Abstract
Objective
Children with life-threatening medical conditions frequently undergo invasive medical procedures that may elicit anxiety and distress. However, there are few empirically validated interventions that reduce mental health symptoms and increase the resilience of children during the acute stages of illness. This study aimed to evaluate the efficacy of the Make a Wish intervention for children with life-threatening cancer.
Methods
The design was a wait-list-controlled trial with two parallel groups. Sixty-six children aged 5–12 with an initial diagnosis of life-threatening cancer were identified and randomly assigned to the Make a Wish intervention (n = 32) or a wait-list control group (n = 34). Children completed measures of psychiatric and health-related symptoms, positive and negative affect, hope, and optimism pre-intervention and post-intervention. After baseline data collection, children were interviewed and made an authentic wish that they wanted to come true. These wishes were made possible 5–6 months after baseline data collection, to fuel anticipation and excitement over the wish-fulfillment event. The post-intervention assessment point was 5 weeks after wish fulfillment (approximately 7 months after baseline data collection).
Results
Children in the intervention group exhibited a significant reduction in general distress (d = 0.54), depression (d = 0.70), and anxiety symptoms (d = 0.41), improved health-related quality of life (d = 0.59), hope (d = 0.71), and positive affect (d = 0.80) compared to decrease in positive affect and no significant changes in the other measures in the control group.
Conclusions
These findings emphasize the role of hope and positive emotions in fostering the well-being of children who suffer from serious illnesses.
Keywords: Children, Resilience, Cancer, Oncology, Hope, Wish-fulfillment
Introduction
In the past 30 years, there has been an increase in the incidence of all forms of invasive cancer in children and adolescents [1]. Concurrently, however, survival rates have improved dramatically for most childhood cancer diseases, thanks to advances in early diagnosis, medical technology, and treatment interventions [1]. Despite this increase in survival rates, children with cancer still experience tremendous physical and psychosocial challenges, including aversive physical symptoms [2], difficulties in psychosocial functioning [3], and high levels of depressive [4], anxiety, fear, and post-traumatic stress symptoms [5]. These psychological symptoms, particularly phobias and anticipatory fear of impending treatment procedures, may interfere with compliance with treatment and can act as a significant barrier to the child's recovery [5, 6].
The rising awareness of the psychological impact of coping with cancer [4] has led to increasingly more community-driven interventions to enhance the quality of life and well-being of these children. Few studies have been conducted on the effects of such activities on children and families; thus, the positive impact of these events and the potentially detrimental outcomes of these well-intentioned initiatives, such as a decline in well-being after the event, remain unclear. To better understand these issues, the Israeli “Make a Wish” organization, which is part of the international “Make a Wish Foundation” that grants the wishes of children with life-threatening medical conditions, authorized us to study the outcomes of their specific interventions. Make a Wish was established in 1980 in Pheonix, Arizona, and has granted more than 280,000 wishes worldwide, in 36 countries. The Make a Wish organization categorizes children's wishes into four themes: to be, to meet, to have, or to go. For example, children have wanted “to meet” Bill Clinton, Lionel Messi, Madonna, “to go” to Disney World; “to have” a puppy or an IPad, or “to be” a pop star for a day or a firefighter. The goal of the intervention is to fulfill the child's greatest wish based on the assumption that evoking hope and joy will potentially give children more strength to cope with their illness. While there are numerous stories of healing and joy in the Make a Wish Foundation's logs, no studies have been conducted to support the anecdotal evidence of the positive influence of the experience on children whose wishes have been granted.
More broadly in the literature, a number of individual protective factors have been associated with better psychosocial outcomes for children with cancer, including hope [7], optimism [8], positive emotions [9], perceived support [10], and positive expectations for the future [11]. The benefits of these factors seem to be related to their involvement in secondary control engagement coping, in that they enable adjustment to stressors through acceptance, positive thinking, and/or distraction [12, 13]. The “Make a Wish” intervention appears to be particularly applicable to the promotion of these modifiable protective factors. By making a wish, having positive expectations that it will be granted, and feeling a sense of accomplishment and satisfaction when the wish comes true, the child may undergo a process that generates hope, positive emotions, and optimism to both patients and their families. The experience may reduce despair while cultivating the child's coping resources. The sense of achievement in actualizing a wish may create a generalized sense of hope, which has been found to be extremely important for recovery and healing in life-threatening conditions [7, 14].
Throughout history, philosophers, scholars, theologians, and religious leaders have recognized the value of wish fulfillment for experiences of happiness, joy, self-fulfillment, and meaning in life. Cross-culturally, there is value attached to the act of making a wish, as evidenced by various traditions and customs in which people are encouraged to make a wish: blowing out the candles on a birthday cake, witnessing a shooting star, throwing coins into a fountain, or viewing the first full moon of the year. However, to date, there is a dearth on studies that can provide an empirical explanation for the positive effects of wish fulfillment.
In this study, we compared a Make a Wish intervention group to a waiting-list control group at two time points: baseline and approximately 7 months after baseline data collection (5 weeks after the wish-fulfillment event). This provided an opportunity to evaluate the effects of the intervention beyond the peak experience of the event itself [15].
Based on the theoretical rationale and previous findings, we hypothesized that the children in the Make a Wish intervention would exhibit a greater decrease in mental health symptoms, and health-related physical symptoms, and increase in positive affect than children on the waiting-list control group. More specifically we predicted that: (a) the Make a Wish intervention group would show significant reductions in mental health symptoms and general distress from baseline to post-intervention compared to an increase in the mental health symptoms in the control group; (b) the Make a Wish intervention would reduce physical symptoms and negative emotions from pre- to post-intervention compared to no change or an increase in these measures in the control group; and (c) the Make a Wish intervention would elevate optimism, hope, and positive affect in the intervention group, compared to no change in these measures in the control group.
Methods
Participants
The study included 66 children with cancer, aged 5–12 (M = 10.39, SD = 3.9) who were referred to Make a Wish Israel in 2013 and 2014. Eligible families had children who: (a) were aged 3–14 years, (b) had an initial diagnosis of cancer, (c) were receiving medical treatment, and (d) had no preexisting developmental disorder.
Research design and randomization
A waiting-list-controlled trial design was used. The participants were stratified by type of disease (leukemia, Hodgkin's lymphoma, Ewing's sarcoma, medulloblastoma, or other solid tumor), and gender, and were randomly (block randomization) assigned to the Make a Wish intervention or to the waiting-list control group. Randomization was done by the study statistician, who was blind to the protocol, and was not otherwise involved in the assessments. A random-number generator program was used to select numbers that established the sequence in which blocks were allocated to the intervention or the control group. A 1:1 ratio was used. The participants could not be blind to the design because of the nature of the intervention.
Procedure
After the academic ethics committee and the institutional review boards approved the study, pediatric oncology social workers in three large hospitals in the Tel Aviv Metropolitan Area (Gush Dan) in Israel collected information about children with cancer whose parents had expressed interest in the “Make a Wish” intervention. Upon receiving referral forms and parental approval, the referred child's doctor provided the consulting pediatric oncologist with medical information to assess whether the medical status of the child met the organization's criteria for wish fulfillment. Children who were severely ill or needed urgent medical care were immediately referred to wish fulfillment and did not participate in the study. Eighty-four remaining children were identified and referred by the doctor for wish fulfillment. These children had similar medical severity ratings and were considered high priority for wish fulfillment. However, it is important to note that because of limited resources, Make a Wish Israel could not fulfill all these children's wishes immediately, and regardless of the study design, some needed to wait several months for wish fulfillment. We utilized this inevitable limitation to randomly allocate children the intervention and control waiting-list groups. Eligible families for the study were then approached by a member of the research team to introduce the research and determine interest in participating in the study. If interested, parents completed an informed consent form, and a demographic and disease survey.
For the intervention group, a research assistant who was not involved in the intervention, made appointments with the families and children at their homes to fill in the questionnaires. All of the participants received a thorough explanation of the study, and all provided their consent with the understanding that if they declined to participate, it would have no impact on their participation in the Make a Wish intervention.
Research assistants read the questionnaires out loud and explained the rating scales to 5- and 6-year-olds who could not read the questionnaires on their own, while older children who were literate self-completed the questionnaires. After filling out the questionnaires, the Make a Wish organization sent trained interviewers to the homes of each child. Children were interviewed individually in a quiet room separately from their parents. The goal of this interview was to become acquainted with the child and learn more about his/her wish. The interviewer encouraged the children to make a wish that they felt was true and dear to their hearts, without outside pressure from their parents. The wishes were granted 5–6 months after the first time point. Posttest data collection took place 5 weeks after the wish-fulfillment event. At Time 2, 5 weeks after the wish-fulfillment event, the research assistant made an appointment with the children and asked them to fill out a set of questionnaires identical to Time 1.
Each child in the intervention group was matched with a child of the same age and gender in the waiting-list group. One of the researchers coordinated a meeting with the control group parents and obtained their consent for their children to participate in the study. After consenting to participate in the study, the children were given the questionnaire packets. The questionnaires were administered to the wait-list control participants and the children in the intervention group at approximately the two same time points, either on the same day or, at the most, with a 1-day difference, within 24 h.
Outcome measures
The primary outcomes in the study related to predicted changes in psychiatric symptoms. The secondary outcomes consisted of the children's ratings of health-related quality of life, hope, optimism, and positive and negative emotions.
Measures
Psychiatric symptoms
The Brief Symptom Inventory 18 (BSI) [16] was used to assess children's mental health symptoms. This instrument is composed of 18 items rated on a Likert-type scale from 0 (not at all) to 4 (very much) and includes four subscales: Somatization, Depression, Anxiety, and Panic. The Global Severity Index (GSI) calculates overall distress and is the sum of the four BSI subscales. The BSI has been widely used for assessment of psychopathology in Israeli preadolescents [17, 18] and American children [19] and exhibits high internal consistency and concurrent validity. In the current study, the Cronbach's alpha was 0.87.
Health-related quality of life
Health-related quality of life was assessed on the physical functioning subscale of the Pediatric Quality of Life Inventory (PedsQL™4.0) [20], an 8-item scale that assesses basic physical functioning abilities and limitations, such as difficulty running, difficulty walking more than a block, pain, or lack of energy. In this study, the child self-report version of PedsQL™ was used for participants aged 5–18, which employs a 5-point Likert scale ranging from “never” to “almost always.” Items were reverse-scored and linearly transformed to a 0–100 scale (4 = 0, 3 = 25, 2 = 50, 1 = 75, 0 = 100), so that higher scores indicated better physical health. The physical health summary score was computed as the sum of the items divided by the number of items answered [20]. In the current study, the Cronbach's α was 0.80.
Positive affectivity indicators
Three assessment tools were used. The Positive and Negative Affect Schedule for Children (PANAS-C) was used to measure children's positive and negative emotions [21]. This scale consists of 10 adjectives that describe five positive and five negative emotions. Children rated the extent to which they had felt each mood in the previous few days on a scale ranging from 1—very slightly, to 5—extremely. Earlier research supports high internal consistency and convergent validity [21]. The alpha coefficients were 0.91 and 0.94 for the positive and negative affect subscales, respectively.
The Life Orientation Test-Revised (LOT-R) [22] adaptation for children [23] comprises 10 items that assess optimism and expectations regarding the favorability of future outcomes. Responses are obtained on a scale ranging from 0—strongly disagree, to 4—strongly agree. The Cronbach's alphas in this study were 0.61 for optimism and 0.63 for pessimism.
Children's hope was assessed by the Herth Hope Index (HHI) [24], a 12-item index rated on a 4-point Likert scale that assesses a global sense of hope. Summative scores range from 12 to 48, with a higher score indicating greater hope. The Cronbach's alpha was = 0.90 at Time 1.
Sample size calculation
On the basis of BSI (psychiatric symptoms) changes in previous resilience-promoting interventions in trauma samples compared to control groups (e.g., [25, 26]), we calculated that a minimum of n = 25 per group would be needed to detect an intervention effect of −0.18 points (SD = 0.32) on the GSI (global severity index) with 0.80 power and alpha set at p < 0.05.
Statistical analyses
In preliminary analyses, we examined the effects of positive affectivity indicators on psychiatric and health-related quality of life at baseline while controlling for possible effects of demographic variables and disease characteristics. For this purpose, two hierarchical linear regression analyses were computed. The baseline levels of the GSI and the physical health summary scale of the PedsQL were entered as the dependent variables in each regression model. Age, gender, SES (first block), duration of illness, type of current treatment (second block), positive and negative emotions, optimism, and hope (third block) were entered as predictor variables. Alpha was set at p < 0.05 for statistical significance.
Repeated measures ANOVAs were conducted to examine the overall intervention effect and change for the outcome variables in the intervention and control groups at the two assessment points (baseline and after wish fulfillment). A Bonferroni correction was used to account for multiple comparisons between groups (p ≤ 0.005). Paired sample t tests were used to test for differences in the dependent variables within each group. The standardized effect sizes were calculated by using Cohen's Ds. Effect sizes of 0.2–0.5 were interpreted as small, 0.5–0.8 as medium, and >0.80 as large [27].
We used the SPSS Missing Value Analysis package to estimate the pattern of missing data and impute missing values by the appropriate procedures. Little's MCAR test was not significant (χ2 = 31.93, df = 27, p = 0.24), indicating that the missing data did not show a significant pattern. We used maximum likelihood estimation to account for missing data that were less than 3 % across all the study variables and assessment points. There were no significant differences in the proportion of missing versus present data in the intervention versus control groups.
Results
Participant flow
Figure 1 charts the participant flow in the study. Eighty-four families were approached for participation in this study, and 88 % (n = 74) of these families consented to participate, and were randomly allocated to the intervention or control condition. Eight families dropped out after the first measurement point due to busy schedules (n = 4, intervention; n = 1, control group), refusal for personal reasons (n = 2, both groups), or death (n = 1, control group), leaving a final sample of 66 families. The dropped out participants were not considered in the analyses, and the intention-to-treat analysis was not performed. The final sample was made up of 32 children in the wish-fulfillment intervention group and 34 children in the waiting-list control group.
Fig. 1.
CONSORT diagram of the inclusion, assignment, and retention of the intervention group (Make a Wish) and control group. T0, baseline; T1, corresponds to 5 weeks post-intervention
Participant characteristics
The study population consisted of 66 Israeli-born Jewish children with cancer, aged 5–12.
The participating families were tested between 0.2 and 4.5 years after the child's first diagnosis (M = 1.65 years, SD = 1.20). The sociodemographic and medical characteristics of the intervention and control groups are presented in Table 1. The intervention and control groups did not differ significantly on any demographic or outcome variable at baseline.
Table 1.
Demographic and sample characteristics at baseline
| Mean (SD) |
Statistic | p value | ||
|---|---|---|---|---|
| Control group (n = 34) | Intervention group (n = 32) | |||
| Gender | χ2 = 0.29 | 0.58 | ||
| Boys [n (%)] | 19 (55.9 %) | 20 (62.5 %) | ||
| Age (years) | 10.67 (4.71) | 10.13 (3.51) | t = 0.53 | 0.60 |
| Socioeconomic status | χ2 = 0.63 | 0.73 | ||
| Upper middle class [n (%)] | 7 (21 %) | 7 (22 %) | ||
| Middle class | 20 (58 %) | 16 (50 %) | ||
| Lower middle class | 7 (21 %) | 9 (28 %) | ||
| Type of disease | χ2 = 0.69 | 0.95 | ||
| Leukemia [n (%)] | 10 (29 %) | 9 (28 %) | ||
| Hodgkin's lymphoma [n (%)] | 6 (18 %) | 4 (13 %) | ||
| Ewing's sarcoma [n (%)] | 4 (12 %) | 5 (15 %) | ||
| Medulloblastoma | 3 (9 %) | 4 (13 %) | ||
| Other solid tumor | 11 (32 %) | 10 (31 %) | ||
| Type of current treatment | χ2 = 0.11 | 0.98 | ||
| Chemotherapy | 14 (41.2 %) | 14 (43.8 %) | ||
| Biological therapy | 6 (17.6 %) | 5 (15.6 %) | ||
| Combination of therapies | 7 (20.6 %) | 7 (21.8 %) | ||
| Other | 7 (20.6 %) | 6 (18.8 %) | ||
| Hope | 38.07 (6.48) | 38.11 (5.59) | t = 0.03 | 0.97 |
| Positive emotions | 18.55 (3.68) | 18.72 (3.51) | t = 0.19 | 0.85 |
| Negative emotions | 12.65 (3.87) | 12.38 (2.85) | t = 0.27 | 0.74 |
| Optimism | 16.42 (3.99) | 16.01 (3.38) | t = 0.41 | 0.65 |
| Health-related quality of life | 46.50 (24.01) | 44.91 (22.90) | t = 0.28 | 0.78 |
| Psychological distress (GSI) | 0.94 (0.52) | 0.97 (0.35) | t = 0.35 | 0.79 |
Note Other solid tumor = Specific types of tumors, such as nervous system tumors, retinoblastoma, and nephroblastoma
Predictors of psychiatric and health-related quality of life at baseline
Preliminary data analyses suggested that the study variables were normally distributed with no unusual kurtosis or skewness. The means and standard deviations of the variables before and after wish fulfillment are presented in Table 2.
Table 2.
Descriptive statistics for psychiatric symptoms, positive affect, and health-related quality of life of children in the intervention and control groups
| Intervention (n = 32) |
Control (n = 34) |
|||||||
|---|---|---|---|---|---|---|---|---|
| T1 Mean (SD) | T2 Mean (SD) | Cohen's d | p | T1 Mean (SD) | T2 Mean (SD) | Cohen's d | p | |
| Hope | 38.11 (5.59) | 41.52 (3.89) | 0.71 | 0.004** | 38.07 (6.48) | 37.22 (6.65) | 0.13 | 0.583 |
| Positive emotions | 18.72 (3.51) | 21.48 (3.42) | 0.80 | 0.003** | 18.55 (3.68) | 17.69 (3.88) | 0.24 | 0.000*** |
| Negative emotions | 12.38 (2.85) | 10.71 (3.25) | 0.55 | 0.033 | 12.65 (3.87) | 12.61 (3.56) | 0.01 | 0.871 |
| Optimism | 16.01 (3.38) | 16.89 (2.95) | 0.28 | 0.188 | 16.42 (3.99) | 16.18 (3.18) | 0.07 | 0.423 |
| Health-related quality of life | 44.91 (22.90) | 57.34 (18.92) | 0.59 | 0.004** | 46.50 (24.01) | 38.77 (23.30) | 0.33 | 0.173 |
| Somatization | 1.04 (0.73) | 0.97 (0.69) | 0.10 | 0.040 | 1.05 (0.79) | 1.26 (0.79) | 0.27 | 0.248 |
| Depression | 1.03 (0.51) | 0.68 (0.49) | 0.70 | 0.000*** | 0.97 (0.75) | 1.12 (0.61) | 0.22 | 0.304 |
| Anxiety | 1.01 (0.52) | 0.79 (0.55) | 0.41 | 0.000*** | 0.98 (0.65) | 1.15 (0.57) | 0.28 | 0.114 |
| Panic | 0.80 (0.84) | 0.70 (0.79) | 0.12 | 0.024 | 0.76 (0.77) | 0.80 (0.75) | 0.05 | 0.548 |
| GSI-global Severity Index | 0.97 (0.34) | 0.79 (0.33) | 0.54 | 0.000*** | 0.94 (0.52) | 1.08 (0.45) | 0.29 | 0.178 |
p Values after Bonferroni correction for multiple testing.
p < 0.01
p < 0.001
The linear combination of the disease characteristics and the child's affectivity indicators was found to be significantly related to the baseline levels of psychiatric symptoms in the total sample, R = 0.69, R2 = 0.48, F(10, 55) = 4.17, p < 0.001, and indicated that approximately 48 % of the variance of the GSI levels in the sample could be accounted for by the linear combination of the predictors. Chemotherapy (β = 0.30, SE B = 0.15, partial r = 0.5, p = 0.02) and biologically based therapies (β = 0.24, SE B = 0.23, partial r = 0.27, p = 0.04) together with negative emotions (β = 0.47, SE B = 0.007, partial r = 0.51, p < 0.001) were significantly and negatively correlated with high levels of mental health symptomatology. However, illness duration, positive emotions, hope, and optimism were not significantly related to the baseline levels of the psychiatric symptoms.
For baseline levels of health-related quality of life (PedsQL), the entire model significantly predicted 36 % of the variance of the physical health summary scale, R = 0.60, R2 = 0.36, F(10, 55) = 2.47, p = 0.02. The predictor of negative emotions was negatively associated with physical health (β = −0.34, SE B = 0.12, partial r = 0.36, p = 0.01), whereas the types of treatment, illness duration, positive emotions, hope, and optimism were not significantly related to the baseline levels of the physical health.
Intervention impact on psychological symptomatology
Primary outcomes
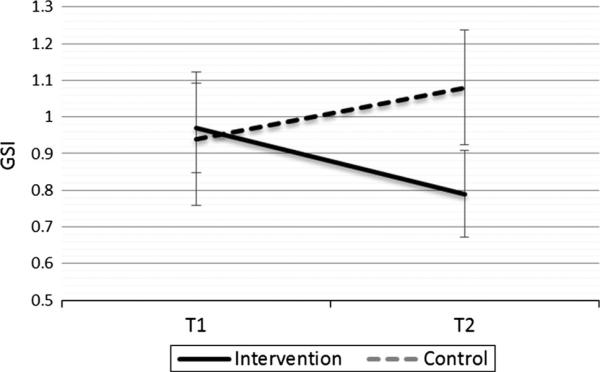
The intervention effects were analyzed using repeated measures ANOVAs. The Time × Group effects for GSI, depression, and anxiety scores were significant, with a significant differential rate of change in GSI levels, F(1, 64) = 9.30, p = 0.003, partial η2 = 0.14, depressive symptoms, F(1, 64) = 11.29, p = 0.001, partial η2 = 0.15, and anxiety symptoms, F(1, 64) = 12.51, p = 0.001, partial η2 = 0.16, between the intervention and waiting-list groups from baseline to Time 2 (see Table 2). The mean reduction in GSI for intervention participants was 0.18, with a medium effect size, t(31) = 23.46, p < 0.001, d = 0.54, compared to a nonsignificant increase of 0.14 for the waiting-list participants, t(33) = 1.38, p = 0.18, d = 0.29 (Fig. 2). Similarly, the mean reduction in depression for the intervention group was 0.35, with a medium effect size t(31) = 18.92, p < 0.001, d = 0.70, compared to a nonsignificant increase of 0.15 for the waiting-list control group, t(33) = 1.05, p = 0.30, d = 0.22. For anxiety, there was a significant reduction of 0.22 in the intervention group, t(31) = 9.83, p < 0.001, d = 0.41, compared to a nonsignificant increase of 0.17 in the waiting-list control group, t(33) = 1.62, p = 0.11, d = 0.28. There were no statistically significant differences in panic or somatization over time for either of the groups.
Fig. 2.
Changes in the mean scores for mental health symptoms (GSI) from baseline to post-intervention assessment (7 months after baseline), with corresponding 95 % confidence intervals
Intervention impact on health-related quality of life and positive affectivity outcomes
Secondary outcomes
For health-related quality of life, there was a significant difference between the intervention and control groups over time for physical health, F(1, 64) = 8.57, p = 0.005, partial η2 = 0.12. The intervention group presented an increase in physical health of 12.43, with a medium effect size, t(31) = 3.15, p = 0.004, d = 0.59, compared to a nonsignificant decrease of 7.73 in the control group from baseline to Time 2, t(33) = 1.39, p = 0.17, d = 0.33.
For the additional secondary outcomes, there was a significant differential rate of change in the general sense of hope between the intervention and control groups from Time 1 to Time 2, F(1, 64) = 8.54, p = 0.005, partial η2 = 0.14. Children in the intervention group demonstrated a significant increase in their general sense of hope from baseline to Time 2 of 3.41, with a medium effect size, t(31) = 3.12, p = 0.004, d = 0.71, compared to a nonsignificant decrease of 0.85 for the waiting-list participants, t(33) = 0.55, p = 0.58, d = 0.13 (see Fig. 3). In addition, there was a significant difference between the intervention and control groups over time for positive emotions, F(1, 64) = 17.85, p < 0.001, partial η2 = 0.22. Children in the intervention group presented a significant increase of 2.76 in positive emotions over time, with a large effect size, t(31) = 3.18, p = 0.003, d = 0.80, compared to a significant reduction of 0.86, with a small effect size, in the control group, t(33) = 5.48, p < 0.001, d = 0.24. There were no significant differences between the intervention and control groups for negative emotions or levels of optimism over time.
Fig. 3.
Changes in mean scores for hope from baseline to post-intervention, with corresponding 95 % confidence intervals
Discussion
Accumulating research evidence points to a relationship between the emotional aspects of hope, optimism, and positive expectations and the psychological symptoms that accompany coping with a life-threatening illness [7, 8, 11]. However, few studies have dealt with specific interventions tailored to elicit and activate the emotional mechanisms that serve as protective factors in coping with a life-threatening illness. In response to this need, the present study empirically tested a wish-fulfillment intervention for children suffering from cancer that aimed to promote well-being and resilience during a period of high risk of the emergence of psychological difficulties.
The examination of the predictors of baseline levels of psychological distress and physical health indicated that active treatment, such as chemotherapy, or biological treatments along with negative emotions were correlated with psychological distress. The level of negative emotions was also significantly correlated with the level of physical limitations without any significant effect of age, gender, or socioeconomic status on psychological and physiological symptomatology.
The findings indicated that the children who received the wish-fulfillment intervention had higher levels of hope regarding their future, increased positive emotions and health-related quality of life, and a better psychological profile manifested by lower levels of depression, anxiety, and psychological symptomatology. On the other hand, the control group showed lower levels of positive emotions over time, and no significant changes in their levels of hope, health-related quality of life, or psychological symptomatology.
These findings raise questions regarding the possible emotional processes induced by having a wish fulfilled, which may account for the positive changes in the children whose wishes were fulfilled. A wish is different from a goal or a regular aim. It is coveted, “magical,” and out of the ordinary. A wish is beyond mundane desires or goals that are obtainable. It is possible that wishing enabled these children to dream about something that seemed unobtainable, out of reach, and thus created an experience of achieving the “impossible.” From a motivational point of view, wish fulfillment can be seen as a motivator for coping and hope for the future.
Additionally, the expectation and realization of the wish resulted in enhanced positive emotions. Beyond the immediate benefits of positive affect, the broaden-and-build theory proposes that positive emotions expand people's thought-action repertoires and the forming of personal, physical, intellectual, social, and psychological resources [28]. Experiencing positive emotions is believed to promote more adaptive environmental responses and resilience and vastly improve an individual's daily functioning and overall well-being [29].
From a cognitive perspective, during the process of wish fulfillment the child is in a continuous process in which he imagines the moment of fulfillment. These cognitive processes may be a possible source of distraction from the day-to-day worries of coping with a serious illness and may be a critical coping mechanism for children in difficult and uncontrollable situations [13]. Distractions such as these may normalize their daily life and retain childhood experiences of happiness, play, imagination, fun, and entertainment, which may have been disrupted by the diagnosis and the start of treatment. Moreover, fantasizing about wish fulfillment may help replace negative automatic thoughts by positive ones that have been shown to be important when coping with life-threatening illnesses [30].
Interestingly, the findings point to an increase in children's hope but not optimism. This finding may also hint at the conscious processes that took place after the wish was fulfilled. Hope and optimism are both constructs related to positive expectations about one's future. Optimism seems to be related to a generalized expectation of a positive outcome, whereas hope is related to agency and the sense that one has knowledge of how to obtain a desired goal [31]. This further supports our claim that the wish fulfillment may have provided the children a sense of agency; namely, wishing for something and having it come true.
Physical limitations are one of the most distressing aspects of oncological and other life-threatening illnesses and have been shown to limit quality of life and physical functioning [32]. Therefore, it is important to highlight the moderate but significant decrease in the perception of physical limitations in the intervention group. Physical symptoms have roots in the physiology of the illness and side effects of the treatment; however, it has been shown that the frequency, intensity, and course of physical symptoms are affected by psychosocial factors [32]. Thus, overall, the findings reinforce the need for interventions that promote resilience, increase emotional well-being, and enhance the health-related quality of life among children with life-threatening illnesses.
Limitations and conclusions
There are several limitations that must be recognized in this study. First, there were slight differences in the type of diseases and treatments of the children in the intervention and control groups. However, the nonsignificant differences in the baseline variables between groups indicated sufficient resemblance between the intervention and control groups. Second, the second measurement point in the study (posttest) was approximately 7 months after baseline data collection and 5 weeks after the wish-fulfillment event. We deliberately selected this time point to leave enough time for any residual excitement related to the wish fulfillment to subside [15]. Unfortunately, because of practical limitations, we were not able to obtain a third time point to further examine the lasting effects of wish fulfillment.
Furthermore, these conclusions are limited by the small sample size. A larger sample and multiple measurements over time would be desirable in future studies.
Another limitation is that in a study of this nature, participants and their caretakers could not be blind to their assignment to a group. As a result, children in the waiting-list control group knew that they were likely to receive the treatment (wish granting) when the study ended. This sense of anticipation for the fulfillment of a wish in the future may also have influenced their psychological well-being and potentially affected the data in the control group. Additionally, an intention-to-treat analysis was not conducted in this study. However, given that the participants who dropped out of the study did not complete the follow-up questionnaires and had certain constraints that prevented them from participating in the intervention, they could be excluded from the remaining analyses without a high risk of increasing bias [33, 34]. Nevertheless, the decision to focus solely on the population of participants who completed the intervention limits the generalizability of the findings and may suggest a selection bias due to the fact that those who dropped out of the study were not included in the analyses. In addition, for ethical reasons, the children who were in severe conditions and need of immediate medical attention did not participate in the study and were directly referred to wish fulfillment. Therefore, the present study sample was not entirely representative of the overall population of children experiencing wish fulfillment and precludes any conclusions regarding the positive effects of the intervention on children in acute, immediate life-threatening conditions. Finally, the data in this study were analyzed using the individual children as the units of analysis and ignored their groupings within hospitals or other potential contexts that could affect the outcomes in this study. As such, it would be prudent to address this issue in further research.
The emotional and psychosocial complexity that characterizes the experience of life- threatening illnesses in childhood requires systemic and holistic treatment in caring for the emotional side effects that continue to reverberate in the child's physical and emotional state. The tailoring of such care requires continued evidence-based research on positive psychological interventions for children coping with serious illnesses. Interventions that instill hope should be included in these types of studies.
Acknowledgments
We would like to thank the families and the children who found the time and energy to participate in this study. We would also like to express our deepest gratitude to Denise Bar Aharon, Dorit Dovrat, and the Make a Wish Israel team for their help in this effort.
Footnotes
Compliance with ethical standards
Conflict of interest The authors declare that they have no conflict of interest.
Ethical approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent Informed consent was obtained from all individual participants included in the study.
References
- 1.Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, et al. SEER cancer statistics review, 1975–2011. National Cancer Institute; Bethesda, MD: 2014. [January 27, 2015]. from http://seer.cancer.gov/csr/1975_2011/. [Google Scholar]
- 2.Collins JJ, Byrnes ME, Dunkel IJ, Lapin J, Nadel T, Thaler HT, et al. The measurement of symptoms in children with cancer. Journal of Pain and Symptom Management. 2000;19(5):363–377. doi: 10.1016/s0885-3924(00)00127-5. doi:10.1016/S0885-3924(00)00127-5. [DOI] [PubMed] [Google Scholar]
- 3.Vance YH, Eiser C. The school experience of the child with cancer. Child: Care, Health and Development. 2002;28(1):5–19. doi: 10.1046/j.1365-2214.2002.00227.x. doi:10.1046/j.1365-2214.2002.00227.x. [DOI] [PubMed] [Google Scholar]
- 4.Curtis CE, Luby JL. Depression and social functioning in preschool children with chronic medical conditions. The Journal of Pediatrics. 2008;153(3):408–413. doi: 10.1016/j.jpeds.2008.03.035. doi:10.1016/j.jpeds.2008.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pao M, Bosk A. Anxiety in medically ill children/adolescents. Depression and Anxiety. 2011;28(1):40–49. doi: 10.1002/da.20727. doi:10.1002/da.20727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Griffiths M, Schweitzer R, Yates P. Childhood experiences of cancer an interpretative phenomenological analysis approach. Journal of Pediatric Oncology Nursing. 2011;28(2):83–92. doi: 10.1177/1043454210377902. doi:10.1177/1043454210377902. [DOI] [PubMed] [Google Scholar]
- 7.Germann JN, Leonard D, Stuenzi TJ, Pop RB, Stewart SM, Leavey PJ. Hoping is coping: A guiding theoretical framework for promoting coping and adjustment following pediatric cancer diagnosis. Journal of Pediatric Psychology. 2015 doi: 10.1093/jpepsy/jsv027. doi:10.1093/jpepsy/jsv027. [DOI] [PubMed] [Google Scholar]
- 8.Williams NA, Davis G, Hancock M, Phipps S. Optimism and pessimism in children with cancer and healthy children: Confirmatory factor analysis of the youth life orientation test and relations with health-related quality of life. Journal of Pediatric Psychology. 2010;35(6):672–682. doi: 10.1093/jpepsy/jsp084. doi:10.1093/jpepsy/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chaves C, Hervas G, García FE, Vazquez C. Building life satisfaction through well-being dimensions: A longitudinal study in children with a life-threatening illness. Journal of Happiness Studies. 2015 doi:10.1007/s10902-015-9631-y. [Google Scholar]
- 10.Kim DH, Yoo IY. Factors associated with resilience of school age children with cancer. Journal of Pediatrics and Child Health. 2010;46(7–8):431–436. doi: 10.1111/j.1440-1754.2010.01749.x. doi:10.1111/j.1440-1754.2010.01749.x. [DOI] [PubMed] [Google Scholar]
- 11.Grootenhuis MA, Last BF. Children with cancer with different survival perspectives: Defensiveness, control strategies, and psychological adjustment. Psycho-Oncology. 2001;10(4):305–314. doi: 10.1002/pon.529. doi:10.1002/pon.529. [DOI] [PubMed] [Google Scholar]
- 12.Connor-Smith JK, Compas BE, Wadsworth ME, Thomsen AH, Saltzman H. Responses to stress in adolescence: Measurement of coping and involuntary stress responses. Journal of Consulting and Clinical Psychology. 2000;68(6):976. doi:10.1037/0022-006X.68.6.976. [PubMed] [Google Scholar]
- 13.Phipps S. Adaptive style in children with cancer: Implications for a positive psychology approach. Journal of Pediatric Psychology. 2007;32:1055–1066. doi: 10.1093/jpepsy/jsm060. doi:10.1093/jpepsy/jsm060. [DOI] [PubMed] [Google Scholar]
- 14.Whitney SN, McCullough LB, Frugé E, McGuire AL, Volk R. Beyond breaking bad news: The roles of hope and hopefulness. Cancer. 2008;113(2):442–445. doi: 10.1002/cncr.23588. [DOI] [PubMed] [Google Scholar]
- 15.Privette G. Peak experience, peak performance, and flow: A comparative analysis of positive human experiences. Journal of Personality and Social Psychology. 1983;45:1361–1368. doi:10.1037/0022-3514.45.6.1361. [Google Scholar]
- 16.Derogatis LR, Spencer PM. Brief symptom inventory: BSI. Pearson; Upper Saddle River, NJ: 1993. [Google Scholar]
- 17.Lavi T, Green O, Dekel R. The contribution of personal and exposure characteristics to the adjustment of adolescents following war. Journal of Adolescence. 2013;36:21–30. doi: 10.1016/j.adolescence.2012.09.003. doi:10.1016/j.adolescence.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 18.Slone M, Shoshani A. Psychiatric effects of protracted conflict and political life events exposure among adolescents in Israel: 1998–2011. Journal of Traumatic Stress. 2014;27:353–360. doi: 10.1002/jts.21918. doi:10.1002/jts.21918. [DOI] [PubMed] [Google Scholar]
- 19.Burnett-Ziegler I, Walton MA, Ilgen M, Barry KL, Chermack ST, Blow FC, et al. Prevalence and correlates of mental health problems and treatment among adolescents seen in primary care. Journal of Adolescent Health. 2012;50:559–564. doi: 10.1016/j.jadohealth.2011.10.005. doi:10.1016/j.jadohealth.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 20.Varni JW, Seid M, Kurtin PS. PedsQL™ 4.0: Reliability and validity of the Pediatric Quality of Life Inventory™ Version 4.0 Generic Core Scales in healthy and patient populations. Medical Care. 2001;39(8):800–812. doi: 10.1097/00005650-200108000-00006. doi:10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Ebesutani C, Regan J, Smith A, Reise S, Higa-McMillan C, Chorpita BF. The 10-item positive and negative affect schedule for children, child and parent shortened versions: Application of Item Response Theory for more efficient assessment. Journal of Psychopathology and Behavioral Assessment. 2012;34:191–203. doi:10.1007/s10862-011-9273-2. [Google Scholar]
- 22.Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A reevaluation of the Life Orientation Test. Journal of Personality and Social Psychology. 1994;67(6):1063. doi: 10.1037//0022-3514.67.6.1063. doi:10.1037/0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- 23.Bamford C, Lagattuta KH. Looking on the bright side: Children's knowledge about the benefits of positive versus negative thinking. Child Development. 2012;83:667–682. doi: 10.1111/j.1467-8624.2011.01706.x. doi:10.1111/j.1467-8624.2011.01706.x. [DOI] [PubMed] [Google Scholar]
- 24.Herth K. Abbreviated instrument to measure hope: Development and psychometric evaluation. Journal of Advanced Nursing. 1992;17(10):1251–1259. doi: 10.1111/j.1365-2648.1992.tb01843.x. doi:10.1111/j.1365-2648.1992.tb01843.x. [DOI] [PubMed] [Google Scholar]
- 25.Slone M, Shoshani A. Efficacy of a school-based primary prevention program for coping with exposure to political violence. International Journal of Behavioral Development. 2008;32(4):348–358. doi:10.1177/0165025408090976. [Google Scholar]
- 26.Slone M, Shoshani A, Lobel T. Helping youth immediately following war exposure: A randomized controlled trial of a school-based intervention program. The Journal of Primary Prevention. 2013;34:293–307. doi: 10.1007/s10935-013-0314-3. doi:10.1007/s10935-013-0314-3. [DOI] [PubMed] [Google Scholar]
- 27.Cohen J. Statistical power analysis for the behavioral sciences. Psychology Press; Hillsdale, New Jersey: 1988. [Google Scholar]
- 28.Fredrickson BL. The broaden-and-build theory of positive emotions. Philosophical Transactions-Royal Society of London Series B Biological Sciences. 2004;359(1449):1367–1378. doi: 10.1098/rstb.2004.1512. doi:10.1098/rstb.2004.1512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reschly AL, Huebner ES, Appleton JJ, Antaramian S. Engagement as flourishing: The contribution of positive emotions and coping to adolescents’ engagement at school and with learning. Psychology in the Schools. 2008;45:419–431. doi:10.1002/pits.20306. [Google Scholar]
- 30.Folkman SK, Moskowitz JT. Positive affect and the other side of coping. American Psychologist. 2000;55:647–654. doi: 10.1037//0003-066x.55.6.647. doi:10.1037//0003-066X.55.6.647. [DOI] [PubMed] [Google Scholar]
- 31.Gallagher MW, Lopez SJ. Positive expectancies and mental health: Identifying the unique contributions of hope and optimism. The Journal of Positive Psychology. 2009;4:548–556. doi:10.1080/17439760903157166. [Google Scholar]
- 32.Barakat LP, Daniel LC, Sills RH. Functional somatic symptoms in pediatric hematology and oncology. In: Anbar RD, editor. Functional symptoms in pediatric disease. Springer; New York: 2014. pp. 145–156. doi:10.1007/978-1-4899-8074-8. [Google Scholar]
- 33.Fergusson D, Aaron SD, Guyatt G, Hébert P. Post-randomisation exclusions: The intention to treat principle and excluding patients from analysis. British Medical Journal. 2002;325(7365):652–654. doi: 10.1136/bmj.325.7365.652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Heritier SR, Gebski VJ, Keech AC. Inclusion of patients in clinical trial analysis: The intention-to-treat principle. Medical Journal of Australia. 2003;179(8):438–440. doi: 10.5694/j.1326-5377.2003.tb05627.x. [DOI] [PubMed] [Google Scholar]