Abstract
Background
Postoperative pain from open reduction and internal fixation of mandibular fracture is a serious issue. Amantadine is an N-methyl-D-aspartic acid or N-methyl-D-aspartate (NMDA) receptor antagonist that can be effective against postoperative pain.
Objectives
The present study examined the efficacy of amantadine in alleviating the postoperative pain of mandibular fracture surgery.
Patients and Methods
In this double-blind study, 60 patients (ASA physical status I–II) were randomly divided into two groups. The mean ages of the participants were 31.2 ± 13.1 years and 32.3 ± 18.1 years, respectively. The male/female ratios were 24/6 and 26/4, respectively, in the case and control groups. Randomization was based on a single sequence of random assignments using computer-generated random numbers. Group I was given oral amantadine 100 mg 1 hour before surgery, and group II received a placebo at the identical time. Through PCA pumps, patients received a bolus dose of morphine at 0.02 mg/kg body weight, to a maximum of 1.5 mg. PCA pumps were set at 6 minutes lockout intervals and a maximum dose of 0.15 mg/kg/h, to a maximum of 10 mg/h. Pain was assessed using a visual analog scale (VAS) at 0, 2, 4, 6, 12, and 24 hours and 1, 2, 3, 4, 5, and 6 months after surgery. The amounts of analgesic consumed were recorded for the first 24 hours, and for 6 months after surgery.
Results
There were no significant differences between the two groups with respect to age, gender, nausea and vomiting, sleep quality, blood pressure, and heart rate. No significant differences were observed between the two groups in pain scores (P = 0.39) and analgesic consumption (P = 0.78).
Conclusions
The results suggest that a single dose of preoperative oral amantadine did not reduce acute or chronic postoperative pain, nor analgesic consumption.
Keywords: Anesthesia and Analgesia, Amantadine, Maxillofacial Injuries
1. Background
Current evidence shows that inadequate management of acute pain can have lasting effects. Brief harmful stimulation and frank injury may have strong effects on the central nervous system, extending the injury. Intraoperative and postoperative pain cause the firing of nerve impulses entering the spinal cord. Prolonged postoperative pain is a consequence of the release of excitatory amino acids and neuropeptides from small-diameter afferent C-fibers in spinal dorsal horn neurons, which induce a state of hyperexcitability. This situation, “pain memory,” is referred to as central sensitization and may contribute to persistent pain (1-3).
Modern concepts of postoperative pain therapy focus on influencing specific pain receptors via a multimodal pharmacologic intervention by receptor modulation before the pain stimulus develops. One solution for acute postoperative pain is utilizing compounds pre-emptively, alleviating pain by reducing sensitivity and lowering the chance of acute postoperative pain becoming chronic pain. Previous studies have investigated the effectiveness of different medications, such as gabapentinoids, in controlling acute postoperative pain, including after major operations. Some authors have suggested that administering these compounds preemptively could considerably reduce pain intensity after an operation, and could lower the required dose of opioids. However, some studies point out that these agents lack sufficient efficacy after major operations, with their effects limited to minor operations (4-6).
The N-methyl-D-aspartate (NMDA) receptor plays an important role in the process of central sensitization. Renewed sensitization is related to the role of NMDA receptors in central sensitization, and in opioid-induced hyperalgesia and acute opioid tolerance (7, 8). Thus, excitatory amino acids such as NMDA have provoked interest in receptor antagonists for clinical use (1, 9, 10).
Dextromethorphan and ketamine have been studied discriminately against clinically available substances that antagonize the NMDA receptor-ion channel complex (11-13), such as amantadine (1-aminoadamantane). Amantadine has been clinically used for more than 30 years as an antiviral drug, for dementia, and in the treatment of Parkinson’s disease and spasticity. It is a non-competitive NMDA receptor antagonist (14, 15), and compared to ketamine, it is well-tolerated with fewer side effects (mainly dizziness, sedation, and dry mouth). For these reasons, we chose amantadine for use in this study.
Amantadine’s formulation permits the oral route for drug delivery, as well as the IV route. The side-effects profile of amantadine via all routes seems not to be harmful in appropriate dosages. IV-administered amantadine in two clinical reports showed less chronic neuropathic pain and decreased neuropathic pain in cancer patients compared to a control group (16, 17). Thus, amantadine may be useful for analgesia by preventing acute opioid-induced hyperalgesia and postsurgical central sensitization tolerance.
The present study examines whether the advantages of NMDA receptor inhibition described for neuropathic pain can be transferred to surgical patients. This double-blind, randomized, clinical trial study investigated the opioid-sparing and postoperative analgesic effects of amantadine given orally during the preoperative period in patients undergoing mandibular fracture surgery.
2. Objectives
The aim of this study was to evaluate the effects of 100 mg of oral amantadine, administered before mandibular fracture surgery, on pain intensity measured with a visual analog scale (VAS).
3. Patients and Methods
The steps of the current study were designed and performed based on the consolidated standards of reporting trials (CONSORT) guidelines. Approval was obtained from the local ethics committee. Patients who did not respond to the invitation or who declined to participate were not assessed. After excluding other participants who were not eligible for the study, 60 adult patients of both genders and in different age groups (20 - 60 years) with an ASA physical status of 1 - 2, who were undergoing open reduction and internal fixation (ORIF) of a recent mandibular unilateral body fracture, were enrolled. There was homogenous disease severity and disease duration in this placebo-controlled study. All operations were performed by the same surgeon, and the patients were extubated at the end of the operation. We used simple randomization to allocate subjects to each group due to homogenous disease severity. Randomization based on a single sequence of random assignments was performed using computer-generated random numbers.
Written informed consent was obtained from each participant in accordance with the code of ethics of the world medical association (declaration of Helsinki) for experiments involving humans. To avoid bias, subject allocation was concealed to the two groups. The exclusion criteria were preoperative opioid use or dependency, peptic ulcer disease, hepatic or renal dysfunction, psychological disease, allergy to amide local anesthetics and narcotics, epileptic seizure, closed-angle glaucoma, chronic heart failure, a drop in blood pressure upon standing, kidney disease, eczema, visible water retention, a malignant pigmented mole or tumor, mental disorder with loss of normal personality and reality, mental disturbance, suicidal thoughts, and alcoholism. No subjects in either arm of the study dropped out due to lack of benefit. Patients in group I (the amantadine group) received a 100 mg dose of amantadine (Ammorel® 100 mg capsules) one hour before surgery. The control patients in group II took placebo capsules (red gelatin capsules filled with lactose powder) one hour before surgery. The study was double-blinded, so that all patients and personnel involved in patient care, data collection, scoring, and entry were unaware of the group to which each patient had been assigned.
All patients were given general anesthesia after the establishment of mandatory monitoring (pulse oximetry, electrocardiography, and noninvasive blood pressure monitoring [HEYER medical AG Pasithec]). The same general anesthetic technique was used for all patients. After pre-oxygenation with 100% O2, the patients received fentanyl 1 µg/kg (50 mcg/mL Mylan S.A.S., Haupt Pharma Livron, France), midazolam 0.04 mg/kg (5 mg/mL amp, Aburaihan Pharmaceutical Co., Tehran, Iran), propofol 2 mg/kg (propofol-Lipuro® 200 mg/20 mL vial), and cisatracurium besylate 0.5 mg/kg (2 mg/mL, 5 mL amp). All patients were intubated, and 0.1 mg/kg/min of IV propofol was used for the maintenance of anesthesia.
Postoperative pain management was performed with analgesic drugs if needed, and the duration of analgesia was recorded. All patients received a bolus dose of morphine sulfate (10 mg/mL amp, Darou Pakhsh, Iran) at a dose of 0.02 mg/kg body weight, to a maximum of 1.5 mg, through a PCA pump (BioMedix Medical). The PCA pumps were set at 6 minutes lockout intervals at a maximum dose of 0.15 mg/kg/h, to a maximum of 10 mg/h. The VAS was used to estimate the patients’ degree of pain at 0, 2, 4, 6, 12, and 24 hours, and then at 1, 2, 3, 4, 5, and 6 months after surgery. The application of the VAS was explained to the patients before the operation. If necessary, pain management at 1, 2, 3, 4, 5, and 6 months after surgery was achieved with the analgesic ibuprofen 400 mg (Gelofen® 400 mg pearl, Dana Corporation). The patients were instructed to take the ibuprofen when they felt it was necessary, with a maximum dose of 3.2 g per day, split into four doses. The pittsburgh sleep quality index (PSQT) was used to measure sleep quality.
The demographic data were analyzed using SPSS version 21 for statistical analysis. For comparison of groups, the independent t-test was used for comparison of quantitative demographic data, VAS scores between the study groups, and the amount of analgesic drugs administrated. The chi-square test was used for comparison of qualitative demographic data. The sample size was calculated based on studies with similar methodologies. Based on the results of Alimian et al. (6), we used the mean and standard deviation of VAS scores during recovery time (mean 6.6 ± 1.5 vs. 5.1) to calculate the sample size. According to the CONSORT flowchart, we considered the type I error rate to be alpha = 0.05 and the type II error rate to be beta = 0.05. The calculated sample size was 52 (26 per group). Then, according to the CONSORT flowchart, we added 15% to the result to compensate for possible dropouts, and the required sample size was finally calculated to be 60 (30 per group) (6). The patients’ VAS and PSQT scores were assessed by the physician on duty. P values of < 0.05 were considered statistically significant.
4. Results
In this study, 60 patients were evaluated, and the blinding process was successful. The data on demographics, vomiting and nausea, sleep quality, blood pressure, and heart rate are presented in Table 1. There were no significant differences between the two groups with respect to age, gender, nausea and vomiting, sleep quality, blood pressure, and heart rate. The length of surgery also did not differ significantly between the case and control groups (42.8 - 47.6 and 41.9 - 47.4 minutes, respectively; 95% CI for the mean, P = 0.7).
Table 1. Statistical Evaluation of Demographic Parameters (N = 30).
| Variable | Amantadine Group (I) | Control Group (II) | P Value |
|---|---|---|---|
| Age, y | 31.2 ± 13.1 | 32.3 ± 18.1 | 0.78 |
| Gender | 0.73 | ||
| Male | 24 | 26 | |
| Female | 6 | 4 | |
| Vomiting and nausea | 1 | ||
| No | 28 | 28 | |
| Yes | 2 | 2 | |
| Sleep quality | 0.18 | ||
| Good | 20 | 25 | |
| Moderate | 7 | 2 | |
| Bad | 3 | 3 | |
| Systolic blood pressure, mmHg a | 125.8 ± 21 | 123 ± 16.1 | 0.55 |
| Diastolic blood pressure, mmHg a | 75.2 ± 12.7 | 73.9 ± 13 | 0.69 |
| Heart rate a | 76.6 ± 14.4 | 78.1 ± 16.3 | 0.70 |
| Systolic blood pressure, mmHg b | 124.9 ± 20 | 123 ± 15.9 | 0.54 |
| Diastolic blood pressure, mmHg b | 74.8 ± 13 | 73.1 ± 13.1 | 0.7 |
| Heart rate b | 74.6 ± 14.3 | 77.1 ± 16.1 | 0.68 |
apostoperative.
bperioperative.
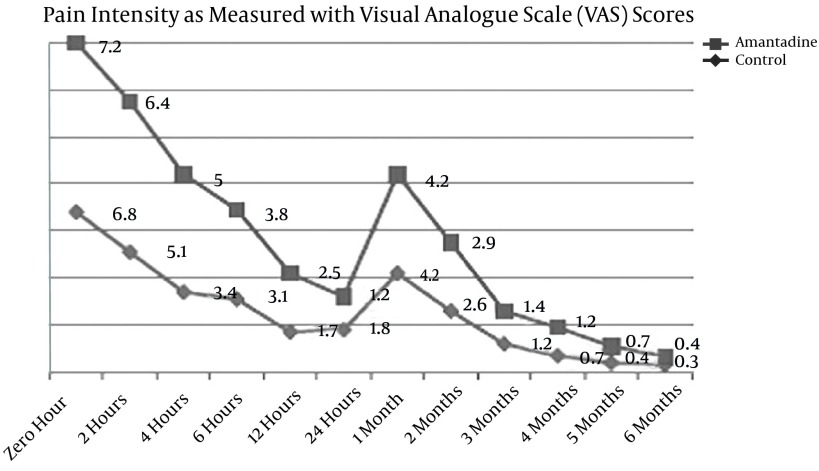
VAS scores at 0, 2, 4, 6, 12, and 24 hours and at 1, 2, 3, 4, 5, and 6 months after surgery are presented in Table 2 and Figure 1. No significant differences were observed between the two groups at all time-points except for 4 hours after surgery.
Table 2. VAS Statistical Comparison Between the Amantadine and Control Groups (N = 30).
| Variable | Amantadine Group (I) | Control Group (II) | P Value |
|---|---|---|---|
| VAS at 0 | 7.20 ± 2.83 | 6.80 ± 2.88 | 0.59 |
| VAS after 2 hours | 6.63 ± 2.63 | 5.10 ± 2.83 | 0.06 |
| VAS after 4 hours | 5.03 ± 2.87 | 3.43 ± 2.68 | 0.03 |
| VAS after 6 hours | 3.86 ± 2.87 | 3.13 ±2.60 | 0.30 |
| VAS after 12 hours | 2.53 ± 2.68 | 1.76 ± 2.28 | 0.32 |
| VAS after 24 hours | 1.43 ± 1.92 | 1.81 ± 2.84 | 0.54 |
| VAS after 1 month | 4.23 ± 3.37 | 4.20 ±2.61 | 0.96 |
| VAS after 2 months | 2.96 ± 3.36 | 2.60 ± 2.66 | 0.64 |
| VAS after 3 months | 1.40 ± 2.79 | 1.20± 2.13 | 0.75 |
| VAS after 4 months | 1.20 ± 2.65 | 0.70 ± 1.84 | 0.40 |
| VAS after 5 months | 0.70 ± 2 | 0.46 ± 1.45 | 0.60 |
| VAS after 6 months | 0.43 ± 1.40 | 0.30 ± 0.95 | 0.66 |
Figure 1. Pain Intensity Based on VAS Scores.
No statistically significant differences were noted at all time-points except at 4 hours after surgery.
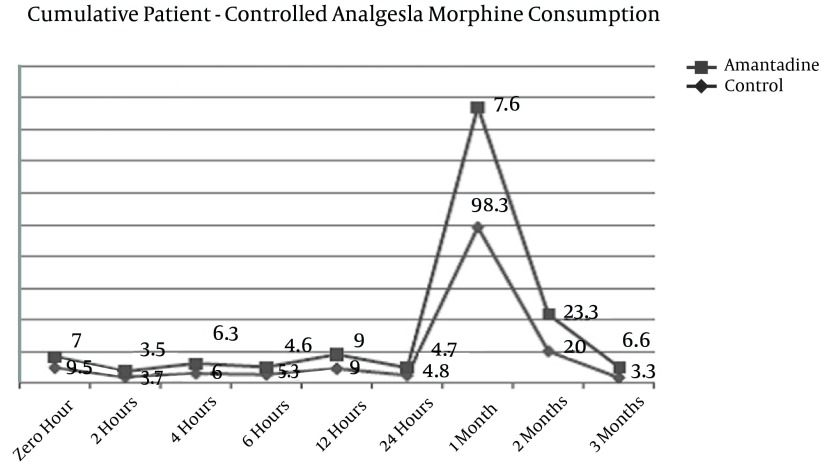
The duration and type of analgesia used for pain control in the first 24 hours and at 6 months after surgery are presented in Table 3 and Figure 2. There were no significant differences between the two groups with respect to duration and type of analgesia used for pain control in first 24 hours and at 6 months after surgery.
Table 3. Statistical Comparison of Morphine Use and Analgesia Duration Between the Two Groups (N = 30).
| Variable | Amantadine Group (I) | Control Group (II) | P Value |
|---|---|---|---|
| Analgesia duration, min | 24.33 ± 35.83 | 25.33 ± 17.80 | 0.89 |
| Morphine use (mg) in first 24 hours after surgery | 38.43 ± 14.35 | 35.41 ± 12.61 | 0.39 |
| Morphine use (mg) in first six months after surgery | 121.66 ± 100.58 | 106 ± 135.35 | 0.61 |
Figure 2. Cumulative Patient-Controlled Analgesia Morphine Consumption.
No statistically significant differences were noted at all time-points.
5. Discussion
The present study examined whether the preemptive use of an NMDA receptor inhibitor can be effective in relieving chronic and acute postoperative pain in patients undergoing ORIF for posttraumatic mandibular fractures. There are several NMDA receptor antagonists available, such as amantadine, methadone, ketamine, and dextromethorphan (18), with different levels of activity against the NMDA receptor. Ketamine is a strong NMDA antagonist, while the others are weaker NMDA receptor blockers (19). Affinity for the NMDA receptor determines the frequency and severity of side effects. The adverse effects of NMDA antagonists in adults are mainly central nervous system (CNS) side effects, including lightheadedness, hallucinations, dizziness, headache, fatigue, nightmares, sensory changes, and an out-of-body sensation. Ketamine is a strong NMDA antagonist that is less tolerable than the others due to a higher incidence of side effects, in particular hallucinations and a dissociative mental state (20). Amantadine in comparison to ketamine is well-tolerated, with a lower rate of side effects (mainly dizziness, sedation, and dry mouth). For these reasons, we used amantadine in this study.
A double-blinded, randomized, placebo-controlled trial was conducted on 15 cancer patients with surgical neuropathic pain (17). One week apart from each other, in a randomized order, the patients received a 200 mg infusion of placebo or amantadine. During and after treatment, evoked and spontaneous pain was measured and compared to 48 hours before. On average, there was an 85% pain reduction with amantadine versus a 45% reduction with the placebo at the end of the infusion (P = 0.009) (17). However, our study focused on acute postoperative pain, which might differ from other pain states, such as inflammatory or neuropathic pain. Also, in 2006, Aoki et al. reported preemptive analgesic effects of noncompetitive NMDA antagonists in patients undergoing tonsillectomy (21). In contrast to our study, in which preexisting pain could affect the success of preemptive analgesic interventions, Aoki et al.’s patients did not suffer from preexisting pain. Chau-In et al. reported a weaker, though still measurable, effect in a clinical trial compared with low-dose non-competitive NMDA antagonists (22). Chau-In et al. used stronger NMDA receptor antagonists in comparison to amantadine, which has relatively decreased NMDA-receptor-blocking potency (22). The effects of perioperative oral amantadine on analgesic consumption and postoperative pain in patients undergoing radical prostatectomy were evaluated by Snijdelaar et al. Less intense mechanical sensitivity around the surgical wound, a reduced incidence of bladder spasm pain, and lower postoperative morphine requirements were associated with perioperative oral amantadine (23). However, in our study, the sparing effects of amantadine may have been offset in the study group due to increased opioid requirements in younger versus older patients, whereas in the studies by Snijdelaar et al. (23) and Gagliese et al. (24), age diversity was much less significant.
Fukui et al. performed an amantadine study on 19 patients who had failed to respond to conventional treatments for neuropathic pain, including antidepressants, anticonvulsants, and nerve blocks. The patients took oral amantadine 100 mg/day for one week, then titrated to 200 mg/day. The results were positive in only two of the 19 patients (10.5%). Adverse effects, including dry mouth, hallucinations, drowsiness, irritation, excitation, dizziness, dyskinesia, and loss of hair, were experienced in 52.6% of the patients (25); these results are in line with our study. The previous study focused on neuropathic pain, whereas our study investigated acute postoperative pain. The results of that study are in contrast with Eisenberg et al., who also investigated neuropathic pain, using the IV route instead of the oral route, which can explain the difference in results (17). In a review by Azari et al. based on eligible studies, no improved postoperative analgesic effects were demonstrated in a comparable setting (26). Elia et al. obtained the same results in a systematic review, finding no preemptive analgesic effect with non-competitive NMDA antagonists (27), which are both in line with our study. Despite investigating stronger NMDA antagonists, these studies demonstrate the unclear effectiveness of preoperative administration of NMDA antagonists. A large variety of different ketamine regimens and surgical settings were included in these systematic reviews, which makes the results of our study incompatible for a comparison. Gottschalk et al. also showed that in women undergoing abdominal hysterectomy, a single dose of 200 mg amantadine intravenously administered 30 minutes before induction of general anesthesia resulted in no postoperative opioid-sparing effect (28). However, that study used a smaller power to investigate the effect of amantadine in comparison to ours.
The current placebo-controlled study failed to show improved analgesia when the NMDA-receptor antagonist (oral amantadine) was administered before surgery in patients undergoing ORIF for mandibular fractures. Although several studies have suggested analgesic effects of amantadine in neuropathic pain, acute postoperative pain might differ from other pain states, such as inflammatory or neuropathic pain. Our results are in line with data obtained by other investigators, who also could find no improvement in postoperative analgesia by the pre-administration of noncompetitive NMDA antagonists (26, 29-31).
Several factors may lead to this diversity of results. For example, preexisting pain can affect the success of preemptive analgesic interventions (32). In addition, some papers have suggested that visceral pain might not be responsive to the concept of early (i.e. before tissue injury) NMDA receptor inhibition (33). Also, mixed results are shown in clinical trials. With few exceptions, little has been published describing the use of amantadine for its analgesic properties (23, 29, 34), and these publications relate to the treatment of chronic neuropathic pain rather than acute postoperative pain (25, 34, 35). However, the sparing effects of amantadine may have been offset in the amantadine group because of increased opioid requirements in younger versus older patients; the amantadine patients were younger than the patients in the control group (24, 36), leading to the absence of a difference in outcome between the two groups. In addition, the amantadine group had significantly more intense preoperative pain on the day of the operation than did the patients in the control group, and increased preoperative pain intensity could mask the effects of amantadine. Perhaps because central sensitization is established before surgery, the efficacy of amantadine may be reduced in much the same way that presurgical pain has been found to be less responsive to preoperative treatment with analgesics (32).
In addition, various other factors, such as wound infiltration with local anesthetics and the intraoperative administration of opioids and NSAIDs, influenced the results of the previous studies and the present one that investigated the analgesic effects of NMDA receptor blockade.
Multiple doses versus a single dose might assist in the prevention and therapy of postoperative pain by greater NMDA receptor blockade, and further explanations of the ineffectiveness of amantadine treatment in this study are required.
One of the limitations of this study was that higher doses of amantadine and the IV administration of the drug were not evaluated. In comparison to other NMDA receptor antagonists, such as ketamine, the relatively decreased potency of amantadine in NMDA receptor blocking suggests that a larger dose of amantadine would be required and that it must be continued after surgery to obtain significant effects.
In conclusion, a single dose of amantadine 100 mg preoperatively did not significantly reduce postoperative pain or opioid usage compared to the placebo group. Further studies on noncompetitive NMDA antagonists with more intense affinity for the specific receptor, or a larger dose or earlier application of the drug, are needed. NMDA receptor antagonists with few side effects, such as amantadine, that can be used in the clinical setting of fast-tracking general anesthesia and that might be effective at reducing analgesic requirements and postoperative pain intensity, are yet to be identified.
Acknowledgments
This investigation was based on a thesis submitted by the third author to the Tabriz University of Medical Sciences, Tabriz, Iran.
Footnotes
Authors’ Contribution:Javad Yazdani: study concept and design; administrative, technical, and material support; Davood Aghamohamadi: study concept and design, study supervision; Masoomeh Amani: acquisition of data, analysis and interpretation of data; Ali Hossein Mesgarzadeh: analysis and interpretation of data; Davood Maghbooli Asl: administrative, technical, and material support; Tannaz Pourlak: acquisition of data.
References
- 1.Bouwense SA, Olesen SS, Drewes AM, Frokjaer JB, van Goor H, Wilder-Smith OH. Is altered central pain processing related to disease stage in chronic pancreatitis patients with pain? An exploratory study. PLoS One. 2013;8(2):e35900. doi: 10.1371/journal.pone.0055460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Taghipour Anvari Z, Afshar-Fereydouniyan N, Imani F, Sakhaei M, Alijani B, Mohseni M. Effect of clonidine premedication on blood loss in spine surgery. Anesth Pain Med. 2012;1(4):252–6. doi: 10.5812/aapm.2197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Imani F. Postoperative pain management. Anesth Pain Med. 2011;1(1):6–7. doi: 10.5812/kowsar.22287523.1810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alimian M, Imani F, Hassani V, Rahimzadeh P, Sharifian M, Safari S. Effects of single-dose pregabalin on postoperative pain in dacryocystorhinostomy surgery. Anesth Pain Med. 2012;2(2):72–6. doi: 10.5812/aapm.4301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Imani F, Rahimzadeh P. Gabapentinoids: gabapentin and pregabalin for postoperative pain management. Anesth Pain Med. 2012;2(2):52–3. doi: 10.5812/aapm.7743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alimian M, Imani F, Faiz SH, Pournajafian A, Navadegi SF, Safari S. Effect of oral pregabalin premedication on post-operative pain in laparoscopic gastric bypass surgery. Anesth Pain Med. 2012;2(1):12–6. doi: 10.5812/aapm.4300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Miranda A, Mickle A, Bruckert M, Kannampalli P, Banerjee B, Sengupta JN. NMDA receptor mediates chronic visceral pain induced by neonatal noxious somatic stimulation. Eur J Pharmacol. 2014;744:28–35. doi: 10.1016/j.ejphar.2014.09.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xu T, Zhong W, Zhao J, Ma X, Zhao D, Jiang W, et al. Does modulation of spinal N-methyl-D-aspartic acid receptor by pre-activation accelerate the development of morphine tolerance? Med Hypotheses. 2015;84(2):91–3. doi: 10.1016/j.mehy.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 9.Bessiere B, Laboureyras E, Ben Boujema M, Laulin JP, Simonnet G. A high-dose of fentanyl induced delayed anxiety-like behavior in rats. Prevention by a NMDA receptor antagonist and nitrous oxide (N(2)O). Pharmacol Biochem Behav. 2012;102(4):562–8. doi: 10.1016/j.pbb.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 10.Salas S, Frasca M, Planchet-Barraud B, Burucoa B, Pascal M, Lapiana JM, et al. Ketamine analgesic effect by continuous intravenous infusion in refractory cancer pain: considerations about the clinical research in palliative care. J Palliat Med. 2012;15(3):287–93. doi: 10.1089/jpm.2011.0353. [DOI] [PubMed] [Google Scholar]
- 11.Ahern TL, Herring AA, Stone MB, Frazee BW. Effective analgesia with low-dose ketamine and reduced dose hydromorphone in ED patients with severe pain. Am J Emerg Med. 2013;31(5):847–51. doi: 10.1016/j.ajem.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 12.Bornemann-Cimenti H, Lederer AJ, Wejbora M, Michaeli K, Kern-Pirsch C, Archan S, et al. Preoperative pregabalin administration significantly reduces postoperative opioid consumption and mechanical hyperalgesia after transperitoneal nephrectomy. Br J Anaesth. 2012;108(5):845–9. doi: 10.1093/bja/aes004. [DOI] [PubMed] [Google Scholar]
- 13.Santoso JT, Ulm MA, Jennings PW, Wan JY. Multimodal pain control is associated with reduced hospital stay following open abdominal hysterectomy. Eur J Obstet Gynecol Reprod Biol. 2014;183:48–51. doi: 10.1016/j.ejogrb.2014.10.007. [DOI] [PubMed] [Google Scholar]
- 14.Olivares D, Deshpande VK, Shi Y, Lahiri DK, Greig NH, Rogers JT, et al. N-methyl D-aspartate (NMDA) receptor antagonists and memantine treatment for Alzheimer's disease, vascular dementia and Parkinson's disease. Curr Alzheimer Res. 2012;9(6):746–58. doi: 10.2174/156720512801322564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Geldenhuys WJ, Van der Schyf CJ. Rationally designed multi-targeted agents against neurodegenerative diseases. Curr Med Chem. 2013;20(13):1662–72. doi: 10.2174/09298673113209990112. [DOI] [PubMed] [Google Scholar]
- 16.Smith EM, Bridges CM, Kanzawa G, Knoerl R, Kelly J, Berezovsky A, et al. Cancer treatment-related neuropathic pain syndromes--epidemiology and treatment: an update. Curr Pain Headache Rep. 2014;18(11):459. doi: 10.1007/s11916-014-0459-7. [DOI] [PubMed] [Google Scholar]
- 17.Eisenberg E, Kleiser A, Dortort A, Haim T, Yarnitsky D. The NMDA (N-methyl-D-aspartate) receptor antagonist memantine in the treatment of postherpetic neuralgia: a double-blind, placebo-controlled study. Eur J Pain. 1998;2(4):321–7. doi: 10.1016/s1090-3801(98)90030-1. [DOI] [PubMed] [Google Scholar]
- 18.Lipton SA. Failures and successes of NMDA receptor antagonists: molecular basis for the use of open-channel blockers like memantine in the treatment of acute and chronic neurologic insults. NeuroRx. 2004;1(1):101–10. doi: 10.1602/neurorx.1.1.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.American Chronic Pain Association I . Resource Guide To Chronic Pain Medication and Treatment. ACPA; 2015. 2 p. [Google Scholar]
- 20.Niesters M, Martini C, Dahan A. Ketamine for chronic pain: risks and benefits. 2 pBr J Clin Pharmacol. 2014;77(2):357–67. doi: 10.1111/bcp.12094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aoki T, Yamaguchi H, Naito H, Shiiki K, Ota Y, Kaneko A. Dextromethorphan premedication reduced postoperative analgesic consumption in patients after oral surgery. 2 pOral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102(5):591–5. doi: 10.1016/j.tripleo.2005.10.060. [DOI] [PubMed] [Google Scholar]
- 22.Chau-In W, Sukmuan B, Ngamsangsirisapt K, Jirarareungsak W. Efficacy of pre- and postoperative oral dextromethorphan for reduction of intra- and 24-hour postoperative morphine consumption for transabdominal hysterectomy. 2 pPain Med. 2007;8(5):462–7. doi: 10.1111/j.1526-4637.2006.00226.x. [DOI] [PubMed] [Google Scholar]
- 23.Snijdelaar DG, Koren G, Katz J. Effects of perioperative oral amantadine on postoperative pain and morphine consumption in patients after radical prostatectomy: results of a preliminary study. 2 pAnesthesiology. 2004;100(1):134–41. doi: 10.1097/00000542-200401000-00022. [DOI] [PubMed] [Google Scholar]
- 24.Gagliese L, Weizblit N, Ellis W, Chan VW. The measurement of postoperative pain: a comparison of intensity scales in younger and older surgical patients. 2 pPain. 2005;117(3):412–20. doi: 10.1016/j.pain.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 25.Fukui S, Komoda Y, Nosaka S. Clinical application of amantadine, an NMDA antagonist, for neuropathic pain. 2 pJ Anesth. 2001;15(3):179–81. doi: 10.1007/s005400170025. [DOI] [PubMed] [Google Scholar]
- 26.Azari L, Santoso JT, Osborne SE. Optimal pain management in total abdominal hysterectomy. 2 pObstet Gynecol Surv. 2013;68(3):215–27. doi: 10.1097/OGX.0b013e31827f5119. [DOI] [PubMed] [Google Scholar]
- 27.Elia N, Tramer MR. Ketamine and postoperative pain--a quantitative systematic review of randomised trials. 2 pPain. 2005;113(1-2):61–70. doi: 10.1016/j.pain.2004.09.036. [DOI] [PubMed] [Google Scholar]
- 28.Gottschalk A, Schroeder F, Ufer M, Oncu A, Buerkle H, Standl T. Amantadine, a N-methyl-D-aspartate receptor antagonist, does not enhance postoperative analgesia in women undergoing abdominal hysterectomy. 2 pAnesth Analg. 2001;93(1):192–6. doi: 10.1097/00000539-200107000-00038. [DOI] [PubMed] [Google Scholar]
- 29.Treskatsch S, Klambeck M, Mousa SA, Kopf A, Schafer M. Influence of high-dose intraoperative remifentanil with or without amantadine on postoperative pain intensity and morphine consumption in major abdominal surgery patients: a randomised trial. 2 pEur J Anaesthesiol. 2014;31(1):41–9. doi: 10.1097/01.EJA.0000434967.03790.0e. [DOI] [PubMed] [Google Scholar]
- 30.Verghese ST, Hannallah RS. Acute pain management in children. 2 pJ Pain Res. 2010;3:105–23. doi: 10.2147/jpr.s4554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McCartney CJ, Sinha A, Katz J. A qualitative systematic review of the role of N-methyl-D-aspartate receptor antagonists in preventive analgesia. 2 pAnesth Analg. 2004;98(5):1385–400. doi: 10.1213/01.ane.0000108501.57073.38. table of contents. [DOI] [PubMed] [Google Scholar]
- 32.Aida S, Fujihara H, Taga K, Fukuda S, Shimoji K. Involvement of presurgical pain in preemptive analgesia for orthopedic surgery: a randomized double blind study. 2 pPain. 2000;84(2-3):169–73. doi: 10.1016/s0304-3959(99)00196-7. [DOI] [PubMed] [Google Scholar]
- 33.Ong CK, Lirk P, Seymour RA, Jenkins BJ. The efficacy of preemptive analgesia for acute postoperative pain management: a meta-analysis. 2 pAnesth Analg. 2005;100(3):757–73. doi: 10.1213/01.ANE.0000144428.98767.0E. table of contents. [DOI] [PubMed] [Google Scholar]
- 34.Bujak-Gizycka B, Kacka K, Suski M, Olszanecki R, Madej J, Dobrogowski J, et al. Beneficial effect of amantadine on postoperative pain reduction and consumption of morphine in patients subjected to elective spine surgery. 2 pPain Med. 2012;13(3):459–65. doi: 10.1111/j.1526-4637.2011.01321.x. [DOI] [PubMed] [Google Scholar]
- 35.Pud D, Eisenberg E, Spitzer A, Adler R, Fried G, Yarnitsky D. The NMDA receptor antagonist amantadine reduces surgical neuropathic pain in cancer patients: a double blind, randomized, placebo controlled trial. 2 pPain. 1998;75(2-3):349–54. doi: 10.1016/s0304-3959(98)00014-1. [DOI] [PubMed] [Google Scholar]
- 36.Gagliese L, Jackson M, Ritvo P, Wowk A, Katz J. Age is not an impediment to effective use of patient-controlled analgesia by surgical patients. 2 pAnesthesiology. 2000;93(3):601–10. doi: 10.1097/00000542-200009000-00007. [DOI] [PubMed] [Google Scholar]