Abstract
Objectives
To examine trajectories in academic achievement for children with oral clefts versus unaffected classmates and explore predictors of persistently low achievement among children with oral clefts.
Design
Longitudinal cohort study of academic achievement in a population-based sample.
Setting and Participants
Children born from 1983 through 2003 with oral clefts were identified from the Iowa Registry for Congenital and Inherited Disorders and matched to unaffected classmates by sex, school/school district, and month and year of birth.
Main Outcome Measures
Academic achievement was measured from Iowa Testing Programs (ITP) data. Outcomes included achievement scores in reading, language, and mathematics.
Results
Academic achievement data were available for 586 children with oral clefts and 1,873 unaffected classmates. Achievement trajectories were stable for both groups. Children with oral clefts were more likely than their classmates to be classified into persistent, low achievement trajectories, including when adjusting for socioeconomic differences: OR=1.63, 95% CI: 1.23–2.16 for reading; OR=1.73, 95% CI: 1.29–2.31 for language; OR=1.45, 95% CI: 1.05–1.99 for math. Predictors of low achievement were cleft palate only (versus other cleft types), adolescent mothers, low maternal education, and less frequent use of prenatal care.
Conclusions
Most children have steady academic trajectories and children with oral clefts are at greater risk for persistent, low achievement in school than unaffected classmates. These findings support the need for routine, early screening for academic deficits in this population. Cleft palate only, low parental education and adolescent mothers are associated with increased risk for persistent low achievement.
Keywords: oral clefts, cleft lip, cleft palate, academic achievement, schooling problems
Isolated oral clefts, including cleft lip only (CL), cleft lip and palate (CLP), and cleft palate only (CP) affect 1 in ~700 live births.[1] In the United States, children with oral clefts are typically cared for by interdisciplinary teams for surgical repair of the cleft and follow-up care for complications with feeding, speech, and dental/orthodontic needs.[2–4] Children with oral clefts have been shown to be at elevated risk for learning problems compared to unaffected children, particularly in reading and related tasks.[5–10] Children with oral clefts have been found to receive more special education services, have lower grades, and complete secondary school at a lower rate than peers.[11,12] Recently, children with oral clefts have been shown to score lower than unaffected classmates on standardized tests of reading, math, and science, even when adjusting for potential confounders.[13]
Cross-sectional studies suggest that learning disabilities are less common in adolescents versus school-aged children with clefts.[5] However, some evidence of continued learning impairment comes from finding lower rate of college attendance among adults with oral clefts.[14] To our knowledge, there are no previous longitudinal studies tracking academic achievement in children with clefts. In addition to clarifying the persistence of academic deficits in children with oral clefts, longitudinal data are needed to identify achievement trends among these children and characteristics that differentiate those with persistent academic problems from those who consistently perform well in school or ultimately ‘catch up’ to their peers.
We used trajectory analysis to examine patterns of achievement in reading, math, and language from elementary school through high school for children with and without isolated oral clefts in a population-based sample. This analysis allows for a more thorough characterization of trends in a child’s academic achievement over time than analyses that focus on average differences over time or on cross-sectional comparisons at specific grade levels or ages. Trajectory analysis identifies groups of children that have similar patterns of academic achievement over their school years, such as persistently low or high academic achievement, or starting at low achievement but improving over time or vice-versa. We first determined whether children could be grouped based on their achievement trajectories, and whether these groups differed for children with oral clefts versus unaffected classmates. Next, among affected children, we examined sociodemographic and clinical variables that might be used to identify children at risk for persistently low achievement. This population is of particular clinical relevance, as children facing greater risks of academic deficits require educational and related developmental interventions that tend to be most effective when delivered in early elementary school or even before school entry.[15,16] Furthermore, persistent low achievement is a key risk factor for adverse long-term social and economic outcomes.[16]
METHODS
Study Population and Data Linkages
The study population and procedures have been described previously.[13] Briefly, children with isolated oral clefts were identified from the Iowa Registry for Congenital and Inherited Disorders (IRCID). There were 763 children with isolated clefts (without syndromes or other major birth defects) born to Iowa resident mothers from January 1, 1983 through December 31, 2003. IRCID data were linked with academic achievement data from the Iowa Testing Programs (ITP), described below, and birth certificate data on household sociodemographic characteristics. Twenty children died prior to school entry and 129 were not found in the ITP data (likely due to residing in other states in most cases), leaving 614 children with oral clefts (82.6% of the total sample) who had academic achievement scores.
Two classmates were identified for each affected child from the ITP database and matched by sex, month and year of birth, grade, and school. However, in several cases the affected child (~21%) or classmates (~25%) switched school districts during the study period. In these cases, additional classmates were selected and matched to the affected child by school district. We compared affected children to all their (first and latter) matched classmates over all grades to maintain the same composition of the classmate sample over time and to limit the effect of any potential bias from switching schools due to child academic performance or school factors. Matching criteria were relaxed when needed to locate two classmates, beginning with month then year of birth and then school. Matching on exact birth month, birth year, and school was relaxed for 78%, 9%, and 49% of affected children for at least one classmate. However, classmates were always matched by sex, grade, and school district. We describe below a sensitivity check to evaluate the effect of relaxing the matching criteria.
Academic achievement
We used the Iowa Tests of Basic Skills (ITBS, grades K-8) and the Iowa Tests of Educational Development (ITED, grades 9–12) to assess academic achievement in reading, language, and mathematics.[17] The ITBS and ITED are widely used standardized achievement tests with strong psychometrics. The norms and standardization for both tests were developed using a student sample representative of the United States population. These norms permit tracking each student’s achievement across time compared to national averages. These tests are administered to virtually all students in Iowa.
Test scores were the student’s national percentile rankings (NPRs), which reflect the percent of students in the normative sample who scored below the student in a particular domain. Test scores were linked to each study child (case/classmate) across their years in Iowa schools. The study was approved by the University of Iowa Institutional Review Board.
Predictors of Low Achievement
Sociodemographic and prenatal exposure data were collected from Iowa birth certificates completed from maternal/infant medical records and maternal self-reports. We investigated whether main sociodemographic and clinical measures modified the risk of being in the lowest academic trajectory among children with oral clefts. These variables were maternal education, age, and marital status at child’s birth, number of prenatal visits, child’s sex, first-born child, birth weight, low apgar scores, and cleft type.
Study Sample
Our analytical sample included child-grade observations of achievement at a given grade. To improve generalizability, we dropped kindergarten and grades 1 and 12 due to limited testing of students. We included ITP data through 2010, because tests and scoring changed significantly in 2011 (last year of available data). After all exclusions, the sample consisted of 586 children with oral clefts and 1873 classmates with test data on at least one domain. We included data on all matched classmates for all grades (before and after switching school districts) to preserve the classmate-sample composition over evaluated grades (2 through 11).
Because some children did not have test data for all outcomes, sample sizes ranged from 543 children with oral clefts (contributing 3261 child-grade observations) and 1772 classmates (11594 child-grade observations) for language to 584 children with oral clefts (3548 child-grade observations) and 1868 classmates (12533 child-grade observations) for mathematics. The analyses investigating predictors of membership in the lowest achievement trajectories (detailed below) included 548, 519, and 559 children with oral clefts who had testing data on reading, language, and mathematics, respectively, and on evaluated predictors.
Statistical Analysis
Trajectory analysis
Achievement trajectories were identified separately for reading, language, and mathematics using a maximum-likelihood finite-mixture model based on a censored-normal distribution to identify groups of children with similar patterns of academic achievement over time. The model estimates the child’s probability of belonging to each of the identified trajectories and assigns the child to the group with the highest probability. [18–20] We did not restrict the maximum number of achievement groups/trajectories a priori. Instead, we first assumed a minimum of four achievement trajectories/groups: (1) a steady low achievement group; (2) a group that begins low but improves over time; (3) a group that begins high but declines over time; and (4) a steady high achievement group. To determine whether to add or drop groups, we assessed the percentage of the total sample assigned to each group and differences in achievement between groups. A group was retained if it included ~10% or more of the sample (to ensure a reasonable minimum frequency per group and avoid estimating trajectories that apply to very few children) and the trajectory was statistically significant (p <0.05). We also used the Akaike-information-criterion (AIC) to assess model goodness-of-fit and its change with adding or eliminating trajectories. A new achievement group/trajectory was added if it had ~10% of the sample at minimum (and did not reduce frequency of other trajectories below 10%), was statistically significant, and lowered the AIC. For each trajectory, we first considered a polynomial function of achievement over grade/time beginning with a cubic relationship and eliminated non-linear terms (cubic and then squared terms) if non-significant.
We first tested the overall difference in group assignment between children with oral clefts and classmates using a chi-square test of association for each academic domain. Next, we tested the difference in probability of being in the lowest academic trajectory between children with oral clefts and their matched classmates only. We employed two estimations of the probability model. The first was conditional logistic regression which only compares children with oral clefts and their classmates when at least one child is not in the same group assignment as the others (e.g. a child with oral clefts assigned to the lowest trajectory with all his/her matched classmates will be excluded). Therefore, we also estimated a linear probability model with fixed effects for each child with oral clefts and his/her matched classmates, which retains the full sample. In addition to the unadjusted models, we estimated regressions adjusting for child’s birth order and maternal age, marital status, and maternal education to evaluate if they explain differences in assignment to the lowest trajectory. Maternal marital status and education are important indicators of socioeconomic status which is related to cleft risk and child development.[21–23] Maternal age is also a risk factor for oral clefting but also captures differences in parenting skills and experience.[24] Finally, birth order has also been related to both academic achievement (with an advantage generally for firstborn children, although the direction of effects may vary by socioeconomic status), as well as risk for oral clefting (reduced risk among firstborns).[25,26]
To examine the effect of relaxing matching criteria on our results, we re-estimated the linear probability models for risk of persistent, low achievement between affected and unaffected children controlling for fixed effects (0/1 dummy variables) for schools, month of birth, and year of birth instead of the fixed effects for the groups of each child with oral clefts and his/her matched classmates. These new controls account for the relaxing of matching criteria by conditioning on their effects.
Predicting the risk of being in low achievement trajectories
For each academic outcome, we evaluated potential predictors of being in the lowest achievement trajectory among children with oral clefts. Based on the child’s probabilities of belonging to each identified trajectory estimated as described above, the child was assigned to the trajectory with the highest probability. Then a binary variable was coded (for each testing domain) for whether the child was assigned to the lowest achievement trajectory or higher trajectories. Next, we employed logistic regression to predict the probability of being in the lowest trajectory, separately for each testing domain, as a function of the child and maternal characteristics described above. For comparison, we also estimated this model separately among classmates.
RESULTS
Sample Description
Children with oral clefts and classmates were similar on sociodemographic and clinical characteristics (Table 1). Most mothers were married, age 20–35 years at child’s birth, and had graduated high school or completed some college. The average number of tests per child was comparable between the two groups and across testing domains (approximately 4 tests).
Table 1.
Sample Descriptive Statistics for Children with Oral Clefts and Their Classmates
| Variable | Children with Oral Clefts | Classmates | ||
|---|---|---|---|---|
|
| ||||
| N | % | N | % | |
| Oral Clefts | ||||
| All Cleft Types | 586 | 100 | ||
| CL only | 218 | 37.2 | ||
| CP only | 135 | 23.0 | ||
| CLP | 233 | 39.8 | ||
|
| ||||
| Child sex | ||||
| Female | 248 | 42.3 | 798 | 42.6 |
| Male | 338 | 57.7 | 1075 | 57.4 |
|
| ||||
| Child first born | ||||
| No | 360 | 61.4 | 1163 | 62.1 |
| Yes | 226 | 38.6 | 710 | 37.9 |
|
| ||||
| Child birth weight (grams) | ||||
| <2500 | 34 | 5.8 | 100 | 5.3 |
| 2500–4000 | 467 | 79.7 | 1511 | 80.7 |
| >4000 | 85 | 14.5 | 262 | 14.0 |
|
| ||||
| Apgar score < 7 | ||||
| No | 510 | 87.0 | 1662 | 88.7 |
| Yes | 74 | 12.6 | 210 | 11.2 |
| Missing | 2 | 0.3 | 1 | 0.1 |
|
| ||||
| Mother married | ||||
| No | 118 | 20.1 | 361 | 19.3 |
| Yes | 467 | 79.7 | 1504 | 80.3 |
| Missing | 1 | 0.2 | 8 | 0.4 |
|
| ||||
| Maternal age (years) | ||||
| < 20 | 59 | 10.1 | 172 | 9.2 |
| 20–25 | 181 | 30.9 | 584 | 31.2 |
| 26–35 | 295 | 50.3 | 972 | 51.9 |
| > 35 | 51 | 8.7 | 144 | 7.7 |
| Missing | 1 | 0.1 | ||
|
| ||||
| Maternal education | ||||
| < High school | 78 | 13.3 | 216 | 11.5 |
| High school or some college | 402 | 68.6 | 1278 | 68.2 |
| ≥4 years of college | 101 | 17.2 | 368 | 19.7 |
| Missing | 5 | 0.9 | 11 | 0.6 |
|
| ||||
| Prenatal visits | ||||
| ≤6 | 25 | 4.3 | 84 | 4.5 |
| 7–9 | 77 | 13.1 | 221 | 11.8 |
| 10–12 | 272 | 46.4 | 952 | 50.8 |
| 13–15 | 155 | 26.5 | 449 | 24.0 |
| ≥15 | 40 | 6.8 | 125 | 6.7 |
| Missing | 17 | 2.9 | 42 | 2.2 |
|
| ||||
| N | 586 | 1873 | ||
Notes: The Table reports the percentages of the demographic, socioeconomic, and health variables for children with testing data in at least one academic domain.
Trajectories of Academic Achievement
The final trajectory models for reading, language, and mathematics identified 6 trajectories/groups (see Figures 1–3). For all three academic domains, achievement in Group 1 was characterized by steady, very low achievement (scores ≤ 30th percentile). Group 2 was characterized by consistently low average scores (~40th percentile) in reading and mathematics, and by gradually increasing scores in language. Groups 3 and 4 had variable scores across outcomes, showing improvement in some domains and declines in others. Groups 5 and 6 were the highest scoring groups with steady trajectories and scores ranging from the 70th to 90th percentile for all domains.
Figure 1. Reading Trajectories for Children with Oral Clefts and their Classmates.
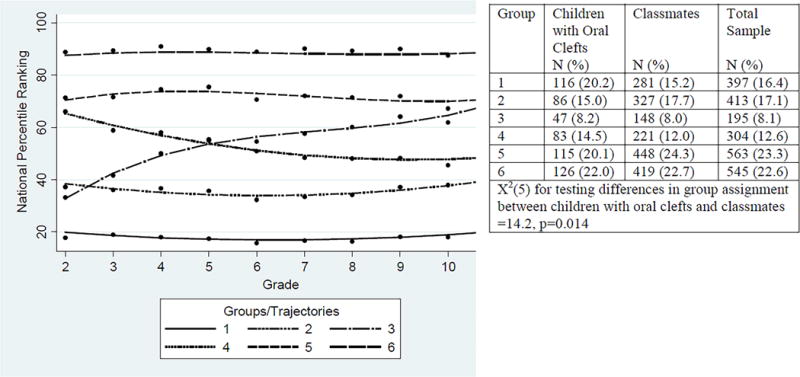
Notes: The dots show the actual group (trajectory) mean of percentile rankings at each grade level. Percentages of total sample, children with oral clefts, and unaffected classmates in each group/trajectory is shown on the right.
Figure 3. Mathematics Trajectories for Children with Oral Clefts and their Classmates.
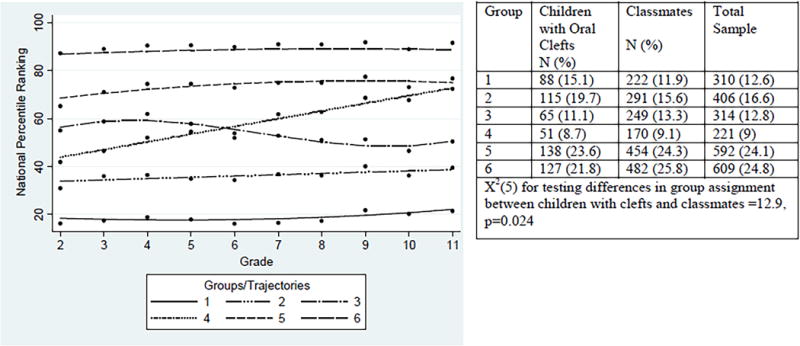
Notes: The dots show the actual group (trajectory) mean of percentile rankings at each grade level. Percentages of total sample, children with oral clefts, and unaffected classmates in each group trajectory is shown on the right.
Across all achievement domains, there were significant differences in group assignment between children with oral clefts and classmates (Figures 1–3). Children with clefts were more likely to be included in Group 1 (persistent, low achievement) than unaffected classmate. Group 1 included 15%-22% of children with oral clefts and 12%-1% of classmates. The greatest difference was for language, where one-fifth of children with oral clefts scored in the lowest trajectory, compared to 15% of classmates. Conversely, about one-quarter of classmates scored in the highest trajectory (Group 6) for language, compared to 18% of children with oral clefts. Findings were similar when comparing each child with an oral cleft only to his/her own matched classmates, to control for school/school-district effects, and with adjusting for maternal and child demographic characteristics (Table 2).
Table 2.
Differences in Risk of Assignment to Lowest Trajectory between Children with Oral Clefts and their Classmates
| Academic Domain | Linear Probability Model with Child-Classmates Fixed Effects | Conditional (Fixed-Effect) Logistic Regression | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| B | SE | N | OR | 95 % CI | N | |
| Reading | ||||||
| Unadjusted | 0.064*** | 0.017 | 2393 | 1.67*** | 1.28, 2.18 | 1134 |
| Adjusted | 0.057*** | 0.017 | 2393 | 1.63*** | 1.23, 2.16 | 1134 |
|
| ||||||
| Language | ||||||
| Unadjusted | 0.074*** | 0.018 | 2291 | 1.81*** | 1.38, 2.39 | 1055 |
| Adjusted | 0.065*** | 0.017 | 2291 | 1.73*** | 1.29, 2.31 | 1055 |
|
| ||||||
| Mathematics | ||||||
| Unadjusted | 0.038** | 0.015 | 2427 | 1.48** | 1.1, 2.0 | 938 |
| Adjusted | 0.032** | 0.015 | 2427 | 1.45** | 1.05, 1.99 | 938 |
Notes: Adjusted models include child’s first born status and maternal age, marital status, and education (the variables are entered as defined in Table 1). The βs represent difference in risk of assignment to lowest trajectory between children with an oral cleft and their classmates; standard errors (SE) are in parentheses. Odds Ratios (ORs) represent the ratio of the odds of children with oral clefts to be assigned to lowest trajectory to that of their classmates; 95% confidence intervals (CI) of ORs are reported. The fixed effects are for each child with oral clefts and his/her group of classmates. The conditional logistic regression only includes children with oral clefts and their classmates when they differ in their assignment to lowest trajectory. Because children with oral clefts are matched to their classmates on sex, the fixed effects account for sex (and the other matching characteristics that did not vary between affected children and classmates). The unadjusted model is estimated for the same sample with complete data on all variables included in the adjusted model.
p < 0.1,
p < 0.05,
p < 0.01
Relaxing matching criteria by including school, month of birth, and year of birth fixed effects also show consistent differences between cases and controls (Supplementary Table S1). Differences are slightly smaller and are no longer significant for Mathematics partly because of increased standard errors (because the school indicators have jointly insignificant effects on Mathematics scores in this model; thus, adding them removes variation from the case-classmate indicator without reducing the error-term variance).
Predictors of Low Academic Achievement in Children with Oral Clefts
Table 3 reports the results from the logistic regression predicting risk of persistent low achievement (Group 1) across the three testing domains among children with oral clefts. Children with CP tended to be classified in the low achievement trajectory group more often than those with CLP (and CL) for reading (marginally significant) and mathematics. Children of adolescent mothers were also more likely to be in the lowest trajectory for reading and language compared to mothers 26–35 years old. Higher maternal education was consistently related to a reduced risk of persistent poor performance across the three testing domains. Finally, receiving ≤ 9 prenatal visits compared to ≥ 15 was associated with greater risk of poor performance for reading and language. High maternal education was also associated with a decline in risk of low achievement among classmates but no significant associations with prenatal care and maternal age were found in that group (detail results available upon request).
Table 3.
Odds Ratios for Variables Predicting Assignment to Lowest Trajectory among Children with Oral Clefts
| Reading | Language | Mathematics | |
|---|---|---|---|
| Cleft Type (Ref=CLP) | |||
| CL | 0.85 [0.50,1.46] |
0.93 [0.55,1.56] |
0.80 [0.44,1.45] |
| CP | 1.65* [0.91,2.99] |
1.40 [0.76,2.60] |
2.02** [1.07,3.80] |
| Male (Ref=Female) | 0.78 [0.48,1.27] |
1.89** [1.14,3.13] |
0.96 [0.56,1.63] |
| First born (yes vs. no) | 0.68 [0.39,1.17] |
0.88 [0.52,1.50] |
0.74 [0.41,1.33] |
| Birth weight (Ref=2500–4000 gm) | |||
| < 2500 gm | 0.47 [0.16,1.39] |
0.29* [0.07,1.10] |
1.08 [0.36,3.25] |
| > 4000 gm | 0.81 [0.40,1.62] |
1.03 [0.55,1.95] |
1.13 [0.55,2.33] |
| Apgar < 7 (vs. ≥8) | 1.00 [0.50,2.03] |
0.86 [0.42,1.76] |
1.17 [0.56,2.44] |
| Mother married (vs. unmarried) | 0.82 [0.45,1.48] |
1.06 [0.59,1.91] |
0.80 [0.42,1.53] |
| Maternal age (Ref=26–35 years) | |||
| < 20 years | 2.39** [1.04,5.47] |
2.77** [1.22,6.29] |
1.75 [0.72,4.22] |
| 20–25 years | 1.44 [0.84,2.47] |
1.37 [0.81,2.34] |
1.12 [0.62,2.02] |
| > 35 years | 2.20* [0.92,5.24] |
1.40 [0.54,3.65] |
1.43 [0.52,3.90] |
| Maternal education (Ref= High school or some college) | |||
| < high school | 2.50*** [1.36,4.62] |
1.81* [0.97,3.38] |
2.52*** [1.32,4.83] |
| ≥4 years of college | 0.13*** [0.04,0.45] |
0.04*** [0.01,0.30] |
0.12*** [0.03,0.53] |
| Prenatal visits (Ref=≥15) | |||
| 6 or less | 4.53* [0.94,21.83] |
5.11** [1.09,23.91] |
1.01 [0.20,5.13] |
| 7–9 | 6.04*** [1.57,23.25] |
4.19** [1.07,16.35] |
1.71 [0.48,6.05] |
| 10–12 | 3.40* [0.95,12.11] |
2.92* [0.82,10.41] |
1.62 [0.51,5.11] |
| 13–15 | 2.09 [0.56,7.81] |
2.28 [0.62,8.41] |
1.19 [0.36,3.97] |
|
| |||
| N | 548 | 519 | 559 |
Notes: Odds ratios were estimated from logistic regression for risk of assignment to lowest trajectory while simultaneously including all variables. 95% confidence intervals are in brackets.
p < 0.1,
p < 0.05,
p < 0.01.
Coefficients for CL and CP were marginally different for Reading (p=0.09) and significantly different for Mathematics based on a Chow test (p=0.005).
DISCUSSION
This is the first longitudinal study of academic achievement in a population-based cohort of children with and without isolated oral clefts. Academic achievement was remarkably stable for children in both groups. Children with oral clefts were more likely than their classmates to exhibit persistent, low achievement for all outcomes and this gap was not explained by sociodemographic differences alone. This argues against the notion that children with oral clefts initially exhibit low achievement, but ‘catch up’ to their peers in late adolescence.[5] Among children with clefts, low academic achievement was associated with cleft type, with children with CP tending to be classified in this trajectory more often than those with CLP (or CL), and with characteristics such as younger maternal age and lower maternal education.
The stability of academic achievement scores suggests the importance of early identification of children with oral clefts who are at greatest risk for academic deficits. Although we do not yet have adequate data on the malleability of achievement trajectories for children with oral clefts, in other populations (e.g., children at risk for reading failure), there is good evidence that academic interventions beginning in early elementary school result in clinically meaningful improvements.[27,28] Children with oral clefts are typically followed by a craniofacial team, and screening for learning problems has been recommended as part of this team care.[29] Although screening practices vary across centers, and may or may not include formal assessments of early learning, most centers routinely assess development and cognitive functioning.[30] Such evaluations can be coordinated with school personnel, ensuring that children receive special education or other needed services. Characteristics found to predict poor academic achievement in this study (e.g., diagnosis of CP, children born to adolescent and low educated mothers, and children born to mothers who received few prenatal visits) can be easily obtained from interviewing mothers and examining clinical records, and craniofacial teams are encouraged to evaluate these characteristics and consider using them to identify children and families who might benefit from closer monitoring and early intervention. Screening and interventions may be initiated prior to school entry, using public-health models developed for primary care settings (e.g., Reach out and Read).[31]
In addition to the longitudinal design, the strengths of our study include population-based sampling of a large cohort of children with and without oral clefts. This allowed us to control for several confounders that have limited earlier studies of clinic-based samples. The ITBS and ITED are psychometrically sound, widely used measures of achievement and contribute to the external validity of our findings. Limitations include the relatively homogeneous sample. Our sample was representative of the state of Iowa, and children with and without oral clefts were demographically comparable, though the trajectories observed might differ in other populations. We did not have data on the interventions that children in our sample received, which may affect achievement trajectories. For example, while we have data on special education placement, data are not available on the types of interventions received or special education classification. Educational interventions in school and community (e.g., private tutoring), might modify academic trajectories.
Finally, we do not have data on child, family, or school variables that might account for the observed differences. Previous studies have reported differences in brain morphology in individuals with clefts, which may account for the greater risk for persistent low academic achievement.[32] However, other factors (e.g., missed school due to illness or medical procedures, differential treatment by caregivers or teachers) are also plausible and warrant investigation. Also, other confounders such as maternal use of medications during pregnancy may be at play. To further check for confounding, we estimated a model adding maternal smoking during pregnancy, a well-known risk factor for oral clefts and child development, as a covariate in addition to a dummy variable to indicate observations with missing data on smoking (~40%) to retain the full sample.[33,34] We found the same results as those in Table 2 (Supplementary Table S1). Potential confounding does not necessarily take away from the main implications of finding that children with oral clefts are at greater risk of persistent, low academic achievement than classmates. However, accounting for confounding is important for understanding the mechanisms, and whether the risk difference results from having a cleft or from differences in maternal and household factors that predispose to oral clefts. Given the similar results between adjusted and unadjusted models and controlling for school/school-district effects, it is unlikely that the risk difference is primarily driven by confounders although the possibility of confounding remains.
Conclusion
This is the first longitudinal study to track academic achievement of children with oral clefts compared to unaffected classmates. Children with oral clefts were more likely than classmates to receive persistent, low achievement scores in core academic skills. Future research is needed to explore the malleability of achievement trajectories for children with oral clefts in response to intervention efforts. These findings support the recommendation for children with oral clefts to be screened for learning problems as part of their craniofacial team care.
Supplementary Material
Figure 2. Language Trajectories for Children with Oral Clefts and their Classmates.
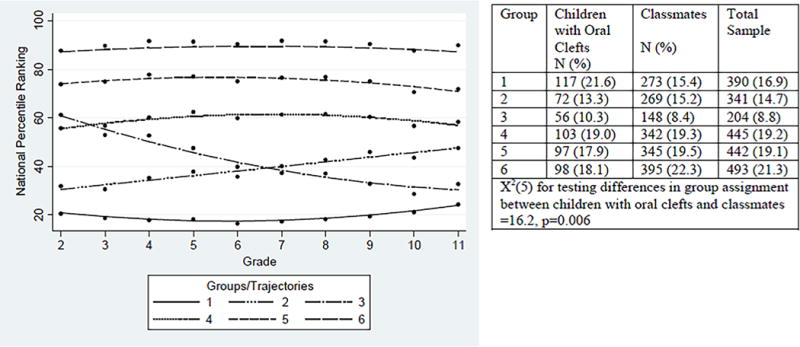
Notes: The dots show the actual group (trajectory) mean of percentile rankings at each grade level. Percentages of total sample, children with oral clefts, and unaffected classmates in each group trajectory is shown on the right.
WHAT IS ALREADY KNOWN ON THIS TOPIC.
Children with isolated oral clefts are at greater risk for academic failure than unaffected controls. Cross sectional studies suggest that children with isolated clefts may ‘catch up’ to their peers academically in adolescence.
WHAT THIS STUDY ADDS.
This is the first longitudinal study to track academic achievement in children with isolated oral clefts from early elementary school through high school. Children with oral clefts were more likely than their classmates to exhibit persistent, low achievement on reading, language and mathematics. Predictors of persistent low achievement included cleft palate only, younger maternal age at delivery, and low maternal education.
Acknowledgments
FUNDING. This work was supported by grant 1 R03 DE022094 from the National Institutes of Health/National Institute of Dental and Craniofacial Research.
Footnotes
COMPETING INTERESTS. None
Publication statement:
The Corresponding Author has the right to grant on behalf of all authors and does grant on behalf of all authors, an exclusive licence (or non-exclusive for government employees) on a worldwide basis to the BMJ and co-owners or contracting owning societies (where published by the BMJ on their behalf), and its Licensees to permit this article (if accepted) to be published in Archives of Disease in Childhood and any other BMJ products and to exploit all subsidiary rights, as set out in our licence.
References
- 1.Mai CT, Cassell CH, Meyer RE, et al. Birth Defects Data from Population-based Birth Defects Surveillance Programs in the United States, 2007 to 2011: Highlighting Orofacial Clefts. Birth Defects Res A Clin Mol Teratol. 2014 doi: 10.1002/bdra.23329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bluestone CD. Studies in otitis media: Children’s Hospital of Pittsburgh-University of Pittsburgh progress report–2004. The Laryngoscope. 2004;114(11 Pt 3 Suppl 105):1–26. doi: 10.1097/01.mlg.0000148223.45374.ec. [DOI] [PubMed] [Google Scholar]
- 3.Kuehn DP, Moller KT. The state of the art: Speech and language issues in the cleft palate population. Cleft Palate-Cran J. 2000;37(4):348–348. [Google Scholar]
- 4.Masarei AG, Sell D, Habel A, et al. The nature of feeding in infants with unrepaired cleft lip and/or palate compared with healthy noncleft infants. Cleft Palate Craniofac J. 2007;44(3):321–328. doi: 10.1597/05-185. [DOI] [PubMed] [Google Scholar]
- 5.Richman LC, McCoy TE, Conrad AL, et al. Neuropsychological, behavioral, and academic sequelae of cleft: early developmental, school age, and adolescent/young adult outcomes. Cleft Palate Craniofac J. 2012;49(4):387–396. doi: 10.1597/10-237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Collett BR, Stott-Miller M, Kapp-Simon KA, et al. Reading in Children with Orofacial Clefts versus Controls. J Pediatr Psychol. 2010;35(2):199–208. doi: 10.1093/jpepsy/jsp047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Richman LC. Neuropsychological development in adolescents: cognitive and emotional model for considering risk factors for adolescents with cleft. Cleft Palate Craniofac J. 1995;32(2):99–103. doi: 10.1597/1545-1569_1995_032_0099_ndiaca_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 8.Richman LC, Ryan SM. Do the reading disabilities of children with cleft fit into current models of developmental dyslexia? Cleft Palate-Cran J. 2003;40(2):154–157. doi: 10.1597/1545-1569_2003_040_0154_dtrdoc_2.0.co_2. [DOI] [PubMed] [Google Scholar]
- 9.Richman LC, Wilgenbusch T, Hall T. Spontaneous verbal labeling: visual memory and reading ability in children with cleft. Cleft Palate Craniofac J. 2005;42(5):565–569. doi: 10.1597/04-128r.1. [DOI] [PubMed] [Google Scholar]
- 10.Conrad AL, Richman L, Nopoulos P, et al. Neuropsychological Functioning in Children with Non-Syndromic Cleft of the Lip and/or Palate. Child Neuropsychology. 2009;15(5):471–484. doi: 10.1080/09297040802691120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yazdy MM, Autry AR, Honein MA, et al. Use of special education services by children with orofacial clefts. Birth Defects Research Part A: Clinical and Molecular Teratology. 2008;82(3):147–154. doi: 10.1002/bdra.20433. [DOI] [PubMed] [Google Scholar]
- 12.Persson M, Becker M, Svensson H. Academic achievement in individuals with cleft: a population-based register study. Cleft Palate Craniofac J. 2012;49(2):153–159. doi: 10.1597/09-047. [DOI] [PubMed] [Google Scholar]
- 13.Wehby G, Collett BR, Romitti P, et al. Academic achievement of children and adolescents with oral clefts. Pediatrics. 2014;133:785–792. doi: 10.1542/peds.2013-3072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ramstad T, Ottem E, Shaw WC. Psychosocial adjustment in Norwegian adults who had undergone standardised treatment of complete cleft lip and palate: I. Education, employment and marriage. Scand J Plast Reconstr Surg. 1995;29:251–257. doi: 10.3109/02844319509050135. [DOI] [PubMed] [Google Scholar]
- 15.Reynolds RJ, Temple JA, Ou S, Arteaga IA, White BAB. School-based early childhood education and age-28 well-being: Effects by timing, dosage, and subgroups. Science. 2011;333:360–364. doi: 10.1126/science.1203618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heckman JJ. Skill formation and the economics of investing in disadvantaged children. Science. 2006;312:1900–1902. doi: 10.1126/science.1128898. [DOI] [PubMed] [Google Scholar]
- 17.Hoover HD, Dunbar SB, Frisbie DA. The Iowa Test of Basic Skills: Guide to research and development. Itasca, IL: Riverside; 2003. [Google Scholar]
- 18.StataCorp. Stata Statistical Software: Release 12. College Station, TX: StataCorp LP; 2011. [Google Scholar]
- 19.Jones BL, Nagin DS. A Stata Plugin for Estimating Group-Based Trajectory Models. 2012 http://www.indiana.edu/~wim/docs/Info%20about%20STATA%20plugin.pdf.
- 20.Jones BL, Nagin DS. A Note on a Stata Plugin for Estimating Group-based Trajectory Models. Sociol Methods Res. 2013;42:608. [Google Scholar]
- 21.Clark JD, Mossey PA, Sharp L, Little J. Socioeconomic status and orofacial clefts in Scotland, 1989 to 1998. Cleft Palate Craniofac J. 2003;40:481–485. doi: 10.1597/1545-1569_2003_040_0481_ssaoci_2.0.co_2. [DOI] [PubMed] [Google Scholar]
- 22.Wehby GL, McCarthy AM. Economic gradients in early child neurodevelopment: a multi-country study. Soc Sci Med. 2013;78:86–95. doi: 10.1016/j.socscimed.2012.11.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wehby GL, McCarthy AM, Castilla EE, Murray JC. The Impact of Household Investments on Early Child Neurodevelopment and on Racial and Socioeconomic Developmental Gaps - Evidence from South America. Forum Health Econ Policy. 2012;14:11. doi: 10.2202/1558-9544.1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bille C, Skytthe A, Vach W, Knudsen LB, Andersen AM, Murray JC, Christensen K. Parent’s age and the risk of oral clefts. Epidemiology. 2005;16:311–316. doi: 10.1097/01.ede.0000158745.84019.c2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Black Sandra E, Devereux Paul J, Salvanes Kjell G. The More the Merrier? The Effect of Family Size and Birth Order on Children’s Education Quarterly. J Econ. 2005;120:669–700. [Google Scholar]
- 26.Kantarevic Jasmin, Mechoulan Stephane. Birth Order, Educational Attainment, and Earnings: An Investigation Using the PSID. J Hum Resour. 2006;41:755–77. [Google Scholar]; Vieira AR, Orioli IM. Birth order and oral clefts: a meta analysis. Teratology. 2002;66:209–216. doi: 10.1002/tera.10088. [DOI] [PubMed] [Google Scholar]
- 27.Connor CM, Morrison FJ, Fishman B, et al. A longitudinal cluster-randomized controlled study on the accumulating effects of individualized literacy instruction on students’ reading from first through third grade. Psychol Sci. 2013;24:1408–19. doi: 10.1177/0956797612472204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Saine NL, Lerkkanen MK, Ahonen T, et al. Computer-assisted remedial reading intervention for school beginners at risk for reading disability. Child Dev. 2011;82(3):1013–1028. doi: 10.1111/j.1467-8624.2011.01580.x. [DOI] [PubMed] [Google Scholar]
- 29.Parameters for the Evaluation and Treatment of Patients with Cleft Lip/Palate or Other Craniofacial Anomalies. American Cleft Palate-Craniofacial Association. Cleft Palate-Craniofac J. 1993;30(Suppl 1) [PubMed] [Google Scholar]
- 30.Hood MM, Cradock MM, Vander Wal JS. A survey of psychological assessment on interdisciplinary craniofacial teams. Cleft Palate-Craniofac J. 2011;48:425–444. doi: 10.1597/09-252. [DOI] [PubMed] [Google Scholar]
- 31.Zuckerman B. Promoting early literacy in pediatric practice: Twenty years of Reach Out and Read. Pediatrics. 2009;124:1660–1665. doi: 10.1542/peds.2009-1207. [DOI] [PubMed] [Google Scholar]
- 32.Nopoulos P, Langbehn DR, Canady J, et al. Abnormal brain structure in children with isolated clefts of the lip or palate. Arch Pediatr Adolesc Med. 2007;161:753–758. doi: 10.1001/archpedi.161.8.753. [DOI] [PubMed] [Google Scholar]
- 33.Wehby G, Jugessur A, Murray JC, Moreno L, Wilcox A, Lie RT. Genes as instruments for studying risk behavior effects: An application to maternal smoking and orofacial clefts. Health Serv Outcomes Res Methodol. 2011;11:54–78. doi: 10.1007/s10742-011-0071-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wehby GL, Prater K, McCarthy AM, Castilla EE, Murray JC. The impact of maternal smoking during pregnancy on early child neurodevelopment. J Hum Cap. 2011;5:207–254. doi: 10.1086/660885. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


