Abstract
Alien hand syndrome (AHS) is an involuntary and rare neurological disorder emerges at upper extremity. AHS is a disconnection syndrome with the symptoms of losing sense of agency and sense of ownership, and presence of involuntary autonomic motor activity. There are frontal, callosal and posterior types of AHS and each of them occurs depend on the lesions of different of the brain. Posterior variant is a rarely encountered AHS type compared to others. AHS, generally regarded as persistent, but rarely maybe observed as paroxysmal. In this article, we present 71 year old patient with right posterior parietal lobe infarction and developed posterior variant AHS on left arm 1 month after discharge from the hospital. To discriminate AHS from conditions such as extrapyramidal movement disorders and epileptic seizures that take part in differential diagnosis should be kept in mind by the clinicians. Wrong and unnecessary treatments could be prevented in this way.
Keywords: Alien hand syndrome, Posterior type, Stroke, Parietal lobe
Introduction
Alien hand syndrome (AHS) is a clinical condition characterized by involuntary, uncontrolled but seemingly purposeful movements at upper extremity (Park et al. 2012). This clinical condition commonly presents in the six decade or older male patients (Kikkert et al. 2006). In 1908, the syndrome was first defined by Goldstein as the apraxia of the person unable to recognize his/her own arm (Park et al. 2012). After 60 years, Brion et al. presented 3 cases with similar symptoms and identified AHS for the first time (Park et al. 2012; Kikkert et al. 2006). Anterior variant AHS occurs due to damage of frontal lobe and corpus callosum however in posterior variant AHS the territory of damage is in thalamus, parietal and occipital lobe (Park et al. 2012; Kikkert et al. 2006; Dolado et al. 1995). In order to raise the clinicians’ awareness of this rarely seen syndrome, we presented an AHS case in which involuntary motor symptoms emerged in left arm depending on the right parietal lobe infarction after the stroke.
Case
A right-handed 71-year old male patient consulted at the emergency service with a 2 months history of weakness in left arm and leg. Diffusion MRI revealed right posterior parietal lobe infarct associated with right median cerebral artery obstruction (Figs. 1, 2) He had hypertension in his medical history. The patient was screened for the cardio embolic causes of stroke. In MR angiography of the patient, 30 % occlusion in the right internal carotid artery was determined. 100 mg/day acetylsalicylic acid and anti-hypertensive treatment were given to the patient.
Fig. 1.

Cranial CT of case: right posterior parietal lobe enfact was shown. CT computed tomography
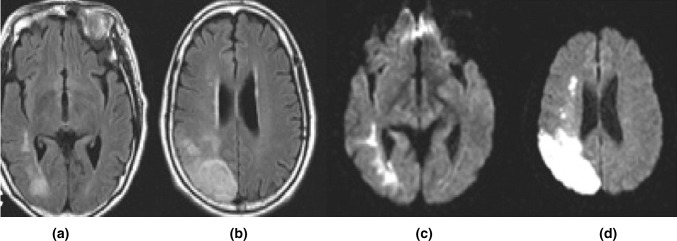
Fig. 2.
Diffusion MRI (a, b) and T1 MRI (c, d) of case: right posterior parietal lobe enfact was shown. MRI magnetic resonance image
One month after being discharged from hospital, the patient visited our outpatient neurology clinic with the complaint of ignoring the items in his left hand although he is conscious and sometimes, he does not feel the items in his hand. His left hand was moving involuntarily and paroxysmally and making seemingly purposeful movements (raising his arm up) for 30–40 min during the day. Meanwhile, the patient was conscious but the movements were out of his control. These movements were not rhythmic and there were no spasms in his arm. He could only stop movements and take control of his left hand with the effort of his right hand. Physical examination revealed no pathology. In neurological examination he had hemi hypoesthesia, central facial paralysis and lower limb weakness (4/5 on MRC scale) on the left side. His cerebellar, deep sensation and superficial sensory examinations were normal. His mini-mental state examination score was 28/30 points.
Brain computed tomography and MRI showed no new abnormality. Electroencephalography (EEG) was evaluated as normal. The patient was diagnosed with AHS upon the findings of his clinical anamnesis and neurological examination. The medical treatment was initiated with 1 mg/day of clonazepam. He was referred to the rehabilitation department for spatial recognition exercises; the patient was trained for recognizing different shapes and spatial arrangements and transferring the acquired skills to his daily tasks, leading to improve bimanual coordination and mirror box treatment. During the post-rehabilitation state frequency of symptoms were decreased compared to the initial stage. The patient continues to visit our neurology outpatient clinic regularly.
Discussion
AHS is one of the most intriguing disconnection syndromes of neurology. Commonly develops dissociation between targeted movement and actual movement of the hand. It’s typical symptoms contains of feeling of strange feeling towards the arm, lack of sense of ownership and involuntary autonomic motor activity (Leiguarda et al. 1993a; Doody and Jankovic 1992).
AHS may emerge with numerous symptoms and findings in the people having neurodegenerative diseases (corticobasal degeneration) and brain damage such as stroke, epilepsy, midline tumors, aneurysm and callosal damage (Kikkert et al. 2006).
There are 3 clinical variants in AHS. First variant (motor type) is associated with lesions in supplemental motor area, anterior singular gyrus or medial prefrontal cortex of the dominant hemisphere, grasping and groping reflexes on the right side are observed to involuntarily. In the second variant, conflicting movements between arms could be seen due to anterior corpus callosum lesions. The development of the third variant (posterior or sensitive type) is associated with corticobasal degeneration, lesions in posterior parietal lobe, occipital lobe or thalamus of the right hemisphere leads the unfamiliar and strange feeling and repetitive levitating movement in the hand (Terazzi et al. 2010; Kessler and Hathout 2009).
Our patient was found to have the diagnosis of posterior variant AHS, since he had unfamiliar feeling associated with the lesion in the posterior parietal lobe. He was ignoring items in his left hand and he had involuntary levitation movements. In order to differential diagnose, extrapyramidal system disorders should be considered. Our patient had parietal lobe damage and the nature of his movements were non-rhythmic and paroxysmal. Epileptic seizures were also eliminated, since the patient was conscious during the abnormal movements, the characteristics of movements were not tonic or clonic type, he was able to stop the movements voluntarily and EEG monitorization was normal.
Several hypotheses have been proposed but the pathophysiology of the posterior AHS remains unclear. Some authors proposed the hypothesis that AHS is a variant of neglect. It is a cortical sensory disorder associated with neglect, parietal lobe damage and characterized by the patient’s denial of the contralateral side of space. In posterior variant AHS, neglect occurs only in the contralateral arm due to the partial parietal lobe damage. While other studies suggest that the damage of inferior parietal lobe results with the dysfunction of various motor association fibers leading AHS (Martí-Fàbregas et al. 2000; Goldberg and Bloom 1990; Jeannerod 1988). However there have been cases observed as paroxysmal, clinical presentation of AHS is generally seen as persistent (André and Dominques 1996; Leiguarda et al. 1993b). This situation is generally confuses with epileptic seizures and could be distinguished with simultaneous EEG and clinical observation (Brázdil et al. 2006). Our case differs from the other AHS cases, because of the posterior variant AHS continues for 30–40 min of intervals.
AHS does not have a definite treatment yet. Some cases recovered by rehabilitation therapies such as mirror therapy and spatial recognition therapy. As a medical therapy clonazepam and botulinum toxin therapies also have been administered (Sarva and Deik 2014). Our case recovered partially with oral clonazepam and mirror therapy.
In this article a case of paroxysmal AHS associated with right parietal lobe damage was presented. Clinicians should be careful to distinguish this rare syndrome from the other clinical conditions such as extra-pyramidal movement disorders and epileptic seizures. By this way, wrong and unnecessary treatments could be prevented.
References
- André C, Dominques RC. Transient alien hand syndrome: is this a seizure or a transient ischaemic attack? J Neurol Neurosurg Psychiatry. 1996;60(2):232–233. doi: 10.1136/jnnp.60.2.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brázdil M, Kuba R, Rektor I. Rostral cingulate motor area and paroxysmal alien hand syndrome. J Neurol Neurosurg Psychiatry. 2006;77(8):992–993. doi: 10.1136/jnnp.2005.082529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolado AM, Castrillo C, Urra DG, de Seijas EV. Alien hand sign or alien hand syndrome? J Neurol Neurosurg Psychiatry. 1995;59:100–101. doi: 10.1136/jnnp.59.1.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doody RS, Jankovic J. The alien hand and related signs. J Neurol Neurosurg Psychiatry. 1992;55:806–810. doi: 10.1136/jnnp.55.9.806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg G, Bloom KK. The alien hand sign. Localization, lateralization and recovery. Am J Phys Med Rehabil. 1990;69:228–238. doi: 10.1097/00002060-199010000-00002. [DOI] [PubMed] [Google Scholar]
- Jeannerod M. The neuronal and behavioral organization of goal-directed movements. Oxford: Clarendon Press; 1988. [Google Scholar]
- Kessler J, Hathout G. Dominant posterior-variant alien hand syndrome after acute left parietal infarction. Clin Neurol Neurosurg. 2009;111:633–635. doi: 10.1016/j.clineuro.2009.05.006. [DOI] [PubMed] [Google Scholar]
- Kikkert MA, Ribbers GM, Koudstaal PJ. Alien hand syndrome in stroke: a report of 2 cases and review of the literature. Arch Phys Med Rehabil. 2006;87:728–732. doi: 10.1016/j.apmr.2006.02.002. [DOI] [PubMed] [Google Scholar]
- Leiguarda R, Starkstein S, Nogues M, Berthier M, Arbelaiz R. Paroxysmal alien hand syndrome. J Neurol Neurosurg Psychiatry. 1993;56:788–792. doi: 10.1136/jnnp.56.7.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leiguarda R, Starkstein S, Nogues M, Berthier M, Arbelaiz R. Paroxysmal alien hand syndrome. J Neurol Neurosurg Psychiatry. 1993;56:788–792. doi: 10.1136/jnnp.56.7.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martí-Fàbregas J, Kulisevsky J, Baró E, Mendoza G, Valencia C, Martí-Vilalta JL. Alien hand sign after a right parietal infarction. Cerebrovasc Dis. 2000;10:70–72. doi: 10.1159/000016028. [DOI] [PubMed] [Google Scholar]
- Park YW, Kim CH, Kim MO, Jeong HJ, Jung HY. Alien hand syndrome in stroke—case report and neurophysiologic study. Ann Rehabil Med. 2012;36(4):556–560. doi: 10.5535/arm.2012.36.4.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarva H, Deik A, Severt WL. Pathophysiology and treatment of alien hand syndrome. Tremor Other Hyperkinet Mov (N Y) 2014;4:241. doi: 10.7916/D8VX0F48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terazzi E, Mittino D, Monaco F (2010) Posterior alien hand in a left-handed person. BMJ Case Rep 19–24. doi:10.1136/bcr.10.2010.3401 [DOI] [PMC free article] [PubMed]