Abstract
Context:
Caffeine is the most commonly used psychoactive legal drug in the world. Caffeine’s role in controlling pain has received less attention in the past, yet is being increasingly considered. This article briefly reviewed the literature to clarify the role of caffeine as a drug for pain control and attract investigators to this topic.
Evidence Acquisition:
The data on Caffeine as an adjuvant therapy or as a main component for pain modulation has been narratively reviewed.
Results:
Caffeine plays an important role in pain modulation through their action on adenosine receptors which are involved in nociception. The use of caffeine as adjuvant treatment was well-established in the literature and caffeine is currently available in some over the counter medications. Studies showed controversial results about the interaction between caffeine and morphine for pain relief in patients with terminal stage cancer. As a main component for pain modulation, Caffeine can be used for hypnic headache and postdural puncture headache.
Conclusions:
Caffeine has a potential role for pain modulation. Current evidence on caffeine use for migraine and terminal stage cancer is not well-established. Future studies should address the use of caffeine alone for different types of pain with dose escalation and standardization of outcome measurement.
Keywords: Caffeine, Adenosine, Role, Pain Management
1. Context
1.1. Brief History of Caffeine
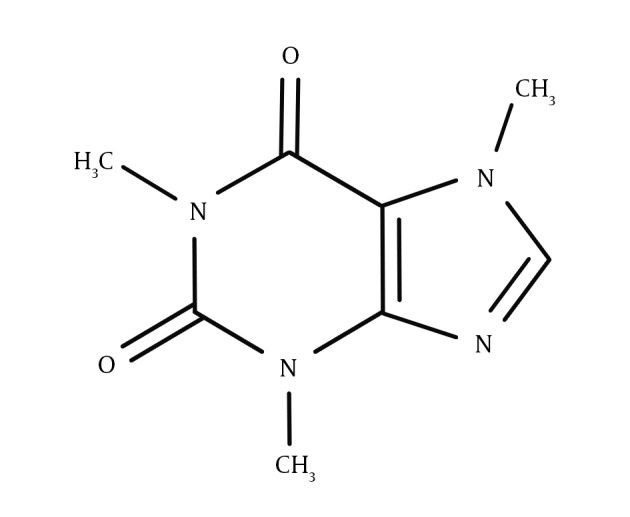
Caffeine is an alkaloid named “3,7-dihydro-1,3,7-trimethyl-1H-purine-2,6-dione”, with its chemical structure presented in Figure 1. Caffeine is a psychoactive and central nervous system stimulant of the methylxanthine class, that unlike many other psychoactives, is legal all around the world (1). Based on some historical documents, caffeine effects were noticed by a goat herder named Khaldi in southern Abyssinia in the year 850, yet it was extracted for the first time by a German chemist named “Friedlieb Ferdinand Runge” in 1819 (2, 3). Drinks containing caffeine such as tea and coffee became widespread in the 15th and 16th centuries in Arabian countries and in the 18th and 19th centuries in Europe. Nowadays, many people start their day with a cup of coffee. It seems that caffeine’s medical effects had been known long before it became a part of regular daily drinks (4). Based on the available scientific evidence, caffeine seems to have minor health risks yet its long-term benefits outweigh the potentially negative short-term health effects. On the other hand, there has not been a lot of research on caffeine, so the risks could be underestimated (5, 6). Consumption of moderate amounts of caffeine is safe for healthy non-pregnant adults. It increases energy, alertness, wakefulness, the accuracy of reactions, and the ability to concentrate and focus attention and decreases fatigue. It also enhances physical performance, short-term memory and cognitive performance (6). Caffeine’s role in controlling pain is one of the aspects, which has been less considered in the past yet is being increasingly considered. This article briefly reviewed the literature to clarify the role of caffeine as a drug for pain control and attract investigators to this topic.
Figure 1. Chemical Structure of the Caffeine Molecule.
2. Evidence Acquisition
In this review, we searched PubMed using this query “Caffeine AND Pain”. Relevant studies were identified and data on caffeine role as an adjuvant therapy and as a main component for pain modulation was narratively reviewed. Experts from emergency department at Shahid Beheshti University of Medical Sciences were consulted about relevant studies on caffeine and pain management.
2.1. Caffeine for Pain Management
Pain management has been studied with various scenarios, and it is still being investigated (7-10). Caffeine’s role in pain management is among questionable yet attractive subjects in this regard. The effects of caffeine on pain control are somewhat complex yet understanding such effects is valuable (11). Before addressing the role of caffeine in pain control, first we must be familiar with a substance called adenosine. Adenosine is an inhibitor of neuronal activity in the central nervous system (CNS) and peripheral nervous system (PNS). There are four subtypes of adenosine receptors in human bodies including A1, A2A, A2B, and A3, which are expressed in different parts of the CNS and PNS. The endogenous compound adenosine has various modulatory effects in the central and peripheral nervous systems and its receptors have been known to be involved in antinociception. Enhancing these receptors could lead to arousal, concentration and vigilance. It was discovered that activation of A1 and A2A receptors leads to antinociception in neuropathic pain, nociceptive and inflammatory models (12-14). The structure of caffeine is similar to adenosine and therefore Caffeine compete with adenosine for A2a receptors causing their inhibition. Despite this, caffeine does not alter dopamine release and therefore does not have abuse potential like other adenosine blocking agents, such as cocaine. Understanding these effects, leads to renewed interest as a novel option for pain control. Caffeine could reduce pain sensation through its effects on adenosine receptors (14-18). Caffeine seems to express its direct effect via central blocking of adenosine receptors that influence pain signaling or by blocking of peripheral adenosine receptors on sensory afferents. Antagonism of adenosine receptors, as well as inhibition of cyclooxygenase activity at some sites, may explain caffeine antinociceptive effects and its adjuvant actions (11, 14, 18-20). Interestingly, some researchers claim that genetics can influence the response of individuals to caffeine consumption (21).
3. Results
3.1. Role of Caffeine as an Adjuvant Component in Pain Management
An adjuvant component is something that is added to a medicine to enhance its effectiveness (22). Low doses of caffeine are present as an adjuvant in combination with antidepressant, acetaminophen and non-steroidal anti-inflammatory drugs in many over the counter (OTC) analgesics. Clinical studies have tested and demonstrated its adjuvant analgesic effects since decades ago (23, 24). Its inhibitory effects on A2A and A2B receptors, as well as inhibition of cyclooxygenase activity, have been raised to explain these effects (11). Some reviews found that adding low doses of caffeine to a standard dose of common analgesics enhances pain relief in a small yet important proportion of patients, compared to the analgesic alone. Following a systematic review performed by Derry et al. it was demonstrated that the mentioned effect was small yet statistically significant (22, 25). Derry et al. found 19 eligible studies (involving 7238 participants), which added 100 - 130 mg of caffeine to the main drug such as ibuprofen or paracetamol. Headache, postoperative dental pain and postpartum pain were more prevalent conditions that have been evaluated. No serious adverse event was reported in these studies and their authors claimed that adding 100 mg of caffeine or more to an analgesic could be useful (22, 25).
Despite what has been said, caffeine in combination with morphine, results in complex outcomes including inhibition or augmentation depending on the disease and the amount and route of administration (11). Researchers in South Korea ran a double-blind randomized, placebo-controlled trial to assess the efficacy of 200 mg of caffeine intravenous infusion once a day for two days as an adjuvant to opioid for pain management in patients with advanced cancer. They assigned 20 patients to the caffeine group and 21 to the placebo group. They concluded that caffeine infusion significantly reduced pain and drowsiness, yet the reduction did not reach clinical significance in patients with advanced cancer undergoing opioid therapy (26).
It should be noted that based on the current evidence, use of analgesics containing caffeine may be associated with overuse headache, physical dependence, or withdrawal symptoms upon abrupt discontinuation. Therefore, it is generally recommended to use these compounds on a temporary basis for acute pain control (24).
3.2. Role of Caffeine as the Main Component in Pain Management
Hypnic headache is a rare benign primary headache disorder, commonly affecting middle-aged patients at night. It was first described in 1988 by Raskin, and adopted by the international classification of headache disorders in 2004 within the “other primary headache” group (code 4.5) (27, 28). Based on a literature review that only consisted of case reports or smaller open case series, it seems that caffeine can be used as a first line agent for acute treatment in this type of headache, and also as a prophylactic agent as well. It was reported that caffeine, even in a cup of strong black coffee or using OTC analgesics containing caffeine, could be an effective treatment option for this type of headache. Some authors even believe that dramatic response to caffeine can be considered as pathognomonic clinical feature in diagnosis of hypnic headache. An appropriate randomized clinical trial is still needed to confirm such claims (29-33).
Postdural puncture headache (PDPH) is frequently reported as a complication of lumbar puncture and relatively common after spinal anesthesia. Postdural puncture headache pathogenesis is still doubtful, yet it has been assumed to be a consequence of CSF leakage into the epidural space. The hallmark of PDPH is decreased pain score in the supine position and its increase in the upright position (34, 35). Caffeine was first prescribed as a treatment agent for PDPH in 1949 and some investigators have orally used it at different doses, intramuscularly and intravenously (36). Most investigators recommend caffeine as a therapeutic option for treatment of this type of headache. Many studies have been conducted with different roots of administration and dosage, and varying success rates (37, 38). Yucel et al. performed a double-blind randomized clinical trial on this topic. The investigators randomly administered 1000 mL of normal saline with 500 mg of caffeine sodium benzoate or 1000 mL of normal saline during the first 90 minutes after spinal anesthesia administration. They claimed that administrating intravenous caffeine sodium benzoate during and after spinal anesthesia could minimize the rate of PDPH (39). Camann et al. also conducted a double-blind, placebo-controlled trial in this regard. They administered 300 mg of oral caffeine to forty postpartum patients with PDPH and assessed the pain scale immediately before drug administration and four and 24 hours later. They concluded that oral caffeine could be considered for pain relief in PDPH (38). By blocking adenosine receptors, caffeine increases cerebral arterial vasoconstriction, and leads to a decrease in cerebral blood inflow and brain blood volume. On the other hand, caffeine leads to augmentation of cerebrospinal fluid production by stimulating sodium-potassium pumps (35, 40). It seems that caffeine administration is a noninvasive and safe option that may prevent the use of invasive methods such as epidural blood patching, or epidural injection of NaCl 0.9% (35, 41).
Caffeine is frequently used as an adjuvant therapeutic agent for migraine headache. After new findings about migraine pathophysiology, caffeine landed a more prominent role as a treatment option. Caffeine has the ability to cross the blood-brain barrier, and act as a vasoconstrictor on cerebral vessels. In a pilot study performed in 2014, intravenous administration of 60 mg of caffeine citrate for 61 patients affected by acute migraine attack, was reported as a safe and well-tolerated abortive option at the emergency department (42).
4. Conclusions
Caffeine’s role in pain control is a subject that has received less attention in the past, yet is being increasingly considered. The current article briefly reviewed the literature to clarify the role of caffeine as a drug for pain control and attract investigators to this topic. For instance, the difference between short and long acting analgesics, when caffeine is added as an adjuvant, has not been considered. Therefore, there are many topics in this regard that willing investigators could explore.
Acknowledgments
We would like to express our special thanks to the faculty members of the emergency department of Shahid Beheshti University of Medical Sciences.
Footnotes
Authors’ Contribution:Study concept and design, Alireza Baratloo; selection of relevant studies: all authors; data synthesis and drafting manuscript: all authors; revising the manuscript: all authors; proofreading: Ahmed Negida.
Funding/Support:All authors declared that this study was accomplished without any funding or support, and the authors were responsible for all expenses.
References
- 1.Nehlig A, Daval JL, Debry G. Caffeine and the central nervous system: mechanisms of action, biochemical, metabolic and psychostimulant effects. Brain Res Brain Res Rev. 1992;17(2):139–70. doi: 10.1016/0165-0173(92)90012-b. [DOI] [PubMed] [Google Scholar]
- 2.Waldvogel SR. Caffeine--a drug with a surprise. Angew Chem Int Ed Engl. 2003;42(6):604–5. doi: 10.1002/anie.200390173. [DOI] [PubMed] [Google Scholar]
- 3.Xu J. Coffee. Journal of Agricultural & Food Information. 2003;5(3):79–86. doi: 10.1300/J108v05n03_07. [DOI] [Google Scholar]
- 4.Fredholm BB. Notes on the history of caffeine use. Handb Exp Pharmacol. 2011;(200):1–9. doi: 10.1007/978-3-642-13443-2_1. [DOI] [PubMed] [Google Scholar]
- 5.Ennis D. The Effects of Caffeine on Health: The Benefits Outweigh the Risks. USA: University of New Hampshire; 2014. Available from: http://cola.unh.edu/sites/cola.unh.edu/files/student-journals/Perspectives2014_Ennis.pdf. [Google Scholar]
- 6.Glade MJ. Caffeine-Not just a stimulant. Nutrition. 2010;26(10):932–8. doi: 10.1016/j.nut.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 7.Imani F, Rahimzadeh P, Faiz SH. Comparison of the efficacy of adding clonidine, chlorpromazine, promethazine, and midazolam to morphine pumps in postoperative pain control of addicted patients. Anesth Pain Med. 2011;1(1):10–4. doi: 10.5812/kowsar.22287523.1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sluijter ME, Imani F. Evolution and mode of action of pulsed radiofrequency. Anesth Pain Med. 2013;2(4):139–41. doi: 10.5812/aapm.10213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alimian M, Imani F, Hassani V, Rahimzadeh P, Sharifian M, Safari S. Effects of single-dose pregabalin on postoperative pain in dacryocystorhinostomy surgery. Anesth Pain Med. 2012;2(2):72–6. doi: 10.5812/aapm.4301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Imani F, Rahimzadeh P. Gabapentinoids: gabapentin and pregabalin for postoperative pain management. Anesth Pain Med. 2012;2(2):52–3. doi: 10.5812/aapm.7743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sawynok J. Methylxanthines and pain. Handb Exp Pharmacol. 2011;(200):311–29. doi: 10.1007/978-3-642-13443-2_11. [DOI] [PubMed] [Google Scholar]
- 12.Zylka MJ. Pain-relieving prospects for adenosine receptors and ectonucleotidases. Trends Mol Med. 2011;17(4):188–96. doi: 10.1016/j.molmed.2010.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zylka MJ. Needling adenosine receptors for pain relief. Nat Neurosci. 2010;13(7):783–4. doi: 10.1038/nn0710-783. [DOI] [PubMed] [Google Scholar]
- 14.Sawynok J. In: Adenosine. Adenosine and Pain. Masino S, Boison D, editors. New York: Springer; 2013. pp. 343–60. [DOI] [Google Scholar]
- 15.Sawynok J. Adenosine receptor activation and nociception. Eur J Pharmacol. 1998;347(1):1–11. doi: 10.1016/s0014-2999(97)01605-1. [DOI] [PubMed] [Google Scholar]
- 16.Latini S, Pedata F. Adenosine in the central nervous system: release mechanisms and extracellular concentrations. J Neurochem. 2001;79(3):463–84. doi: 10.1046/j.1471-4159.2001.00607.x. [DOI] [PubMed] [Google Scholar]
- 17.Rogers NL, Dinges DF. Caffeine: implications for alertness in athletes. Clin Sports Med. 2005;24(2):e1–13. doi: 10.1016/j.csm.2004.12.012. [DOI] [PubMed] [Google Scholar]
- 18.Sollevi A. Adenosine for pain control. Acta Anaesthesiol Scand Suppl. 1997;110:135–6. doi: 10.1111/j.1399-6576.1997.tb05532.x. [DOI] [PubMed] [Google Scholar]
- 19.Astorino TA, Terzi MN, Roberson DW, Burnett TR. Effect of caffeine intake on pain perception during high-intensity exercise. Int J Sport Nutr Exerc Metab. 2011;21(1):27–32. doi: 10.1123/ijsnem.21.1.27. [DOI] [PubMed] [Google Scholar]
- 20.Benowitz NL. Clinical pharmacology of caffeine. Annu Rev Med. 1990;41:277–88. doi: 10.1146/annurev.me.41.020190.001425. [DOI] [PubMed] [Google Scholar]
- 21.Carvey CE, Thompson LA, Mahoney CR. In: Sleep Deprivation, Stimulant Medications, and Cognition. Caffeine: mechanism of action, genetics, and behavioral studies conducted in task. Wesensten NJ, editor. US: Cambridge University Press; 2012. p. 93. [Google Scholar]
- 22.Derry CJ, Derry S, Moore RA. Caffeine as an analgesic adjuvant for acute pain in adults. The Cochrane Library. 2014. doi: 10.1002/14651858.cd009281.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Laska EM, Sunshine A, Mueller F, Elvers WB, Siegel C, Rubin A. Caffeine as an analgesic adjuvant. JAMA. 1984;251(13):1711–8. [PubMed] [Google Scholar]
- 24.Nikolajsen L, Haroutiunian S. [Caffeine as adjuvant analgeticum for treating acute pain]. Ugeskr Laeger. 2013;175(42):2486–8. [PubMed] [Google Scholar]
- 25.Derry CJ, Derry S, Moore RA. Caffeine as an analgesic adjuvant for acute pain in adults. Cochrane Database Syst Rev. 2012;3:Cd009281. doi: 10.1002/14651858.CD009281.pub2. [DOI] [PubMed] [Google Scholar]
- 26.Suh SY, Choi YS, Oh SC, Kim YS, Cho K, Bae WK, et al. Caffeine as an adjuvant therapy to opioids in cancer pain: a randomized, double-blind, placebo-controlled trial. J Pain Symptom Manage. 2013;46(4):474–82. doi: 10.1016/j.jpainsymman.2012.10.232. [DOI] [PubMed] [Google Scholar]
- 27.Raskin NH. The hypnic headache syndrome. Headache. 1988;28(8):534–6. doi: 10.1111/j.1526-4610.1988.hed2808534.x. [DOI] [PubMed] [Google Scholar]
- 28.Lanteri-Minet M, Donnet A. Hypnic headache. Curr Pain Headache Rep. 2010;14(4):309–15. doi: 10.1007/s11916-010-0124-8. [DOI] [PubMed] [Google Scholar]
- 29.Lanteri-Minet M. Hypnic headache. Headache. 2014;54(9):1556–9. doi: 10.1111/head.12447. [DOI] [PubMed] [Google Scholar]
- 30.Holle D, Obermann M. Hypnic headache and caffeine. Expert Rev Neurother. 2012;12(9):1125–32. doi: 10.1586/ern.12.100. [DOI] [PubMed] [Google Scholar]
- 31.Evers S, Goadsby PJ. Hypnic headache: clinical features, pathophysiology, and treatment. Neurology. 2003;60(6):905–9. doi: 10.1212/01.wnl.0000046582.21771.9c. [DOI] [PubMed] [Google Scholar]
- 32.Liang JF, Wang SJ. Hypnic headache: a review of clinical features, therapeutic options and outcomes. Cephalalgia. 2014;34(10):795–805. doi: 10.1177/0333102414537914. [DOI] [PubMed] [Google Scholar]
- 33.Dodick DW, Mosek AC, Campbell JK. The hypnic ("alarm clock") headache syndrome. Cephalalgia. 1998;18(3):152–6. doi: 10.1046/j.1468-2982.1998.1803152.x. [DOI] [PubMed] [Google Scholar]
- 34.Bezov D, Lipton RB, Ashina S. Post-dural puncture headache: part I diagnosis, epidemiology, etiology, and pathophysiology. Headache. 2010;50(7):1144–52. doi: 10.1111/j.1526-4610.2010.01699.x. [DOI] [PubMed] [Google Scholar]
- 35.Ragab A, Facharzt KN. Caffeine, Is it effective for prevention of postdural puncture headache in young adult patients? Egypt J Anaesthesia. 2014;30(2):181–6. doi: 10.1016/j.egja.2013.11.005. [DOI] [Google Scholar]
- 36.Halker RB, Demaerschalk BM, Wellik KE, Wingerchuk DM, Rubin DI, Crum BA, et al. Caffeine for the prevention and treatment of postdural puncture headache: debunking the myth. Neurologist. 2007;13(5):323–7. doi: 10.1097/NRL.0b013e318145480f. [DOI] [PubMed] [Google Scholar]
- 37.Jarvis AP, Greenawalt JW, Fagraeus L. Intravenous caffeine for postdural puncture headache. Anesth Analg. 1986;65(3):316–7. [PubMed] [Google Scholar]
- 38.Camann WR, Murray RS, Mushlin PS, Lambert DH. Effects of oral caffeine on postdural puncture headache. A double-blind, placebo-controlled trial. Anesth Analg. 1990;70(2):181–4. doi: 10.1213/00000539-199002000-00009. [DOI] [PubMed] [Google Scholar]
- 39.Yucel A, Ozyalcin S, Talu GK, Yucel EC, Erdine S. Intravenous administration of caffeine sodium benzoate for postdural puncture headache. Reg Anesth Pain Med. 1999;24(1):51–4. [PubMed] [Google Scholar]
- 40.Straube A, Neudert C, Glas M, Bruning R, Padovan CS. [The so-called spontaneous low CSF pressure pressure syndrome. Case results indicating a disturbance in CSF/blood volume regulation]. Nervenarzt. 2004;75(12):1194–9. doi: 10.1007/s00115-004-1752-1. [DOI] [PubMed] [Google Scholar]
- 41.Lin W, Geiderman J. Myth: fluids, bed rest, and caffeine are effective in preventing and treating patients with post-lumbar puncture headache. West J Med. 2002;176(1):69–70. doi: 10.1136/ewjm.176.1.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Baratloo A, Negida A, El Ashal G. Intravenous Caffeine for the Treatment of Acute Migraine: A Pilot Study. J Caffeine Res. 2015;5(3):125–9. doi: 10.1089/jcr.2015.0004.. [DOI] [Google Scholar]


