Abstract
Objective
To report three cases of embryonal rhabdomyosarcoma (ERMS) of the cervix in young women successfully treated with fertility-sparing surgery and chemotherapy.
Methods
Between January 2014 and December 2015, three cases of ERMS of the cervix were confirmed in young women at a single tertiary cancer center. All cases were managed by a pediatric oncologist and a gynecologic oncologist with a combination of surgery and chemotherapy. Fertility-sparing surgeries (cervical conization or robotic-assisted radical trachelectomy) were offered to patients depending on the tumor size.
Results
All patients were nulliparous and aged 14, 20 and 21 years and all presented with abnormal uterine bleeding. The first patient was managed with radical trachelectomy followed by adjuvant chemotherapy. The second patient underwent primary hysteroscopic resection of the tumor followed by completion cervical conization and adjuvant chemotherapy. The third patient received neoadjuvant chemotherapy followed by loop electrosurgical excision procedure (LEEP) with positive residual margins. She then underwent completion radical trachelectomy. None of the patients experienced perioperative complications. None of the women received radiation. All patients are alive with no evidence of disease.
Conclusion
Fertility-sparing surgery and chemotherapy in well-selected patients with ERMS of the cervix result in low complication rates and excellent oncologic outcomes. This treatment option may be considered in young patients who wish to preserve fertility by avoiding hysterectomy. A collaborative effort between pediatric oncologists and gynecologic oncologists is imperative to facilitate innovative approaches to these rare tumors in young adults.
Keywords: Embryonal rhabdomyosarcoma, Sarcoma botryoides, Fertility-sparing surgery, Radical trachelectomy
Highlights
-
•
Embryonal RMS of the cervix has an excellent prognosis when treated adequately.
-
•
Embryonal RMS of the cervix is treated with surgery and multi-agent chemotherapy.
-
•
Fertility-sparing surgery can be offered in young patients with early cervical RMS.
1. Introduction
Rhabdomyosarcomas (RMS) are soft tissue sarcomas arising from primitive mesenchymal cells. RMS can arise from any part of the body, with head and neck region and genitourinary tract being the most common sites (Dehner et al., 2012). These tumors are uncommon in adults but account for over half of soft tissue sarcomas in children (Pastore et al., 2006). The Intergroup Rhabdomyosarcoma Study Group (IRSG) identified three histologic subtypes including embryonal, alveolar, and undifferentiated (Kriseman et al., 2012). The embryonal subtype is further divided into classic, botryoid, and spindle cell (Kriseman et al., 2012). Botryoid variant is responsible for the majority of cases of embryonal RMS (ERMS) of the cervix.
Cervical RMS are rare and usually affect young women in the first or second decades of life (Bernal et al., 2004). In the adult literature, there are no standard treatments for the management of ERMS of the cervix as only small case series and case reports are available. Often multimodality treatments with a combination of surgery or RT and systemic chemotherapy are utilized. The 5-year overall survival for locoregional disease is excellent ranging from 80 to 90% (Ferguson et al., 2007, Arndt et al., 2001). Significantly, the cost of cure often includes infertility secondary to pelvic RT and/or hysterectomy.
Through collaboration with our pediatric oncology colleagues, we treated 3 patients with ERMS of the cervix with fertility-sparing surgery and chemotherapy, and herein report their outcome. In our study, cervical conization was performed in the management of one patient, while robotic-assisted radical trachelectomy was performed in the other two cases. To our knowledge, only one other case report is available in the literature describing the use of radical trachelectomy in the management of cervical ERMS (Kayton et al., 2009).
2. Methods
Between January 2014 and December 2015, three cases of ERMS of the cervix were confirmed in young women at a single tertiary cancer center. All cases were managed by a multidisciplinary team including a pediatric oncologist, a gynecologic oncologist and a gynecologic pathologist. A combination of minimally invasive fertility-sparing surgery and systemic chemotherapy was offered to all patients. Fertility-sparing surgery included cervical conization or robotic-assisted radical trachelectomy depending on the tumor size. All patients underwent pre-operative imaging including pelvic MRI to assess tumor size and local spread as well as CT scans of the chest, abdomen and pelvis to rule out metastatic disease. A frozen section of the cervical cone or trachelectomy specimen was performed intraoperatively to evaluate surgical margin. The chemotherapy regimen included a combination of vincristine, actinomycin-D and cyclophosphamide (VAC). Patients were referred for genetic counseling for consideration of DICER1 molecular genetic analysis. A written informed consent was obtained from all patients included in the study.
3. Results
3.1. Case #1
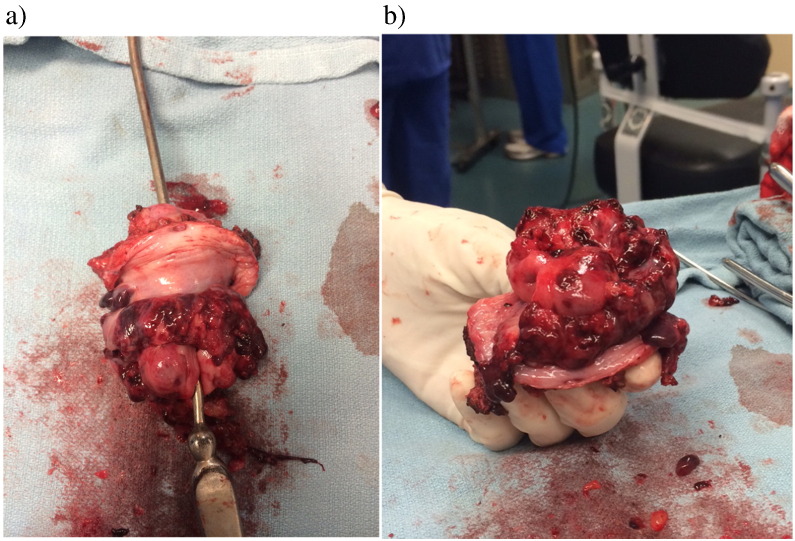
A 14 year-old gravida 0 adolescent girl was experiencing dysfunctional uterine bleeding after menarche. A year later, she noticed a mass protruding through the vagina. A pelvic MRI confirmed a large exophytic mass measuring 5.3 × 2.9 × 6.7 cm and involving the lower aspect of the cervix. She had no evidence of vaginal, parametrial or uterine invasion. Pelvic MRI and CT scans showed no evidence of extra-cervical disease. Pathological confirmation of the tumor histology was performed pre-operatively. Robotic-assisted radical trachelectomy with placement of abdominal cerclage was performed without complications (Fig. 1). She was discharged home on post-operative day 1. Final pathology confirmed ERMS with diffuse anaplastic features and heterologous (cartilage) differentiation. Surgical margins were negative for malignancy (4.8 mm from radial margin, 18 mm from endocervical margin, 14 mm from vaginal margin). Patient was referred for molecular genetic analysis of DICER1. She was enrolled in Children's Oncology Group ARST 0531 clinical trial and received 43 weeks of VAC alternating with vincristine and irinotecan. Her menses have resumed and are regular. She has no evidence of disease 10 months following diagnosis.
Fig. 1.
a - Radical trachelectomy specimen of case # 1 with 5.3 × 2.9 × 6.7 cm cervical RMS involving the lower aspect of the cervix. b - The completely excised embryonal rhabdomyosarcoma is observed in the trachelectomy specimen with negative vaginal, uterine and parametrial margins.
3.2. Case #2
A 20 year-old gravida 0 woman presented with heavy vaginal bleeding and a mass protruding through the vaginal introitus. On exam, she was found to have a 5 cm polypoid mass with pedunculated narrow stalk arising from the posterior lip of the cervix. Ultrasound confirmed a 5.9 × 3.9 × 2.9 cm polypoid cervical mass. She was taken to the operating room at an outside institution for an examination under anesthesia. At that time, the mass had detached from the posterior aspect of the cervix with only the stalk remaining. Pathological assessment confirmed ERMS of the cervix. Postoperatively a pelvic MRI showed no evidence of residual disease and CT scans were negative for distant disease. She underwent a hysteroscopic assessment of the cervical canal and uterine cavity followed by a cervical conization to remove potential residual disease. Frozen section assessment showed negative margins and identified the site of the previous tumor stalk. Final pathology showed no residual tumor. She then received adjuvant chemotherapy with 4 cycles of VAC followed by 4 cycles of VA. Molecular genetic analysis of DICER1 is underway. Her menses have resumed and are regular. She has no evidence of disease 25 months from diagnosis.
3.3. Case #3
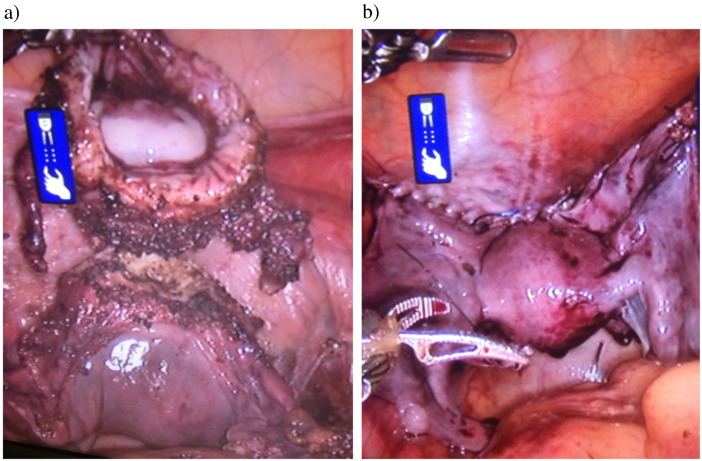
A 21 year-old gravida 0 woman presented with a one-year history of abnormal uterine bleeding. Pelvic examination revealed a large polypoid cervical mass which was confirmed to be an embryonal RMS on biopsy. Pelvic MRI demonstrated a 3.3 × 1.7 × 2.8 cm polypoid mass involving the cervix and extending into the endocervical canal. The mass appeared to be involving the vaginal fornices and upper vagina. Considering the size of the cervical lesion and the vaginal involvement, neoadjuvant chemotherapy was recommended and she received 6 cycles of VAC. She had a near complete response and underwent a diagnostic LEEP at an outside institution. Pathological assessment indicated that the deep resection margin was positive for residual RMS. She was counseled regarding management options which included a cold knife cone versus a trachelectomy and she elected to proceed with a completion trachelectomy. She underwent an uncomplicated robotic assisted radical trachelectomy and placement of an abdominal cerclage (Fig. 2). Frozen section assessment showed negative margins and the final pathology showed no residual disease and confirmed negative vaginal and uterine margins. Molecular genetic analysis did not detect a pathogenic variant in DICER1. Her menses have not yet resumed. She has no evidence of disease 21 months after diagnosis.
Fig. 2.
a - The vaginectomy is performed with adequate margins. The cervix is amputated from the uterus at the level of the internal os. b - At the end of the procedure, the peritoneum is sutured over the abdominal cerclage and adequate perfusion of the uterus is observed.
Clinical results for all patients are summarized in Table 1.
Table 1.
Baseline characteristics, treatments and clinical outcomes.
NACT: neoadjuvant chemotherapy; VAC: vincristine, actinomycin-D and cyclophosphamide; VA: vincristine and actinomycin-D; RTrach: robotic-assisted radical trachelectomy; LEEP: loop electrosurgical excisional procedure; NED: no evidence of disease.
| Case | Age | Size of cervical lesion (cm) | Pre-operative NACT | Surgery | Post-operative adjuvant chemotherapy | Vital status, months of follow-up |
|---|---|---|---|---|---|---|
| 1 | 14 | 5.3 × 2.9 × 6.7 | No | Primary RTrach | 35 of 43 weeks – ARST 0531 protocol | NED, 8 months |
| 2 | 20 | 5.9 × 3.9 × 2.0 | No | Hysteroscopy + cone | 4 cycles of VAC and 4 cycles of VA | NED, 22 months |
| 3 | 21 | 3.3 × 1.7 × 2.8 | 6 cycles of VAC | LEEP followed by RTrach | No | NED, 21 months |
4. Discussion
Embryonal rhabdomyosarcoma of the cervix is a rare malignancy; occurring in less than 0.2% of all cervical malignancies (Bernal et al., 2004, Daya and Scully, 1988). The standard treatment remains controversial as most of our understanding of this disease is derived from case reports with varying surgical treatments and adjuvant therapies or pediatric literature. ERMS of the cervix usually affects adolescent girls and young adults (Daya and Scully, 1988). In recent years, there has been a paradigm shift favoring fertility-preservation in young women with varying malignancies, which poses a greater challenge in the management of cervical RMS. We report three cases of ERMS of the cervix managed successfully with fertility-sparing surgery (cervical conization or robotic-assisted radical trachelectomy) in combination with multi-agent chemotherapy.
ERMS of the cervix rarely presents in older women and is thought to behave more aggressively in the older age-group (Ferguson et al., 2007). The classic presentation of cervical RMS is abnormal bleeding with a palpable mass protruding through the vagina (Bernal et al., 2004). All three patients experienced these symptoms. Our patients were in the first or second decade of life and were nulliparous, therefore, fertility-sparing surgery was important to consider when discussing treatment options. Two patients underwent robotic-assisted radical trachelectomy and one patient had a cervical conization. Importantly, all three patients had successful fertility preserving therapy despite having a large cervical mass at presentation.
Between 1972 and 1978, the first Intergroup Rhabdomyosarcoma Study Group (IRSG) trial, recommended radical surgery followed by chemotherapy for the management of embryonal RMS of the genital tract (Arndt et al., 2001, Hays et al., 1985). Radical surgeries included radical hysterectomy and, in some instances, pelvic exenteration were performed as part of the treatment protocol for this disease. The second IRSG trial (1978–1984) introduced neoadjuvant chemotherapy to shrink the tumor size, allowing for a less radical surgery with organ preservation such as polypectomy or cervical conization (Raney et al., 1990). Notably, the survival outcomes of embryonal RMS of the genital tract were not compromised by a more conservative surgery and remained excellent with 5-year overall survival of 87% in non-metastatic tumors (Arndt et al., 2001). Brand et al. reached similar results with survival rate of 80% at 68 months with the use of multimodality therapy including conservative surgery and combination chemotherapy (Brand et al., 1987).
Interestingly, the radical trachelectomy procedure was first described by Professor Dargent in the 1990s for the management of early-stage cervical cancer in women who wish to retain fertility (Dargent et al., 2000). This procedure can be performed using either a vaginal, abdominal, laparoscopic or robotic approach. Complications rates are comparable to radical hysterectomy. In cervical carcinoma, radical trachelectomy achieves similar oncologic outcomes to the gold standard radical hysterectomy. We encountered one case report in the literature that describes the use of radical abdominal trachelectomy for the management of ERMS (Kayton et al., 2009). Kayton et al. reported a case of ERMS of the cervix in a 12-year-old girl who received 4 cycles of combination chemotherapy followed by radical abdominal trachelectomy (Kayton et al., 2009). Radical trachelectomy allows for complete removal of the cervical tumor with vaginal and parametrial margins, while preserving the uterine fundus and lower uterine segment. To our knowledge, our report is the first report on the use of minimally invasive surgery to perform radical trachelectomy in the management of ERMS of the cervix.
Interestingly, ERMS of the cervix has been associated with other primary cancers. Kriseman et al. reported on 2 patients with cervical embryonal RMS who also had Sertoli-Leydig tumors (Kriseman et al., 2012). Similarly, Daya et al. described two cases of Sertoli-Leydig tumors in patients with cervical RMS (Daya and Scully, 1988). In the recent years, DICER1 germline variants have been detected in 60% of Sertoli-Leydig tumors (Heravi-Moussavi et al., 2012). Patient #3 completed DICER1 germline molecular genetic analysis and was found to have no pathologic variants or mutations. Genetic testing on the other patients is pending. Although DICER1 mutations are more commonly seen in cases of ERMS presenting with a positive family history, sporadic cases of ERMS have also been reported, suggesting all ERMS should have DICER1 analysis given its rarity and implication on malignancy risk in other organs (Doros et al., 2012). The exact spectrum of DICER1-related malignancies is currently expanding and remains to be fully elucidated.
Multi-disciplinary tumor board discussions are imperative in rare malignancies such as sarcoma. Additionally, cross-institutional collaboration between pediatric and adult oncologists was crucial in order to ensure that these young adults received ideal therapy to not only maximize chance of cure, but, also minimize cost of cure by avoiding hysterectomy or pelvic RT which are dictated by pediatric protocols. The extrapolation of similar fertility-sparing surgical techniques to younger adolescents deserve further exploration. Importantly, the involvement of reproductive endocrinology specialists in the management of these young women is imperative.
In conclusion, we believe that a combination of fertility-sparing surgery and chemotherapy in well-selected patients with ERMS of the cervix results in low complication rates and excellent oncologic outcomes with high likelihood of cure and spared fertility. We favor the use of radical trachelectomy in patients with large ERMS of the cervix to achieve negative resection margins and preserve fertility. A collaborative effort between pediatric oncologists and gynecologic oncologists is imperative to facilitate innovative approaches to these rare tumors in young adults. Larger studies and longer follow up are necessary to determine the long-term survival outcomes and fertility outcomes in these patients.
Conflicts of interests
The authors have no conflicts of interests to disclose.
References
- Arndt C.A., Donaldson S.S., Anderson J.R. What constitutes optimal therapy for patients with rhabdomyosarcoma of the female genital tract? Cancer. 2001;91(12):2454–2468. [PubMed] [Google Scholar]
- Bernal K.L., Fahmy L., Remmenga S. Embryonal rhabdomyosarcoma (sarcoma botryoides) of the cervix presenting as a cervical polyp treated with fertility-sparing surgery and adjuvant chemotherapy. Gynecol. Oncol. 2004;95(1):243–246. doi: 10.1016/j.ygyno.2004.06.049. [DOI] [PubMed] [Google Scholar]
- Brand E., Berek J.S., Nieberg R.K. Rhabdomyosarcoma of the uterine cervix. Sarcoma botryoides. Cancer. 1987;60(7):1552–1560. doi: 10.1002/1097-0142(19871001)60:7<1552::aid-cncr2820600724>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- Dargent D., Martin X., Sacchetoni A. Laparoscopic vaginal radical trachelectomy: a treatment to preserve the fertility of cervical carcinoma patients. Cancer. 2000;88(8):1877–1882. [PubMed] [Google Scholar]
- Daya D.A., Scully R.E. Sarcoma botryoides of the uterine cervix in young women: a clinicopathological study of 13 cases. Gynecol. Oncol. 1988;29(3):290–304. doi: 10.1016/0090-8258(88)90228-4. [DOI] [PubMed] [Google Scholar]
- Dehner L.P., Jarzembowski J.A., Hill D.A. Embryonal rhabdomyosarcoma of the uterine cervix: a report of 14 cases and a discussion of its unusual clinicopathological associations. Mod. Pathol. 2012;25(4):602–614. doi: 10.1038/modpathol.2011.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doros L., Yang J., Dehner L. DICER1 mutations in embryonal rhabdomyosarcomas from children with and without familial PPB-tumor predisposition syndrome. Pediatr. Blood Cancer. 2012;59(3):558–560. doi: 10.1002/pbc.24020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson S.E., Gerald W., Barakat R.R. Clinicopathologic features of rhabdomyosarcoma of gynecologic origin in adults. Am. J. Surg. Pathol. 2007;31(3):382–389. doi: 10.1097/01.pas.0000213352.87885.75. [DOI] [PubMed] [Google Scholar]
- Hays D.M., Shimada H., Raney R.B., Jr. Sarcomas of the vagina and uterus: the intergroup rhabdomyosarcoma study. J. Pediatr. Surg. 1985;20(6):718–724. doi: 10.1016/s0022-3468(85)80032-4. [DOI] [PubMed] [Google Scholar]
- Heravi-Moussavi A., Anglesio M.S., Cheng S.W. Recurrent somatic DICER1 mutations in nonepithelial ovarian cancers. N. Engl. J. Med. 2012;366(3):234–242. doi: 10.1056/NEJMoa1102903. [DOI] [PubMed] [Google Scholar]
- Kayton M.L., Wexler L.H., Lewin S.N. Pediatric radical abdominal trachelectomy for anaplastic embryonal rhabdomyosarcoma of the uterine cervix: an alternative to radical hysterectomy. J. Pediatr. Surg. 2009;44(4):862–867. doi: 10.1016/j.jpedsurg.2008.11.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kriseman M.L., Wang W.L., Sullinger J. Rhabdomyosarcoma of the cervix in adult women and younger patients. Gynecol. Oncol. 2012;126(3):351–356. doi: 10.1016/j.ygyno.2012.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pastore G., Peris-Bonet R., Carli M. Childhood soft tissue sarcomas incidence and survival in European children (1978–1997): report from the automated childhood cancer information system project. Eur. J. Cancer. 2006;42(13):2136–2149. doi: 10.1016/j.ejca.2006.05.016. [DOI] [PubMed] [Google Scholar]
- Raney R.B., Jr., Gehan E.A., Hays D.M. Primary chemotherapy with or without radiation therapy and/or surgery for children with localized sarcoma of the bladder, prostate, vagina, uterus, and cervix. A comparison of the results in intergroup rhabdomyosarcoma studies I and II. Cancer. 1990;66(10):2072–2081. doi: 10.1002/1097-0142(19901115)66:10<2072::aid-cncr2820661006>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]