Abstract
Over the past decade, the dental field has benefited from recent findings in stem cell biology and tissue engineering that led to the elaboration of novel ideas and concepts for the regeneration of dental tissues or entire new teeth. In particular, stem cell-based regenerative approaches are extremely promising since they aim at the full restoration of lost or damaged tissues, ensuring thus their functionality. These therapeutic approaches are already applied with success in clinics for the regeneration of other organs and consist of manipulation of stem cells and their administration to patients. Stem cells have the potential to self-renew and to give rise to a variety of cell types that ensure tissue repair and regeneration throughout life. During the last decades, several adult stem cell populations have been isolated from dental and periodontal tissues, characterized, and tested for their potential applications in regenerative dentistry. Here we briefly present the various stem cell-based treatment approaches and strategies that could be translated in dental practice and revolutionize dentistry.
1. Introduction
Repair of dental pulp and periodontium remains an immense clinical challenge since human teeth have a very limited capacity to regenerate [1]. Current therapeutic interventions in dentistry are based on sophisticated biomaterials and implants with still questionable efficacy and durability [2–5]. Moreover, these therapies do not always allow the appropriate physiological function of the tooth organ. Therefore, there is an enormous unmet need for innovative methods enabling a balance between new dental tissue formation and unaltered physiological functions of the tooth organ [6, 7].
In order to reconstruct such natural structures we need to have a deep knowledge of the cellular and molecular events linked to odontogenesis. Classical experiments have shown that teeth form as a result of sequential and reciprocal interactions between cells of the oral epithelium and neural crest-derived mesenchyme [8]. Epithelial cells differentiate into enamel-forming ameloblasts, while mesenchymal cells give rise to the dental pulp, the dentin-secreting odontoblasts, and the periodontal ligament cells that anchor the tooth to the surrounding alveolar bone [8, 9]. The dental pulp forms a connective tissue that conveys vascularization and innervation and hosts stem cells that are capable of regenerating this tissue, as well as the dentin [1]. Sensory nerves from the trigeminal ganglia (TG) and sympathetic nerves from the superior cervical ganglia innervate the adult teeth [10–12]. During odontogenesis, nerve fibers emanate from the TG project towards the developing tooth germs and progressively surround them without entering the dental pulp. The first axons penetrate the dental pulp when odontoblasts differentiate and enamel deposition starts. Dental pulp innervation is completed soon after tooth eruption into the oral cavity [10], a process that is concomitant with root growth, cementum matrix deposition, and periodontium formation [7].
A common issue in dental practice is the infection and the subsequent extirpation of the dental pulp. Since structures and cells within the dental pulp provide trophic support, sensation, and defense against the various pathogens, devitalized teeth (e.g., after classical endodontic therapy) are subject to severe complications that cause tooth fragility and fracture [13]. It becomes thus evident that the maintenance of dental pulp vitality is of prime importance and therefore new regenerative approaches have started to be experimented in endodontic clinics in the last few years [14]. These new regenerative techniques could also apply in other dental disciplines, where current treatment options are based on a constantly increasing number of dental biomaterials and implants [1–4]. For example, tooth loss caused after severe traumatic injuries, periodontitis (i.e., a severe inflammation of the periodontium), advanced carious lesions, age-related alternations, or cancer [6, 7, 15–19] could be resolved by whole new tooth regeneration.
2. Stem Cell-Based Regenerative Dentistry
Regeneration involves the replacement of a pathologic tissue, as well as the reconstruction of a missing or lost tissue, by a new one that can ensure its biological function [20]. Regenerative approaches are based on the potential of human stem cells to self-renew and give rise to a diversity of cell types under appropriate conditions [21]. Throughout life, adult stem cells support tissue homeostasis and repair upon injury [6, 22, 23]. Therefore, adult stem cells from different tissues have been isolated, characterized, and tested for their potential applications in regenerative medicine [20]. In particular, mesenchymal stem cells (MSCs) have been the subject of intense investigation due to their accessibility and their potential to differentiate towards the chondrogenic, osteogenic, adipogenic, myogenic, and neurogenic lineages [24].
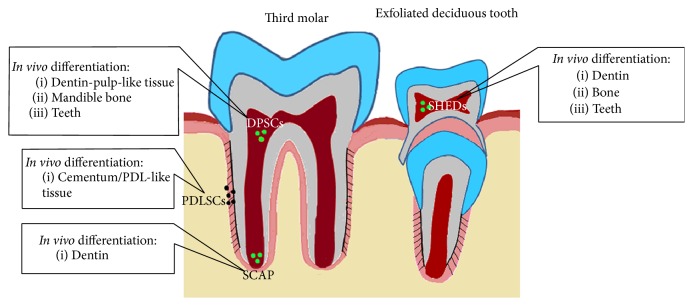
Different stem cell populations have been isolated from human adult teeth (Figure 1). The dental pulp of third molars is the most common source of dental mesenchymal stem cells, the so called dental pulp stem cells (DPSCs) [25]. Human DPSCs are able to differentiate into odontoblasts, osteoblasts, adipocytes, chondrocytes, and other cell types both in vitro and in vivo [26–28]. Other populations of dental MSCs (i.e., SHEDs) have been isolated from dental pulp of exfoliated deciduous teeth and from the apical part of the papilla (i.e., SCAPs), similar to the DPSCs differentiation potential [29–31]. Dental MSCs have been also isolated from the periodontal ligament (i.e., periodontal ligament stem cells, PDLSCs) that have the capacity to give rise to cementum/PDL-like tissue in vivo [32, 33].
Figure 1.
Schematic representation of the main stem cell sources in the human teeth and their differentiation potential in vivo. DPSCs: dental pulp stem cells, SHEDs: stem cells from human exfoliated deciduous teeth, PDLSCs: periodontal ligament stem cells, and SCAP: stem cells from the apical part of the papilla.
The behavior and properties of stem cells are strongly influenced by the surrounding environment, the so-called stem cell niche [24, 34, 35]. This specific microenvironment is a combination of cells, extracellular matrix, and growth factors that is under the influence by mechanical and chemical stresses [24]. Niches maintain and regulate the balance between stem cell self-renewal and differentiation [35]. In this context, considerable effort is produced to understand how the different components of the niches regulate stem cell function. Among these actors, innervation could play an important role in the fate and function of stem cells [36–42], thus affecting regenerative events. For example, recent studies have shown that parasympathetic nerves regulate progenitor cells and are necessary for the development and regeneration of the salivary glands [37, 39]. Similarly, it has been demonstrated that innervation is essential for the development and maintenance of taste buds [43–46]. Although the role of innervation in the initiation, development, and regeneration of teeth is still highly controversial [34, 47–49], it has been recently shown that sensory nerves regulate MSCs in mouse incisors [42]. Therefore, it is important to better study the role of innervation in tooth regeneration and most particularly its effect in dental stem cell populations. At the same time, it is of equal importance to ensure proper reinnervation of the regenerated dental tissues. Vascularization represents another key aspect of tooth regeneration. The dental pulp is richly vascularized, and teeth depend on blood supply for nutrients and oxygen transport. In addition, blood vessels allow the transport of systemic signals and the recruitment of inflammatory and other circulatory cells into the niches that can strongly affect stem cell function [35]. Blood vessels within the pulp are associated with the so-called perivascular stem cell niches. These niches host MSCs that contribute to the homeostasis and the regeneration of the dental pulp [42, 50]. The growth of blood vessels and nerves often proceeds in parallel, sharing the same paths through tissues [51]. Teeth are peculiar organs in the sense that innervation and vascularization display extremely divergent timing. While blood vessels are found in the pulp of tooth germs during early developmental stages, innervation is established only at late stages of odontogenesis [6, 52]. As both innervation and vascularization are fundamental for tooth physiology and pathology, the identification of the mechanisms that regulate these two processes will be fundamental in the light of partial (e.g., pulp regeneration) or full tooth regeneration.
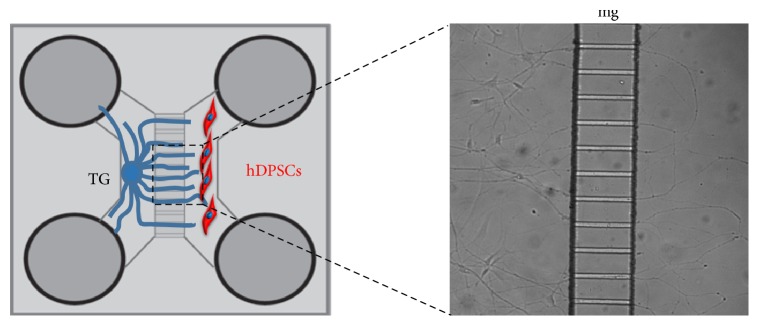
Several in vivo and in vitro studies have provided important information about the patterns of innervation of dental tissues in different animal models as well as the main molecules involved in nerve trophic support, repulsion, and attraction [10, 53–56]. To date, little information is available concerning the effects of innervation on human dental stem cells [57]. Cocultures have been used and constitute a valuable method to investigate and manipulate the interactions between nerve fibers and target tissues of human origin in a controlled and isolated environment (Figure 2) [57, 58]. The use of these and other state-of-the-art techniques, in combination with in vivo approaches in animal models, will allow gaining fundamental knowledge regarding the role of innervation in stem cell behavior and the mechanisms that drive tooth reinnervation [6]. To date, only very few studies investigating the possibility of restoring innervation in damaged teeth have been conducted [59].
Figure 2.
Schematic representation of coculture between trigeminal ganglia (TG) and human dental pulp stem cells (hDPSCs) through microfluidic devices. In this system, both cell types/tissues are cultured in optimal conditions, while allowing the growth of trigeminal ganglia axons through microgrooves (mg) to innervate the stem cells.
Pulp revascularization is currently used as a method for its regeneration in not yet fully developed teeth [59]. In this approach, pulp revascularization is induced by filling the empty root canal with a blood clot. Although already in the clinical practice, this method is characterized by low efficiency and by ectopic mineralization within the pulp [59]. Moreover, a major issue that accompanies these revascularization approaches is the connection with the circulation system [59]. Tissue engineering approaches that exploit combinations of functionalized scaffolds and dental stem cells are providing promising results, ensuring variable degrees of pulp regeneration and vascularization in vivo in animal models [60–62]. In these studies, good vascularization and connection with the circulatory system were observed, thus suggesting that such approaches could ensure proper trophic support to the regenerated dental tissues [60, 61].
3. Clinical Implications: How the Knowledge Obtained from These Approaches Could Be Used
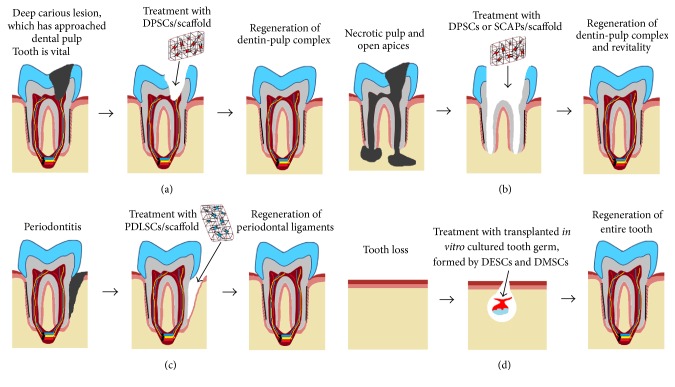
Stem cell-based therapies are very promising long-term alterative in dentistry since they could offer full restoration of dental tissues keeping thus the structural integrity, physiology, and function of the intact teeth. In vivo studies in animals have demonstrated the potential of different tooth stem cells populations for the regeneration of specific dental tissues, such as dentin, pulp, periodontium, or even the entire tooth organ [59, 60, 63–66] (Figure 3). These regenerative approaches that have been successfully tested in animal models could be also applied to humans. It is obvious that these treatments will necessitate a sufficient number of specific stem cell populations that will be transplanted to damaged and pathological dental sites, alone or together with scaffolds.
Figure 3.
Schematic representation of different stem cell-based approaches for partial or whole tooth regeneration after pathologies and tooth loss using transplantation of tooth stem cells combined with scaffolds. The various dental pathologies: (a) carious lesion, (b) necrotic pulp, (c) periodontitis, and (d) tooth loss. DPSCs, dental pulp stem cells; PDLSCs, periodontal ligament stem cells; SCAP, stem cells from the apical part of the papilla; DESCs, dental epithelial stem cells; DMSCs, dental mesenchymal stem cells.
It is worth noting that stem cell-based approaches have already started to be applied with success in other medical disciplines [67–70]. In dentistry, several specialties took advantage of the recent progress in the fields of stem cell biology and tissue engineering and developed innovative strategies for restoring the full function and physiology of specific dental tissues. For example, regenerative endodontics focuses on reestablishment of dental pulp vitality and new dentin formation using DPSCs/SCAPs combined with scaffolds loaded with bioactive molecules [26, 71–75]. These new procedures allow the transplanted stem cells to differentiate into pulp fibroblasts and odontoblasts and progressively fill the empty pulp chamber after pulpotomy or pulpectomy, thus allowing root growth in not yet fully developed teeth [63, 71, 76–78] (Figure 3). Several clinical attempts based on the bleeding technique and focused in pulp regeneration have been successfully applied in immature teeth with pulp necrosis and mature teeth with apical lesions [71, 78–80]. In this procedure, the blood clot acts as a scaffold that delivers stem cells into the empty root canal.
Although the use of stem cell-based techniques has started to be applied in endodontic clinics, these approaches are still at the animal experimental level for other dental specialties such as in periodontology. For example, while the potential of human PDLSCs or other stem cell populations for periodontal tissue regeneration has been evidenced in animal models [81–84], there are not equivalent trials yet in clinics (Figure 3).
Similarly, although attempts for the regeneration of entire brand new teeth have been successfully performed the last few years in small animal models [85, 86] dental implants still monopolize and offer the therapeutic solution after tooth loss in clinics. However, it is obvious that the ideal therapy after tooth loss would be the regeneration of an entire tooth, and therefore a bigger effort should be produced towards these revolutionary stem cell-based approaches. These novel techniques tested in mice have shown that dental mesenchymal and epithelial stem cells combined with collagen drops or scaffolds in vitro allows the formation of tooth germs that thereafter could be transplanted into the alveolar bone, where the tooth germs will develop, erupt, and finally become entire functional teeth [85, 86] (Figure 3). The application of this technique in humans has some limitations. The biggest challenge is the time needed for human tooth regeneration, since the whole process of odontogenesis in humans takes more than 7 years [1, 17]. This may represent a discouragement for patients looking for a quick replacement of the missing teeth.
4. Conclusion
Stem cell-based therapies represent the most promising alternative for successful regeneration of damaged or pathological dental tissues or even the entire tooth following tooth loss. It is therefore fundamental to understand the exact mechanisms underlying the potential of the various dental stem cell populations as well as their behavior after transplantation in ectopic sites. Innervation and vascularization play fundamental roles in the regulation of stem cell niches homeostasis, thus affecting the fate and behavior of stem cells [34, 87]. Therefore, it would be of great interest to further investigate the role of innervation in these processes. Stem cell-based approaches are only starting to emerge in dentistry, and huge challenges and problems such the enamel and entire tooth regeneration should be overcome. The majority of the experimental attempts mentioned above were exclusively performed in small animal models and thus they cannot be directly translated into the clinics yet. Nevertheless, stem cell-based regenerative approaches are the future of dentistry that will benefit millions of patients worldwide.
Acknowledgments
This work was supported by funds of the University of Zurich.
Competing Interests
The authors declare no conflict of interests.
Authors' Contributions
All authors equally contributed to the planning, writing, critical reading, and editing of the present paper.
References
- 1.Mitsiadis T. A., Orsini G., Jimenez-Rojo L. Stem cell-based approaches in dentistry. European Cells and Materials. 2015;30:248–257. doi: 10.22203/ecm.v030a17. [DOI] [PubMed] [Google Scholar]
- 2.Adell R., Eriksson B., Lekholm U., Brånemark P. I., Jemt T. Long-term follow-up study of osseointegrated implants in the treatment of totally edentulous jaws. The International Journal of Oral & Maxillofacial Implants. 1990;5(4):347–359. [PubMed] [Google Scholar]
- 3.Catón J., Bostanci N., Remboutsika E., De Bari C., Mitsiadis T. A. Future dentistry: cell therapy meets tooth and periodontal repair and regeneration. Journal of Cellular and Molecular Medicine. 2011;15(5):1054–1065. doi: 10.1111/j.1582-4934.2010.01251.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dodson T. B. Predictors of dental implant survival. Journal of the Massachusetts Dental Society. 2006;54(4):34–38. [PubMed] [Google Scholar]
- 5.Jiménez-Rojo L., Granchi Z., Woloszyk A., Filatova A., Pagella P., Mitsiadis T. A. Regenerative Dentistry: Stem Cells meet Nanotechnology. chapter 1. Boca Raton, Fla, USA: Pan Stanford; 2016. [Google Scholar]
- 6.Pagella P., Neto E., Lamghari M., Mitsiadis T. A. Investigation of orofacial stem cell niches and their innervation through microfluidic devices. European Cells and Materials. 2015;29:213–223. doi: 10.22203/ecm.v029a16. [DOI] [PubMed] [Google Scholar]
- 7.Mitsiadis T. A., Harada H. Regenerated teeth: the future of tooth replacement. An update. Regenerative Medicine. 2015;10(1):5–8. doi: 10.2217/rme.14.78. [DOI] [PubMed] [Google Scholar]
- 8.Mitsiadis T. A., Graf D. Cell fate determination during tooth development and regeneration. Birth Defects Research Part C: Embryo Today: Reviews. 2009;87(3):199–211. doi: 10.1002/bdrc.20160. [DOI] [PubMed] [Google Scholar]
- 9.Nanci A. Ten Cate's Oral Histology: Development, Structure, and Function. 8th. Louis, Mo, USA: Elsevier; 2013. [Google Scholar]
- 10.Mohamed S. S., Atkinson M. E. A histological study of the innervation of developing mouse teeth. Journal of Anatomy. 1983;136(4):735–749. [PMC free article] [PubMed] [Google Scholar]
- 11.Luukko K. Immunohistochemical localization of nerve fibres during development of embryonic rat molar using peripherin and protein gene product 9.5 antibodies. Archives of Oral Biology. 1997;42(3):189–195. doi: 10.1016/S0003-9969(97)00004-6. [DOI] [PubMed] [Google Scholar]
- 12.Johnsen D. C. Innervation of teeth: qualitative, quantitative, and developmental assessment. Journal of Dental Research. 1985;64:555–563. doi: 10.1177/002203458506400410. [DOI] [PubMed] [Google Scholar]
- 13.Ricketts D. Management of the deep carious lesion and the vital pulp dentine complex. British Dental Journal. 2001;191(11):606–610. doi: 10.1038/sj.bdj.4801246. [DOI] [PubMed] [Google Scholar]
- 14.Potdar P. D., Jethmalani Y. D. Human dental pulp stem cells: applications in future regenerative medicine. World Journal of Stem Cells. 2015;7(5):839–851. doi: 10.4252/wjsc.v7.i5.839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mao J. J., Robey P. G., Prockop D. J. Stem cells in the face: tooth regeneration and beyond. Cell Stem Cell. 2012;11(3):291–301. doi: 10.1016/j.stem.2012.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Scheller E. L., Krebsbach P. H., Kohn D. H. Tissue engineering: state of the art in oral rehabilitation. Journal of Oral Rehabilitation. 2009;36(5):368–389. doi: 10.1111/j.1365-2842.2009.01939.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mitsiadis T. A., Papagerakis P. Regenerated teeth: the future of tooth replacement? Regenerative Medicine. 2011;6(2):135–139. doi: 10.2217/rme.10.101. [DOI] [PubMed] [Google Scholar]
- 18.Marec-Berard P., Azzi D., Chaux-Bodard A. G., Lagrange H., Gourmet R., Bergeron C. Long-term effects of chemotherapy on dental status in children treated for nephroblastoma. Pediatric Hematology and Oncology. 2005;22(7):581–588. doi: 10.1080/08880010500198848. [DOI] [PubMed] [Google Scholar]
- 19.Matalova E., Fleischmannova J., Sharpe P. T., Tucker A. S. Tooth agenesis: from molecular genetics to molecular dentistry. Journal of Dental Research. 2008;87(7):617–623. doi: 10.1177/154405910808700715. [DOI] [PubMed] [Google Scholar]
- 20.Jiménez-Rojo L., Granchi Z., Woloszyk A., Filatova A., Pagella P., Mitsiadis T. A. Regenerative Dentistry: Stem Cells meet Nanotechnology. chapter 1. Pan Standford; 2009. [Google Scholar]
- 21.Uccelli A., Moretta L., Pistoia V. Mesenchymal stem cells in health and disease. Nature Reviews Immunology. 2008;8(9):726–736. doi: 10.1038/nri2395. [DOI] [PubMed] [Google Scholar]
- 22.Blau H. M., Brazelton T. R., Weimann J. M. The evolving concept of a stem cell: entity or function? Cell. 2001;105(7):829–841. doi: 10.1016/s0092-8674(01)00409-3. [DOI] [PubMed] [Google Scholar]
- 23.Zhang Y. D., Chen Z., Song Y. Q., Liu C., Chen Y. P. Making a tooth: growth factors, transcription factors, and stem cells. Cell Research. 2005;15(5):301–316. doi: 10.1038/sj.cr.7290299. [DOI] [PubMed] [Google Scholar]
- 24.Mitsiadis T. A., Barrandon O., Rochat A., Barrandon Y., De Bari C. Stem cell niches in mammals. Experimental Cell Research. 2007;313(16):3377–3385. doi: 10.1016/j.yexcr.2007.07.027. [DOI] [PubMed] [Google Scholar]
- 25.Huang G. T.-J., Gronthos S., Shi S. Mesenchymal stem cells derived from dental tissues vs. those from other sources: their biology and role in regenerative medicine. Journal of Dental Research. 2009;88(9):792–806. doi: 10.1177/0022034509340867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gronthos S., Mankani M., Brahim J., Robey P. G., Shi S. Postnatal human dental pulp stem cells (DPSCs) in vitro and in vivo. Proceedings of the National Academy of Sciences of the United States of America. 2000;97(25):13625–13630. doi: 10.1073/pnas.240309797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Batouli S., Miura M., Brahim J., et al. Comparison of stem-cell-mediated osteogenesis and dentinogenesis. Journal of Dental Research. 2003;82(12):976–981. doi: 10.1177/154405910308201208. [DOI] [PubMed] [Google Scholar]
- 28.D'Aquino R., De Rosa A., Lanza V., et al. Human mandible bone defect repair by the grafting of dental pulp stem/progenitor cells and collagen sponge biocomplexes. European Cells and Materials. 2009;18:75–83. doi: 10.22203/ecm.v018a07. [DOI] [PubMed] [Google Scholar]
- 29.Miura M., Gronthos S., Zhao M., et al. SHED: stem cells from human exfoliated deciduous teeth. Proceedings of the National Academy of Sciences of the United States of America. 2003;100(10):5807–5812. doi: 10.1073/pnas.0937635100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cordeiro M. M., Dong Z., Kaneko T., et al. Dental pulp tissue engineering with stem cells from exfoliated deciduous teeth. Journal of Endodontics. 2008;34(8):962–969. doi: 10.1016/j.joen.2008.04.009. [DOI] [PubMed] [Google Scholar]
- 31.Sonoyama W., Liu Y., Fang D., et al. Mesenchymal stem cell-mediated functional tooth regeneration in Swine. PLoS ONE. 2006;1, article e79 doi: 10.1371/journal.pone.0000079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Seo B.-M., Miura M., Gronthos S., et al. Investigation of multipotent postnatal stem cells from human periodontal ligament. The Lancet. 2004;364(9429):149–155. doi: 10.1016/s0140-6736(04)16627-0. [DOI] [PubMed] [Google Scholar]
- 33.Wang L., Shen H., Zheng W., et al. Characterization of stem cells from alveolar periodontal ligament. Tissue Engineering—Part A. 2011;17(7-8):1015–1026. doi: 10.1089/ten.tea.2010.0140. [DOI] [PubMed] [Google Scholar]
- 34.Pagella P., Jiménez-Rojo L., Mitsiadis T. A. Roles of innervation in developing and regenerating orofacial tissues. Cellular and Molecular Life Sciences. 2014;71(12):2241–2251. doi: 10.1007/s00018-013-1549-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jones D. L., Wagers A. J. No place like home: anatomy and function of the stem cell niche. Nature Reviews Molecular Cell Biology. 2008;9(1):11–21. doi: 10.1038/nrm2319. [DOI] [PubMed] [Google Scholar]
- 36.Méndez-Ferrer S., Lucas D., Battista M., Frenette P. S. Haematopoietic stem cell release is regulated by circadian oscillations. Nature. 2008;452(7186):442–447. doi: 10.1038/nature06685. [DOI] [PubMed] [Google Scholar]
- 37.Knox S. M., Lombaert I. M. A., Reed X., Vitale-Cross L., Gutkind J. S., Hoffman M. P. Parasympathetic innervation maintains epithelial progenitor cells during salivary organogenesis. Science. 2010;329(5999):1645–1647. doi: 10.1126/science.1192046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Martínez-Martínez E., Galván-Hernández C. I., Toscano-Márquez B., Gutiérrez-Ospina G. Modulatory role of sensory innervation on hair follicle stem cell progeny during wound healing of the rat skin. PloS one. 2012;7(5) doi: 10.1371/journal.pone.0036421.e36421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Knox S. M., Lombaert I. M. A., Haddox C. L., et al. Parasympathetic stimulation improves epithelial organ regeneration. Nature Communications. 2013;4, article 1494 doi: 10.1038/ncomms2493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Katayama Y., Battista M., Kao W.-M., et al. Signals from the sympathetic nervous system regulate hematopoietic stem cell egress from bone marrow. Cell. 2006;124(2):407–421. doi: 10.1016/j.cell.2005.10.041. [DOI] [PubMed] [Google Scholar]
- 41.Brownell I., Guevara E., Bai C. B., Loomis C. A., Joyner A. L. Nerve-derived sonic hedgehog defines a niche for hair follicle stem cells capable of becoming epidermal stem cells. Cell Stem Cell. 2011;8(5):552–565. doi: 10.1016/j.stem.2011.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhao H., Feng J., Seidel K., et al. Secretion of shh by a neurovascular bundle niche supports mesenchymal stem cell homeostasis in the adult mouse incisor. Cell Stem Cell. 2014;14(2):160–173. doi: 10.1016/j.stem.2013.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Oakley B., Witt M. Building sensory receptors on the tongue. Journal of Neurocytology. 2005;33(6):631–646. doi: 10.1007/s11068-005-3332-0. [DOI] [PubMed] [Google Scholar]
- 44.Oakley B., Brandemihl A., Cooper D., Lau D., Lawton A., Zhang C. The morphogenesis of mouse vallate gustatory epithelium and taste buds requires BDNF-dependent taste neurons. Developmental Brain Research. 1998;105(1):85–96. doi: 10.1016/S0165-3806(97)00178-8. [DOI] [PubMed] [Google Scholar]
- 45.Sun H., Oakley B. Development of anterior gustatory epithelia in the palate and tongue requires epidermal growth factor receptor. Developmental Biology. 2002;242(1):31–43. doi: 10.1006/dbio.2001.0526. [DOI] [PubMed] [Google Scholar]
- 46.Mistretta C. M., Goosens K. A., Farinas I., Reichardt L. F. Alterations in size, number, and morphology of gustatory papillae and taste buds in BDNF null mutant mice demonstrate neural dependence of developing taste organs. Journal of Comparative Neurology. 1999;409(1):13–24. [PMC free article] [PubMed] [Google Scholar]
- 47.Løes S., Kettunen P., Kvinnsland I., Luukko K. Mouse rudimentary diastema tooth primordia are devoid of peripheral nerve fibers. Anatomy and Embryology. 2002;205(3):187–191. doi: 10.1007/s00429-002-0247-8. [DOI] [PubMed] [Google Scholar]
- 48.Lumsden A. G. S., Buchanan J. A. G. An experimental study of timing and topography of early tooth development in the mouse embryo with an analysis of the role of innervation. Archives of Oral Biology. 1986;31(5):301–311. doi: 10.1016/0003-9969(86)90044-0. [DOI] [PubMed] [Google Scholar]
- 49.Kollar E. J., Lumsden A. G. S. Tooth morphogenesis: the role of the innervation during induction and pattern formation. Journal de Biologie Buccale. 1979;7(1):49–60. [PubMed] [Google Scholar]
- 50.Oh M., Nör J. E. The perivascular niche and self-renewal of stem cells. Frontiers in Physiology. 2015;6, article 367 doi: 10.3389/fphys.2015.00367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Carmeliet P., Tessier-Lavigne M. Common mechanisms of nerve and blood vessel wiring. Nature. 2005;436(7048):193–200. doi: 10.1038/nature03875. [DOI] [PubMed] [Google Scholar]
- 52.Nait Lechguer A., Kuchler-Bopp S., Hu B., Haïkel Y., Lesot H. Vascularization of engineered teeth. Journal of Dental Research. 2008;87(12):1138–1143. doi: 10.1177/154405910808701216. [DOI] [PubMed] [Google Scholar]
- 53.Luukko K., Kettunen P. Coordination of tooth morphogenesis and neuronal development through tissue interactions: lessons from mouse models. Experimental Cell Research. 2014;325(2):72–77. doi: 10.1016/j.yexcr.2014.02.029. [DOI] [PubMed] [Google Scholar]
- 54.Lillesaar C., Eriksson C., Johansson C. S., Fried K., Hildebrand C. Tooth pulp tissue promotes neurite outgrowth from rat trigeminal ganglia in vitro. Journal of Neurocytology. 1999;28(8):663–670. doi: 10.1023/A:1007008815621. [DOI] [PubMed] [Google Scholar]
- 55.Nosrat I. V., Smith C. A., Mullally P., Olson L., Nosrat C. A. Dental pulp cells provide neurotrophic support for dopaminergic neurons and differentiate into neurons in vitro; implications for tissue engineering and repair in the nervous system. European Journal of Neuroscience. 2004;19(9):2388–2398. doi: 10.1111/j.0953-816X.2004.03314.x. [DOI] [PubMed] [Google Scholar]
- 56.Nosrat I. V., Widenfalk J., Olson L., Nosrat C. A. Dental pulp cells produce neurotrophic factors, interact with trigeminal neurons in vitro, and rescue motoneurons after spinal cord injury. Developmental Biology. 2001;238(1):120–132. doi: 10.1006/dbio.2001.0400. [DOI] [PubMed] [Google Scholar]
- 57.Pagella P., Miran S., Mitsiadis T. A. Analysis of developing tooth germ innervation using microfluidic co-culture devices. Journal of Visualized Experiments. 2015;(102) doi: 10.3791/53114.e53114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pagella P., Neto E., Jiménez-Rojo L., Lamghari M., Mitsiadis T. A. Microfluidics co-culture systems for studying tooth innervation. Frontiers in Physiology. 2014;5, article 326 doi: 10.3389/fphys.2014.00326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yang J., Yuan G., Chen Z. Pulp regeneration: current approaches and future challenges. Frontiers in Physiology. 2016;7:1–8. doi: 10.3389/fphys.2016.00058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Li X., Ma C., Xie X., Sun H., Liu X. Pulp regeneration in a full-length human tooth root using a hierarchical nanofibrous microsphere system. Acta Biomaterialia. 2016;35:57–67. doi: 10.1016/j.actbio.2016.02.040. [DOI] [PubMed] [Google Scholar]
- 61.Dissanayaka W. L., Hargreaves K. M., Jin L., Samaranayake L. P., Zhang C. The interplay of dental pulp stem cells and endothelial cells in an injectable peptide hydrogel on angiogenesis and pulp regeneration in vivo. Tissue Engineering—Part A. 2015;21(3-4):550–563. doi: 10.1089/ten.tea.2014.0154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Galler K. M., Hartgerink J. D., Cavender A. C., Schmalz G., D'Souza R. N. A customized self-assembling peptide hydrogel for dental pulp tissue engineering. Tissue Engineering—Part A. 2012;18(1-2):176–184. doi: 10.1089/ten.tea.2011.0222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zheng Y., Wang X. Y., Wang Y. M., et al. Dentin regeneration using deciduous pulp stem/progenitor cells. Journal of Dental Research. 2012;91(7):676–682. doi: 10.1177/0022034512449834. [DOI] [PubMed] [Google Scholar]
- 64.Iwata T., Yamato M., Tsuchioka H., et al. Periodontal regeneration with multi-layered periodontal ligament-derived cell sheets in a canine model. Biomaterials. 2009;30(14):2716–2723. doi: 10.1016/j.biomaterials.2009.01.032. [DOI] [PubMed] [Google Scholar]
- 65.Akita D., Kano K., Saito-Tamura Y., et al. Use of rat mature adipocyte-derived dedifferentiated fat cells as a cell source for periodontal tissue regeneration. Frontiers in Physiology. 2016;7:1–12. doi: 10.3389/fphys.2016.00050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wang W., Dang M., Zhang Z., et al. Dentin regeneration by stem cells of apical papilla on injectable nanofibrous microspheres and stimulated by controlled BMP-2 release. Acta Biomaterialia. 2016;36:63–72. doi: 10.1016/j.actbio.2016.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Forbes S. J., Rosenthal N. Preparing the ground for tissue regeneration: from mechanism to therapy. Nature Medicine. 2014;20(8):857–869. doi: 10.1038/nm.3653. [DOI] [PubMed] [Google Scholar]
- 68.Nishida K., Yamato M., Hayashida Y., et al. Corneal reconstruction with tissue-engineered cell sheets composed of autologous oral mucosal epithelium. The New England Journal of Medicine. 2004;351(12):1187–1196. doi: 10.1056/nejmoa040455. [DOI] [PubMed] [Google Scholar]
- 69.Frank M. H., Frank N. Y. Restoring the cornea from limbal stem cells. Regenerative Medicine. 2015;10(1):1–4. doi: 10.2217/rme.14.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Eming S. A., Martin P., Tomic-Canic M. Wound repair and regeneration: mechanisms, signaling, and translation. Science Translational Medicine. 2014;6(265) doi: 10.1126/scitranslmed.3009337.265sr6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chrepa V., Henry M. A., Daniel B. J., Diogenes A. Delivery of apical mesenchymal stem cells into root canals of mature teeth. Journal of Dental Research. 2015;94(12):1653–1659. doi: 10.1177/0022034515596527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Peters O. A. Translational opportunities in stem cell-based endodontic therapy: where are we and what are we missing? Journal of Endodontics. 2014;40(4):S82–S85. doi: 10.1016/j.joen.2014.01.017. [DOI] [PubMed] [Google Scholar]
- 73.Hayashi Y., Murakami M., Kawamura R., Ishizaka R., Fukuta O., Nakashima M. CXCL14 and MCP1 are potent trophic factors associated with cell migration and angiogenesis leading to higher regenerative potential of dental pulp side population cells. Stem Cell Research and Therapy. 2015;6, article 111 doi: 10.1186/s13287-015-0088-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Huang G. T.-J., Yamaza T., Shea L. D., et al. Stem/Progenitor cell-mediated de novo regeneration of dental pulp with newly deposited continuous layer of dentin in an in vivo model. Tissue Engineering—Part A. 2010;16(2):605–615. doi: 10.1089/ten.tea.2009.0518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Volponi A. A., Pang Y., Sharpe P. T. Stem cell-based biological tooth repair and regeneration. Trends in Cell Biology. 2010;20(12):715–722. doi: 10.1016/j.tcb.2010.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Iohara K., Imabayashi K., Ishizaka R., et al. Complete pulp regeneration after pulpectomy by transplantation of CD105+ stem cells with stromal cell-derived factor-1. Tissue Engineering—Part A. 2011;17(15-16):1911–1920. doi: 10.1089/ten.tea.2010.0615. [DOI] [PubMed] [Google Scholar]
- 77.Iohara K., Murakami M., Takeuchi N., et al. A novel combinatorial therapy with pulp stem cells and granulocyte colony-stimulating factor for total pulp regeneration. Stem Cells Translational Medicine. 2013;2(7):521–533. doi: 10.5966/sctm.2012-0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lovelace T. W., Henry M. A., Hargreaves K. M., Diogenes A. Evaluation of the delivery of mesenchymal stem cells into the root canal space of necrotic immature teeth after clinical regenerative endodontic procedure. Journal of Endodontics. 2011;37(2):133–138. doi: 10.1016/j.joen.2010.10.009. [DOI] [PubMed] [Google Scholar]
- 79.Deepak B. S., Nandini D. B. Stem cells: challenges in endodontics. Journal of Pharmacy and Bioallied Sciences. 2012;4(1):p. 84. doi: 10.4103/0975-7406.92744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sönmez I. S., Akbay Oba A., Erkmen Almaz M. Revascularization/regeneration performed in immature molars: case reports. Journal of Clinical Pediatric Dentistry. 2013;37(3):231–234. doi: 10.17796/jcpd.37.3.j6007761g8811453. [DOI] [PubMed] [Google Scholar]
- 81.Ding G., Liu Y., Wang W., et al. Allogeneic periodontal ligament stem cell therapy for periodontitis in swine. Stem Cells. 2010;28(10):1829–1838. doi: 10.1002/stem.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Du J., Shan Z., Ma P., Wang S., Fan Z. Allogeneic bone marrow mesenchymal stem cell transplantation for periodontal regeneration. Journal of Dental Research. 2014;93(2):183–188. doi: 10.1177/0022034513513026. [DOI] [PubMed] [Google Scholar]
- 83.Fu X., Jin L., Ma P., Fan Z., Wang S. Allogeneic stem cells from deciduous teeth in treatment for periodontitis in Miniature Swine. Journal of Periodontology. 2014;85(6):845–851. doi: 10.1902/jop.2013.130254. [DOI] [PubMed] [Google Scholar]
- 84.Khorsand A., Eslaminejad M. B., Arabsolghar M., et al. Autologous dental pulp stem cells in regeneration of defect created in canine periodontal tissue. Journal of Oral Implantology. 2013;39(4):433–443. doi: 10.1563/AAID-JOI-D-12-00027. [DOI] [PubMed] [Google Scholar]
- 85.Ikeda E., Tsuji T. Growing bioengineered teeth from single cells: potential for dental regenerative medicine. Expert Opinion on Biological Therapy. 2008;8(6):735–744. doi: 10.1517/14712598.8.6.735. [DOI] [PubMed] [Google Scholar]
- 86.Oshima M., Tsuji T. Functional tooth regenerative therapy: tooth tissue regeneration and whole-tooth replacement. Odontology. 2014;102(2):123–136. doi: 10.1007/s10266-014-0168-z. [DOI] [PubMed] [Google Scholar]
- 87.Kumar A., Brockes J. P. Nerve dependence in tissue, organ, and appendage regeneration. Trends in Neurosciences. 2012;35(11):691–699. doi: 10.1016/j.tins.2012.08.003. [DOI] [PubMed] [Google Scholar]