Abstract
Background
Evaluation of the state of health, quality of life, and the relationship between the level of the quality of life and health status in a group of women at an advanced age (90 years of age and older) in Poland.
Material/Methods
The study was conducted in 2014 in an all-Polish sample of 870 women aged 90 years and older. The research instruments were: the authors’ questionnaire and several standardized tests: Katz Index of Independence in Activities of Daily Living (Katz ADL), Abbreviated Mental Test Score (AMTS), and the World Health Organization Quality of Life (WHOQOL)-BREF. The results of the study were statistically analyzed using significant t-test for mean and regression analysis.
Results
The majority of women at an advanced age suffered from chronic pain (76%) and major geriatric problems such as hypoacusis (81%), visual disturbances (69%) and urinary incontinence (60%); the minority of women at an advanced age suffered from falls and fainting (39%), stool incontinence (17%), severe functional impairment (24%), and cognitive impairment (10%).
On a scale of 1 to 5, women at an advanced age assessed positively for overall quality of life (mean 3.3), social relationships (3.5), and environment (3.2), but negatively for general health, physical health, and psychological health (2.7, 2.7, and 2.8, respectively).
The presence of chronic pain and geriatric problems, including urinary and stool incontinences, falls and faint ing, visual disturbances and hypoacusis, significantly decreased overall quality of life; general health, physical health, psychological health, social relationships, and environment.
Overall quality of life, general health, physical health, psychological health, social relationships, and environment was correlated with functional and cognitive impairments.
Conclusions
Quality of life of women at an advanced age decreased if chronic pain, major geriatric problems, or functional or cognitive impairments occurred.
MeSH Keywords: Quality of Life, Statistics as Topic, Women’s Health
Background
In the last half of the century in Poland, the number of persons aged 60 years and older has increased about three fold, while the number of “old” persons age 85 years and older has increased over four fold. This phenomenon has been called “double” aging, i.e., an increase in the number of people in a population older than 80 years, and an increasing population of old people [1,2].
One of the key problems often discussed is the average life span of women [3]. The average life expectancy at birth for persons born during the period 2008–2010 in 27 countries of the European Union is: 75.3 years for males and 81.7 years for females [4]. In 2006 in Poland, the number of people aged a hundred (100+) was 1,963, and the ratio of females to males was 3. The mean value of an increase in the number of people aged a hundred and over (100+) in 27 countries of the European Union was 2.0, and the mean ratio of females to males in this group was 6.0 [5].
The aging of society necessitates not only reflection, but also actual solutions aimed at improvement in the quality of aging. In the general model of health, the World Health Organization (WHO) focuses attention on the differences which may occur between life span and the period lived without chronic diseases and limited efficacy. Considering these WHO guidelines, the European Union included as part of the pool of health indicators, the indicators for life expectance in health. One indicator is the HLY (Healthy Life Years), i.e., the expected life span without long-term limitation of activities of daily life (ADL). In 2009, the life expectancy (LE) in Poland for people aged 65 years was 19.2 years for females (including HLY 7.4 years, i.e., 39% of lifetime), and 14.8 years for males (including HLY 6.8 years, i.e., 46% of lifetime). The indicators for all countries of the EU were: male LE of 76.7 years (HLY 80%); females LE of 82.6 years (HLY 75%). These indicators confirm that the position of Poland is unfavorable compared to the leading EU countries. An older person, especially an older woman in Poland, has lower chances for successful aging [6,7].
In older women worldwide, a greater decrease has been observed in the areas of physical, mental, and social health, compared to men [8,9]. Therefore, it is necessary to investigate the state of health of older women as a group. Studies have shown that a poor state of health in older people exerts an effect on their functional efficacy, fulfillment of social roles, possibilities of further development, and their perception of their own old age [10–12]. In turn, good health decreases the risk of physical and social disability [13], increases the tendency towards further development [8], and slows down physical changes [14,15]. Good health is also related to a higher level of the quality of life [9].
Quality of life is a multidimensional and interdisciplinary phenomenon. According to the definition of the World Health Organization (WHO), quality of life is a subjective category and depends on how an individual perceives their own position in life [16,19]. The degree of the effect of health on quality of life of older people increases with age [20,21]. Many studies have shown a decrease in quality of life together with the deterioration of health and increase in poor general physical well-being [8,14,22,23].
The objective of this study was to evaluation the state of health, quality of life, and the relationship between quality of life and state of health in a group of Polish women who are at an advanced age of 90 years and older. The state of health was defined by functional and cognitive impairments, occurrence of major geriatric problems, and the presence of chronic pain.
Material and Methods
This study was conducted in 2014 with organizational support from the Social Welfare Centers in east, central, and west Poland. It included a group of 870 women aged 90 years or older. A systematic sampling of 250 community social welfare centers (out of 2,500 available centers) were selected (every tenth center from the Central Statistical Office list) to take part in the study. One hundred and fifty-three centers agreed to participate. We sent 10 questionnaires along with information about inclusion and exclusion criteria to each participating center. We received back 870 completed questionnaires, i.e., 56% response rate.
The criteria for inclusion in the study was: women who were age 90 years and older, and who could maintain verbal-logical contact.
The criteria for exclusion was: addiction to psychotropic drugs or alcohol, dementia, or impaired verbal-logical contact making the survey impossible.
The surveys were conducted in the presence of an employee of the local Social Welfare Center and used the study questionnaire designed by the authors and international standardized tests: ADL, AMTS, and WHOQOL-BREF.
-
Self-designed questionnaire titled “Conditions of life of women at advanced age – 90 and over” collected demographic data, and data on occurrence of chronic pain and common, major geriatric problems.
In older people, there is a higher risk of chronic pain of various origins, which is the factor seriously limiting efficacy and decreasing quality of life [24]. In our study, the patients replied Yes or No to the question: “Do you experience so-called chronic pain/Are you constantly in pain?”
The conditions identified as major geriatric problems were defined as multi-cause and chronic syndromes of senile disability. Their presence is considered to lead to the loss of autonomy and control over life, and constitutes a great psychological, organizational, and economic burden for family caregivers and the welfare system [25]. The presence of these problems can result in a decrease in the quality of life of seniors by limiting their life activities, mobility, and contact with others and the environment [26]. Major geriatric problems most often identified include: urinary incontinence, stool incontinence, falls and fainting, visual disturbances, and hypoacusis.
Katz Index of Independence in Activities of Daily Living (Katz ADL) indicates functional impairment in performance of basic daily living activities. This index assesses six functions: bathing, dressing, toileting, transferring, continence, and feeding [27]. The respondent has a choice of two answers: Yes or No. For each reply confirming independence, the respondent obtains a score of one. A total score of five or six indicates full function, three or four indicates moderate functional impairment, a score of zero to two indicates severe functional impairment [28].
The Polish version of Abbreviated Mental Test Score (AMTS) was used. The test consists of 11 items aimed at evaluating the cognitive status of older patients with respect to: recent memory (reference memory) and distant memory, attention concentration, and ability to count. The participant responses are evaluated as follows: one for a correct answer, zero for an incorrect answer. Scores of nine to eleven indicate a normal mental state; scores of seven or eight indicate a mild cognitive impairment, scores from four to six indicate a moderate cognitive impairment, and scores from zero to three indicate a severe cognitive impairment.
The World Health Organization Quality of Life (WHOQOL) is recommended by the WHO as a universal research instrument for the evaluation of the quality of life. Its abbreviated version, i.e., the WHOQOL-BREF scoring is designed mainly for clinical purposes. It contains 26 questions for the analysis of four domains: physical health (seven questions), psychological health (six questions), social relationships (three questions), environment (eight questions), and separately, the overall quality of life (one question) and general health (one question) [19,29]. The answers are evaluated using a 5-degree scale (the range of scoring 1–5). The scoring for the domains is established by the calculation of the arithmetic mean from the items within individual domains. The results have a positive direction (the higher the number of scores, the higher the quality of life) [30–32]. The efficient reliability of four complex domains was determined (Cronbach’s α was 0.867 for physical health, 0.833 for psychological health, 0.738 for social relationships and 0.773 for environment). In addition, based on the numerical results, categories were created evaluating the quality of life, adopting the following range of intervals: very poor (1.0–1.8); poor (1.9–2.6); neither good nor poor (2.7–3.4); good (3.5–4.2); very good (4.2–5.0).
Methods of statistical analysis
Statistical analysis was performed using a statistical software package STATISTICA, with the level of significance of p<0.05. In the tables, absolute numbers are presented (n) and relative numbers (ratio between the number of units of a given characteristic to the number of the sample expressed in%) for qualitative variables, while for quantitative variables the following was used: arithmetic mean values (M) reflecting the average level, and standard deviation (SD) measuring the degree of dispersion of measurements around the arithmetic mean. Significant t-test was used to determine whether empirical mean was equal to midpoint of the scale (3 in WHOQOL domains).
Univariate regression models for quality of life dependent on characteristics of health status were estimated. Dependent variables were overall quality of life, general health, physical health, psychological health, social relationships, and environment from the WHOQOL-BREF, whereas independent variables were the presence of chronic pain and five major geriatric problems: urinary incontinence, stool incontinence, falls and fainting, visual disturbances, and hypoacusis (No versus Yes responses), number of daily living activities performed independently (IADL) and number of correct answers (AMTS). All independent variables were significantly correlated to each other, so multivariate regression models was not used. Estimates of slope terms in regression analyses, describing estimated mean changes in quality of life dependent on health status characteristics were included.
Results
The 870 women surveyed were age 90 years to 106 years, 94.3±2.9 years on average.
Health state of the women examined
About three-fourths of the surveyed women suffered from chronic pain. Among the major geriatric problems, hypoacusis was the most common (80.46%), followed by visual disturbances (68.74%), and urinary incontinence (60.34%); less common were falls and fainting (39.08%); the least common was stool incontinence (16.90%) (Figure 1).
Figure 1.
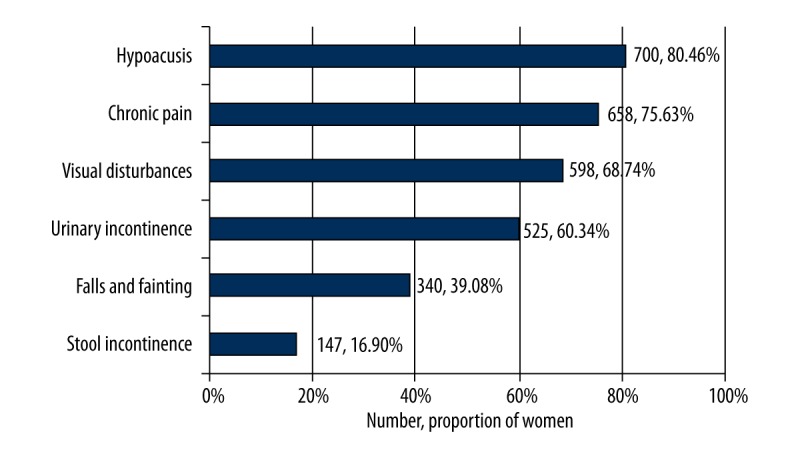
Occurrence of chronic pain and giant geriatric problems in the examined women at advanced age.
Of the surveyed women, 8.96% did not declare any major geriatric problem, 14.93% reported one major geriatric problems, 31% reported two, 27.44% reported three, 11.34% reported four, and 4.25% reported five major geriatric problems.
Based on the Katz ADL (Table 1), 23.56% of the women were severely functionally impaired (6.9% reported they did not independently perform any basic daily living activities, 7.7% reported they independently performed only one such activity, and about 9% reported they performed only two such activities). Of the surveyed women, 22.87% were moderately functionally impaired (10% of the women independently performed three basic daily living activities and 12.87% of the women performed four such activities). While 53.33% of the surveyed women were considered full functioning (22.41% independently performed five basic daily living activities and 30.92% independently performed six basic daily living activities). On average, women at an advanced age independently performed 4.1±1.9 basic daily living activities, which indicated a moderate functional impairment.
Table 1.
Katz index of independence in Activities of Daily Living (ADL) in the examined women at advanced age.
| Functional impairment | n | % | Number of daily living activities performed independently | n | % |
|---|---|---|---|---|---|
| Severe functional impairment | 205 | 23.56 | 0 | 60 | 6.90 |
| 1 | 67 | 7.70 | |||
| 2 | 78 | 8.97 | |||
| Moderate functional impairment | 199 | 22.87 | 3 | 87 | 10.00 |
| 4 | 112 | 12.87 | |||
| Full function | 464 | 53.33 | 5 | 195 | 22.41 |
| 6 | 269 | 30.92 |
M=4.1; SD=1.9 daily living activities performed independently.
Abbreviated Mental Test Score (AMTS) (Table 2) showed severe cognitive impairment in almost 10% of the surveyed women (3.45% of the women answered three questions correctly, 2.07% answered two questions correctly, 1.84% answered one question correctly, and 2.3% did not answer any question correctly). Moderate cognitive impairment was found in 22.07% of the surveyed women (5.06% answered four questions correctly, 8.28% answered five questions correctly, and 8.74% answered six questions correctly.). Mild cognitive impairment was found in 30.54% of the surveyed women (12.87% of the women answered seven questions correctly and 17.47% answered eight questions correctly.). Normal state of cognitive function occurred in approximately one-third of the surveyed women (13.22% answered nine questions correctly, 11.61% answered 10 questions correctly, and 13% answered all questions correctly). The AMT mean score was 7.4±2.7 correct answers out of 11 questions asked, and showed a mild cognitive impairment on average.
Table 2.
Abbreviated Mental Test Score (AMTS) in the examined women at advanced age.
| Cognitive impairment | n | % | Number of correct answers | n | % |
|---|---|---|---|---|---|
| Severe | 84 | 9.66 | 0 | 20 | 2.30 |
| 1 | 16 | 1.84 | |||
| 2 | 18 | 2.07 | |||
| 3 | 30 | 3.45 | |||
| Moderate | 192 | 22.07 | 4 | 44 | 5.06 |
| 5 | 72 | 8.28 | |||
| 6 | 76 | 8.74 | |||
| Mild | 266 | 30.54 | 7 | 112 | 12.87 |
| 8 | 152 | 17.47 | |||
| Normal state | 329 | 37.82 | 9 | 115 | 13.22 |
| 10 | 101 | 11.61 | |||
| 11 | 113 | 12.99 |
M=7.4, SD=2.7 correct answers.
Significant positive correlation was found between Katz ADL and AMT scores (r=0.306, p<0.001). The surveyed women who had more severe functional impairment also had more severe cognitive impairment on average.
Quality of life of women at advanced age
On the basis of the WHOQOL-BREF (Table 3), the study found that the surveyed women had good overall quality of life (mean 3.3), social relationships (3.5), and environment (3.2), but poor general, physical, and psychological health (mean 2.7, 2.7, and 2.8, respectively). The largest number of good and very good evaluations were reported with respect to overall quality of life (45.3% and 4.5%, respectively), social relationships (59% and 8%, respectively), and slightly less in the environmental domain (31% and 4.4%, respectively), while general, physical, and psychological domains had about 20% each. In turn, the quality of life in these three domains (general, physical, and psychological health) was most frequently evaluated as poor or very poor. Overall quality of life was assessed as poor or very poor by respectively 3.44% and 12.29% of the surveyed women.
Table 3.
Quality of life of the examined women at advanced age.
| Domains | Very poor | Poor | Neither good nor poor | Good | Very good | M | SD | Significant differences* | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | t | p | |||
| Overall quality of life | 30 | 3.44 | 107 | 12.29 | 300 | 34.49 | 394 | 45.28 | 39 | 4.48 | 3.3 | 0.9 | 11.306 | <0.001 |
| General health | 94 | 10.80 | 318 | 36.55 | 236 | 27.14 | 207 | 23.79 | 17 | 1.95 | 2.7 | 1.0 | –8.461 | <0.001 |
| Physical health | 106 | 12.18 | 317 | 36.43 | 280 | 32.14 | 155 | 17.81 | 16 | 1.83 | 2.7 | 0.7 | –11.782 | <0.001 |
| Psychological health | 62 | 7.12 | 285 | 32.75 | 352 | 40.48 | 153 | 17.58 | 18 | 2.06 | 2.8 | 0.7 | –8.066 | <0.001 |
| Social relationships | 20 | 2.29 | 109 | 12.52 | 155 | 17.18 | 516 | 59.31 | 71 | 8.16 | 3.5 | 0.7 | 18.360 | <0.001 |
| Environment | 11 | 1.26 | 139 | 15.97 | 414 | 47.61 | 0,6 | 30.80 | 38 | 4.36 | 3.2 | 0.6 | 7.899 | <0.001 |
Test whether empirical mean – midpoint of scale (3).
Relationship between the quality of life and state of health
The results of regression analyses for quality of life dependent on the state of health characteristics showed that overall quality of life, general health, physical health, psychological health, social relationships, and environment were significantly correlated to occurrence of chronic pain and the major geriatric problems, as well as functional impairment and cognitive impairments (Table 4).
Table 4.
Estimates of slope terms in regression analyses of quality of life dependent on health state’s characteristics of the examined women at advanced age.
| Health state’ characteristics | IU | Overall quality of life | General health | Physical health | Psychological health | Social relationships | Environment | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | p | Estimate | p | Estimate | p | Estimate | p | Estimate | p | Estimate | p | ||
| Chronic pain | No vs. yes | 0.23 | <0.001 | 0.28 | <0.001 | 0.37 | <0.001 | 0.25 | <0.001 | 0.11 | 0.001 | 0.26 | <0.001 |
| Urinary incontinence | No vs. yes | 0.13 | <0.001 | 0.19 | <0.001 | 0.34 | <0.001 | 0.31 | <0.001 | 0.13 | <0.001 | 0.24 | <0.001 |
| Stool incontinence | No vs. yes | 0.06 | 0.142 | 0.08 | 0.036 | 0.26 | <0.001 | 0.20 | <0.001 | 0.05 | 0.205 | 0.15 | <0.001 |
| Falls and fainting | No vs. yes | 0.15 | <0.001 | 0.21 | <0.001 | 0.31 | <0.001 | 0.24 | <0.001 | 0.19 | <0.001 | 0.25 | <0.001 |
| Visual disturbances | No vs. yes | 0.09 | 0.015 | 0.10 | 0.010 | 0.19 | <0.001 | 0.20 | <0.001 | 0.03 | 0.500 | 0.15 | <0.001 |
| Hypoacusis | No vs. yes | 0.04 | 0.327 | 0.04 | 0.245 | 0.15 | <0.001 | 0.18 | <0.001 | 0.01 | 0.687 | 0.10 | 0.009 |
| ADL | 1 activity | 0.19 | <0.001 | 0.24 | <0.001 | 0.49 | <0.001 | 0.38 | <0.001 | 0.15 | <0.001 | 0.30 | <0.001 |
| AMTS | 1 correct answer | 0.07 | <0.001 | 0.07 | <0.001 | 0.07 | <0.001 | 0.09 | <0.001 | 0.03 | 0.010 | 0.05 | 0.010 |
The surveyed women without chronic pain had significantly better overall quality of life by 0.23, general health by 0.28, physical health by 0.37, psychological health by 0.25, social relationships by 0.11, and environment by 0.26 compared to the women who reported chronic pain.
Also the surveyed women without major geriatric problems had significantly better overall quality of life, general health, physical health, psychological health, social relationships, and environment compared to women who reported major geriatric problems (Figure 2).
Figure 2.
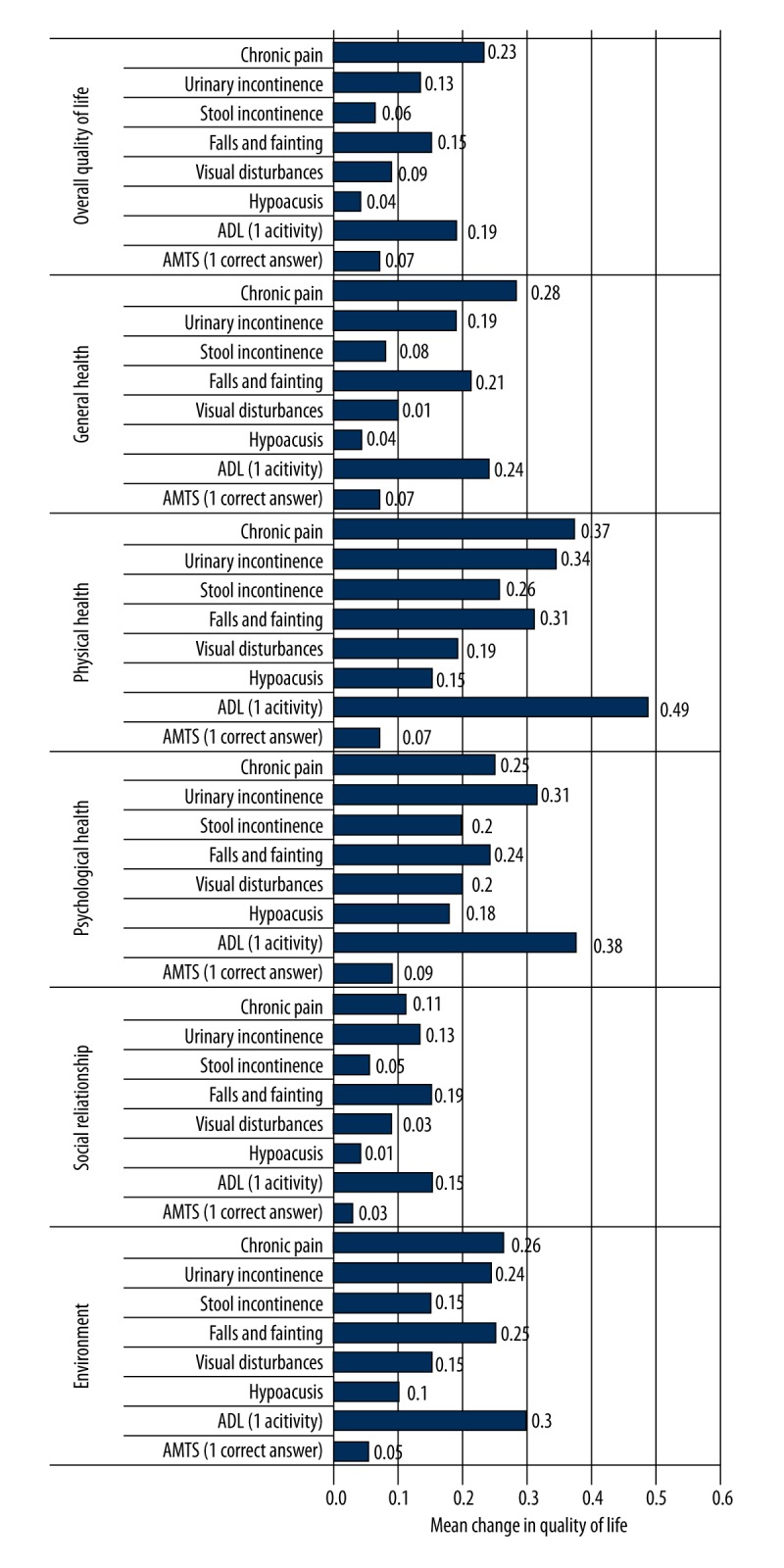
Estimated mean changes in quality of life dependent on health state’s characteristics of the examined women at advanced age.
If the number of independently performed basic daily living activities was higher by one activity, the overall quality of life increased by 0.19, general health by 0.24, physical health by 0.49, psychological health by 0.38, social relationships by 0.15 and environment by 0.30.
If the women correctly answered one more question, their overall quality of life increased by 0.07, general health by 0.07, physical health by 0.07, psychological health by 0.09, social relationships by 0.03 and environment by 0.05.
Discussion
For many years, many international organizations have recognized that an increasing percentage of the overall global population is elderly, especially elderly women. The European Commission, United Nations, and organizations functioning within the World Health Organization have drawn attention to the increasing number of seniors in all societies. As a result there is a need to undertake actions that encourage the activation of the elderly, and the protection of this group against health, psychological, and social consequences. A clear outcome of these undertakings should be an increase in life satisfaction and health, and a measurable increase in the quality of life, maintaining the major parameter which is life span [33–41].
The goal of this study was to analysis of the state of health, quality of life, and the relationship between quality of life and the state of health in a group of women at an advanced age (90–106 years old) in Poland.
Women’s state of health at advanced age
An important issue is not only the self-reported state of health of women at an advanced age, but it is also important to know to what extent this group maintains physical and mental efficacy, and what limits their state of health. It is known that with age general efficacy decreases, and an increase is observed in the number of people disabled and the number of people who need health-related care. In this study, it was confirmed that according to the Katz ADL, the majority of women aged 90 years and older (53%) had full function, and moderate impairment was reported by approximately 56% of respondents.
Data from the NHANES III study (National Health and Nutrition Examination Survey) showed that in the USA, 23% of persons aged 80 years and older were not able to independently prepare their meals, and 17% are not able to walk independently. The above-presented data clearly showed that in the population aged 80 years and older in the United States, 40% were disabled, which was a higher percentage than in the Polish population [42]. Similarly, in other population studies of the elderly in the United States, a group of nearly 32% women were was found, aged 70–79, who complained of limited mobility at walking one-fourth mile (402 meters), or climbing stairs (10 steps in the sample); these results were respectively correlated with the loss of muscle mass and atrophy of muscle fibers to the benefit of adipose tissue [43].
In the studies of the European population (Austria), the researchers reported a group of women aged 75–84 years, a 10–20% limitation of physical efficacy in the activities of daily life (ADL), according to the type of activity. Independence taking a bath or shower was especially a problem. The limitation also concerned the instrumental scale of activities of daily life (IADL), especially for respondents aged older than 75 years [3,44]. In addition it has been observed that the process of the loss of efficacy is greater among females than males [45].
In this study, we used the AMTS test, and found that the majority of women at advanced age did not show cognitive impairment (68%), while 32% showed a moderate or severe cognitive impairment. This result is consistent with that obtained in a study of older women in an Austrian population who completed the AMTS test, where individual groups obtained scores from 4.1–5.9 [46], and a Swedish population, where cognitive disorders occurred in 29% of the oldest women [47]. Similar results were obtained in a nine-year study conducted in the United Kingdom. The study confirmed a relatively high cognitive efficacy in older people aged 80.8 and older [48].
A separate issue to consider is symptoms belonging to the so-called major geriatric problems (urinary and stool incontinences, falls and fainting, visual disturbances and hypoacusis), the occurrence of which is more frequent among women, increases with age, and their occurrence quickly leads to the decline in efficacy, deterioration of the quality of life, and is the cause of increase in morbidity and mortality [49,50].
In this study, 9% of the surveyed women at advanced age did not declare any major geriatric problem, 15% suffered from one of the major geriatric problems, 31% for two, 27% for three, 11% from four, and 4% from five major geriatric problems. The largest number of respondents reported problems with hearing (80%), vision (68%), and urinary incontinence (60%). The smallest number of respondents complained of stool incontinence (17%). The frequency of urinary incontinence among American women aged 70–79 years was 21% [51]; in Scandinavian studies in women aged over 80 years it was 32% [52]. About 44–51% of women aged over 65 years have a problem of urinary incontinence [53].
Quality of life of women at advanced age
The reported satisfaction with general health in the surveyed women at advanced age was on low (2.7 WHOQOL-BREF). Nearly one half of the women evaluated their state of health and the physical aspect of functioning as very poor or poor. However, it is noteworthy that 25% of the women evaluated their health and the physical aspect of satisfaction with life as good or very good.
In Austrian studies looked at self-reported-health in women aged older than 75 years and found women evaluated their state of health as follows: 5.7% reported that it was very good, 29.8% that it was good; 44.5% considered their state of health as mediocre, 17.8% reported their health as poor, while 2.3% reported that it was very poor [44]. In comparing these groups of women, it is evident that in the Austrian study the percentage of those satisfied with their health was higher than that of those who perceived their state of health as poor. Nevertheless, it should be noted that our study focused on women aged 90 years and older, whereas the Austrian study focused on women aged 75 years and older. As confirmed by studies conducted in a population in Angola, the quality of life decreases with age [54].
Self-evaluation of health and health-related quality of life, when confronted with the developments in medicine and improvements in economic conditions and the resulting longevity of life, evokes a dilemma: which is more important, the quality of life or life span. The American Geriatrics Society acknowledges this problem in its motto “Adding life to years, not just more years to life” [55]. Thus, it seems that the quality of life and health are more important and necessary than the prolongation of life when it is devoid of its values.
In this study, it was discovered that satisfaction with life of a woman at advanced age is on a mediocre level. To a great degree women are dissatisfied with their health and physical sphere, whereas they are most satisfied with life and social relations. In the PolSenior study the subjective evaluation of the quality of life was on a high level, i.e., 59.6% of respondents mentioned that it was good or very good; however, in women at advanced age it was slightly lower at 54.4%, which still seems to be a high value. For the total number of respondents in the age group 80 years and older, this value was even increased (61.2%). Satisfaction with health of people at an advanced age in the PolSenior study was also relatively high; however, the percentage was lower than for satisfaction with life. For all respondents this percentage was 44.7% of males at an advanced age declaring better self-reported health than females. As many as 50% of males evaluated their health as good or very good, while females shared this evaluation of their health at 38.5%. Satisfaction with health in the group of respondents aged 80 years and older was 44.4%, on average [56].
Other researchers observed satisfaction with life on a mediocre level. The environmental, social, and psychological domains obtained the lowest evaluations [57].
Relationship between the quality of life and of health state of women at advanced age
Cross-sectional studies confirmed that in older people with health problems the level of the quality of life is considerably lower [20,21]. Those who were dissatisfied with their health also presented more negative attitudes towards their own aging from a physical aspect [58].
In our study, a significant effect was found for functional efficacy on the quality of life. Each domain of the quality of life increased with an increase in functional efficacy. In other studies, attention was paid to the fact that although in the age group 80–84 years to 100–105 years a dramatic decline in physical and mental efficacy was observed, the level of satisfaction with life was maintained [59].
In our study, a low result on the AMTS decreased the quality of life in the psychological sphere. In another study concerning people at advanced age who were intellectually active, participated in courses at the University of Third Age, no differences were observed with respect to evaluations of the state of health and the quality of life. Both values were on a similar high level [60].
In our study, it was observed that the problem of urinary incontinence exerts a negative effect on the quality of life (physical, psychological, environmental domains and social relations). In another study of the risk factors of urinary incontinence among women, a significant correlation was found with low education level, number of natural childbirths, and previous abortions, and the occurrence of this problem considerably decreases the quality of life [61]. The limitation of the negative effect of major geriatric problems, especially urinary and stool incontinence, on the quality of life may be achieved by an improvement in physical efficacy [62].
An important factor affecting the quality of life at an advanced age is the occurrence of chronic pain. In our study, 75% of the surveyed women complained of this problem. The occurrence of pain significantly correlated with quality of life. The quality in the domains: satisfaction with life and health, physical, psychological and environmental significantly decreases in persons who experience pain. According to Koziak and Sangl, women experience pain in a different way than men, and more often experience complaints of a chronic nature [63]. However, in a Norwegian study of a group of older people, a more negative effect of pain was noted in the group of males [64].
Our study, as well as many studies by other researchers, indicates that there is a relationship between the quality of life and state of health. However, it should not be forgotten that this relationship may be modified by intervening variables. Recently conducted studies pay attention to the effect of such variables as the sense of coherence and self-transcendence on the quality of life of people at advanced age [65–68].
Conclusions
The majority of women at an advanced age suffered from chronic pain and such major geriatric problems as hypoacusis, visual disturbances, and urinary incontinence; the minority of women suffered from falls and fainting, stool incontinence, and severe functional and cognitive impairment.
Women at an advanced age assessed positively for overall quality of life, social relationships and environment, but negatively for general, physical, and psychological health.
The presence of chronic pain and major geriatric problems such as urinary and stool incontinences, falls and fainting, visual disturbances and hypoacusis, significantly decreased overall quality of life, general health, physical health, psychological health, social relationships, and environment of women at an advanced age.
Overall quality of life, general health, physical health, psychological health, social relationships, and environment correlated with functional and cognitive impairments of women at an advanced age.
Footnotes
Source of support: This study was sponsored by Institute of Rural Health in Lublin, Poland
References
- 1.Szukalski P. [Mortality of the old-old and the oldest-old in Poland – 1931/1932–2005]. Gerontologia Polska. 2007;15(1–2):31–39. [in Polish] [Google Scholar]
- 2.The World Health Organization (WHO) Global brief for World Health Day 2012 [Internet] WHO; 2012. Good health adds life to years. Available from: URL: http://www.who.int/ageing/publications/upcoming_publications/en/index.html. [Google Scholar]
- 3.Vera I, Lucchese R, Nakatani AY, et al. Family functionality in oldest old household residents. Rev Bras Enferm. 2015;68(1):61–88. doi: 10.1590/0034-7167.2015680110p. [DOI] [PubMed] [Google Scholar]
- 4.Jagger C, Gillies C, Moscone F, et al. Inequalities in heal thy life years in the 25 countries of the European Union in 2005: A cross-national meta-regression analysis. Lancet. 2009;20(372):2124–31. doi: 10.1016/S0140-6736(08)61594-9. [DOI] [PubMed] [Google Scholar]
- 5.Robine JM, Saito Y. The number of centenarians in Europe. European Paper On The New Welfare. 2009;13:1–4. [Google Scholar]
- 6.EHEMU Raporty Krajowe. 2012. p. 5. [in Polish] [Google Scholar]
- 7.Hank K. How Successful Do Older European Age? Findings from SHARE. J Gerontol B Psychol Sci Soc Sci. 2011;66(2):230–36. doi: 10.1093/geronb/gbq089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Steverink N, Westerhof GJ, Bode C, Dittmann-Kohli F. The personal experience of aging, individual resources, and subjective well-being. J Gerontol Ser B Psychol Soc Sci. 2001;56B:364–73. doi: 10.1093/geronb/56.6.p364. [DOI] [PubMed] [Google Scholar]
- 9.Kalfoss M, Low G, Molzahn A. Suitability of the WHOQOL-BREF among older Canadians and Norwegians. Eur J Ageing. 2008;5:77–89. doi: 10.1007/s10433-008-0070-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Demakakos P, Gjonca E, Nazroo J. Age identity, age perceptions, and health: evidence from the English longitudinal study of aging. Ann New York Acad Sci. 2007;1114:279–87. doi: 10.1196/annals.1396.021. [DOI] [PubMed] [Google Scholar]
- 11.Schafer MH, Shippee TP. Age identity, gender, and perceptions of decline: Does feeling older lead to pessimistic dispositions about cognitive aging? J Geront Ser B Psychol Soc Sci. 2010;65:91–96. doi: 10.1093/geronb/gbp046. [DOI] [PubMed] [Google Scholar]
- 12.Walker CA. Change readiness: A construct to explain health and life transitions. J Theory Constr Test. 2004;8:26–33. [Google Scholar]
- 13.Timmer E, Steverink N, Dittmann-Kohli F. Cognitive representations of future gains, maintenance, and losses in the second half of life. Int J Aging Hum Dev. 2002;55(4):321–39. doi: 10.1177/009141500205500401. [DOI] [PubMed] [Google Scholar]
- 14.Furstenberg AL. Trajectories of aging: imagined pathways in later life. Int J Aging Hum Dev. 2002;55:1–24. doi: 10.2190/3H62-78VR-6D9D-PLMH. [DOI] [PubMed] [Google Scholar]
- 15.Wilcox S. Age and gender in relation to body attitudes: is there a double standard of aging? Psychol Women Q. 1997;21:549–65. [Google Scholar]
- 16.The WHOQOL Group. Development of the WHOQOL. Rationale and current status. Int J Mental Health. 1994;23:24–56. [Google Scholar]
- 17.The WHOQOL Group. The World Health Organization Quality of Life Assessment (WHOQOL): position paper from the World Health Organization. Soc Sci Med. 1995;41:1403–9. doi: 10.1016/0277-9536(95)00112-k. [DOI] [PubMed] [Google Scholar]
- 18.Bowling A. The concept of quality of life in relation to health. Med Secoli. 1995;7:633–45. [PubMed] [Google Scholar]
- 19.Naumann VJ, Byrne GJ. WHOQOL-BREF as a measure of quality of life in older patients with depression. Int Psychogeriatr. 2004;16:159–73. doi: 10.1017/s1041610204000109. [DOI] [PubMed] [Google Scholar]
- 20.Helvik AS, Engedal K, Selbaek G. The quality of life and factors associated with it in the medically hospitalized elderly. Aging Ment Health. 2010;14:861–69. doi: 10.1080/13607861003801003. [DOI] [PubMed] [Google Scholar]
- 21.Helvik AS, Engedal K, Krokstad S, Selbaek G. A comparison of life satisfaction in elderly medical inpatients and the elderly in a population-based study: Nord-Trondelag Health Study 3. Scand J Public Health. 2011;39:337–44. doi: 10.1177/1403494811405093. [DOI] [PubMed] [Google Scholar]
- 22.Levy BR, Slade MD, Kasl SV. Longitudinal benefit of positive perceptions of aging on functional health. J Geront Ser B Psychol Soc Sci. 2002;57B:409–17. doi: 10.1093/geronb/57.5.p409. [DOI] [PubMed] [Google Scholar]
- 23.Gift HC, Atchison KA. Oral health, health, and health-related quality of life. Med Care. 1995;33:57–77. doi: 10.1097/00005650-199511001-00008. [DOI] [PubMed] [Google Scholar]
- 24.Abdulla A, Adams N, Bone M, et al. Guidance on the management of pain in older people. Age Ageing. 2013;42(1):1–57. doi: 10.1093/ageing/afs200. [DOI] [PubMed] [Google Scholar]
- 25.Sherman FT. The geriatric giants. Don’t miss their footprints! Geriatrics. 2003;58(4):8. [PubMed] [Google Scholar]
- 26.Musso CG, Núñez JF. Feed-back between geriatric syndromes: general system theory in geriatrics. Int Urol Nephrol. 2006;38(3–4):785–86. doi: 10.1007/s11255-005-0060-4. [DOI] [PubMed] [Google Scholar]
- 27.Mendes de Leon CF, Rajan KB. Psychosocial influences in onset and progression of late life disability. J Gerontol B Psychol Sci Soc Sci. 2014;69(2):287–302. doi: 10.1093/geronb/gbt130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Katz S, Ford AB, Moskowitz RW, et al. Studies of illness in the aged: the index of ADL, a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–19. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 29.Wołowicka L, Jaracz K. [Quality of life in medical science]. Poznań: Wydawnictwo Uczelniane Akademii Medycznej w Poznaniu; 2001. [in Polish] [Google Scholar]
- 30.Costanza R, Fisher B, Ali S, et al. An integrative approach to quality of life measurement, research, and policy. Surv Perspect Integr Environ Soc. 2008;1(11–15):1–21. [Google Scholar]
- 31.Skevington SM, Lotfy M, O’Connell KA. The World Health Organization’s WHOQOL-BREF quality of life assessment: Psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res. 2004;13:299–310. doi: 10.1023/B:QURE.0000018486.91360.00. [DOI] [PubMed] [Google Scholar]
- 32.The WHOQOL Group. Development of the World Health Organization WHOQOL-BREF. Quality of Life Assessment. Psychol Med. 1998;28:551–58. doi: 10.1017/s0033291798006667. [DOI] [PubMed] [Google Scholar]
- 33.Nowakowska I, Rasińska R, Głowacka MD. [Analysis of relationships between perimenopausal symptoms and professional functioning and lifesatisfaction – Subjective perception of the dependence in women aged 40+]. Med Pr. 2015;66(3):351–58. doi: 10.13075/mp.5893.00243. [in Polish] [DOI] [PubMed] [Google Scholar]
- 34.Banaczek Z, Saracen A. [Life satisfaction and self-esteem among women in the menopausal time]. Wiad Lek. 2016;69(2):174–79. [in Polish] [PubMed] [Google Scholar]
- 35.URL: eceuropa.eu/health/newsletter/88/newsletter_plhtm 04.2012
- 36.Stadnicka G, Łepecka-Klusek C, Pilewska-Kozak AB, Jakiel G. Psychosocial problems of women with stress urinary incontinence. Ann Agric Environ Med. 2015;22(3):499–503. doi: 10.5604/12321966.1167723. [DOI] [PubMed] [Google Scholar]
- 37.Bojar I, Owoc J, Wójcik-Fatla A, et al. Cognitive functions, lipid profile, and Apolipoprotein E gene polymorphism in postmenopausal women. Ann Agric Environ Med. 2015;22(2):313–19. doi: 10.5604/12321966.1152086. [DOI] [PubMed] [Google Scholar]
- 38.European Economy. Feb, 2012. The 2012 Ageing Report – Economic and budgetary projections for 27 EU Member States (2010–2060) [Google Scholar]
- 39.European Year for Active Ageing and Intergenerational Solidarity. Available from: URL: www.europarleuropa.eu/news/pl/news-room/content/20110314IPR15479012.
- 40.Bączyk G, Samborski W, Jaracz K. Evaluation of the quality of life of postmenopausal osteoporotic and osteopenic women with or without fractures. Arch Med Sci. 2016;12(4):819–27. doi: 10.5114/aoms.2015.55012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bojar I. Prophylaxis of cognitive functions disorders progressing with age in women. Ann Agric Environ Med. 2015;22(4):573–75. [PubMed] [Google Scholar]
- 42.Drewnowski A, Evans WJ. Nutrition, physical activity, and quality of life in older adults. J Gerontol A Biol Sci Med Sci. 2001;56(2):89–94. doi: 10.1093/gerona/56.suppl_2.89. [DOI] [PubMed] [Google Scholar]
- 43.Visser M, Goodpaster BH, Kritchevsky SB, et al. Muscle mass, muscle strength, and muscle fat infiltration as predictors of incident mobility limitations in well-functioning older persons. J Gerontol A Biol Sci Med Sci. 2005;60(3):324–33. doi: 10.1093/gerona/60.3.324. [DOI] [PubMed] [Google Scholar]
- 44.Winkler P, Pochobradsky E, Wirl Ch. Wien: Gesundheit und Krankheit der älteren Generation in Österreich. 2012. [in German] [Google Scholar]
- 45.Sjölund BM. Physical functioning in old age: Temporal trends and geographical variation in Sweden. Karolinska Institutet; Solna: 2014. Available from: URL: http://hdl.handle.net/10616/41968. [Google Scholar]
- 46.Kerse N, Shaw L, Walker D. Staying Upright in Rest Home Care Trial-Final Report June 2009. 2008 Sep 18;4 [Google Scholar]
- 47.Marengoni A, Winblad B, Karp A, Fratiglioni L. Prevalence of chronic diseases and multimorbidity among the eldery population in Sweden. Am J Public Health. 2008;98(7):1198–200. doi: 10.2105/AJPH.2007.121137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Muniz-Terrera MF, Matthews F, et al. CC75C Group. Education and trajectories of cognitive decline over 9 years in very old people: methods and risk analisis. Age Ageing. 2009;38(3):277–82. doi: 10.1093/ageing/afp004. [DOI] [PubMed] [Google Scholar]
- 49.Hazra NC, Dregan A, Jackson S, Gulliford MC. Differences in health at age 100 according to sex: population-based cohort study of centenarians using electronic health records. J Am Geriatr Soc. 2015;63(7):1331–37. doi: 10.1111/jgs.13484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Leskowitz MJ, Caruana FF, Siedlecki B, et al. Asymmetric hearing loss is common and benign in patients aged 95 years and older. Laryngoscope. 2016;126(7):1630–32. doi: 10.1002/lary.25503. [DOI] [PubMed] [Google Scholar]
- 51.Jackson RA, Vittinghoff E, Kanaya AM, et al. Urinary incontinence in eldery woman: Findings from the health aging, and body composition study. Obstet Gynecol. 2004;104(2):301–7. doi: 10.1097/01.AOG.0000133482.20685.d1. [DOI] [PubMed] [Google Scholar]
- 52.Simenova Z, Milson J, Kullendorff AM, et al. The Prevalence of urinary incontinence and its influence on the quality of life in women from an urban Swedish population. Acta Obstet Gynecol Scand. 1999;78:546–51. [PubMed] [Google Scholar]
- 53.Minassian VA, Drutz HP, Al-Badr A. Urinary incontinence as a worldwide problem. Int J Gynaecol Obstet. 2003;82:327–33. doi: 10.1016/s0020-7292(03)00220-0. [DOI] [PubMed] [Google Scholar]
- 54.Galiana L, Gutiérrez M, Sancho P, et al. Socio-demographic variables and successful aging of the angolan elderly. Scientifica. 2016;2016:5306756. doi: 10.1155/2016/5306756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rowe JW, Kahn RL. Successful aging. Gerontologist. 1997;37(4):433–44. doi: 10.1093/geront/37.4.433. [DOI] [PubMed] [Google Scholar]
- 56.Waszkiewicz L, Połtyn-Zaradna K, Einhorn J, et al. Polityka Społeczna. Numer specjalny. Aspekty medyczne, psychologiczne, socjologiczne i ekonomiczne starzenia się ludzi w Polsce. Warszawa: PolSenior; 2011. [in Polish] [Google Scholar]
- 57.Fidecki W, Wysokiński M, Wrońska I, et al. [Life quality of senior citizens receiving long-term care in rural areas]. Probl Hig Epidemiol. 2011;92(2):221–25. [Google Scholar]
- 58.Low G, Molzahn AE, Schopflocher D. Attitudes to aging mediate the relationship between older peoples’ subjective health and quality of life in 20 countries. Health Qual Life Outcomes. 2013;11:146. doi: 10.1186/1477-7525-11-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zeng Y, Vaupel JW. Functional capacity and self-evaluation of health and life of oldest old in China. J Soc Issues. 2002;58(4):733–48. [Google Scholar]
- 60.Kozieł D, Trafiałek E. [Education at senior universities in relation to life quality of seniors. Assessing the influence of the studying]. Gerontologia Polska. 2007;15(3):104–8. [in Polish] [Google Scholar]
- 61.El-Azab A, Mohamed EM, Sabra HI. The prevalence and risk factors of urinary incontinence and its influence on the quality of life among Egyptian women. Neurourol Urodyn. 2007;26(6):783–88. doi: 10.1002/nau.20412. [DOI] [PubMed] [Google Scholar]
- 62.Erekson EA, Ciarleglio MM, Hanissian PD, et al. Functional disability among older women with fecal incontinence. Am J Obstet Gynecol. 2015;212(3):327. doi: 10.1016/j.ajog.2014.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Koziak B, Sangl J, Correa-de-Araujo R. Quality of health care for older women: What do we know? Women’s Health Issues. 2006;16:89–99. doi: 10.1016/j.whi.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 64.Kalfoss M, Halvorslud L. Important issues to quality of life among Norwegian older adults: An exploratory study. Open Nurs J. 2009;3:45–55. doi: 10.2174/1874434600903010045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Helvik AS, Engedal K, Selbæk G. Sense of coherence and quality of life in older in-hospital patients without cognitive impairment – a 12 month follow-up study. BMC Psychiatry. 2014;19(14):82. doi: 10.1186/1471-244X-14-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Norberg A, Lundman B, Gustafson Y, et al. Self-transcendence (ST) among very old people – Its associations to social and medical factors and development over five years. Arch Gerontol Geriatr. 2015;61(2):247–53. doi: 10.1016/j.archger.2015.04.003. [DOI] [PubMed] [Google Scholar]
- 67.Silverstein M, Heap J. Sense of coherence changes with aging over the second half of life. Adv Life Course Res. 2015;23:98–107. doi: 10.1016/j.alcr.2014.12.002. [DOI] [PubMed] [Google Scholar]
- 68.Błachnio A, Buliński L. Prejudices and elderly patients’ personality – the problem of quality of care and quality of life in geriatric medicine. Med Sci Monit. 2013;19:674–80. doi: 10.12659/MSM.889501. [DOI] [PMC free article] [PubMed] [Google Scholar]


