlling for socio-demographic and educational characteristics, and setting (intensive care units versus palliative care units), higher burnout levels were significantly and positively associated with experiencing conflicts in the workplace. Having post-graduate education in intensive/palliative care was significantly but inversely associated to higher burnout levels.
Conclusions
Compared to palliative care, working in intensive care units more than doubled the likelihood of exhibiting burnout. Experiencing conflicts (e.g., with patients and/or families, intra and/or inter-teams) was the most significant determinant of burnout and having post-graduate education in intensive/palliative care protected professionals from developing this syndrome. This highlights the need for promoting empowering workplace conditions, such as team empowerment and conflict management. Moreover, findings suggest the need for implementing quality improvement strategies and organizational redesign strategies aimed at integrating the philosophy, principles and practices of palliative care in intensive care units.
Introduction
Professionals working in intensive and palliative care units, hence caring for patients suffering from a life-threatening disease, sometimes at the end-of-life, are at risk of developing work-related problems, such as burnout. Burnout is a syndrome of exhaustion related to the job. It is characterized by physical and emotional fatigue, and is usually related to work stress and dedication to a cause, a way of life that does not match the person’s expectations [1]. Burnout syndrome is widely described in its tri-dimensionality: (i) Emotional exhaustion (EE); (ii) Depersonalization (DEP); and (iii) (reduced sense of) Personal and Professional Accomplishment (PPA) [2,3].
High incidences of burnout were described in helping professions due to the establishment of intense interpersonal relationships [4]. In the context of healthcare, particularly in intensive and palliative care settings, professionals are often confronted with very complex and highly demanding situations (e.g., end-of-life decisions, communication about difficult issues such as life-threatening diagnosis and limited prognosis, family conflicts, human suffering and vulnerability), which, together with disempowering conditions of the workplace (e.g., work overload, role ambiguity, conflicts), can be a source of considerable stress, emotional constraint, moral distress, disempowerment and burnout [1,4–7]. According to several authors [2,3,8,9], these risk factors can be organized into four main dimensions: personal characteristics, organizational factors, quality of working relationships and exposure to end-of-life issues. Organizational and services’ negative working culture, in which perceived burnout complaints among professionals are common, might create a “contagion effect” among professionals [10].
Evidence shows that working in intensive care units (ICUs) is associated to higher burnout levels and it may vary across countries [4,8–15]. In fact, a recent systematic review showed that the prevalence of burnout among healthcare professionals in ICUs varied from 0% to 70.1% with this syndrome being associated to a broad range of variables, such as the work environment, professional role and conflicts [16]. In the United States of America, a recent report issued by the Critical Care Societies Collaborative highlighted that up to 45% of the critical care physicians and nearly a third (25% to 33%) of critical care nurses in this country were experiencing severe burnout [9].
A Portuguese study conducted with nurses and physicians working in ICUs found that 31% out of 300 respondents exhibited burnout [4]. The authors concluded that higher burnout levels were associated to organizational factors, workload and workplace experiences, such as making ethical decisions [4,17]. Similar findings were reported elsewhere, indicating that organizational factors are indeed associated with higher burnout levels in ICUs [9,11,12,14,16]. Experiencing conflicts (e.g., with patients and/or families, intra and/or inter-teams) is also a determinant variable of burnout [8,14]. Furthermore, it seems that professional groups are affected in diverse manners: while nurses are more affected in their sense of exhaustion and accomplishment, physicians are affected mostly in terms of depersonalization [4].
Contrarily, working in palliative care units (PCUs) is not associated to higher burnout levels [1], especially when compared to other work contexts. A study conducted with nurses and physicians working in PCUs in Portugal indicated that only 3% of professionals exhibited this syndrome. The majority of the respondents were at low (55%) and medium risk (30%) of burnout [5,18]. Diverse findings, however, were reported in other countries. A significant prevalence of burnout was identified, for instance, among hospice and palliative care (PC) practitioners in Singapore, being associated with working more hours and in different work settings [19]. Effective coping mechanisms like physical well-being, setting boundaries, transcendental meditation and quiet reflection, passion for one’s work, realistic expectations, remembering patients, rituals after a patient’s death, inter-professional team-based communication and strategies, and organizational activities were associated with less burnout in palliative care [1,5,18,19]. The mediating role of coping styles in the development of burnout has been highlighted in other healthcare settings, suggesting the need to implement active strategies aiming at enhancing professional performance [20].
Several differences and similarities can be found in the workplace experiences faced by professionals working in ICUs and PCUs. On the one hand, while in intensive care (IC) the major goal is to save lives and professionals feel they have the patient’s life “in their hands”, in palliative care (PC) the major purpose is to promote the quality of life, minimize suffering and provide a peaceful death. This may have an effect in the way professionals cope with the demanding situations of their daily practice. On the other hand, professionals working in ICUs and in PCUs care for patients with life-threatening diseases or conditions, provide end-of-life care, make ethical decisions, and face human vulnerability, suffering, dying and death. Beyond these experiences, in both ICUs and PCUs as in many other healthcare settings, professionals face other common experiences, such as communication issues, different perspectives about the patients’ best interest and conflicts that may affect their emotional well-being and influence the quality of care. Furthermore, particularly nowadays, due to the economic crisis, financial constrains cause resource shortages and work overload in healthcare services, which can contribute to physical and emotional exhaustion [1,3,4,7–20].
Despite the broad spectrum of literature about burnout in healthcare professions, there is a lack of specific studies comparing burnout among professionals working in intensive and palliative care units. To our knowledge, this comparison has never been investigated thoroughly, even less in Portugal. Moreover, when looking at the existing evidence on burnout in intensive and palliative care, findings lack of consistency; therefore, justifying the need to study this phenomenon.
The objectives of our study are: (i) To identify and compare burnout levels between professionals working in ICUs and PCUs; and (ii) to assess which workplace experiences are significantly associated with burnout among these professionals.
Methods
A nationwide, multicentre cross-sectional quantitative survey study was conducted in Portugal.
Survey instruments
A questionnaire of socio-demographic variables and data on professional background (e.g., post-graduate education in intensive care/palliative care).
A questionnaire, based on Embriaco et al [12], with a set of workplace experiences in the week prior to and day of questionnaire completion, including workload and conflicts (intra-team, inter-team, with a superior, with patients, with family members).
A questionnaire on ethical decisions in the week prior to and day of questionnaire completion, including withholding/withdrawing treatment; palliative sedation; communication and information disclosure of the diagnosis and prognosis to a patient/family.
The Maslach Burnout Inventory—Human Services Survey (MBI-HSS). This is a self-report questionnaire that comprises a total of 22 items, corresponding to the three burnout sub-dimensions defined by Maslach et al [21–25]: Emotional Exhaustion (EE) with nine items; Depersonalization (DEP) with five items; and Personal and Professional Accomplishment (PPA) with eight items. The MBI-HSS asks respondents to indicate on a seven-point Likert scale the frequency of experiencing certain feelings related to their work. The MBI-HSS is scored according to the presence and severity of Emotional Exhaustion (EE), Depersonalization (DEP), and reduced sense of Personal and Professional Accomplishment (PPA). This is the most common, widely described and internationally validated instrument used to assess all the three dimensions of burnout. The MBI-HSS has been found to be reliable, valid, and easy to administer [24].
A Portuguese cross-culturally adapted and validated version of the MBI-HSS was used [26], which is aligned with recent international methodological recommendations in this field [27]. Cut-off scores were defined for each dimension and we adopted the following internationally established definition of burnout: high levels of EE and DEP combined with low PPA [3,21–26]. Both the cut-off scores and the definitions of burnout were cross-culturally adapted and validated into the Portuguese context [26]. The risk of burnout was defined as follows: high risk, two of the three dimensions beyond the cut-off point; average risk, one of the three dimensions beyond the cut-off point; low risk, average or low levels in the dimensions EE and DEP, and high or average levels in PPA [24–26,28,29]. For the present statistical analysis, a high level of burnout (high burnout) was defined as the sum of being both in burnout and with high risk of burnout [4,18,22–24,26,28–30].
Setting, participants, data collection and ethical approval
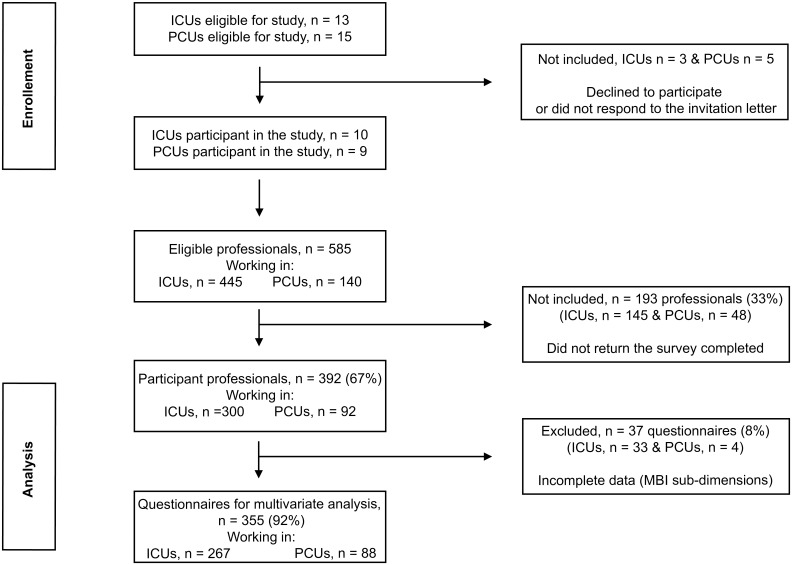
All 15 Portuguese PC teams designated in the webpage of the Portuguese Association for Palliative Care (Associação Portuguesa de Cuidados Paliativos, APCP) in September 2008, hence recognized as providing a specialist level of palliative care, and 13 ICUs based in state hospitals in the North of Portugal were invited to participate in this study. Nine PCUs (N = 140 physicians and nurses) and ten ICUs (N = 445 physicians and nurses) accepted this invitation (Fig 1). PCUs were geographically dispersed, covering the North, Centrum and South regions of the country. ICUs were polyvalent and the median Simplified Acute Physiology Score II score at admission was 45. The final sampling frame (i.e., a list of all physicians and nurses in the target population) was 585. These physicians and nurses from all participant PCUs and ICUs were invited to complete the survey.
Fig 1. Study flowchart.
This figure illustrates all the steps followed from participants’ enrollment throughout their inclusion in the analyses.
The study was presented during team-meetings at all participant units where the self-administered questionnaires were distributed. Professionals who were absent or on shift work were handed questionnaires by the head nurse of the unit at a separate time. Completed surveys were inserted into an envelope-box in each unit and collected by the researchers. Participation was anonymous and voluntary. Data collection occurred from October 2008 throughout December 2009.
Ethical approval was obtained from the ethics and scientific committees of the Instituto de Bioética, Universidade Católica Portuguesa. Institutional and ethical approvals were also obtained from all participant institutions, together with the informed consent of each team and participant. Participation was anonymous and voluntary. Data were analyzed and presented with full anonymity.
Statistical analysis
Data analysis was performed using proper software (SPSS version 21.0). Summary statistics were applied as appropriate. Categorical variables were described through absolute frequencies (n) and relative (%) ones. As the distribution of continuous variables was asymmetric, they were described using the median together with 25th and 75th percentiles. Due to the different sample sizes and the skewness of distributions, only nonparametric exact tests were applied. A Chi-square (χ2) independence test was used to examine the association between categorical variables. The Fisher exact test was used when the expected frequency (in any cell of the contingency table analysis) on the association of two categorical variables was less than five. The Mann-Whitney test was used to test hypotheses concerning continuous variables, since their distribution was asymmetric. Univariate and multivariate logistic regression analysis were used to determine odds ratio (OR) sidelong with 95% Confidence Intervals (CI). A significance level of 0.05 was used for all hypothesis tests.
Results
Characteristics of the participants
A total of 392 professionals from ICUs and PCUs completed the survey (67% response rate) (Fig 1). Out of these 392 professionals, 300 (77%) worked in ICUs and 92 (23%) in PCUs. The majority (69%) was women, had a median age of 32, and was non-married (55%). The sample comprised a total of 292 (74%) nurses and 100 (26%) physicians. 361 (92%) respondents were graduated in medicine/nursing and a minority was awarded with a master (6%) or a PhD (2%) degree. 107 (28%) respondents obtained post-graduate education/training in intensive/palliative care. This occurred more frequently among professionals working in PCUs (p = .031). See Table 1.
Table 1. Characteristics of participants.
med: median. P: Percentile.
| Total (n = 392) |
Setting | p | |||||
|---|---|---|---|---|---|---|---|
| Intensive Care | Palliative Care | ||||||
| (n = 300; 76.5%) | (n = 92; 23.5%) | ||||||
| Gender | |||||||
| Female | 271 | (69) | 195 | (65) | 76 | (83) | 0.001* |
| Male | 121 | (31) | 105 | (35) | 16 | (17) | |
| Age, med (P25-P75) | 32 | (28–39) | 32 | (28–39) | 32 | (26–40) | 0.848§ |
| Marital Status | |||||||
| Not married | 171 | (55) | 139 | (46) | 38 | (41) | 0.099* |
| Married | 177 | (45) | 161 | (54) | 54 | (59) | |
| Profession | |||||||
| Physician | 100 | (26) | 82 | (27) | 18 | (20) | 0.135* |
| Nurse | 292 | (74) | 218 | (73) | 74 | (80) | |
| Education level | |||||||
| Graduation degree | 361 | (92) | 280 | (94) | 80 | (87) | 0.028* |
| Master | 25 | (6) | 12 | (4) | 12 | (13) | |
| Doctorate | 6 | (2) | 6 | (2) | 0 | (0) | |
| Post-graduate education in intensive/palliative care | |||||||
| No | 273 | (72) | 215 | (75) | 58 | (63) | 0.031* |
| Yes | 107 | (28) | 73 | (25) | 34 | (37) | |
* Independent χ2 exact test.
§ Mann-Whitney Test.
Significant findings highlighted in bold.
Burnout levels in ICUs and PCUs
A high level of burnout was identified in 27% of the respondents (19% were in high risk and 8% were experiencing burnout). 62% of the participants exhibited average and high levels of Emotional Exhaustion (EE), 60% average and high levels of Depersonalization (DEP), and 38% high levels of Personal and Professional Accomplishment (PPA). Significant differences were found between ICUs and PCUs. While 31% of the professionals working in ICUs had a high level of burnout, only 16% of the professionals working in PCUs presented that level of burnout (p = .006). Furthermore, the majority of PC practitioners (55%) exhibited a low risk of burnout; diverse findings were found among intensivists (39%), p = .022. Nevertheless, the latter group of professionals showed higher levels of PPA (42%) when compared to those working in PC (27%), p = .001. Contrariwise, the highest levels of DEP were found among professionals working in ICUs (27% of the respondents of this group reported a high level of DEP) and the lowest levels of DEP were identified among those working in PCUs (54% of the participants of this group), p = .001. No significant differences were found when comparing both settings for the sub-dimension of EE (Table 2).
Table 2. Results from the three dimensions of the Maslach Burnout Inventory–Human Services Survey (MBI-HSS) per setting of care (ICU vs. PCU).
| Setting | |||||||
|---|---|---|---|---|---|---|---|
| Total (n = 392) |
PCU (n = 92; 23.5%) |
ICU (n = 300; 76.5%) |
p* | ||||
| n | (%) | n | (%) | n | (%) | ||
| Maslach Burnout Inventory–Human Services Survey (MBI-HSS) | |||||||
| Emotional Exhaustion (EE) | |||||||
| Low (< = 14) | 144 | (39) | 38 | (43) | 106 | (38) | 0.637 |
| Average (15 a 24) | 110 | (30) | 26 | (29) | 84 | (30) | |
| High (> = 25) | 117 | (32) | 25 | (28) | 92 | (33) | |
| Depersonalization (DEP) | |||||||
| Low (< = 3) | 154 | (40) | 50 | (54) | 104 | (36) | 0.001 |
| Average (4 a 9) | 142 | (37) | 33 | (36) | 109 | (37) | |
| High (> = 10) | 87 | (23) | 9 | (10) | 78 | (27) | |
| Personal and Professional Accomplishment (PPA) | |||||||
| Low (> = 40) | 104 | (28) | 39 | (43) | 65 | (23) | 0.001 |
| Average (33 a 39) | 124 | (34) | 27 | (30) | 97 | (35) | |
| High (< = 32) | 140 | (38) | 25 | (27) | 115 | (42) | |
| Burnout | |||||||
| Low risk | 152 | (43) | 48 | (55) | 104 | (39) | 0.022 |
| Medium risk | 106 | (30) | 26 | (30) | 80 | (30) | |
| High risk (Hr) | 69 | (19) | 11 | (13) | 58 | (22) | |
| In Burnout (InB) | 28 | (8) | 3 | (3) | 25 | (9) | |
| High level of Burnout | |||||||
| No | 258 | (73) | 74 | (84) | 184 | (69) | 0.006 |
| Yes (Hr + InB) | 97 | (27) | 14 | (16) | 83 | (31) | |
*Independent χ2 exact test.
Significant findings highlighted in bold.
In order to perform logistic regression analysis, 37 (8%) questionnaires had to be removed from our sample due to incomplete responses in the sub-dimensions of the MBI-HSS. Hence, the following results refer to a sample of 355 participants (Fig 1).
Univariate logistic regression analysis showed that the odds of exhibiting burnout were 2.384 times higher in ICUs than in PCUs. When controlling for socio-demographic, profession and workplace related variables, differences between both settings remained significant: OR = 2.525 (Table 3).
Table 3. Burnout in ICU versus PCU.
| Burnout | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Total (n = 355) |
No (n = 258; 73%) |
Yes (n = 97; 27%) |
P¶ | OR* (95%CI) | OR** (95%CI) | ||||
| Setting | |||||||||
| PCU | 88 | (25) | 74 | (29) | 14 | (14) | 0.006 | 1.000 | 1.000 |
| ICU | 267 | (75) | 184 | (71) | 83 | (86) | 2.384 (1.273–4.465) | 2.525 (1.025–6.221) | |
¶Independent χ2 exact test.
*Odds Ratio Univariate.
**Odds Ratio Multivariate.
CI: Confidence Interval. Significant findings highlighted in bold.
Burnout in ICUs and PCUs: Determinant workplace conditions
Univariate regression analyses showed that, amongst others, higher burnout levels were significantly associated with the following workplace experiences: night shifts (OR = 2.232) and occurrence of conflicts (OR = 2.074) in the week prior to questionnaire completion, conflicts with other professionals in the week prior to (OR = 6.995) and day of questionnaire completion (OR = 7.176), and conflicts with patients (OR = 4.782) in the week before filling-in the survey. Burnout was also associated with experiencing a patient’s death in the day of questionnaire completion (OR = 1.866) and with ethical decision-making in the prior week. (Tables 4 and 5)
Table 4. Burnout related to workplace experiences in the week prior to survey completion.
| Burnout | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Total (n = 355) |
No (n = 258; 73%) |
Yes (n = 97; 27%) |
P | OR* (95%CI) |
OR** (95%CI) |
||||
| In the week prior to survey completion: | |||||||||
| Nigh shifts | |||||||||
| No | 96 | (28) | 80 | (32) | 16 | (18) | 0.008¶ | 1.000 | 1.000 |
| Yes | 243 | (72) | 168 | (68) | 75 | (82) |
2.232 (1.223–4.075) |
1.877 (1.006–3.500) |
|
| Extra shifts | |||||||||
| No | 229 | (69) | 168 | (69) | 61 | (69) | 0.935¶ | 1.000 | 1.000 |
| Yes | 103 | (31) | 76 | (31) | 27 | (31) | 0.978 (0.577–1.659) |
0.885 (0.518–1.514) |
|
| Days-off | |||||||||
| No | 113 | (33) | 88 | (35) | 25 | (27) | 0.173¶ | 1.000 | 1.000 |
| Yes | 227 | (67) | 161 | (65) | 66 | (73) | 1.443 (0.851–2.448) |
1.443 (0.846–2.461) |
|
| Vacations/Holidays | |||||||||
| No | 300 | (92) | 216 | (91) | 84 | (94) | 0.336¶ | 1.000 | 1.000 |
| Yes | 26 | (8) | 21 | (9) | 5 | (6) | 0.612 (0.224–1.677) |
0.669 (0.241–1.855) |
|
| Patient’s death | |||||||||
| No | 158 | (48) | 122 | (51) | 36 | (42) | 0.163¶ | 1.000 | 1.000 |
| Yes | 169 | (52) | 119 | (49) | 50 | (58) | 1.424 (0.866–2.341) |
1.402 (0.849–2.317) |
|
| Number of deceased patients | |||||||||
| 0 | 158 | (45) | 122 | (47) | 36 | (38) | 0.257¶ | 1.000 | 1.000 |
| 1 a 2 | 141 | (40) | 98 | (38) | 43 | (45) | 1.487 (0.887–2.492) |
1.412 (0.838–2.381) |
|
| ≥3 | 55 | (16) | 38 | (15) | 17 | (18) | 1.516(0.766–2.999) | 1.495(0.750–2.980) | |
| Conflicts | |||||||||
| No | 261 | (79) | 201 | (83) | 60 | (70) | 0.011¶ | 1.000 | 1.000 |
| Yes | 68 | (21) | 42 | (17) | 26 | (30) |
2.074 (1.175–3.659) |
2.170 (1.218–3.866) |
|
| Conflicts with: | |||||||||
| Colleagues | |||||||||
| No | 304 | (92) | 226 | (93) | 78 | (88) | 0.090¶ | 1.000 | 1.000 |
| Yes | 27 | (8) | 16 | (7) | 11 | (12) | 1.992 (0.886–4.476) |
1.952 (0.859–4.432) |
|
| Superiors | |||||||||
| No | 311 | (93) | 230 | (94) | 81 | (91) | 0.360¶ | 1.000 | 1.000 |
| Yes | 23 | (7) | 15 | (6) | 8 | (9) | 1.514 (0.619–3.705) |
1.526 (0.617–3.778) |
|
| Other Professionals | |||||||||
| No | 309 | (93) | 237 | (97) | 72 | (81) | <0.001¶ | 1.000 | 1.000 |
| Yes | 25 | (7) | 8 | (3) | 17 | (19) |
6.995 (2.899–16.876) |
6.701 (2.752–16.318) |
|
| Patients | |||||||||
| No | 325 | (98) | 241 | (99) | 84 | (94) | 0.034₸ | 1.000 | 1.000 |
| Yes | 8 | (2) | 3 | (1) | 5 | (6) |
4.782 (1.119–20.441) |
7.514 (1.624–34.764) |
|
| Family members | |||||||||
| No | 307 | (95) | 225 | (96) | 82 | (92) | 0.262₸ | 1.000 | 1.000 |
| Yes | 17 | (5) | 10 | (4) | 7 | (8) | 1.921 (0.708–5.213) |
2.779 (0.962–8.030) |
|
| Ethical decisions: | |||||||||
| Withdrawing treatment | |||||||||
| No | 245 | (74) | 188 | (77) | 57 | (66) | 0.041¶ | 1.000 | 1.000 |
| Yes | 87 | (26) | 57 | (23) | 30 | (34) |
1.736 (1.019–2.956) |
1.715 (1.001–2.936) |
|
| Withholding treatment | |||||||||
| No | 220 | (67) | 174 | (71) | 46 | (53) | 0.003¶ | 1.000 | 1.000 |
| Yes | 110 | (33) | 70 | (29) | 40 | (47) |
2.161 (1.303–3.587) |
2.108 (1.263–3.518) |
|
| Palliative sedation | |||||||||
| No | 256 | (78) | 197 | (81) | 59 | (69) | 0.020¶ | 1.000 | 1.000 |
| Yes | 74 | (22) | 47 | (19) | 27 | (31) |
1.918 (1.101–3.343) |
1.739 (0.990–3.056) |
|
| Communication about the diagnose/prognoses with the patient | |||||||||
| No | 220 | (66) | 155 | (63) | 65 | (73) | 0.088¶ | 1.000 | 1.000 |
| Yes | 115 | (34) | 91 | (37) | 24 | (27) | 0.629 (0.368–1.074) |
0.684 (0.398–1.177) |
|
| Communication about the diagnose/prognoses with the family | |||||||||
| No | 142 | (42) | 106 | (43) | 36 | (41) | 0.744¶ | 1.000 | 1.000 |
| Yes | 193 | (58) | 141 | (57) | 52 | (59) | 1.086 (0.663–1.780) |
1.101 (0.668–1.813) |
|
¶Independent χ2 exact test.
§ Mann-Whitney Test.
₸ Fisher exact test
*Odds Ratio Univariate.
**Odds Ratio adjusted to the setting (ICU/PCU).
CI: Confidence Interval. Significant findings highlighted in bold.
Table 5. Burnout related to workplace experiences in the day of survey completion.
| Burnout | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Total (n = 355) |
No (n = 258; 73%) |
Yes (n = 97; 27%) |
p | OR* (95%CI) |
OR** (95%CI) |
||||
| In the day of survey completion: | |||||||||
| Caring for a dying patient | |||||||||
| No | 228 | (69) | 172 | (71) | 56 | (63) | 0.141¶ | 1.000 | 1.000 |
| Yes | 102 | (31) | 69 | (29) | 33 | (37) | 1.469 (0.880–2.453) |
1.633 (0.965–2.764) |
|
| Patient’s death | |||||||||
| No | 295 | (94) | 213 | (93) | 82 | (94) | 0.011¶ | 1.000 | 1.000 |
| Yes | 20 | (6) | 15 | (7) | 5 | (6) | 1.866 (1.305–2.459) |
0.720 (0.251–2.060) |
|
| Conflicts | |||||||||
| No | 325 | (96) | 241 | (97) | 84 | (93) | 0.116₸ | 1.000 | 1.000 |
| Yes | 13 | (4) | 7 | (3) | 6 | (7) | 2.459 (0.804–7.525) |
2.629 (0.840–8.224) |
|
| Conflicts with: | |||||||||
| Colleagues | |||||||||
| No | 330 | (98) | 241 | (98) | 89 | (99) | 0.680₸ | 1.000 | 1.000 |
| Yes | 7 | (2) | 6 | (2) | 1 | (1) | 0.451 (0.054–3.801) |
0.371 (0.044–3.137) |
|
| Superiors | |||||||||
| No | 331 | (98) | 244 | (99) | 87 | (97) | 0.196₸ | 1.000 | 1.000 |
| Yes | 6 | (2) | 3 | (1) | 3 | (3) | 2.805 (0.556–14.156) |
2.663 (0.518–13.697) |
|
| Other professionals | |||||||||
| No | 329 | (98) | 244 | (99) | 85 | (94) | 0.007¶ | 1.000 | 1.000 |
| Yes | 7 | (2) | 2 | (1) | 5 | (6) |
7.176 (1.367–37.679) |
7.848 (1.445–42.628) |
|
| Patients | |||||||||
| No | 331 | (99) | 245 | (99) | 86 | (99) | 1.000₸ | 1.000 | 1.000 |
| Yes | 3 | (1) | 2 | (1) | 1 | (1) | 1.424 (0.128–15.907) |
1.188 (0.106–13.304) |
|
| Family members | |||||||||
| No | 331 | (99) | 244 | (100) | 87 | (99) | 0.459₸ | 1.000 | 1.000 |
| Yes | 2 | (1) | 1 | (0) | 1 | (1) | 2.805 (0.174–45.325) |
3.541 (0.205–61.306) |
|
| Ethical decisions: | |||||||||
| Withdrawing treatment | |||||||||
| No | 309 | (92) | 228 | (93) | 81 | (90) | 0.353¶ | 1.000 | 1.000 |
| Yes | 26 | (8) | 17 | (7) | 9 | (10) | 1.490 (0.639–3.475) |
1.567 (0.662–3.705) |
|
| Withholding treatment | |||||||||
| No | 298 | (89) | 214 | (88) | 84 | (92) | 0.232¶ | 1.000 | 1.000 |
| Yes | 37 | (11) | 30 | (12) | 7 | (8) | 0.594 (0.251–1.406) |
0.606 (0.254–1.445) |
|
| Palliative sedation | |||||||||
| No | 308 | (92) | 224 | (91) | 84 | (93) | 0.570¶ | 1.000 | 1.000 |
| Yes | 27 | (8) | 21 | (9) | 6 | (7) | 0.762 (0.297–1.953) |
0.804 (0.310–2.083) |
|
| Communication about the diagnose/prognoses with the patient | |||||||||
| No | 285 | (85) | 210 | (85) | 75 | (82) | 0.506¶ | 1.000 | 1.000 |
| Yes | 52 | (15) | 36 | (15) | 16 | (18) | 1.244 (0.653–2.372) |
1.387 (0.717–2.683) |
|
| Communication about the diagnose/prognoses with the family | |||||||||
| No | 244 | (72) | 179 | (73) | 65 | (71) | 0.808¶ | 1.000 | 1.000 |
| Yes | 93 | (28) | 67 | (27) | 26 | (29) | 1.069 (0.626–1.824) |
1.118 (0.650–1.922) |
|
¶Independent χ2 exact test.
§ Mann-Whitney Test.
₸ Fisher exact test
*Odds Ratio Univariate.
**Odds Ratio adjusted to the setting (ICU/PCU).
CI: Confidence Interval. Significant findings highlighted in bold.
When adjusting for the setting (i.e., ICUs/PCUs), night shifts and experiencing conflicts in the week prior to survey completion were associated with higher burnout levels (OR = 1.877 and 2.170, respectively). Certain experiences in the week before participating in the survey also remained significantly associated to burnout, namely: conflicts with other professionals (OR = 6.701), conflicts with patients (OR = 7.514), withholding treatment (OR = 2.108), and withdrawing treatment (OR = 1.715). Conflicts with other professionals in the day of questionnaire completion remained significant and positively associated to burnout (OR = 7.848). (Tables 4 and 5)
When controlling for socio-demographic and educational characteristics of the participant professionals and for the setting (ICUs vs. PCUs) in the multivariate logistic regression analyses, the only variables that remained significantly associated to burnout were 'conflicts' and having post-graduate education in IC/PC. Experiencing conflicts increased the odds of exhibiting burnout 3.124 times and having post-graduate education diminished its likelihood (OR = 0.395). See Table 6.
Table 6. Burnout in ICU and PCU related to socio-demographic, professional and workplace experiences in the week prior to survey completion.
med-median. P-Percentile.
| Burnout | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total (n = 355) |
No (n = 258; 73%) |
Yes (n = 97; 27%) |
p | OR* (95%CI) |
OR** (95%CI) |
OR*** IC 95% N = 288 (81%) |
||||
| Setting | ||||||||||
| PCU | 88 | (25) | 74 | (29) | 14 | (14) | 0.006¶ | 1.000 | - | 1.000 |
| ICU | 267 | (75) | 184 | (71) | 83 | (86) |
2.384 (1.273–4.465) |
- |
2.525 (1.025–6.221) |
|
| Gender | ||||||||||
| Female | 245 | (69) | 178 | (69) | 67 | (69) | 0.988¶ | 1.000 | 1.000 | 1.000 |
| Male | 110 | (31) | 80 | (31) | 30 | (31) | 0.996 (0.601–1.651) |
0.886 (0.530–1.483) |
0.719 (0.360–1.440) |
|
| Age med (P25-P75) | 32 | (27–38) | 33 | (28–40) | 30 | (27–35) | 0.004§ |
0.955 (0.925–0.986) |
0.955 (0.924–0.986) |
0.915 (0.764–1.097) |
| Marital Status | ||||||||||
| Single | 158 | (45) | 106 | (41) | 52 | (54) | 0.106¶ | 1.000 | 1.000 | 1.000 |
| Married | 156 | (44) | 120 | (47) | 36 | (37) | 0.612 (0.371–1.007) |
0.610 (0.368–1.009) |
1.136 (0.502–2.573) |
|
| Divorced/Widow/Other | 41 | (12) | 32 | (12) | 9 | (9) | 0.573 (0.255–1.289) |
0.631 (0.277–1.435) |
0.872 (0.270–2.817) |
|
| Profession | ||||||||||
| Physician | 91 | (26) | 73 | (28) | 18 | (19) | 0.061¶ | 1.000 | 1.000 | 1.000 |
| Nurse | 264 | (74) | 185 | (72) | 79 | (81) | 1.732 (0.970–3.091) |
1.849 (1.029–3.321) |
1.673 (0.494–5.666) |
|
| Post-graduate education in intensive/palliative care | ||||||||||
| No | 248 | (72) | 177 | (71) | 71 | (76) | 0.285¶ | 1.000 | 1.000 | 1.000 |
| Yes | 96 | (28) | 74 | (29) | 22 | (24) | 0.741 (0.428–1.284) |
0.808 (0.462–1.412) |
0.395 (0.178–0.878) |
|
| Shift work | ||||||||||
| No | 68 | (19) | 56 | (22) | 12 | (12) | 0.045¶ | 1.000 | 1.000 | 1.000 |
| Yes | 286 | (81) | 201 | (78) | 85 | (88) |
1.973 (1.007–3.868) |
1.660 (0.833–3.311) |
0.947 (0.351–2.555) |
|
| Nr. of working hours per week | ||||||||||
| 35 hours | 117 | (33) | 89 | (35) | 28 | (29) | 0.029¶ | 1.000 | 1.000 | 1.000 |
| 40 hours | 125 | (35) | 79 | (31) | 46 | (47) |
1.851 (1.058–3.237) |
1.896 (1.079–3.330) |
1.797 (0.638–5.066) |
|
| 42 hours | 55 | (16) | 43 | (17) | 12 | (12) | 0.887 (0.412–1.912) |
0.949 (0.437–2.060) |
2.124 (0.653–6.912) |
|
| Other | 57 | (16) | 46 | (18) | 11 | (11) | 0.760 (0.347–1.663) |
1.036 (0.453–2.367) |
1.527 (0.483–4.828) |
|
| In the week prior to survey completion: | ||||||||||
| Night shifts | ||||||||||
| No | 96 | (28) | 80 | (32) | 16 | (18) | 0.008¶ | 1.000 | 1.000 | 1.000 |
| Yes | 243 | (72) | 168 | (68) | 75 | (82) |
2.232 (1.223–4.075) |
1.877 (1.006–3.500) |
0.902 (0.421–1.929) |
|
| Patient’s death | ||||||||||
| No | 158 | (48) | 122 | (51) | 36 | (42) | 0.163¶ | 1.000 | 1.000 | 1.000 |
| Yes | 169 | (52) | 119 | (49) | 50 | (58) | 1.424 (0.866–2.341) |
1.402 (0.849–2.317) |
0.950 (0.462–1.953) |
|
| Conflicts | ||||||||||
| No | 261 | (79) | 201 | (83) | 60 | (70) | 0.011¶ | 1.000 | 1.000 | 1.000 |
| Yes | 68 | (21) | 42 | (17) | 26 | (30) |
2.074 (1.175–3.659) |
2.170 (1.218–3.866) |
3.124 (1.475–6.619) |
|
| Ethical decisions | ||||||||||
| Withdrawing treatment | ||||||||||
| No | 245 | (74) | 188 | (77) | 57 | (66) | 0.041¶ | 1.000 | 1.000 | 1.000 |
| Yes | 87 | (26) | 57 | (23) | 30 | (34) |
1.736 (1.019–2.956) |
1.715 (1.001–2.936) |
1.360 (0.536–3.448) |
|
| Withholding treatment | ||||||||||
| No | 220 | (67) | 174 | (71) | 46 | (53) | 0.003¶ | 1.000 | 1.000 | 1.000 |
| Yes | 110 | (33) | 70 | (29) | 40 | (47) |
2.161 (1.303–3.587) |
2.108 (1.263–3.518) |
1.865 (0.840–4.142) |
|
| Palliative sedation | ||||||||||
| No | 256 | (78) | 197 | (81) | 59 | (69) | 0.020¶ | 1.000 | 1.000 | 1.000 |
| Yes | 74 | (22) | 47 | (19) | 27 | (31) |
1.918 (1.101–3.343) |
1.739 (0.990–3.056) |
1.221 (0.494–3.022) |
|
¶Independent χ2 exact test.
§ Mann-Whitney Test.
*Odds Ratio Univariate.
**Odds Ratio adjusted to the setting (ICU/PCU).
***Odds Ratio adjusted to all variables present in the table.
CI: Confidence Interval. Significant findings highlighted in bold.
Discussion
Our results show that a substantial proportion of professionals working in ICUs and PCUs are at high risk of developing burnout and that the likelihood of developing this syndrome is significantly higher in intensive care units (ICUs) when compared to palliative care units (PCUs). Developing burnout is associated with several workplace conditions, such as experiencing conflicts (e.g., with patients and/or families, intra and/or inter-teams). Post-graduate education plays a relevant role in diminishing the risk of burnout.
Burnout in ICUs and PCUs: Does it make a difference?
A significant percentage of physicians and nurses working in ICUs and PCUs either were experiencing burnout or were at high risk of developing burnout. This is of foremost relevance as it means that these professionals were exhausted, established cold, cynical and distant relationships and experienced a reduced sense of personal and professional accomplishment [2,3], thus affecting the quality of interactions, inter-professional relations and care provision. Indeed, our findings pinpointed that a large percentage of professionals had high levels of depersonalization. Patients suffering from life-threatening diseases, at the very end-of-life, are in a condition of vulnerability. This vulnerability may be increased if these patients are being cared for by professionals who are themselves affected in their health status, as high levels of burnout are related to health problems such as depressive symptoms [31–35].
As described elsewhere [1], the ethical dimension and framework to understand burnout is related to its consequences, especially at two levels: (i) the increase in the patient’s vulnerability owing to the consequences that burnout may have for patients and their relatives; and (ii) the increase in professionals’ vulnerability due to their condition of suffering from a work-related syndrome affecting their own health. A third level of the ethical framework to understand burnout refers to the principle of responsibility in terms of burnout prevention at individual (to take care of oneself), team (to take care for oneself and for the others) and organizational (e.g., organizational ethics, creating empowering workplace conditions) levels [1].
In what refers to the sub-dimensions of burnout, our findings are a source of major concern. First, the large proportion of professionals experiencing emotional exhaustion constitutes a risk to patient safety and for the quality of care. Burnout was identified as a predictor of reporting major medical errors by physicians [36–43], affecting patients’ safety and wellbeing. This, however, is not consensual. A recent study showed that medical errors were associated to depressive symptoms among ICU staff but not to burnout [44]. In a six-country cross-national study, it was found that burnout in nurses was associated with reduced quality of care, lower patient satisfaction and increased errors [45]. Second, the consequences of depersonalization may undermine the relationship, communication and inter-connection established among professionals, patients and families. Evidence shows that high levels of depersonalization were associated with self-reported sub-optimal care provision [46] and with a sense of not dedicating enough time to patients [39]. Third, the consequences of a lack of personal and professional accomplishment may affect the whole care system at micro, meso and macro levels due to absenteeism, turnover, and intention to leave [6,12,13,31,47]. In fact, excessive turnover rates increase healthcare costs, decrease productivity, lower staff morale, and reduce the overall quality of care, because experienced professionals who leave their workplaces must be replaced [13,47–50]. Considering the major financial crisis and its effects in the Portuguese healthcare system, this is particularly important. For instance, in Canada, a recent study showed that the total cost of burnout among Canadian physicians was estimated to be more than $200 million [51]. In the United States, replacement costs have been estimated to be at least $250,000 for each primary care physician, an amount certainly higher for other medical specialties, namely intensive and palliative care [52]. It is imperative not only to consider the effect of constrained resources in the shortage of the healthcare workforce, but also to implement strategies aiming at improving organizational structures and processes that can reduce the micro-meso-macro consequences of burnout and increase the satisfaction and wellbeing of healthcare professionals [4,48].
Our findings also showed that working in ICUs more than doubled the likelihood of having burnout when compared to working in PCUs. These findings are similar to those found in other studies, suggesting that burnout in PCUs is comparable or lower than in other healthcare settings [1,9,53,54]. Possible explanations were provided by several authors who emphasize the meaning given by PC professionals and teams to caring for patients facing life-threatening diseases and promoting their wellbeing and quality of life. This contributes to the development of personal awareness and gives a sense of gratification [1,18,19,55–59]. Furthermore, by being one of the dimensions of healthcare professional empowerment, meaning is paramount as it gives a sense of purpose or personal connection about the care provided in the workplace [6,59].
In addition, it seems that PC teams embrace active strategies and rituals when facing a patient’s death, helping them to cope with those losses [1,55–57,60]. Several authors have emphasized that professionals working in palliative care usually make additional recommendations on how to prevent and deal with burnout. These professionals are encouraged to focus on spirituality and human nature, methods for self-care including taking regular breaks from work and focusing on the positive aspects of life, so that one is not overwhelmed by adversity and suffering [61–64].
Contrarily, time pressure in ICUs may damper communication within the team and between professionals and patients. This may increase stress, tensions and conflicts that can boost the risk of developing burnout [9,13,14,47,65–69].
Burnout in ICUs and PCUs: What can make a difference?
Several workplace factors (e.g., night shifts, patient’s death, conflicts, and ethical decisions) were associated with burnout. These findings are aligned with other studies [4,12,16,31,47,66] showing the impact of socio-structural workplace conditions on professionals’ wellbeing. However, when controlling for socio-demographic, setting, and workplace variables, the only variables that remained significantly associated with burnout were conflicts and having post-graduate education in intensive/palliative care. While experiencing conflicts strongly increased the likelihood of burnout, having post-graduate education diminished its chances.
This is not surprising since the occurrence of conflicts at work was identified as a major burnout risk factor in the literature [4,14,16,31,47,66]. We cannot ensure, however, that there is a cause-effect relationship in which conflicts cause burnout. It can also occur that professionals with burnout more often experience conflicts. Conflicts result mainly from disagreements about the goals of treatment and care pathways, the philosophy of care, ethical decision-making, end-of-life care, and inter-professional relations [4,47,65,66,70–74]. Hence, it is paramount to ensure and promote inter-professional and team-based strategies (e.g., team meetings, quality improvement initiatives) aiming at improving communication, organization and sharing visions. Well-led meetings may promote a sense that all team members “have a voice” and contribute equally to the chain-of-events affecting patient and family care outcomes, professionals’ wellbeing, and conflicts [73–76]. This is a current practice, part of daily dynamics in PCUs and a protective factor against burnout [5,18,76,77]. Inter-professional team-based working strategies from PCUs may therefore be translated into ICUs, helping to overcome some burnout-associated factors (e.g., conflicts and end-of-life decision-making). Involving the interdisciplinary team may indeed leverage aspects of interaction among professionals that may ameliorate burnout [5,78,79].
Finally, our findings show that post-graduate education in intensive/palliative care plays a relevant role in protecting professionals from burnout and happened more frequently among PC professionals. This is in line with other studies showing that post-graduate education or other specific education programs were inversely associated to burnout [1,5,16,18] and highlights the need to further implement education programs in intensive/palliative care as part of the integration process of professionals in ICUs and PCUs. Professionals with higher levels of education are able to develop their awareness about the purposes of care provision in their field of practice. Through education, death may not be seen as frustration or failure [5,18,80] and communication and end-of-life decision-making may be improved; for instance, by providing education about PC to professionals working in ICUs [81,82]. By creating awareness, education about palliative care may also increase healthcare professionals’ perceptions of self-efficacy and empowerment. This has been identified as a determinant factor of self-perceived effectiveness among healthcare professionals [6]. Furthermore, a recent systematic review has shown that interventions aimed at improving the wellbeing of staff working in palliative care settings comprised a mixture of activities, including education [83]. The interdisciplinary approaches used in most of the post-graduate programs in IC/PC may foster the development of inter-professional communication competencies, contributing to conflict management. It can also be that post-graduate education programs in palliative care provide healthcare professionals with “managing people and change” competencies, which enhance perceptions of empowerment and effectiveness in the workplace [5,6].
Strengths, limitations and further research
A major strength of our study is its originality and relevance to a wide audience when comparing burnout among healthcare professionals providing end-of-life care in two specific settings: ICUs and PCUs. To our best knowledge, this is the first study making such a comparison. Hence, our findings contribute to the existing literature about burnout in end of life care. Furthermore, it provides relevant information that may foster an understanding and a reflection on the potential and need of integrating palliative care approaches and practices into intensive care. This calls for further research on the best integration models and their effectiveness for patient and family-related outcomes, for professionals and teams’ well-being and for the resilience and sustainability of healthcare services and systems.
Nevertheless, a few limitations need to be considered. First, the study used a cross-sectional design and a nonrandomized sampling procedure. The geographic location of the participant units varied (while palliative care units were located nationwide, intensive care units were situated only in the North of the country). This makes the generalization of findings limited. Second, lower burnout levels in palliative care need to be seen with some caution. It is relevant to note, however, that we obtained a considerably high response rate (approximately 70% of the potential participants completed the survey). Moreover, previous research conducted with the same palliative care units [5,18,57] support our findings. Third, the subjectivity inherent to the concept of conflict may be considered. Since we aggregated all types of conflicts (intra-team, inter-teams, with a superior, with patients, with family members) for the multivariate analysis, more research is needed to complement the understanding of this variable significantly associated to burnout. Finally, while we used internationally and Portuguese validated definition criteria and cut-off scores to assess burnout [3,21–26], it is worth mention that accurate specific cut-off values for US critical care professionals have not been determined yet [9,13]; the same occurs for palliative care professionals. Nevertheless, international evidence indicates that the MBI-HSS seems to be quite usable across diverse national and cultural work settings. In fact, it is striking that results from different countries both in the United States and in Europe are so similar [27–30].
The results of this study highlight the need for a better and regular assessment of professional burnout and its associated organizational factors and workplace experiences in palliative and intensive care. Further research is needed to assess the organizational culture and the factors needed to sustain healthy work environments. In our opinion, these studies should provide an in-depth and meaningful understanding on what and how personal characteristics of the professionals, specific conflicts, organizational and socio-structural factors of the workplace and situations associated to end-of-life care in these settings may increase or prevent burnout.
Conclusions
In this study, a high level of burnout was identified in 27% of the professionals. Working in intensive care units more than doubled the likelihood of exhibiting burnout when compared to working in palliative care units. Experiencing conflicts was the most significant determinant of burnout and post-graduate education in intensive/palliative care protected professionals from developing this syndrome. This highlights the need for promoting empowering workplace conditions, such as education programs, leadership, team empowerment and conflict management. The use of a “toolbox” for early assessment of burnout and the promotion of empowering workplace conditions (e.g., interdisciplinary teamwork, teamwork practices and dynamics, and conflict management) can be determinant for burnout prevention and minimization. These and other strategies aimed at improving organizational structures and processes can reduce the micro-meso-macro consequences of burnout and increase the satisfaction and wellbeing of healthcare professionals. Some of these team-based strategies are a current practice in palliative care and may therefore be translated into intensive care, helping to overcome some burnout-associated factors (e.g., conflicts and ethical decisions at the end of life). In sum, findings suggest the need for implementing quality improvement and organizational redesign strategies aimed at integrating the philosophy, principles and practices of palliative care in intensive care units.
Acknowledgments
The authors would like to thank all the intensive care and palliative care professionals and teams that participated in this study. Members of Project InPalIn: Sandra Martins Pereira (PI), Ana Sofia Carvalho, Carla Teixeira, and Pablo Hernández-Marrero.
Abbreviations
- CI
Confidence Intervals
- DEP
Depersonalization
- EE
Emotional Exhaustion
- IC
Intensive Care
- ICUs
Intensive Care Units
- MBI-HSS
Maslach Burnout Inventory—Human Services Survey
- OR
Odds Ratio
- PC
Palliative Care
- PCUs
Palliative Care Units
- PPA
Personal and Professional Accomplishment
Data Availability
Data is available upon request from the authors. Due to privacy and data protection regulations in Portugal and considering that data refers to personal information of the participant teams and professionals, data cannot be made fully available. All relevant data and information are within the paper and its Supporting Information files. This does not alter the authors' adherence to PLOS ONE policies on data and materials.
Funding Statement
This study was partially supported by Fundação Grünenthal and Fundação Merck, Sharp and Dohme (2007/2011), which provided financial support during the period of data collection.
References
- 1.Pereira SM. Burnout in palliative care: A systematic review. Nurs Ethics. 2011; 18(3):317–326. 10.1177/0969733011398092 [DOI] [PubMed] [Google Scholar]
- 2.Maslach C. What we have learned about burnout and health. Psychol Health. 2001; 16:607–611. 10.1080/08870440108405530 [DOI] [PubMed] [Google Scholar]
- 3.Maslach C, Leiter M. The truth about burnout How organizations cause personal stress and what to do about it. San Francisco, CA: Jossey-Bass; 1997. [Google Scholar]
- 4.Teixeira CM, Ribeiro O, Fonseca AM, Carvalho AS. Burnout in intensive care units—a consideration of the possible prevalence and frequency of new risk factors: a descriptive correlational multicentre study. BMC Anesthesiology. 2013; 13:38 10.1186/1471-2253-13-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hernández-Marrero P, Martins Pereira S, Carvalho AS, on behalf of DELiCaSP. Ethical Decisions in Palliative Care: Interprofessional Relations as a Burnout Protective Factor? Results From a Mixed Methods Multicenter Study in Portugal. Am J Hosp & Palliat Med. 2016; 33(8) 723–732. 10.1177/1049909115583486 [DOI] [PubMed] [Google Scholar]
- 6.Hernández-Marrero P. Determinants of self-perceived managerial effectiveness in the Canarian Health Service. Doctoral dissertation, University of Toronto. 2006. Available: http://www.worldcat.org/title/determinants-of-self-perceived-managerial-effectiveness-in-the-canarian-health-service/oclc/225614031 ISBN: 9780494160121
- 7.Ledger U, Begley A, Reid J, Prior L, McAuley D, Blackwood B. Moral distress in end-of-life care in the intensive care unit. J Adv Nurs. 2013; 69(8):1869–1880. 10.1111/jan.12053 [DOI] [PubMed] [Google Scholar]
- 8.Poncet MC, Toullic P, Papazian L, Kentish-Barnes N, Timsit JF, Pochard F, et al. Burnout syndrome in critical care nursing staff. Am J Respir Crit Care Med. 2007; 175:698–704. 10.1164/rccm.200606-806OC [DOI] [PubMed] [Google Scholar]
- 9.Moss M, Good VS, Gozal D, Kleinpell R, Sessler CN. A Critical Care Societies Collaborative Statement: Burnout Syndrome in Critical Care health-care Professionals. Am J Resp Crit Care Med. 2016; 194(1):106–113. 10.1164/rccm.201604-0708ST [DOI] [PubMed] [Google Scholar]
- 10.Bakker AB, Le Blanc PM, Schaufeli WB. Burnout contagion among intensive care nurses. J Adv Nurs. 2005; 51(3):276–287. 10.1111/j.1365-2648.2005.03494.x [DOI] [PubMed] [Google Scholar]
- 11.Verdon M, Merlani P, Perneger T, Ricou B. Burnout in a surgical ICU team. Intensive Care Med. 2008; 34:152–156. 10.1007/s00134-007-0907-5 [DOI] [PubMed] [Google Scholar]
- 12.Embriaco N, Azoulay E, Barrau K, Kentish N, Pochard F, Loundou A, Papazian L. High level of burnout in intensivists. Am J Respir Crit Care Med. 2007; 75:686–692. 10.1164/rccm.200608-1184OC [DOI] [PubMed] [Google Scholar]
- 13.Moss M, Good VS, Gozal D, Kleinpell R, Sessler CN. An Official Critical Care Societies Collaborative Statement–Burnout Syndrome in Critical Care Health-care Professionals. A Call for Action. Chest. 2016; 150(1):17–26. 10.1016/j.chest.2016.02.649 [DOI] [PubMed] [Google Scholar]
- 14.Embriaco N, Papazian L, Kentish-Barnes N, Pochard F, Azoulay E. Burnout syndrome among critical care healthcare workers. Curr Opin Crit Care. 2007; 13:482–488. [DOI] [PubMed] [Google Scholar]
- 15.Moss M, Good VS, Gozal D, Kleinpell R, Sessler CN. An Official Critical Care Societies Collaborative Statement: Burnout Syndrome in Critical Care Health Professionals: A Call for Action. Am J Crit Care. 2016; 25(4):368–376. 10.4037/ajcc2016133 [DOI] [PubMed] [Google Scholar]
- 16.van Mol MMC, Kompanje EJO, Benoit DD, Bakker J, Nijkamp MD. The Prevalence of Compassion Fatigue and Burnout among Healthcare Professionals in Intensive Care Units: A Systematic Review. PLoS ONE. 2015; 10(8): e0136955 10.1371/journal.pone.0136955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Teixeira CM, Ribeiro O, Fonseca AM, Carvalho AS. Ethical decision making in intensive care units: a burnout risk factor? Results from a multicentre study conducted with physicians and nurses. J Med Ethics. 2014; 40(2):97–103. 10.1136/medethics-2012-100619 [DOI] [PubMed] [Google Scholar]
- 18.Martins Pereira S. Burnout em cuidados paliativos. Uma perspectiva bioética. Doctoral dissertation, Universidade Católica Portuguesa. 2011. Available: http://repositorio.ucp.pt/handle/10400.14/8180
- 19.Hwang Koh MY, Chong PH, Hui Neo PS, Ong YJ, Yong WC, Ong WY, et al. Burnout, psychological morbidity and use of coping mechanisms among palliative care practitioners: A multi-centre cross-sectional study. Palliat Med. 2015; 29(7):633–642. 10.1177/0269216315575850 [DOI] [PubMed] [Google Scholar]
- 20.Li X, Guan L, Chang H, Zhang B. Core Self-Evaluation and Burnout among nurses: The Mediating Role of Coping Styles. PLoS ONE. 2014; 9(12):e115799 10.1371/journal.pone.0115799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maslach C, Jackson SE. MBI: Maslach Burnout Inventory; Manual Research Edition. Palo Alto, CA: Consulting Psychologists Press; 1986. [Google Scholar]
- 22.Maslach C, Jackson S, Leiter M. Maslach Burnout Inventory In: Zalaquett C, Wood R (eds) Evaluating Stress. A Book of Resources. London: The Scarecrow Press; 1997. pp. 191–218. [Google Scholar]
- 23.Maslach C, Schaufeli WB, Leiter MP. Job Burnout In: Fiske ST, Schacter DL, Zahn-Waxler C (eds.) Annual Review of Psychology. 2001; 52: 397–422. 10.1146/annurev.psych.52.1.397 [DOI] [PubMed] [Google Scholar]
- 24.Maslach C, Leiter MP, Schaufeli W. Measuring Burnout In: Cartwright S, Cooper CL, editors. The Oxford Handbook of Organizational Well-Being. London: Oxford University Press; 2008. pp.86–108. [Google Scholar]
- 25.Maslach C, Jackson SE, Leiter MP. MBI: Maslach Burnout Inventory Manual, 3rd ed Palo Alto, CA: Consulting Psychologists Press; 1996. [Google Scholar]
- 26.Vieira S. Burnout em Profissionais de Saúde. Um estudo exploratório. M.Sc. Thesis, Universidade Católica Portuguesa. 2007. Available: http://repositorio.ucp.pt/handle/10400.14/8577
- 27.Squires A, Finlayson C, Gerchow L, Cimiotti JP, Matthews A, Schwendimann R, Griffiths P, Bussef R, Heinen M, Brzostek T, Moreno-Casbas MT, Aiken LH, Sermeus W. Methodological considerations when translating “burnout”. Burnout research. 2014; 1(2): 59–68. 10.1016/j.burn.2014.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brenninkmeijer V, Van Yperen N. How to conduct research on burnout: advantages and disadvantages of a unidimensional approach to burnout. Occupational and Environmental Medicine. 2003; 60: 16–21(suppl.1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Roelofs J, Verbraak M, Keijsers GPJ, de Bruin MBN, Schmidt AJM. Psychometric properties of a Dutch version of the Maslach Burnout Inventory General Survey (MBI-DV) in individuals with and without clinical burnout. Stress and Health. 2005; 21: 17–25. 10.1002/smi.1032 [DOI] [Google Scholar]
- 30.Söderfeldt M, Söderfeldt B, Warg LE, Ohlson CG. The factor structure of the Maslach Burnout Inventory in two Swedish human service organizations. Scand J Psychol. 1996; 37(4): 437–43. [DOI] [PubMed] [Google Scholar]
- 31.Embriaco N, Hraiech S, Azoulay E, Baumstarck-Barrau K, Forel J-M, Kentish-Barnes N, et al. Symptoms of depression in ICU physicians. Ann Intensive Care. 2012; 2:34 10.1186/2110-5820-2-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fahrenkopf AM, Sectish TC, Barger LK, Sharek PJ, Lewin D, Chiang VW, et al. Rates of medication errors among depressed and burnt out residents: Prospective cohort study. BMJ. 2008; 336(7642):488–491. 10.1136/bmj.39469.763218.BE . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bianchi R, Schonfeld IS, Laurent E. Is burnout a depressive disorder? A reexamination with special focus on atypical depression. International Journal of Stress Management. 2014; 21(4):307. [Google Scholar]
- 34.Ahola K, Honkonen T, Isometsä E, Kalimo R, Nykyri E, Aromaa A, et al. The relationship between jobrelated burnout and depressive disorders-results from the Finnish health 2000 study. J Affect Disord. 2005; 88(1):55–62. [DOI] [PubMed] [Google Scholar]
- 35.Wurm W, Vogel K, Holl A, Ebner C, Bayer D, Mörkl S, Szilagyi I-S, Hotter E, Kapfhammer H-P, Hofmann P. Depression-Burnout Overlap in Physicians. PLoS One. 2016; 11(3):e0149913 10.1371/journal.pone.0149913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shanafelt T, Balch CM, Bechamps G, Russell T, Dyrbye L, Satele D, et al. Burnout and medical errors among American surgeons. Ann Surgery. 2010; 251(6):995–1000. [DOI] [PubMed] [Google Scholar]
- 37.Romani M, Ashkar K. Burnout among physicians. Libyan J Med. 2014; 9:23556 10.3402/ljm.v9.23556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chen K, Yang CM, Lien CH, Chiu H-Y, Lin MR, Chang H-R, et al. Burnout, job satisfaction, and medical malpractice among physicians. International Journal of Medical Sciences. 2013; 10(11):1471–1478. 10.7150/ijms.6743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Prins J, van der Heijden F, Hoekstra-Weebers J, Bakker A, van de Wiel H, Jacobs B, Gazendam-Donofrio S. Burnout, engagement and resident physicians' self-reported errors. Psych, Health & Med. 2009; 14(6):654–66. 10.1080/13548500903311554 [DOI] [PubMed] [Google Scholar]
- 40.West CP, Huschka MM, Novotny PJ, Sloan JA, Kolars JC, Habermann TM, et al. Association of perceived medical errors with resident distress and empathy: A prospective longitudinal study. Journal of the American Medical Association. 2006; 296(9):1071–8. 10.1001/jama.296.9.1071 [DOI] [PubMed] [Google Scholar]
- 41.Garrouste-Orgeas M, Philippart F, Bruel C, Max A, Lau N, Misset B. Overview of medical errors and adverse events. Ann Intensive Care 2012; 2:2 published online as 10.1186/2110-5820-2-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hayashino Y, Utsugi-Ozaki M, Feldman MD, Fukuhara S. Hope Modified the Association between Distress and Incidence of Self-Perceived Medical Errors among Practicing Physicians: Prospective Cohort Study. PLoS ONE. 2012; 7(4): e35585 10.1371/journal.pone.0035585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hall LH, Johnson J, Watt I, Tsipa A, O’Connor DB. Healthcare Staff Wellbeing, Burnout, and Patient Safety: A Systematic Review. PLoS One. 2016; 11(7):e0159015 10.1371/journal.pone.0159015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Garrouste-Orgeas M, Perring M, Soufir L, Vesin A, Blot F, Maxime V, et al. The Iatroref study: medical errors are associated with symptoms of depression in ICU staff but not burnout or safety culture. Intensive Care Med. 2015; 41:273–284. 10.1007/s00134-014-3601-4 [DOI] [PubMed] [Google Scholar]
- 45.Poghosyan L, Clarke SP, Finlayson M, Aiken LH. Nurse burnout and quality of care: cross-national investigation in six countries. Res Nurs Health. 2010; 33(4):288–298. 10.1002/nur.20383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002; 136:358–367. [DOI] [PubMed] [Google Scholar]
- 47.Reader TW, Cuthbertson BH, Decruyenaere J. Burnout in the ICU: Potential consequences for staff and patient well-being. Intensive Care Med. 2008; 34:4–6. 10.1007/s00134-007-0908-4 [DOI] [PubMed] [Google Scholar]
- 48.Hinson TD, Spatz DL. Improving nurse retention in a care hospital. J Nurs Adm. 2011; 41(Suppl 3):103–108. [DOI] [PubMed] [Google Scholar]
- 49.Jones CB. Revisiting nurse turnover costs: adjusting for inflation. J Nurs Adm. 2008; 38(1):11–18. [DOI] [PubMed] [Google Scholar]
- 50.Waldman JD, Kelly F, Arora S, Smith HL. The shocking cost of turnover in health care. Health Care Manage Rev. 2004; 29(1):2–7. [DOI] [PubMed] [Google Scholar]
- 51.Dewa CS, Jacobs P, Thanh NX, Loong D. An estimate of the cost of burnout on early retirement and reduction in clinical hours of practicing physicians in Canada. BMC Health Serv Res. 2014; 14:254 10.1186/1472-6963-14-254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Linzer M, Levine R, Meltzer D, Poplau S, Warde C, West CP. 10 bold steps to prevent burnout in general internal medicine. J Gen Intern Med. 2014; 29(1):18–20. 10.1007/s11606-013-2597-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lepnurm R, Lockhart WS, Keegan D. A measure of daily distress in practicing medicine. Can J Psychiatry. 2009; 54:170–180. [DOI] [PubMed] [Google Scholar]
- 54.Dunwoodie D, Auret K. Psychological morbidity and burnout in palliative care doctors in Western Australia. Intern Med J 2008; 37:693–428. 10.1111/j.1445-5994.2007.01384.x [DOI] [PubMed] [Google Scholar]
- 55.Jackson V, Mack J, Matsuyama R, Lakoma MD, Sullivan AM, Arnold RM, et al. A qualitative study of oncologists’ approaches to end-of-life care. J Palliat Med. 2008; 11:893–903. 10.1089/jpm.2007.2480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Olthius G and Dekkers W. Quality of life considered as well-being: views from philosophy and palliative care practice. Theor Med Bioethics. 2005; 26:307–337. 10.1007/s11017-005-4487-5 [DOI] [PubMed] [Google Scholar]
- 57.Pereira SM, Fonseca AM, Carvalho AS. Burnout in nurses working in palliative care teams: a mixed methods study. Int J Palliat Nurs. 2012; 18(8):373–381. 10.12968/ijpn.2012.18.8.373 [DOI] [PubMed] [Google Scholar]
- 58.Block SD. Psychological Considerations, Growth, and Transcendence at the End of Life: The Art of the Possible. JAMA.2001; 285(22):2898–2905. 10.1001/jama.285.22.2898 [DOI] [PubMed] [Google Scholar]
- 59.Martins Pereira S, Hernández-Marrero P. “In Memory of Those Who Left”: How “Thank You” Letters Are Perceived and Used as a Team Empowerment Motivational Factor by a Home-Based Palliative Care Team in the Azorean Islands. Journal of Palliative Medicine. Prepublished June, 21, 2016 10.1089/jpm.2016.0255 [DOI] [PubMed] [Google Scholar]
- 60.Müller M, Pfister D, Markett S, Jaspers B. Wie viel Tod verträgt das Team? Eine bundesweite Befragung der Palliativstationen in Deutschland. Z Palliativ. 2010; 11(5):227–33. 10.1055/s-0030-1248520 [DOI] [PubMed] [Google Scholar]
- 61.Swetz KM, Harrington SE, Matsuyama RK, Shanafelt TD, Lyckholm LJ. Strategies for avoiding burnout in hospice and palliative medicine: peer advice for physicians on achieving longevity and fulfillment. J Palliat Med 2009; 12(9):773–7. 10.1089/jpm.2009.0050 [DOI] [PubMed] [Google Scholar]
- 62.Kearney MK, Weininger RB, Vachon ML, Harrison RL, Mount BM. Self-care of physicians caring for patients at the end of life: "Being connected…a key to my survival". JAMA. 2009; 301(11):1155–64. 10.1001/jama.2009.352 [DOI] [PubMed] [Google Scholar]
- 63.Perez GK, Haime V, Jackson V, Chittenden E, Mehta DH, Park ER. Promoting resiliency among palliative care clinicians: stressors, coping strategies, and training needs. J Palliat Med. 2015; 18(4):332–7. 10.1089/jpm.2014.0221 [DOI] [PubMed] [Google Scholar]
- 64.Maslach C, Leiter MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry. 2016; 15(2):103–11. 10.1002/wps.20311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lederer W, Kinzl JF, Traweger C, Dosch J, Suman G. Fully developed burnout and burnout risk in intensive care personnel at a university hospital. Anaesth Intensive Care. 2008; 36:208 213. [DOI] [PubMed] [Google Scholar]
- 66.Azoulay E, Timsit JF, Sprung CL, Soares M, Rusinová K, Lafabrie A, et al. Prevalence and factors of intensive care unit conflicts: the conflicus study. Am J Respir Crit Care Med. 2009; 180:853–860. 10.1164/rccm.200810-1614OC [DOI] [PubMed] [Google Scholar]
- 67.Chlan LL. Burnout syndrome among critical care professionals: a cause for alarm. Critical Care Alert. 2013; 21:65–68. [Google Scholar]
- 68.Ali NA, Hammersley J, Hoffmann SP, O'Brien JM Jr, Phillips GS, Rashkin M, Warren E, Garland A, Midwest Critical Care Consortium. Continuity of care in intensive care units: a cluster-randomized trial of intensivist staffing. Am J Respir Crit Care Med. 2011; 184(7):803–808. 10.1164/rccm.201103-0555OC [DOI] [PubMed] [Google Scholar]
- 69.Howell MD. Intensivist time allocation: economic and ethical issues surrounding how intensivists use their time. Semin Respir Crit Care Med. 2012; 33(4):401–412. 10.1055/s-0032-1322410 [DOI] [PubMed] [Google Scholar]
- 70.Danjoux Meth N, Lawless B, Hawryluck L. Conflicts in the ICU: perspectives of administrators and clinicians. Intensive Care Med. 2009; 35(12):2068–2077. 10.1007/s00134-009-1639-5 [DOI] [PubMed] [Google Scholar]
- 71.Fassier F, Azoulay E. Conflicts and communication gaps in the intensive care unit. Curr Opin Crit Care. 2010; 16(6):654–665. 10.1097/MCC.0b013e32834044f0 [DOI] [PubMed] [Google Scholar]
- 72.Savel RH, Munro CL. Conflict Management in the Intensive Care Unit. Am J Crit Care; 2013; 22(4):277–280. 10.4037/ajcc2013857 [DOI] [PubMed] [Google Scholar]
- 73.Morgan L, Howe L, Whitcomb J, Smith K. Improving Communication and Cost-effectiveness in the Intensive Care Unit Through Palliative Care. A Review of Literature. Dimens Crit Care Nurs. 2011; 30(3):133–138. 10.1097/DCC.0b013e31820d2114 [DOI] [PubMed] [Google Scholar]
- 74.Quenot J-P, Rigaud J-P, Prin S, Barbar S, Pavon A, Hamet M, et al. Suffering among careers working in critical care can be reduced by an intensive communication strategy on end-of-life practices. Intensive Care Med. 2012; 38:55–61. 10.1007/s00134-011-2413-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hartog CS, Benbenishty J. Understanding nurse-physician conflicts in the ICU. Intensive Care Med. 2015; 41:331–333. 10.1007/s00134-014-3517-z [DOI] [PubMed] [Google Scholar]
- 76.Trankle SA. Is a good death possible in Australian critical and acute settings?: physician experiences with end-of-life care. BMC Palliat Care. 2014; 13:41 10.1186/1472-684X-13-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.O’Mahony S, Gerhart JI, Grosse J, Abrams I, Levy MM. Posttraumatic stress symptoms in palliative care professionals seeking mindfulness training: Prevalence and vulnerability. Palliat Med. 2015; 30(2):189–92. 10.1177/0269216315596459 [DOI] [PubMed] [Google Scholar]
- 78.Back AL, Steinhauser KE, Kamal AH, Jackson VA. Building Resilience for Palliative Care Clinicians: An Approach to Burnout Prevention Based on Individual Skills and Workplace Factors. J Pain Symptom Manage. Prepublished February, 26, 2016 10.1016/j.jpainsymman.2016.02.002 [DOI] [PubMed] [Google Scholar]
- 79.Dreáno-Hartz S, Rhondali W W, Ledou M, et al. Burnout among physicians in palliative care: impact of clinical settings. Palliat Support Care. 2016; 14(4):402–10. 10.1017/S1478951515000991 [DOI] [PubMed] [Google Scholar]
- 80.Sansó N, Galiana L, Oliver A, Pascual A, Sinclair S, Benito E. Palliative Care Professionals’ Inner Life: Exploring the Relationships Among Awareness, Self-Care, and Compassion Satisfaction and Fatigue, Burnout and Coping with Death. J Pain Symptom Manage. 2015; 50(2):200–207. 10.1016/j.jpainsymman.2015.02.013 [DOI] [PubMed] [Google Scholar]
- 81.Reilly J, Ring J. An end-of-life curriculum: empowering the resident, patient, and family. J Palliat Med. 2004; 7(1):55–63. 10.1089/109662104322737250 [DOI] [PubMed] [Google Scholar]
- 82.Kamel G, Paniagua M, Uppalapati A. Palliative Care in the Intensive Care Unit: Are Residents Well Trained to Provide Optimal Care to Critically Ill Patients? Am J Hosp & Palliat Med. 2015; 32(7):758–762. 10.1177/1049909114536979 [DOI] [PubMed] [Google Scholar]
- 83.Hill RC, Dempster M, Donelly M, McCorry NK. Improving the wellbeing of staff who work in palliative care settings: A systematic review of psychosocial interventions. Palliat Med. Prepublished March, 4, 2016. 10.1177/0269216316637237 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is available upon request from the authors. Due to privacy and data protection regulations in Portugal and considering that data refers to personal information of the participant teams and professionals, data cannot be made fully available. All relevant data and information are within the paper and its Supporting Information files. This does not alter the authors' adherence to PLOS ONE policies on data and materials.