Summary
Research shows that many adolescents who enter treatment for substance use do not complete the recommended program, and after discharge, do not connect with continuing care services. Furthermore, the majority of adolescents will return to some level of substance use either during or after participation in treatment. Our review found 10 outcome studies of continuing care treatment for adolescents. Five of six studies with randomized designs resulted in significant clinical improvement for youth receiving the experimental continuing care approaches. Key findings of these trials are that more assertive approaches can increase continuing care initiation rates and that rapid initiation of continuing care made a difference in reducing substance use. Findings suggest that continuing care is not only appropriate for those who successfully complete treatment but also for many individuals who do not. Although there are no randomized controlled studies of adolescent participation in mutual aid groups, evidence is accumulating suggesting that matching adolescents to age-appropriate 12-step and other mutual aid groups can support recovery. Research employing adaptive treatment designs holds promise for establishing decision rules as to which adolescents need low-intensity continuing care services and which need more intensive care.
Keywords: Adolescents, Aftercare, Continuing Care, Assertive Continuing Care, Adaptive Treatment, mutual aid groups
Introduction
Several evidence-based treatments (EBTs) for adolescent substance use have emerged since the early 1990s. Treatments such as Multidimensional Family Therapy, Family Behavior Therapy, the Adolescent Community Reinforcement Approach, Motivational Interviewing, Cognitive Behavioral Therapy, and contingency management have all been adapted for and tested with adolescents. Randomized clinical trials employing singular or integrated protocols of these interventions have demonstrated improved short-term substance use outcomes in outpatient clinics, hospital emergency rooms, and school settings1–12.
Despite these advancements, adolescent relapse rates during the year after treatment often exceed 60%, and many youth cycle between periods of substance use and abstinence1,13–17. These statistics are reinforced by analysis of a large national dataset of adolescents entering outpatient and residential treatment programs for substance use disorders18. Figure 1 shows that over half of adolescents relapse within 90 days of the end of an acute episode of care.
Figure 1.
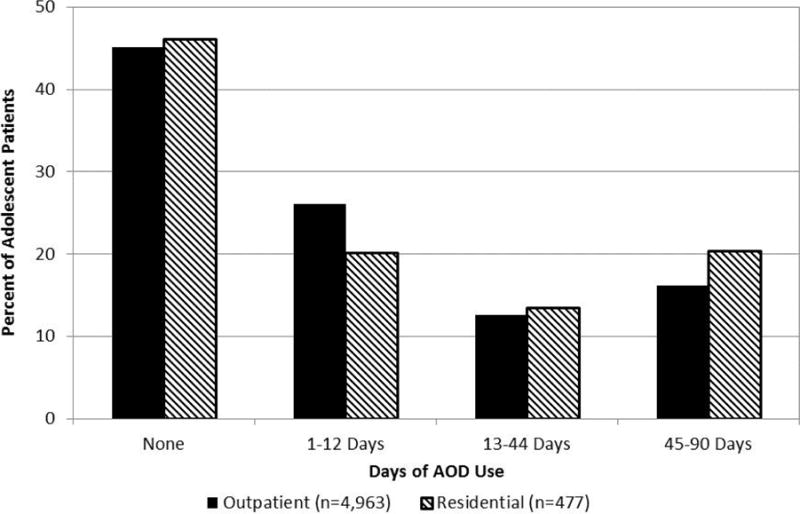
Adolescent AOD use in the 90 days following discharge from treatment.
These data support research that indicates that alcohol and substance use disorders, like other chronic relapsing illnesses (e.g., asthma, diabetes), require long-term monitoring and support19–23. Research also suggests that addressing substance use problems is a process that involves acute treatment, ongoing management, and multiple continuing interventions as needed19,24–27.
While high rates of adolescent relapse may reflect that youth tend to be less motivated to change substance use than adults, have low problem recognition, and enter treatment because of external pressures28–29, it is impossible to know which adolescents are beginning a long term chronic relapsing illness and which will “age out” or enter long term remission and recovery through treatment. Regardless of which path will be followed, recent investigation into adolescent brain development points to the importance of treating substance use disorders in youth30.
Brain imaging research demonstrates that the human brain is still developing until the early 20s, notably in the prefrontal cortex regions that control executive functioning such as reasoning, decision-making, impulse control, and judgment. Therefore, it may be assumed that adolescents entering treatment for substance use disorders have poor executive functioning in the prefrontal cortex and are potentially at higher risk to the effects of drugs31–32. They may make emotional and impulsive decisions. Evidence is accumulating that adolescent brains may be more sensitive to the effects of alcohol in decreasing social discomfort, while they may be less sensitive to its intoxication effects33. Furthermore, laboratory research has shown that adolescent rats display significantly more damage from alcohol to their frontal cortex and working memory than adult rats33–34. More research is needed, however, to determine the extent to which neurocognitive functions may recover over time with abstinence and to tease out the effects of substances and other independent influences on the brain35.
Since substance use disorders can be a chronic relapsing condition that begins in adolescence and adolescent brains may be more vulnerable to the effects of substance use, continuing care services are especially important to help youth maintain treatment gains. Historically, continuing care was referred to as “aftercare” that followed a successful acute treatment episode. “Step-down” care was the first and most common form of aftercare and involved referral to lower intensity treatment (outpatient) upon completion of more intensive services (usually residential or inpatient).
Referral to non-professional recovery supports has also become a common continuing care practice. For example, recommendations to attend mutual support groups became increasingly popular following the founding of Alcoholics Anonymous in 1935, and in the mid-twentieth century, the development of the Minnesota Model of treatment relying on 12-step education and meeting attendance36–38. Treatment programs have traditionally referred both adults and adolescents to these groups39–42.
As aftercare has evolved, there has been a shift from the idea of “aftercare” to the concept of “continuing care.” Aftercare is predicated on the assumption that individuals complete a more intensive level of care and step-down to a less intensive set of services. In reality, most adolescents do not respond to treatment in this manner. Studies show that a large percentage of adolescents entering treatment will relapse and return to the same or a more intensive level of treatment. It is also common for youth to end treatment prematurely13,43–45. Such findings with both adolescents and adults have led the American Society of Addiction Medicine (ASAM)46 to define continuing care as:
The provision of a treatment plan and organizational structure that will ensure that a patient receives whatever kind of care he or she needs at the time. The treatment program thus is flexible and tailored to the shifting needs of the patient and his or her level of readiness to change. (p. 361)
Research on continuing care with adults has shown promise21,47–52 and research on adolescent continuing care is still in its early stages and growing. The purpose of this paper is to review the literature on continuing care and other recovery supports for adolescents and make recommendations for clinical practice and future research.
Research on Adolescent Linkage to Continuing Care Services
Despite evidence of the importance of continuing care and the emphasis placed on continuity of care by ASAM and other organizations, most adolescents do not receive these services. Linkage rates to professional continuing care range from 35% to 45% within 90 days of discharge15,43. Less than half of youth receive a referral for continuing care because they leave treatment early—usually against staff advice or at staff request53. Reports of linkage rates to mutual support groups, typically AA and NA, vary widely between studies. They indicate that anywhere from 42% to 75% of adolescents will attend one or more 12-step meetings in the first three months following discharge from residential treatment54–57.
For youth with a planned discharge, those who are referred to continuing care within the same organization are much more likely to connect than those referred to a different organization (89% versus 50%)15,54. Additional potential influences on linkage rates include distance from a youth’s residence to an outpatient clinic or mutual support meeting, transportation problems, treatment fatigue, and caregiver work schedules15,53. Lack of follow-through with referrals to and drop-out from mutual support groups can be due to age dissimilarity with other group members or the philosophy of the referring treatment program. It may also be affected by, when compared with adults, the presence of less severe substance use problems, briefer substance use histories, lower motivation for abstinence, and lower problem recognition29,41,57–58.
Research on Continuing Care for Adolescents After Residential Treatment for Substance Use Disorders
Most research on adolescent continuing care has focused on delivery of services after discharge from residential treatment.
Early Studies of Continuing Care
In one of the earliest studies, Ralph and McMenamy59 examined data from adolescents who had completed an inpatient substance abuse treatment program. These youth were offered an aftercare program that consisted of adolescent and family multi-groups for a year after discharge. Participation in aftercare was associated with less substance use since discharge and lower amounts of use over six months.
In another study, juvenile offenders in detention facilities were committed to a two-month residential substance abuse treatment program. Those who completed treatment and resided in the county were placed in a four-month aftercare program. “Prerelease” occurred during residential treatment and included a family assessment, treatment contract, weekly family sessions, and support groups. The “intensive” phase included two months of post-release supervision, daily face-to-face contacts, youth and family support meetings, and youth meetings with an addiction counselor. In the “transitional” phase, youth met with case managers two times per week and with an addiction counselor two times per month for a total of two months. Youth were linked with community services. Family support groups continued, and family therapy was provided as needed.
When compared to a no-aftercare group of youth, participation in aftercare was associated with reduced emotional abuse as well as more drug-related, but not personal-related, delinquency. No evidence of a program effect was found for increasing family supervision, attachment, emotional support, and communication, reducing family violence and drug use, increasing internal locus of control, increasing drug knowledge, decreasing health problems, increasing coping and problem-solving skills, or positive urine tests. Results need to be interpreted with caution, however, due to significant differences between the comparison groups, low follow-up completion rates, problems with implementation, and low family involvement60.
Studies of Standard Continuing Care
In one study, a standard recommendation for adolescents who received inpatient care was to attend aftercare sessions with their families at the facility following discharge. Participants could discuss individual concerns and learn about substance use and recovery. Weekly meetings lasted about one hour. While no further detail about these services was provided, findings were that more frequent aftercare meeting attendance was associated with more days of abstinence during the six-month follow-up period61.
Winters, Stinchfield, Latimer, and Lee62 found that adolescents who completed an outpatient or residential program based on the Minnesota Model were expected to enter a half-year outpatient aftercare program that met two to three times per week. The purpose of aftercare was to continue the treatment process, provide ongoing assessment, and make referrals for assistance as necessary. Adolescents who attended aftercare at a moderate/regular level were more likely to show improved substance use than those who attended aftercare at a minimum level or did not attend at all.
Assertive Continuing Care
A current approach aimed at increasing continuing care linkage rates is Assertive Continuing Care (ACC). ACC brings continuing care to the adolescent in his/her home community whether or not residential treatment was completed successfully and shifts responsibility of service delivery from the youth to the clinician. ACC services are initiated as soon as possible after discharge from the initial treatment episode, thereby requiring clinicians to coordinate closely with referring treatment programs. At that time, ACC clinicians deliver case management services combined with an evidence-based treatment–the Adolescent Community Reinforcement Approach (A-CRA).
Case management services include: (a) home visits; (b) help linking the adolescent to necessary services; (c) transportation to needed services, a pro-social activity, or potential jobs; (d) advocacy to access services; (e) monitoring lapse cues and attendance at services and activities; and (f) social support for coping with a lapse or other challenging issues63.
A-CRA includes sessions with the youth alone, the caregivers alone, and the youth and caregivers together. Using principles of operant learning theory and a positive, non-confrontational approach, the clinician helps the youth and his/her family restructure social and recreational activities to compete with time spent using alcohol and drugs. During sessions, the clinician draws from 17 different therapeutic procedures that focus on various skills and life areas. They include relapse prevention, relationship skills, communication skills, problem-solving, goal-setting and working through barriers to completion, analysis of using behaviors, making non-substance-using friends, engaging in satisfying social and leisure activities that do not involve substance use, sampling new activities, and assignment of homework. On an ongoing basis, the youth fills out a self-assessment to develop and monitor progress toward completion of goals. There are also optional procedures for coping with a lapse, anger management, and job-finding15,53,64.
ACC has been tested with adolescents in two randomized clinical trials after residential treatment. In the first study, 183 youth were aged 12–17 years old and met DSM-IV criteria for current alcohol or other drug abuse or dependence. The majority were male (71%), Caucasian (73%), and aged 15–18 (89%). Most were involved with the juvenile justice system (82%) and had one or more co-occurring mental health disorders.
After one week of residential treatment, participating youth were randomized to attend either ACC or usual continuing care for the first 90 days following discharge. All youth were referred to community outpatient clinics in their home communities. Analyses demonstrated that youth receiving ACC had significantly higher linkage rates to continuing care than those receiving UCC (94% versus 54%). They also received more days of continuing care sessions (18.1 versus 6.3 sessions). A main effect for ACC was demonstrated over the nine-month follow-up period for abstinence from marijuana. The intervention produced medium to large effect sizes. Adolescents in the two conditions had the same average length of residential stay (52 days) and comparable unplanned discharge rates (51% and 53%)65. There were no differences in 12-step attendance between conditions, with 65% attending one or more meetings and an average attendance of approximately 12 meetings during the 90-day period53.
The second clinical trial of ACC tested whether or not ACC augmented with motivational incentives would further improve substance use outcomes. Youth (n=337) were recruited from two residential programs and randomized to one of the following conditions for the first 90 days after discharge from residential care: (a) usual continuing care only; (b) motivational incentives only; (c) ACC only; or (d) motivational incentives plus ACC. Motivational incentives in the form of prize drawings were provided weekly contingent upon completion of verifiable prosocial activities and abstinence. The prize bowl contained 510 slips of paper: (a) 150 or 30% of the slips showed a smile face (no prize); (b) 324 or 62.8% of the slips read “small” (prize worth $1); (c) 35 or 7% of the slips read “large” (prize worth $25); and (d) one or 0.2% of the slips read “jumbo” (prize worth $100)66.
Similar to the first trial, youth were aged 12–17 years old and met criteria for substance abuse or dependence. The majority were male (63%) and Caucasian (70%). The average age was 15.7 years (SD=1.2). Most (81%) had one or more co-occurring mental health disorders66.
Results show that youth receiving any of the three experimental conditions were significantly more likely to engage in their continuing care condition (attending four or more sessions within 45 days after residential discharge)67 than youth in usual continuing care only (75%–84% versus 49%). Adolescents in the motivational incentives only and ACC only conditions demonstrated significantly more days of abstinence from substance use over 12 months and were more likely to be in remission at 12 months than those receiving usual continuing care. Furthermore, motivational incentives and ACC resulted in significantly fewer days spent in a controlled environment66. Motivational incentives plus ACC did not result in significantly better outcomes.
Research on Continuing Care for Adolescents after Outpatient Treatment for Substance Use Disorders
While research on continuing care after outpatient treatment is a newer development in the field, there have been a small number of clinical trials.
Active Aftercare
Kaminer and colleagues have been researching the effects of telephone continuing care delivered to adolescents after outpatient treatment. For this trial, 144 youth were randomized to one of three conditions for three months following completion of group treatment: (a) Active Aftercare consisting of five in-person sessions; (b) Active Aftercare consisting of five brief telephone sessions; or (c) a no aftercare control. Sixty-seven percent were male, 82% were Caucasian, and the average age was 15.9 (SD=1.2). Seventy-nine percent were diagnosed with substance abuse or dependence, 58% with an internalizing disorder, and 76% with an externalizing disorder.
Both Active Aftercare conditions were manual-guided and consisted of one session of functional analysis followed by four integrated motivational enhancement and cognitive-behavioral therapy sessions68. Therapists assessed substance use and motivation to change, identified problem areas, and provided skills guidelines to address problems. In-person sessions were 50 minutes, while telephone sessions were 12 to 15 minutes69.
Overall, there was a significant decrease in alcohol abstinence from the end of treatment to the end of aftercare, with those assigned to no active aftercare showing larger decreases than those assigned to Active Aftercare. In-person and telephone conditions were equal and resulted in higher alcohol abstinence rates (37.5%) than no aftercare (26.8%). Adolescents in Active Aftercare also had significantly fewer drinking days per month and heavy drinking days per month. There was a significant overall decrease in marijuana abstinence from end of treatment to end of aftercare but not as a function of condition6. Initial results diminished at the 12-month follow-up assessment70.
ACC
In a trial following outpatient treatment, 320 adolescents were randomized to receive ACC or usual continuing care following outpatient discharge. Youth were aged 13–18 years old and met criteria for substance abuse or dependence. The majority were male (76%) and Caucasian (73%) with an average age of 15.9 (SD=1.2). Most (56%) had one or more co-occurring mental health disorders. There were no statistically significant findings for the effectiveness of ACC71.
In a different trial, Henderson et al.72 compared three months of outpatient A-CRA followed by three months of ACC to services as usual provided by a juvenile probation department. One hundred twenty-six youth between 12–17 years old were enrolled in the study. Average age was 15.2 (SD=1.07), and all screened positive for a moderate to severe alcohol or drug use problem. Most adolescents were male (74%) and Caucasian (79%). While all participating youth reduced substance use frequency and substance-related problems after outpatient treatment, youth receiving ACC demonstrated a substantially greater decrease in substance-related problems.
Adaptive Approaches to Continuing Care
Since research shows that a large segment of youth who enter treatment do not complete the program and that many do not achieve abstinence or sobriety, it is important to examine continuing care interventions aimed at improving outcomes of poor responders to treatment. Godley et al.65 state that because several episodes of treatment are the rule rather than the exception, non-completion of services does not necessarily indicate that youth may fail to benefit from continuing care. Since 94% of adolescents who initiate at least one week of abstinence do so by the sixth week of treatment, this suggests that an adaptive approach to continuing care could benefit youth who do not achieve abstinence by this time. That is, it may be more effective to commence continuing care for poor responders at this point rather than follow a fixed, pre-planned treatment schedule73.
In a recent study, Kaminer et al.74 provided continuing care for adolescents with cannabis use disorders who were poor responders to outpatient treatment. One hundred sixty youth were defined as poor responders because they did not achieve abstinence after seven weeks of outpatient treatment. These youth were randomized into a 10-week continuing care phase of either an individualized enhanced cognitive-behavioral therapy or A-CRA. Thirty-seven percent of poor responders completed the continuing care phase, and 27% percent achieved abstinence. There was neither a difference in retention rates nor in abstinence rates between the two conditions.
Other than the study above, there is little research guidance on adaptive approaches to continuing care with adolescents; however, McKay75 presented a series of key questions about individuals who do not respond to treatment: Should they be switched to another treatment? Which one? Or, should another treatment augment what is already being received? One approach that has the potential to increase rates of participation is to admit individuals to the least restrictive appropriate level of care and then “step” them up to more intensive treatment if warranted by poor initial response. Such stepped care may increase cost-effectiveness and cost-benefit.
Kaminer and Godley25 described several elements thought to be critical for the design of adaptive treatment protocols. First, tailoring variables need to be identified that assess key markers of progress. For example, a therapist may regularly assess substance use and use that information to make treatment decisions. Second, an adaptive treatment protocol needs to offer a menu of clinical interventions that are meaningfully different on at least one dimension, such as frequency or theoretical orientation. For an adaptive strategy to work, treatment options must be different enough that poor response in one treatment approach will not strongly predict failure in other options75. Finally, decision rules need to be created that link the tailoring variables and the menu of interventions into one algorithm, ideally arrived at through expert consensus or experimental study. The adaptive algorithm would then be used to decide what services are provided to which individuals and when.
Research on Other Recovery Supports for Adolescents
While most randomized studies of adolescent continuing care have investigated professionally-provided programs, there has been research with varying levels of rigor into other recovery support services.
Volunteer-Telephone Continuing Care
In one quasi-experimental study, 222 adolescents were recruited to participate. These youth were between 13–18 years old, met criteria for substance abuse or dependence, had remained in either outpatient treatment for at least four sessions within 44 days from the intake session or in residential treatment for at least two weeks, and had telephone access.
Over the course of the study, the intervention was delivered by 60 pre-professional volunteers who were primarily recruited from university undergraduate and graduate programs in social work, psychology, and nursing. All volunteers participated in background checks and a training session on selected A-CRA/ACC procedures, recovery support call procedures, ethics, and confidentiality. In addition to documenting call information, volunteers recorded calls for weekly supervision.
Within the first week after discharge from treatment, trained volunteers initiated recovery support calls. During each session, volunteers asked about:
significant events since the last call;
substance use, if any, since the last contact;
steps recently taken to stay clean and sober;
additional ways to stay clean and sober;
the occurrence of any using thoughts and strategies for dealing with them;
pro-recovery goals and homework to set for the next week;
progress on goals set during the previous call;
recovery-related events in communities; and
the use of additional support services.
Volunteers made referrals for substance abuse treatment services if relapse occurred and referrals for mental health services if emotional and/or behavioral difficulties were reported.
Telephone calls were typically 15 minutes or less in length. Text messaging was used to remind adolescents of upcoming calls or to complete sessions at the adolescent’s request. The goal was to complete sessions with adolescents once per week during the first 90 days after discharge. The frequency of contacts after that time varied depending on adolescents’ functioning and preference.
Six-month outcome data from 202 adolescents who had received recovery support calls were compared to six-month outcome data from a matched comparison sample of adolescents. Results suggested adolescents in the recovery support sample had significantly greater reductions in their recovery environment risk relative to the comparison sample. Analyses also suggested that the reduction in recovery environment risk produced by recovery support calls had indirect impacts on reductions in social risk, substance use, and substance-related problems76.
Mutual Support Groups
There is a growing body of research into adolescent participation in mutual support groups. To date, these studies have focused exclusively on the 12-step groups of Alcoholics Anonymous (AA) and Narcotics Anonymous (NA). Correlational studies suggest that youth who attend AA and/or NA after residential treatment for substance use are more likely to remain abstinent and use substances less frequently41,56–57,77–80.
Despite this preliminary yet inconclusive evidence of benefit, clinicians have anecdotally expressed concerns when referring youth to these groups. Most group members will be significantly older, with longer substance use histories and different life challenges due to their age42. This age difference has also given rise to concerns about safety. Worries include the belief that older male members with criminal histories may intimidate or engage youth in illegal or predatory activities81. Although the majority of youth in one study reported feeling very safe at AA or NA meetings, 22% reported at least one negative experience, such as feeling intimidated, threatened, or sexually harassed. Reports were more common among those who went to NA. However, youth did not report safety concerns as a reason to stop attending82. On the other hand, some clinicians felt that certain youth benefitted from the wisdom and praise of adults at meetings81.
Additional research regarding age indicates that youth who attend 12-step meetings with at least a substantial proportion of people their age after inpatient treatment have better substance use outcomes58. Unfortunately, youth-oriented meetings are not accessible to a large percentage of adolescents due to limited availability.
Which Adolescents Benefit Most from Continuing Care?
Existing research with adults and adolescents provides preliminary ideas for which youth might benefit most from particular continuing care services. In the adult literature, when Lynch et al.83 compared Telephone Monitoring plus Counseling to Treatment as Usual to Telephone Monitoring only, they found that Telephone Monitoring was more beneficial than Treatment as Usual for women and participants with lower readiness to change. McKay et al.51 discovered that adults with high scores on a composite risk indicator had better total abstinence outcomes up to 21 months if they received standard counseling rather than the telephone intervention, whereas those with lower scores had higher abstinence rates in the telephone intervention than in standard counseling. McKay et al.84 found that in adults with alcohol dependence only, the telephone-based monitoring and brief counseling interventions produced better alcohol use outcomes than standard group counseling on all measures examined and better outcomes than relapse prevention on some of the measures.
In the adolescent literature, Godley and Godley53 re-analyzed data from the first ACC clinical trial. They compared youth assigned to the ACC group who failed to link to any continuing care services with those in the Usual Continuing Care (UCC) condition who failed to link to any continuing care despite receiving referrals from their residential treatment counselors. There were no demographic or clinical differences between the two groups. Despite the fact that typical referrals to continuing care failed to work, within the ACC subgroup, all but six participants received varying levels of the ACC intervention delivered by a clinician via home or other community visits. Clinical outcome comparisons between these two subgroups revealed that the ACC subgroup was significantly more likely to remain abstinent from all drugs during the ACC phase and significantly more likely to remain abstinent from marijuana over the total nine-month follow-up period.
Godley and Godley15 analyzed data from adolescents who did not complete residential treatment. Of non-completers assigned to UCC, 33% received continuing care within 14 days of discharge. Of those assigned to an assertive condition (ACC and/or motivational incentives), 64% did. Those who received additional services within 14 days of discharge were more likely to have superior alcohol and marijuana abstinence outcomes even if they did not complete residential treatment, regardless of condition. Within an assertive condition, residential completers and non-completers that received services within 14 days of discharge were significantly more likely to be abstinent from alcohol than non-completers who did not.
Finally, analyses of Volunteer Telephone Continuing Care data demonstrated that the effects of recovery support calls did not differ by gender but were significantly greater for adolescents with lower levels of treatment readiness76.
Taken together, these data suggest that future research is needed to better examine if telephone continuing care could especially benefit individuals with lower readiness to change, only alcohol dependence, and lower risk. They also indicate that continuing care, especially using an assertive approach to reaching and engaging youth, may work well for individuals who do not complete treatment or follow through on typical continuing care referral advice.
Summary and Discussion
Research shows that many adolescents who enter substance use treatment do not complete the program, and after discharge, do not initiate continuing care services. Furthermore, the majority of adolescents will return to some level of substance use either during or after treatment. As youth return to use and problems occur, many will re-enter treatment, and some will do so several times. This pattern of disjointed treatment episodes remains the norm in contemporary practice rather than the intended plan of a course of treatment followed by continuing care. The studies reviewed in this paper offer prospective continuing care options consistent with expert consensus46.
Our review found 10 outcome studies of continuing care treatment for adolescents, six of which used randomized designs. Despite the fact that there are only six prospective, well-controlled continuing care studies, five resulted in clinical improvement for youth receiving the experimental continuing care approaches. Four of the controlled studies used ACC (two post-residential and two post-outpatient), and three of these found a clinical advantage for ACC, suggesting its effectiveness.
Key findings of these trials are that more assertive approaches can increase linkage rates to continuing care75. Another key finding of some trials was that rapid initiation of continuing care (i.e., linking to ongoing services within 14 days of discharge from treatment) made a difference in reducing substance use. Thus, rapid provision of continuing care is likely to prevent or assist in terminating a relapse. Both ACC and motivational incentive approaches can be used to facilitate rapid linkage85. Contrary to aftercare programs that require treatment completion, multiple studies support providing continuing care to those who do not complete53,65–66,74. This suggests that continuing care is appropriate for those who successfully complete treatment and can improve outcomes for individuals who do not.
On the other hand, the effectiveness of continuing care approaches, especially those that are more labor intensive like ACC, may not be necessary for all adolescents. Research employing adaptive treatment designs similar to that employed by Kaminer and colleagues74 holds promise for establishing decision rules as to which individuals need low-intensity continuing care and which need more intensive home-based continuing care such as ACC. Although using decision rules is proving useful to assess who may need continuing care, providers may not have ready access to good follow-up outcome information, especially for individuals discharged early from residential treatment.
Although there are no randomized controlled studies of adolescent participation in mutual aid groups, evidence is accumulating in the published literature suggesting that matching adolescents to age appropriate 12-step and other mutual aid groups can support recovery. Referrals to meetings that are predominantly attended by adults should be carefully assessed to assure a safe match. The lower cost of continuing care delivered through recovery coaches and other volunteers is promising, but controlled prospective studies are required before these approaches can be recommended76,86–88.
Additional continuing care research is needed in several areas. Studies are needed to assess whether patient intake variables (such as substance and/or co-occurring problem severity), treatment process variables (such as treatment completion or attainment of one or more treatment goals), and variables measuring parental involvement in treatment serve as valid predictors of who needs low or high intensity monitoring, support, counseling, and/or case management. Research accessible to therapists serving a broad range of individuals is needed that establishes decision rules using clinical and treatment variables that prove useful in matching level of continuing care services to individuals. Conducting research to establish more accessible predictor variables may be best accomplished through multi-site research collaborations with sufficiently large samples to employ adaptive treatment designs. Particularly for adolescents, more data regarding technology-based interventions would be useful because of its inherent appeal to this population. Research on low-cost and sustainable continuing care delivery methods would help inform treatment programs trying to implement services with shrinking budgets or issues with service reimbursement. Investigation into the use of incentives for continuing care linkage and retention and continuing care research with youth who have co-occurring psychiatric disorders is sorely needed. Finally, with the promise of continuing care research to date and the potential of low cost approaches, incorporating these interventions into adaptive continuing care studies to establish cost-effective decision rules should be a fruitful area for further examination.
Key Points.
Research shows that many adolescents who enter treatment for substance use do not complete the recommended program, and after discharge, return to regular use and do not initiate continuing care services.
Assertive approaches (counselor-initiated home or school-based continuing care) increase linkage to continuing care, and rapid initiation of continuing care makes a difference in reducing substance use.
Findings suggest that continuing care is not only appropriate for those who successfully complete treatment.
Evidence is accumulating to suggest that matching adolescents to age-appropriate 12-step and other mutual aid groups can support recovery.
Research employing adaptive treatment designs holds promise for establishing decision rules as to which individuals need low-intensity continuing care services and which need more intensive care.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Lora L. Passetti, no conflicts of interest
Mark D. Godley, no conflicts of interest
Yifrah Kaminer, no conflicts of interest
Contributor Information
Lora L. Passetti, Email: lpassetti@chestnut.org, Chestnut Health Systems, 448 Wylie Drive, Normal, IL 61761.
Mark D. Godley, Email: mgodley@chestnut.org, Chestnut Health Systems, 448 Wylie Drive, Normal, IL 61761.
Yifrah Kaminer, Email: kaminer@uchc.edu, Alcohol Research Center, University of Connecticut School of Medicine, 263 Farmington Avenue, Farmington, CT 06030.
References
- 1.Dennis ML, Godley SH, Diamond GS, et al. The Cannabis Youth Treatment (CYT) study: Main findings from two randomized trials. J Subst Abuse Treat. 2004;27:197–213. doi: 10.1016/j.jsat.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 2.Diamond GS, Godley SH, Liddle HA, et al. Five outpatient treatment models for adolescent marijuana use: A description of the Cannabis Youth Treatment interventions. Addiction. 2002;97:S70–S83. doi: 10.1046/j.1360-0443.97.s01.3.x. [DOI] [PubMed] [Google Scholar]
- 3.Donohue B, Azrin NA. Treating adolescent substance abuse using family behavior therapy: A step-by-step approach. Hoboken, NJ: John Wiley and Sons; 2012. [Google Scholar]
- 4.Godley SH, Godley MD. Behavioral treatments for adolescents with substance use disorders. In: Miller PM, editor. Interventions for addiction: Comprehensive addictive behaviors and disorders. San Diego: Academic Press; 2013. pp. 167–75. [Google Scholar]
- 5.Kaminer Y. Contingency management reinforcement procedures for adolescent substance abuse. J Am Acad Child Adolesc Psychiatry. 2000;39:1324–26. doi: 10.1097/00004583-200010000-00022. [DOI] [PubMed] [Google Scholar]
- 6.Kaminer Y, Burleson JA, Burke RH. Efficacy of outpatient aftercare for adolescents with alcohol use disorders: A randomized controlled study. J Am Acad Child Adolesc Psychiatry. 2008;7:1405–12. doi: 10.1097/CHI.0b013e318189147c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Monti PM, Colby SM, O’Leary TA, editors. Adolescents, alcohol, and substance abuse: Reaching teens through brief interventions. New York: Guilford Press; 2001. [Google Scholar]
- 8.Petry NM. A comprehensive guide to the application of contingency management procedures in general clinic settings. Drug Alcohol Depend. 2000;58:9–25. doi: 10.1016/s0376-8716(99)00071-x. [DOI] [PubMed] [Google Scholar]
- 9.Stanger C, Budney AJ, Kamon J, Thostensen J. A randomized trial of contingency management for adolescent marijuana abuse and dependence. Drug Alcohol Depend. 2009;105:240–47. doi: 10.1016/j.drugalcdep.2009.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wagner EF, Macgowan MJ. School-based group treatment for adolescent substance abuse. In: Liddle HA, Rowe CL, editors. Adolescent substance abuse: Research and clinical advances. Cambridge: Cambridge University Press; 2006. pp. 333–56. [Google Scholar]
- 11.Waldron HB, Turner CW. Evidence-based psychological treatments for adolescent substance abuse. J Clin Child Adolesc Psychol. 2008;37:238–61. doi: 10.1080/15374410701820133. [DOI] [PubMed] [Google Scholar]
- 12.Winters KC, Leitten W. Brief intervention for drug-abusing adolescents in a school setting. Psychol Addict Behav. 2007;21:349–54. doi: 10.1037/0893-164X.21.2.249. [DOI] [PubMed] [Google Scholar]
- 13.Brown SA, Vik PW, Creamer VA. Characteristics of relapse following adolescent substance abuse treatment. Addict Behav. 1989;14:291–300. doi: 10.1016/0306-4603(89)90060-9. [DOI] [PubMed] [Google Scholar]
- 14.Chung T, Maisto SA. Review and reconsideration of relapse as a change point in clinical course in treated adolescents. Clin Psychol Rev. 2006;26:149–61. doi: 10.1016/j.cpr.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 15.Godley MD, Godley SH. Assertive Continuing Care for adolescents. In: Kelly JF, White WL, editors. Addiction recovery management: Theory, research and practice. New York: Springer Science; 2011. pp. 103–26. [Google Scholar]
- 16.Kaminer Y, Burleson J, Goldberger R. Psychotherapies for adolescent substance abusers: Short-and long-term outcomes. J Nerv Ment Disease. 2002;190:737–45. doi: 10.1097/00005053-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Williams RJ, Chang SY. An assertive and comparative review of adolescent substance abuse treatment outcome. Clin Psychol Sci Prac. 2000;7:138–66. [Google Scholar]
- 18.GAIN Coordinating Center. Briefing book slides on all grantees in the 2012 SAMHSA/CSAT Summary Analytic File [Electronic Version] Normal, IL: Chestnut Health Systems; 2013. Available at: www.gaincc.org/slides. Accessed April 14, 2016. [Google Scholar]
- 19.McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: Implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284:1689–95. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- 20.McLellan AT, McKay JR, Forman R, Cacciola J, Kemp J. Reconsidering the evaluation of addiction treatment: From retrospective follow-up to concurrent recovery monitoring. Addiction. 2005;100:447–58. doi: 10.1111/j.1360-0443.2005.01012.x. [DOI] [PubMed] [Google Scholar]
- 21.Scott CK, Foss MA, Dennis ML. Utilizing Recovery Management Checkups to shorten the cycle of relapse, treatment reentry, and recovery. Drug Alcohol Depend. 2005;78:325–38. doi: 10.1016/j.drugalcdep.2004.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weisner C, McLellan T, Barthwell A, et al. Report of the Blue Ribbon Task Force on health services research at the National Institute on Drug Abuse. Rockville, MD: National Institute on Drug Abuse; 2004. [Google Scholar]
- 23.White WL, Boyle M, Loveland D. Recovery from addiction and recovery from mental illness: Shared and contrasting lessons. In: Ralph R, Corrigan P, editors. Recovery and mental illness: Consumer visions and research paradigms. Washington, DC: American Psychological Association; 2004. pp. 233–58. [Google Scholar]
- 24.Dennis ML, Scott CK. Managing addiction as a chronic condition. Addict Sci Clin Pract. 2007;4:45–55. doi: 10.1151/ascp074145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kaminer Y, Godley M. From assessment reactivity to aftercare for adolescent substance abuse: Are we there yet? Child Adolesc Psychiatr Clin N Am. 2010;19:577–90. doi: 10.1016/j.chc.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 26.Miller WR. What is relapse? Fifty ways to leave the wagon. Addiction. 1996;91:S15–S27. [PubMed] [Google Scholar]
- 27.White WL, Boyle M, Loveland D. Addiction as chronic disease: From rhetoric to clinical application. Alcoholism Treat Quart. 2002;20(3/4):107–30. [Google Scholar]
- 28.Battjes RJ, Gordon MS, O’Grady KE, et al. Factors that predict adolescent motivation for substance abuse treatment. J Subst Abuse Treat. 2003;24:221–32. doi: 10.1016/s0740-5472(03)00022-9. [DOI] [PubMed] [Google Scholar]
- 29.Tims FM, Dennis ML, Hamilton N, et al. Characteristics and problems of 600 adolescent cannabis abusers in outpatient treatment. Addiction. 2002;97(Suppl. 1):S46–S57. doi: 10.1046/j.1360-0443.97.s01.7.x. [DOI] [PubMed] [Google Scholar]
- 30.Winters KC. Adolescent brain development and drug abuse. Loughborough, UK: The Mentor Foundation; 2008. [Google Scholar]
- 31.Giedd JN. Structural magnetic resonance imaging of the adolescent brain. Ann NY Acad Sci. 2004;1021:77–85. doi: 10.1196/annals.1308.009. [DOI] [PubMed] [Google Scholar]
- 32.Rutherford HJV, Mayes LC, Potenza MN. Neurobiology of adolescent substance use disorders: Implications for prevention and treatment. Child Adolesc Psych Clin N Am. 2010;19(3):479–92. doi: 10.1016/j.chc.2010.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Spear LP. Alcohol’s effects on adolescents. Alcohol Health Res World. 2002;26(4):287–91. [PMC free article] [PubMed] [Google Scholar]
- 34.Brown SA, Tapert SF, Granholm E, Delis DC. Neurocognitive functioning of adolescents: Effects of protracted alcohol use. Alcohol Clin Exp Res. 2000;242:164–71. [PubMed] [Google Scholar]
- 35.Gonzalez R, Swanson JM. Long-term effects of adolescent-onset and persistent use of cannabis. Proc Natl Acad Sci USA. 2012;109(40):15970–71. doi: 10.1073/pnas.1214124109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Godley MD, White WL. The history and future of “aftercare”. Counselor. 2003;4(1):19–21. [Google Scholar]
- 37.Jainchill N. Therapeutic communities for adolescents: The same and not the same. In: De Leon G, editor. Community as method: Therapeutic communities for special population and special settings. Westport, CT: Praeger Publishers/Greenwood Publishing Group; 1997. pp. 161–77. [Google Scholar]
- 38.White WL, Dennis ML, Tims FM. Adolescent treatment: Its history and current renaissance. Counselor. 2002;3:20–24. [Google Scholar]
- 39.Drug Strategies. Treating teens: A guide to adolescent drug programs. Washington, DC: Author; 2003. [Google Scholar]
- 40.Humphreys K, Wing S, McCarty D, et al. Self-help organizations for alcohol and drug problems: Toward evidence-based practice and policy. J Subst Abuse Treat. 2004;26:151–58. doi: 10.1016/S0740-5472(03)00212-5. [DOI] [PubMed] [Google Scholar]
- 41.Kelly JF, Myers MG. Adolescents’ participation in Alcoholics Anonymous and Narcotics Anonymous: Review, implications and future directions. J Psychoactive Drugs. 2007;39:259–69. doi: 10.1080/02791072.2007.10400612. [DOI] [PubMed] [Google Scholar]
- 42.Passetti LL, White WL. Recovery support meetings for youths: Considerations when referring young people to 12-step and alternative groups. J Groups Addict Recover. 2008;2(2–4):97–121. [Google Scholar]
- 43.Godley SH, Godley MD, Dennis ML. The Assertive Aftercare Protocol for adolescent substance abusers. In: Wagner E, Waldron H, editors. Innovations in adolescent substance abuse interventions. New York: Elsevier Science; 2001. pp. 311–29. [Google Scholar]
- 44.Godley SH, Passetti LL, Funk RR, Garner BR, Godley MD. One-year treatment patterns and change trajectories for adolescents participating in outpatient treatment for the first time. J Psychoactive Drugs. 2008;40:17–27. doi: 10.1080/02791072.2008.10399758. [DOI] [PubMed] [Google Scholar]
- 45.Office of Applied Studies. Discharges from substance abuse treatment services. Rockville, MD: SAMHSA; 2005. Treatment Episode Data Set (TEDS): 2002. (DASIS Series S-25, DHHS Publication No. (SMA) 04-3967). Available at http://www.dasis.samhsa.gov/teds02/2002_teds_rpt_d.pdf. Accessed April 7, 2016. [Google Scholar]
- 46.American Society of Addiction Medicine. Patient placement criteria for the treatment of substance-related disorders. 2nd. Chevy Chase, MD: ASAM; 2001. [Google Scholar]
- 47.Dennis ML, Scott CK, Funk RR. An experimental evaluation of recovery management check-ups (RMC) for people with chronic substance use disorders. Eval Program Plann. 2003;26:339–52. doi: 10.1016/S0149-7189(03)00037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Godley MD, Coleman-Cowger VH, Titus JC, Funk RR, Orndorff MG. A randomized controlled trial of telephone continuing care. J Subst Abuse Treat. 2010;38:74–82. doi: 10.1016/j.jsat.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gustafson DH, McTavish FM, Chih MY, et al. A smartphone application to support recovery from alcoholism: A randomized clinical trial. JAMA Psychiatry. 2014;71(5):566–72. doi: 10.1001/jamapsychiatry.2013.4642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hubbard RL, Leimberger JD, Haynes L, et al. Telephone Enhancement of Long-Term Engagement (TELE) in continuing care for substance abuse treatment: A NIDA Clinical Trials Network (CTN) study. Am J Addict. 2007;16:495–502. doi: 10.1080/10550490701641678. [DOI] [PubMed] [Google Scholar]
- 51.McKay JR, Lynch KG, Shepard DS, Pettinati HM. The effectiveness of telephone-based continuing care for alcohol and cocaine dependence: 24 month outcomes. Arch Gen Psychiatry. 2005;62:199–207. doi: 10.1001/archpsyc.62.2.199. [DOI] [PubMed] [Google Scholar]
- 52.McKay JR, Van Horn D, Oslin D, et al. Extended telephone-based continuing care for alcohol dependence: 24 month outcomes and subgroup analyses. Addiction. 2011;106:1760–69. doi: 10.1111/j.1360-0443.2011.03483.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Godley MD, Godley SH. Continuing care following residential treatment: History, current practice, and emerging approaches. In: Jainchill N, editor. Understanding and treating adolescent substance use disorders. Kingston, NJ: Civic Research Institute; 2012. pp. 14-2–14-24. [Google Scholar]
- 54.Chun JS, Godley MD, Funk RR, Guydish JR. Residential treatment and continuing care for adolescent substance abusers: An analysis of CSAT’s ART initiative. Paper presented at: 2006 Joint Meeting on Adolescent Treatment Effectiveness (JMATE); March 26–29, 2006; Baltimore, MD. [Google Scholar]
- 55.Godley MD, Godley SH, Dennis ML, Funk RR, Passetti LL. A review of usual, innovative, and assertive continuing care approaches. Paper presented at: 2005 Joint Meeting on Adolescent Treatment Effectiveness (JMATE); March 21-23, 2005; Washington, DC. [Google Scholar]
- 56.Kelly JF, Myers MG, Brown SA. A multivariate process model of adolescent 12-step attendance and substance use outcome following inpatient treatment. Psychol Addict Behav. 2000;14(4):376–89. [PMC free article] [PubMed] [Google Scholar]
- 57.Kelly JF, Myers MG, Brown SA. Do adolescents affiliate with 12-step groups? A multivariate process model of effects. J Stud Alcohol. 2002;63:293–304. doi: 10.15288/jsa.2002.63.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kelly JF, Myers MG, Brown SA. The effects of age composition of 12-step groups on adolescent 12-step participation and substance use outcome. J Child Adolesc Subst Abuse. 2005;15:63–72. doi: 10.1300/J029v15n01_05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ralph N, McMenamy C. Treatment outcomes in an adolescent chemical dependency program. Adolescence. 1996;31:91–107. [PubMed] [Google Scholar]
- 60.Sealock MD, Gottfredson DC, Gallagher CA. Drug treatment for juvenile offenders: Some good and bad news. J Res Crime Delinq. 1997;34:210–36. [Google Scholar]
- 61.Whitney SD, Kelly JF, Myers MG, Brown SA. Parental substance use, family support and outcome following treatment for adolescent psychoactive substance use disorders. J Child Adolesc Subst Abuse. 2002;11:67–81. [Google Scholar]
- 62.Winters KC, Stinchfield RD, Latimer WW, Lee S. Long-term outcome of substance dependent youth following 12-step treatment. J Subst Abuse Treat. 2007;33:61–69. doi: 10.1016/j.jsat.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 63.Godley SH, Godley MD, Karvinen T, et al. The Assertive Continuing Care protocol: A clinician’s manual for working with adolescents after residential treatment of alcohol and other substance use disorders. 2nd. Bloomington, IL: Lighthouse Institute; 2006. [Google Scholar]
- 64.Godley SH, Meyers RJ, Smith JE, et al. The Adolescent Community Reinforcement Approach (ACRA) for adolescent cannabis users. Vol. 4. Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration; 2001. (DHHS Publication No (SMA) 01-3489, Cannabis Youth Treatment (CYT) Manual Series). [Google Scholar]
- 65.Godley MD, Godley SH, Dennis ML, Funk RR, Passetti LL. The effect of Assertive Continuing Care (ACC) on continuing care linkage, adherence and abstinence following residential treatment for adolescents. Addiction. 2006;102:81–93. doi: 10.1111/j.1360-0443.2006.01648.x. [DOI] [PubMed] [Google Scholar]
- 66.Godley MD, Godley SH, Dennis ML, Funk RR, Passetti LL, Petry N. A randomized trial of Assertive Continuing Care and contingency management for adolescents with substance use disorders. J Consult Clin Psychol. 2014;82:40–51. doi: 10.1037/a0035264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Garnick DW, Lee MT, Chalk M, et al. Establishing the feasibility of performance measures for alcohol and other drugs. J Subst Abuse Treat. 2002;23:375–85. doi: 10.1016/s0740-5472(02)00303-3. [DOI] [PubMed] [Google Scholar]
- 68.Kaminer Y, Napolitano C. Dial for therapy: Aftercare for adolescent substance use disorders. J Am Acad Child Adolesc Psychiatry. 2004;43:171–74. doi: 10.1097/01.chi.0000133260.98666.bf. [DOI] [PubMed] [Google Scholar]
- 69.Kaminer Y, Napolitano C. Brief telephone continuing care therapy for adolescents. Center City, MN: Hazelden; 2010. [Google Scholar]
- 70.Burleson JA, Kaminer Y, Burke RH. Twelve-month follow-up of aftercare for adolescents with alcohol use disorders. J Subst Abuse Treat. 2012;42(1):78–86. doi: 10.1016/j.jsat.2011.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Godley SH, Garner BR, Passetti LL, Funk RR, Dennis ML, Godley MD. Adolescent outpatient treatment and continuing care: Main findings from a randomized clinical trial. Drug Alcohol Depend. 2010;110(1–2):44–54. doi: 10.1016/j.drugalcdep.2010.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Henderson CE, Wevodau AL, Henderson SE, et al. An independent replication of the Adolescent Community Reinforcement Approach with justice-involved youth. Am J Addict. 2016;25(3):233–40. doi: 10.1111/ajad.12366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Brown PC, Budney AJ, Thostenson JD, Stanger C. Initiation of abstinence in adolescents treated for marijuana use disorders. J Subst Abuse Treat. 2013;44:384–90. doi: 10.1016/j.jsat.2012.08.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kaminer Y, Ohannessian CM, Burke RH. Adolescents with cannabis use disorders: Adaptive treatment for poor responder outcomes. Paper presented at: 2016 College on Problems of Drug Dependence (CPDD) Annual Meeting; June 11-16, 2016; Palm Springs, CA. [Google Scholar]
- 75.McKay JR. Treating substance use disorders with adaptive continuing care. Washington, DC: American Psychological Association; 2009. [Google Scholar]
- 76.Garner BR, Godley MD, Passetti LL, Funk RR, White WL. Recovery support for adolescents with substance use disorders: The impact of recovery support telephone calls provided by pre-professional volunteers. J Subst Abuse Alcohol. 2014;2(2):1010. [PMC free article] [PubMed] [Google Scholar]
- 77.Chi FW, Kaskutas LA, Sterling S, Campbell CI, Weisner C. Twelve-step affiliation and three-year substance use outcomes among adolescents: Social support and religious service attendance as potential mediators. Addiction. 2009;104:927–39. doi: 10.1111/j.1360-0443.2009.02524.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kelly JF, Myers MG, Rodolico J. What do adolescents exposed to Alcoholics Anonymous think about 12-step groups? Subst Abuse. 2008;29:53–62. doi: 10.1080/08897070802093122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kelly JF, Dow SJ, Yeterian JD, Kahler CW. Can 12-step group participation strengthen and extend the benefits of adolescent addiction treatment? A prospective analysis. Drug Alcohol Depend. 2010;110:117–25. doi: 10.1016/j.drugalcdep.2010.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kelly JF, Urbanoski K. Youth recovery contexts: The incremental effects of 12-step attendance and involvement on adolescent outpatient outcomes. Alcohol Clin Exp Res. 2012;36(7):1219–29. doi: 10.1111/j.1530-0277.2011.01727.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Passetti LL, Godley SH. Adolescent substance abuse treatment clinicians’ self-help meeting referral practices and adolescent attendance rates. J Psychoactive Drugs. 2008;40:29–40. doi: 10.1080/02791072.2008.10399759. [DOI] [PubMed] [Google Scholar]
- 82.Kelly JF, Dow SJ, Yeterian JD, Myers M. How safe are adolescents at Alcoholics Anonymous and Narcotics Anonymous meetings? A prospective investigation with outpatient youth. J Subst Abuse Treat. 2011;40:419–25. doi: 10.1016/j.jsat.2011.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lynch KG, Van Horn D, Drapkin M, et al. Moderators of response to extended telephone continuing care for alcoholism. Am J Health Behav. 2010;34(6):788–800. doi: 10.5993/ajhb.34.6.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.McKay JR, Lynch KG, Shepard DS, et al. The effectiveness of telephone-based continuing care in the clinical management of alcohol and cocaine use disorders: 12-month outcomes. J Consult Clin Psychol. 2004;72:967–79. doi: 10.1037/0022-006X.72.6.967. [DOI] [PubMed] [Google Scholar]
- 85.Stanger C, Budney AJ. Contingency management approaches for adolescent SUD. Child Adolesc Psychiatr Clin N Am. 2010;19:547–62. doi: 10.1016/j.chc.2010.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Douglas-Siegel JA, Ryan JP. The effect of recovery coaches for substance-involved mothers in child welfare: Impact on juvenile delinquency. J Subst Abuse Treat. 2013;45:381–87. doi: 10.1016/j.jsat.2013.05.010. [DOI] [PubMed] [Google Scholar]
- 87.Ryan JP, Choi S, Hong J, Hernandez P, Larrison C. Recovery coaches and substance exposure at birth. Child Abuse Negl. 2008;32(11):1072–79. doi: 10.1016/j.chiabu.2007.12.011. [DOI] [PubMed] [Google Scholar]
- 88.White WL. Sponsor, recovery coach, addiction counselor: The importance of role clarity and role integrity. Philadelphia, PA: Philadelphia Department of Behavioral Health and Mental Retardation Services; 2006. [Google Scholar]


