Abstract
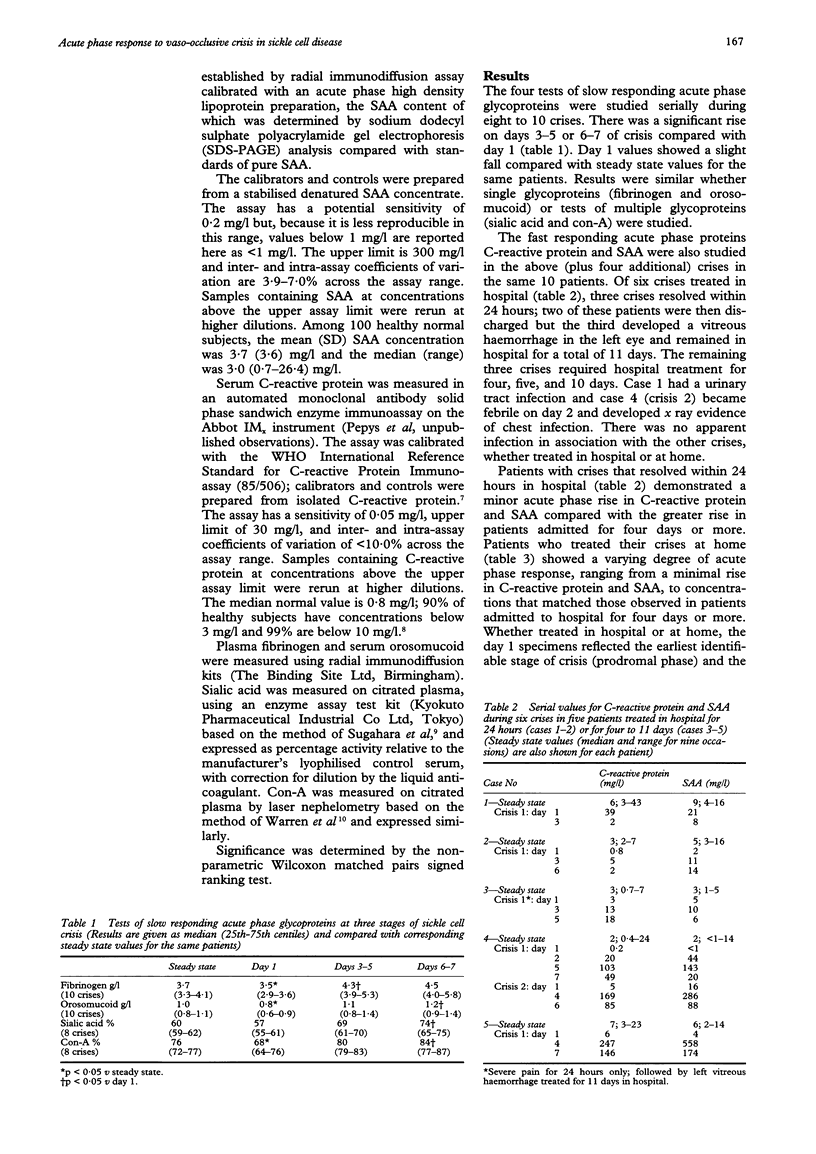
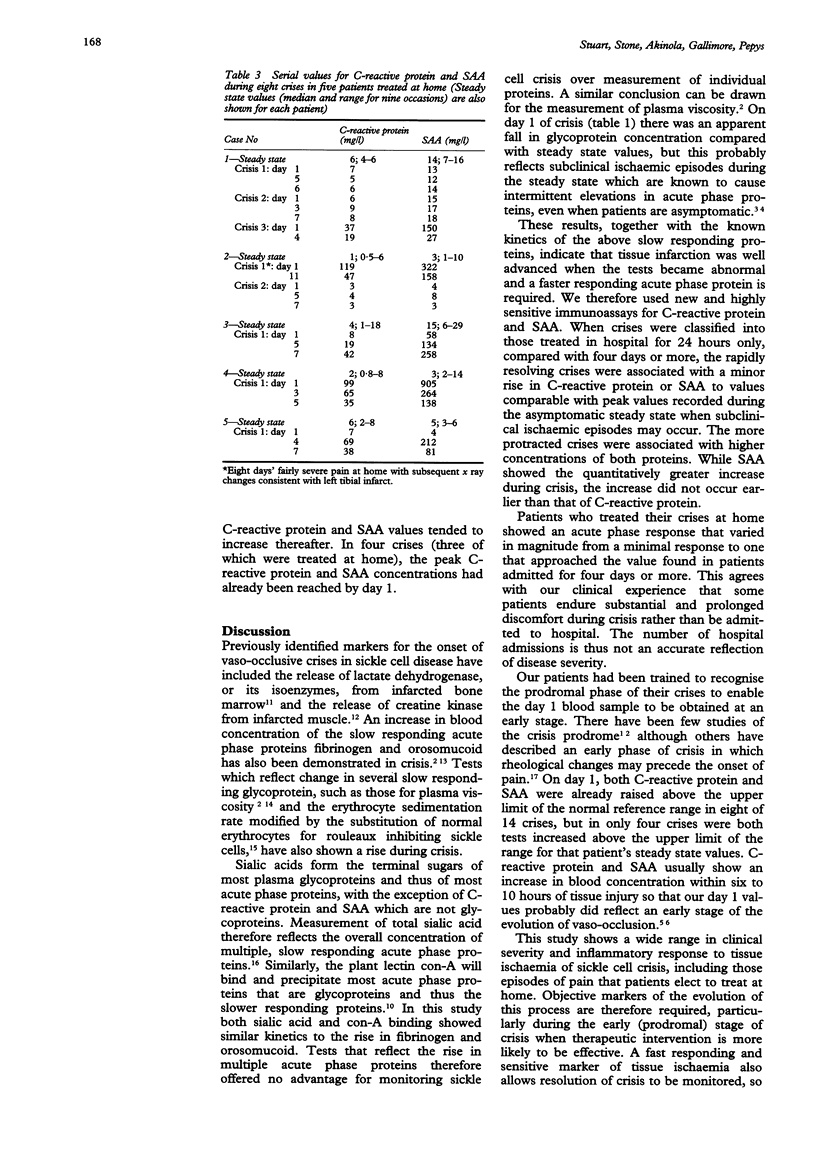
AIMS--To identify suitable acute phase proteins as objective markers of tissue ischaemia during painful vaso-occlusive crises in sickle cell disease. METHODS--The prodromal and established phases of 14 vaso-occlusive crises were studied longitudinally in 10 patients with sickle cell anaemia. Automated solid phase enzyme immunoassays were used to measure the fast responding acute phase proteins C-reactive protein and serum amyloid A protein. Slower responding glycoproteins (fibrinogen, orosomucoid, sialic acid and concanavalin-A binding) were measured in parallel. RESULTS--C-reactive protein and serum amyloid A protein increased early in crisis, sometimes within the early (prodromal) phase. Crises that resolved within 24 hours in hospital showed a minor and transient rise compared with crises that required treatment for four days or more. In eight crises treated by patients at home the acute phase response ranged from minor to a level consistent with extensive tissue ischaemia. CONCLUSIONS--Sensitive enzyme immunoassays for C-reactive protein and serum amyloid A protein are of potential value for monitoring the onset of tissue ischaemia in sickle cell crisis and for confirming subsequent resolution.
Full text
PDF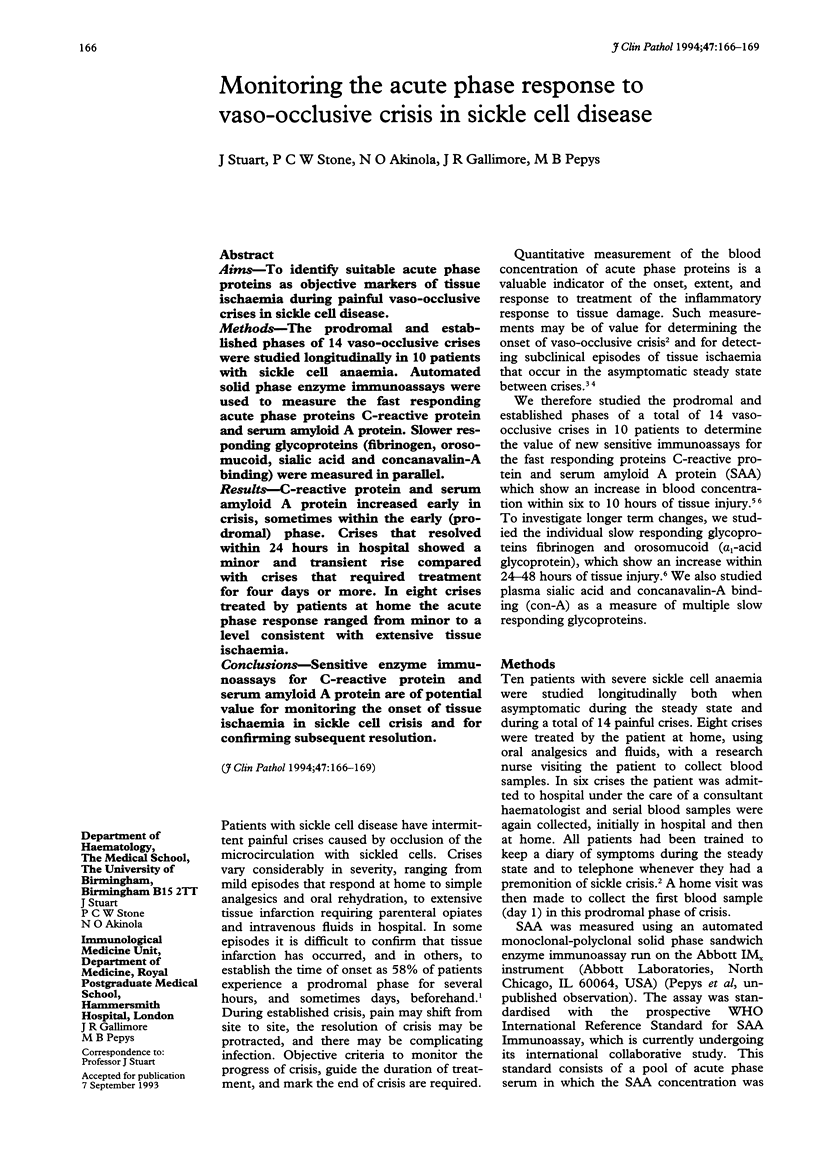
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Akinola N. O., Stevens S. M., Franklin I. M., Nash G. B., Stuart J. Rheological changes in the prodromal and established phases of sickle cell vaso-occlusive crisis. Br J Haematol. 1992 Aug;81(4):598–602. doi: 10.1111/j.1365-2141.1992.tb02998.x. [DOI] [PubMed] [Google Scholar]
- Akinola N. O., Stevens S. M., Franklin I. M., Nash G. B., Stuart J. Subclinical ischaemic episodes during the steady state of sickle cell anaemia. J Clin Pathol. 1992 Oct;45(10):902–906. doi: 10.1136/jcp.45.10.902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballas S. K., Smith E. D. Red blood cell changes during the evolution of the sickle cell painful crisis. Blood. 1992 Apr 15;79(8):2154–2163. [PubMed] [Google Scholar]
- Becton D. L., Raymond L., Thompson C., Berry D. H. Acute-phase reactants in sickle cell disease. J Pediatr. 1989 Jul;115(1):99–102. doi: 10.1016/s0022-3476(89)80339-7. [DOI] [PubMed] [Google Scholar]
- Cox M. L., Rudd A. G., Gallimore R., Hodkinson H. M., Pepys M. B. Real-time measurement of serum C-reactive protein in the management of infection in the elderly. Age Ageing. 1986 Sep;15(5):257–266. doi: 10.1093/ageing/15.5.257. [DOI] [PubMed] [Google Scholar]
- De Beer F. C., Pepys M. B. Isolation of human C-reactive protein and serum amyloid P component. J Immunol Methods. 1982;50(1):17–31. doi: 10.1016/0022-1759(82)90300-3. [DOI] [PubMed] [Google Scholar]
- Famodu A. A., Adedeji M. O., Reid H. L. Serial plasma fibrinogen changes accompanying sickle cell pain crisis. Clin Lab Haematol. 1990;12(1):43–47. doi: 10.1111/j.1365-2257.1990.tb01109.x. [DOI] [PubMed] [Google Scholar]
- Hunt B. J., Korsah P., Eaton S., Brozovic M. Creatine kinase activity in sickle cell disease. J Clin Pathol. 1989 Jul;42(7):712–715. doi: 10.1136/jcp.42.7.712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray N., May A. Painful crises in sickle cell disease--patients' perspectives. BMJ. 1988 Aug 13;297(6646):452–454. doi: 10.1136/bmj.297.6646.452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neely C. L., Wajima T., Kraus A. P., Diggs L. W., Barreras L. Lactic acid dehydrogenase activity and plasma hemoglobin elevations in sickle cell disease. Am J Clin Pathol. 1969 Aug;52(2):167–169. doi: 10.1093/ajcp/52.2.167. [DOI] [PubMed] [Google Scholar]
- Pepys M. B., Baltz M. L. Acute phase proteins with special reference to C-reactive protein and related proteins (pentaxins) and serum amyloid A protein. Adv Immunol. 1983;34:141–212. doi: 10.1016/s0065-2776(08)60379-x. [DOI] [PubMed] [Google Scholar]
- Shine B., de Beer F. C., Pepys M. B. Solid phase radioimmunoassays for human C-reactive protein. Clin Chim Acta. 1981 Nov 25;117(1):13–23. doi: 10.1016/0009-8981(81)90005-x. [DOI] [PubMed] [Google Scholar]
- Singhal A., Doherty J. F., Raynes J. G., McAdam K. P., Thomas P. W., Serjeant B. E., Serjeant G. R. Is there an acute-phase response in steady-state sickle cell disease? Lancet. 1993 Mar 13;341(8846):651–653. doi: 10.1016/0140-6736(93)90418-g. [DOI] [PubMed] [Google Scholar]
- Sugahara K., Sugimoto K., Nomura O., Usui T. Enzymatic assay of serum sialic acid. Clin Chim Acta. 1980 Dec 22;108(3):493–498. doi: 10.1016/0009-8981(80)90360-5. [DOI] [PubMed] [Google Scholar]
- Warren C., Whicher J., Kohn J. The use of concanavalin A to measure acute phase proteins by laser nephelometry. J Immunol Methods. 1980;32(2):141–150. doi: 10.1016/0022-1759(80)90067-8. [DOI] [PubMed] [Google Scholar]
- Waters P. J., Lewry E., Pennock C. A. Measurement of sialic acid in serum and urine: clinical applications and limitations. Ann Clin Biochem. 1992 Nov;29(Pt 6):625–637. doi: 10.1177/000456329202900603. [DOI] [PubMed] [Google Scholar]


