Abstract
When assessing swallowing in infants, it is critical to have confidence that the liquids presented during the swallow study closely replicate the viscosity of liquids in the infant's typical diet. However, we lack research on rheological properties of frequently used infant formulas or breastmilk, and various forms of barium contrast media used in swallow studies. The aim of the current study was to provide objective viscosity measurements for typical infant liquid diet options and barium contrast media. A TA-Instruments AR2000 Advanced Rheometer was used to measure the viscosity, five standard infant formulas, three barium products and two breastmilk samples. Additionally, this study measured the viscosity of infant formulas and breastmilk when mixed with powdered barium contrast in a 20% weight-to-volume (w/v) concentration. Study findings determined that standard infant formulas and the two breastmilk samples had low viscosities, at the lower end of the National Dysphagia Diet (NDD) thin liquid range. Two specialty formulas tested had much thicker viscosities, close to the NDD nectar-thick liquid range lower boundary. The study showed differences in viscosity between two 60% w/v barium products (Liquid E-Z-Paque® and E-Z-Paque® powder); the powdered product had a much lower viscosity, despite identical barium concentration. When E-Z-Paque® powdered barium was mixed in a 20% w/v concentration using water, standard infant formulas or breastmilk, the resulting viscosities were at the lower end of the NDD thin range, and only slightly thicker than the non-barium comparator liquids. When E-Z-Paque® powdered barium was mixed in a 20% w/v concentration with the two thicker specialty formulas (Enfamil AR 20kcal and 24 kcal), unexpected alterations in their original viscosity occurred. These findings highlight the clinical importance of objective measures of viscosity as well as objective data on how infant formulas or breastmilk may change in consistency when mixed with barium.
A modified barium swallow (MBS) is considered the gold standard for the evaluation of deglutition disorders. During a pediatric MBS, a commonly used approach is to mix barium contrast with the child’s typical diet to facilitate optimal cooperation. In addition, to maximize confidence that the MBS represents the child’s typical swallow function, it is critical that the viscosity of the food or liquid presented be as close as possible to the viscosity of the child’s typical diet. While accurate knowledge of the influence of liquid viscosity on deglutition is important for all children with dysphagia, it is particularly critical in young infants who must meet their nutrition and hydration needs exclusively through liquid intake. Yet, the field currently lacks information regarding the viscosity of liquid and powdered contrast media used in pediatric swallow studies and their rheological similarity to frequently used infant formulas or breastmilk. Previous studies highlight the importance of objective viscosity measurements of the liquid used to assess swallow function, and the fallibility of judging viscosity using subjective methods (such as visually comparing liquids based on flow from a nipple or spoon)[1, 2]. If a clinician fails to correctly match the viscosity of the infant’s home diet with the viscosity of the liquid presented during the swallow study, an inaccurate assessment of swallow function may result. Faulty identification of a deglutition disorder resulting from a mismatch between assessment and dietary liquids can have significant ramifications, both for false positive and false negative findings. This may result in unnecessary interventions or place an infant at risk for respiratory consequences.
There is presently a paucity of research literature exploring the rheological characteristics of breastmilk or infant formulas (either thin or thickened) and similarity between these products and barium stimuli used in pediatric videofluoroscopy. Cichero and colleagues [3] measured the viscosities of five different infant formulas available in Australia. Importantly, they showed considerable variation in viscosity between the different formulas, across a shear rate range from 1 to 100s−1. Two non-thickened formulas behaved essentially as Newtonian thin liquids with very low viscosities. The thickened formulas displayed shear-thinning properties with viscosities from 90–430 mPa.s at a shear rate of 50−1, placing them in the nectar to low-honey ranges of the National Dysphagia Diet categories proposed for viscosity-based liquid classification [4, 5]. At a shear rate of 50−1, which is the shear rate point used for classification in the NDD, all of the infant formulas were shown to have significant lower viscosity than liquid Polibar® barium (100% w/v concentration) [3]. The barium product was also shown to have a higher density and higher yield stress than the infant formulas. Stuart and Motz [6] compared the viscosity of 60% w/v barium (Lafayette Tonopaque powdered barium mixed with water) to Enfamil LIPIL with Iron 20 cal/oz formula. Although both of these liquids had low viscosities in the thin liquid range (i.e., < 50 mPa.s), a t-test showed the barium to be significantly thicker than the formula. It is important to note, however, that Stuart and Motz noted qualifications in their thin liquid results secondary to limitations in their viscometer. In that same study, various thickeners were added to both the formula and the barium, and in the majority of cases, the barium product was reported to have significantly higher viscosity than its paired formula comparator.
With respect to breastmilk, it is known that the makeup of breastmilk can be highly variable, while remaining within the NDD range of a thin liquid [4,5]. A variety of factors including the age of the infant, time of day, the fat composition of the mother’s diet, and fullness of the breast can impact the composition of the breastmilk, which may have consequences for viscosity [7–9]. Pasteurized breastmilk has been shown to have higher viscosities than untreated breastmilk, suggesting that temperature changes involved in freezing, thawing and warming pumped breastmilk may lead to changes in composition and consequently viscosity [7].
Current clinical guidelines do not specify a recommended weight-to-volume concentration for barium to be used in pediatric swallowing studies. Recent literature shows that higher weight-to-volume concentrations of barium have higher viscosity [2]. In a study by Baron & Alexander [10], a 20% w/v barium concentration (achieved by diluting 25 ml of 105% w/v Liquid Polibar Plus with 50 ml of water) was found to have acceptable radio-opacity. Fink & Ross [11] showed higher rates of aspiration among adult patients with dysphagia using thin liquid Varibar™ diluted to a 20% w/v concentration compared to the 40% w/v undiluted product. They questioned whether the undiluted product might be providing a therapeutic level of thickening through the increased viscosity associated with higher barium concentration and argued that it is ideal to use less concentrated barium products to evaluate the safety of swallowing with thin liquids. Applying this logic to the preparation of barium stimuli for use in pediatric swallowing studies suggests that the goal should be to use stimuli that are sufficiently radio-opaque to be reliably seen on the radiographic image, while limiting any associated influences on the taste, viscosity or other material characteristics of the test stimuli.
The purpose of this exploratory study was to understand the viscosities of several infant formulas commonly in use in the United States and their similarity to the viscosities of commercially available barium products in an undiluted 60% w/v or a diluted 20% w/v concentration. It was of further interest to understand how viscosity would differ if infant formulas were used rather than water as the solution for mixing with the barium. It is important to confirm whether adding barium powder to infant dietary liquids results in videofluoroscopy stimuli that are similar to or different from the liquids they are intended to represent. Additionally, we were interested in conducting a preliminary exploration of similar questions using breastmilk. There is currently a lack of evidence regarding the impact of viscosity differences on the physiology of swallowing in infants [12]; consequently, the clinical significance of any observed differences in instrumental measurements of viscosity in this study will be interpreted using the categorical classifications of liquid viscosity in the National Dysphagia Diet [4, 5], i.e., thin (0–50 mPa.s), nectar-thick (51–350 mPa.s) and honey-thick (351–1750 mPa.s).
Methods
Stimulus Preparation
All of the stimuli for this study were prepared in a lab according to precise instructions. Three samples of each stimulus were prepared and stored in separate plastic cups with lids for 30–60 minutes prior to rheological testing. The breastmilk and breastmilk plus barium samples were stored in a refrigerator at 4° Celsius. All other samples were stored at room temperature (25° Celsius)
a) Barium
Commercially available E-Z-Paque® barium (Bracco) was chosen for use in this study. This brand of barium was available both in a 60% w/v, 41% w/w liquid suspension form (“Liquid E-Z-Paque®) and in a 96% w/w powdered form, which comes in a 176 gram unit dose bottle marked with fill-lines for adding water to achieve concentrations ranging from 70% to 114% w/v. Based on the manufacturer instructions, a ratio of 109.38 grams of E-Z-Paque® powder to 144.21 grams of water was determined to yield 175 ml of a 60% w/v suspension. To prepare this 60% w/v powdered barium product, the required amount of barium was measured in grams in a weigh boat on a digital balance. The required amount of water (Nestlé Pure Life brand) was placed in a glass beaker on a magnetic stirrer and set to rotate at a low speed. The barium powder was gradually added during stirring. Once added, the mixture was left to stir at room temperature for 2 minutes to ensure adequate dispersion of the powdered contents in the water. Immediately following mixing, the barium was divided into three portions. To create 20% w/v barium from the E-Z-Paque® powder, 1 part of the 60% w/v reconstituted suspension was mixed with 2 parts water.
b) Infant Formulas
Table 1 shows the five different infant formulas that were included in the study, together with mixing instructions. Three of these products were standard 20 kcal while the remaining two were specialty formulas intended to reduce acid reflux and/or include fortification. Formulas that were sourced in a liquid form were shaken prior to use, as per manufacturer instructions. Powdered formulas were prepared by weighing the manufacturer recommended amount of powder in grams in a weigh boat on a digital balance, and then mixing the powder with bottled water (Nestlé Pure Life). In cases where the manufacturer instructions suggested recipes using scoops of powder, the corresponding manufacturer suggested weight of a scoop (in grams) was used to determine the amount of powder required. Formulas were shaken or stirred according to the manufacturer instructions on the label.
Table 1.
List of infant formulas included in the study
| Formula Brand | Form | Mixing Instructions |
|---|---|---|
| Similac® 20 kcal | Powder | Use 16.6 grams (2 scoops) of powder and 4 oz (118 ml) of water. Shake to mix. |
| Enfamil® 20 kcal | Liquid | Shake before use. |
| Similac Sensitive for Fussiness and Gas® |
Liquid | Shake before use. |
| Enfamil A.R. ™ 20 kcal | Powder | Use 9 grams (1 scoop) of powder and 2 oz (59 ml) of water. Shake rigorously, then allow to sit for 5 minutes. Shake again before use. |
| Enfamil A.R. ™ 24 kcal | Powder | Use 27 grams (3scoops) of powder and 5 oz (148 ml) of water. Shake rigorously, then allow to sit for 5 minutes. Shake again before use. |
c) Breastmilk
Frozen breastmilk samples were available from two donors. These samples were defrosted for 24 hours in a refrigerator prior to use. Additional information regarding time post-partum, time of pumping or other factors that might influence the characteristics of the breastmilk were unfortunately not available.
d) Formula or breastmilk plus barium
In order to prepare barium versions of the breast milk and infant formulas, two parts of the non-barium liquid were mixed with one part of 60% w/v E-Z-Paque® barium solution (prepared using powdered barium), to achieve a 20% w/v barium concentration. The non-barium sample was added to the barium liquid during mixing on a magnetic stirrer, and the mixtures were left to stir at room temperature for 10 minutes to ensure adequate dispersion of the barium within the liquid.
Rheological Testing
The viscosity of each test stimulus was measured in millipascal seconds (mPa.s) using a TA-Instruments AR2000 Advanced Rheometer (cone-and-plate geometry: 40mm, 2° cone; truncation gap: 61). Immediately prior to loading each sample on the plate, the sample was hand stirred for 10 seconds to re-suspend any sediment that might have collected at the bottom of the cup. For each test run, a uni-directional steady shear rate sweep was performed from 0.1–1000 reciprocal seconds with 10 points per decade. Each sample was tested in triplicate. Sample temperature was maintained at room temperature (25°C) using the Peltier plate on the rheometer.
The viscosity data were plotted across the shear rate sweep to enable the appreciation of overall flow characteristics (e.g., Newtonian, non-Newtonian, shear thinning) and the comparison of apparent viscosity at 50s−1.
Results
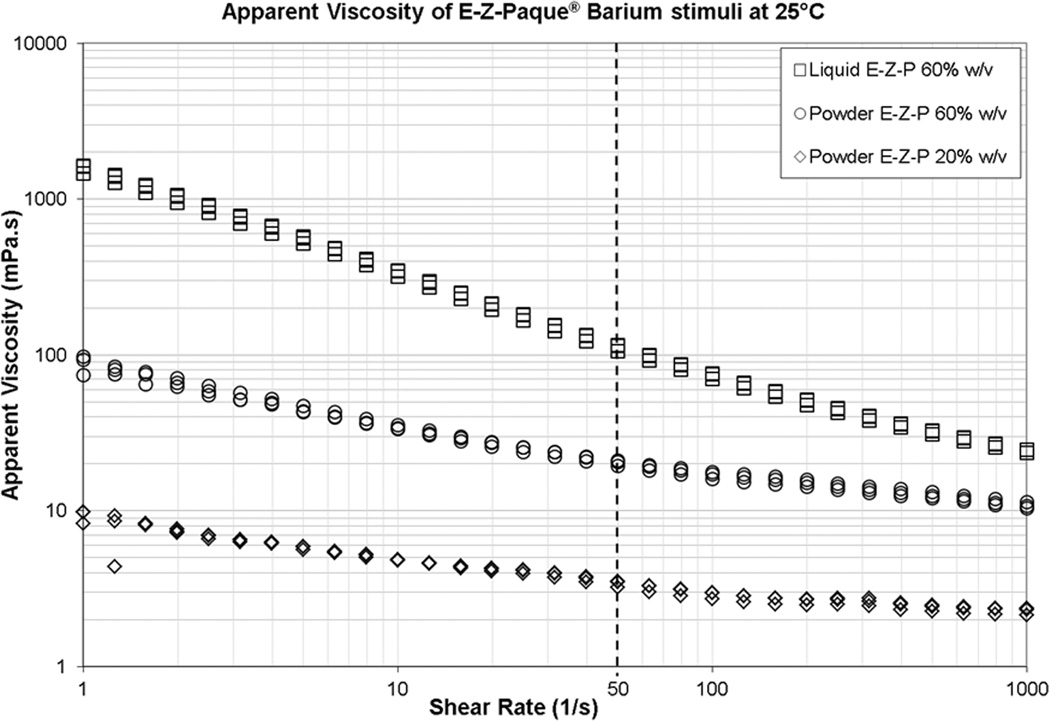
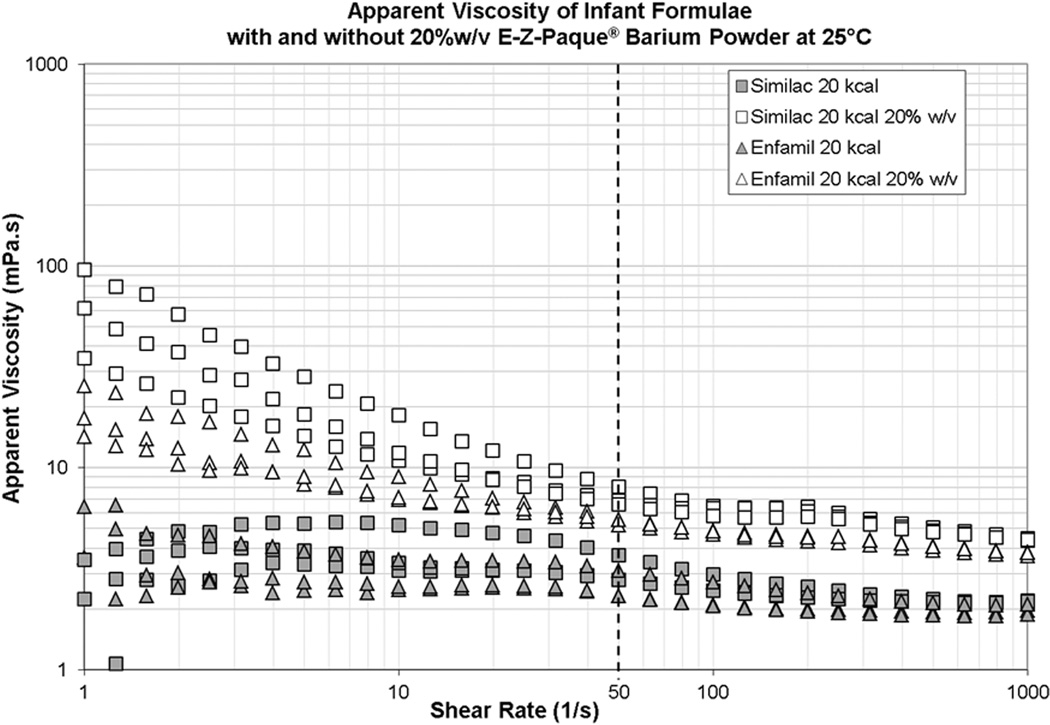
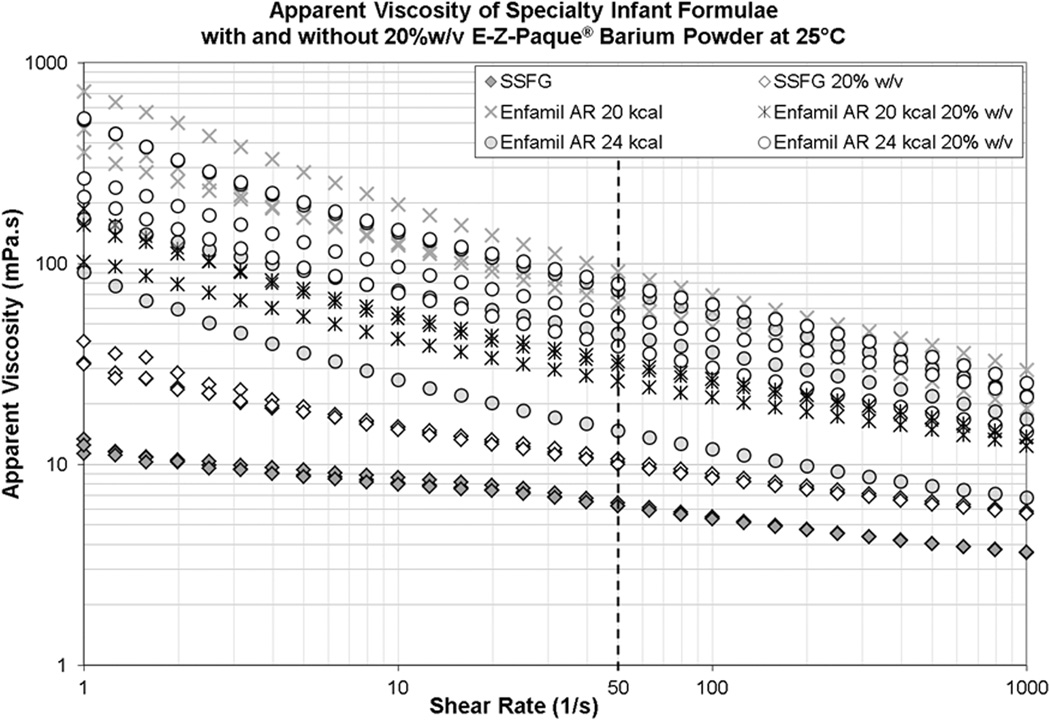
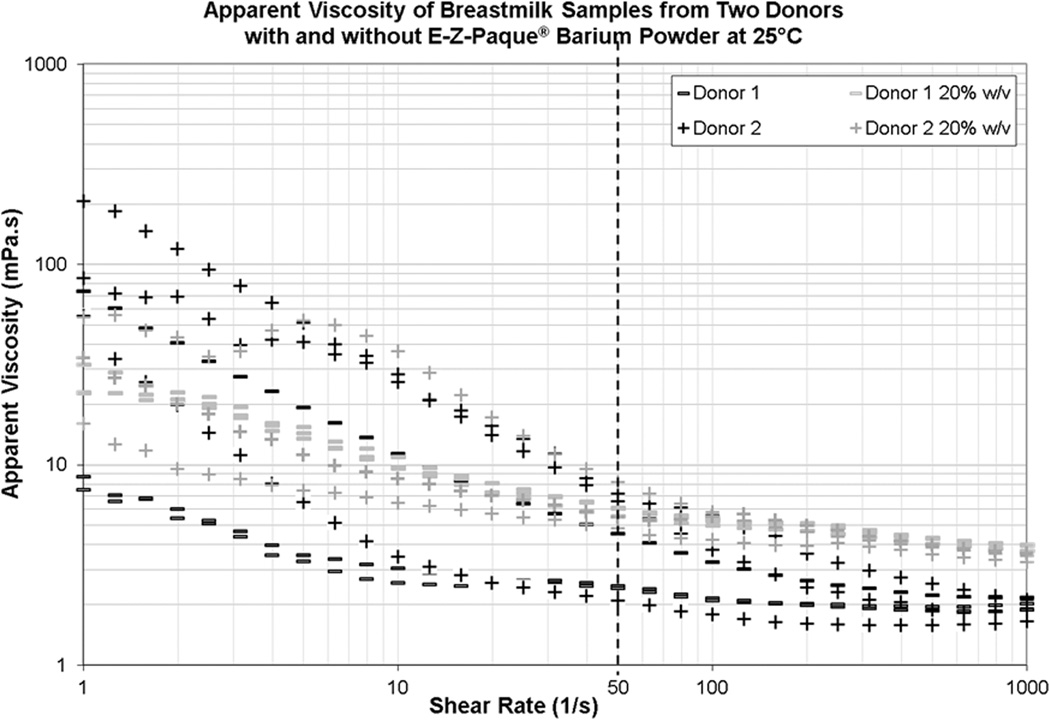
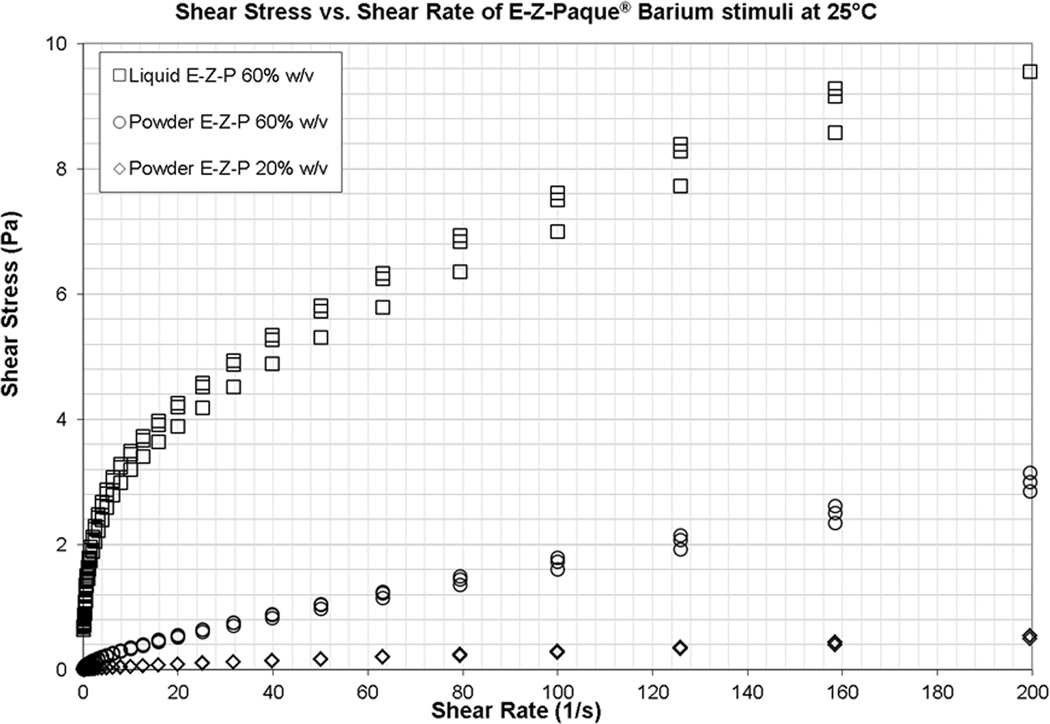
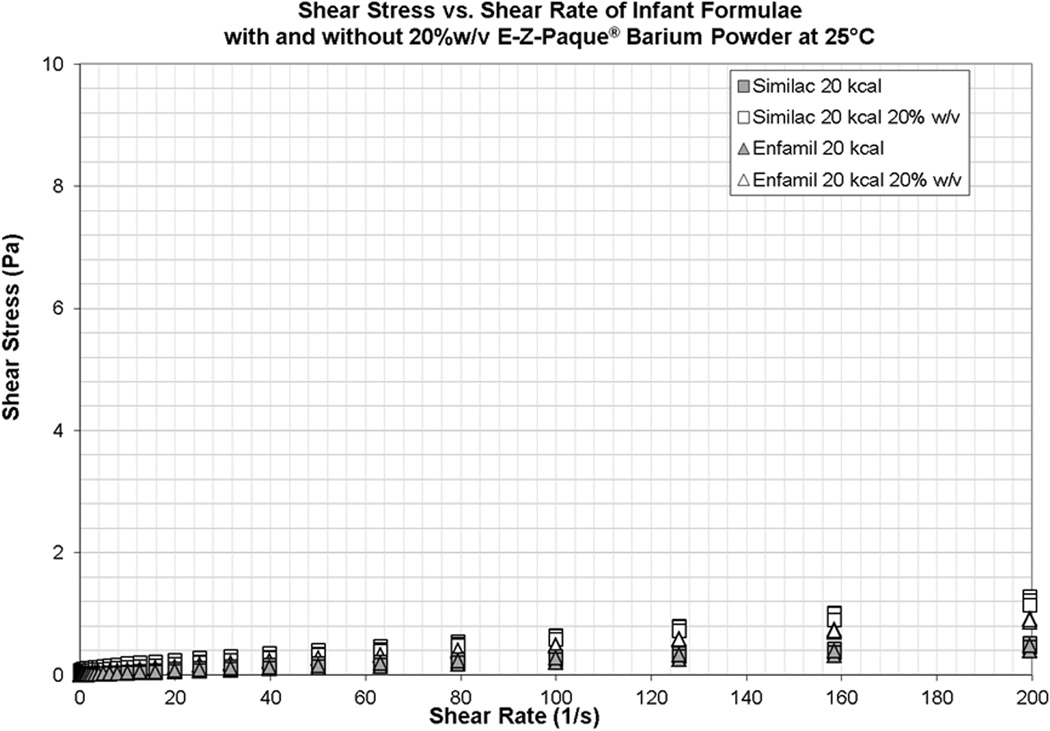
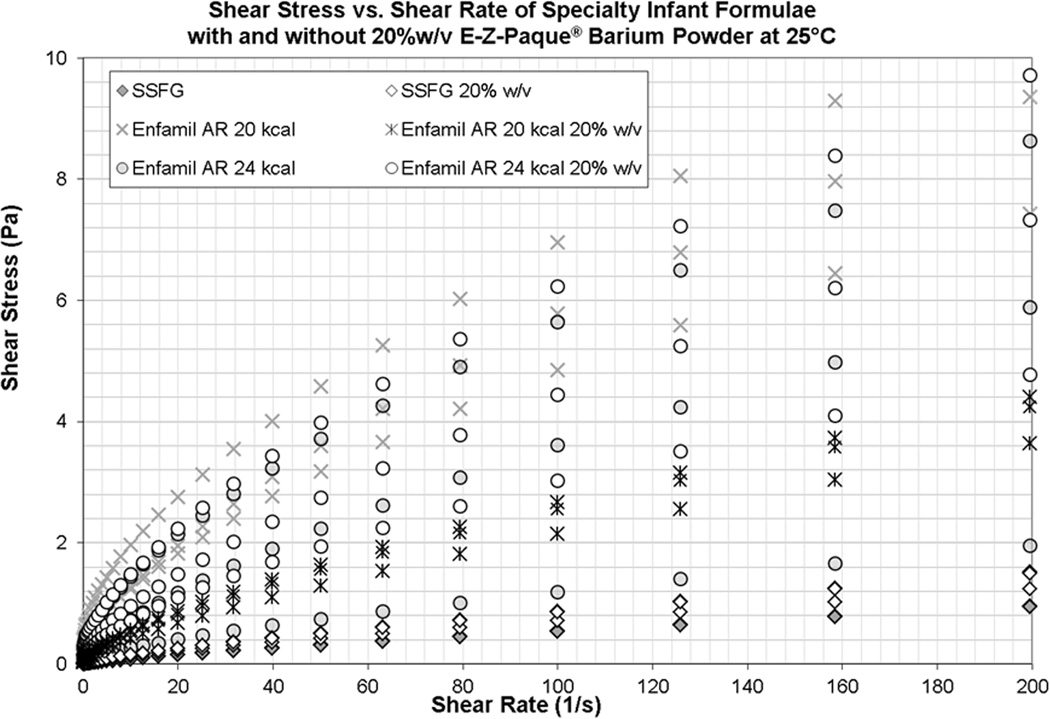
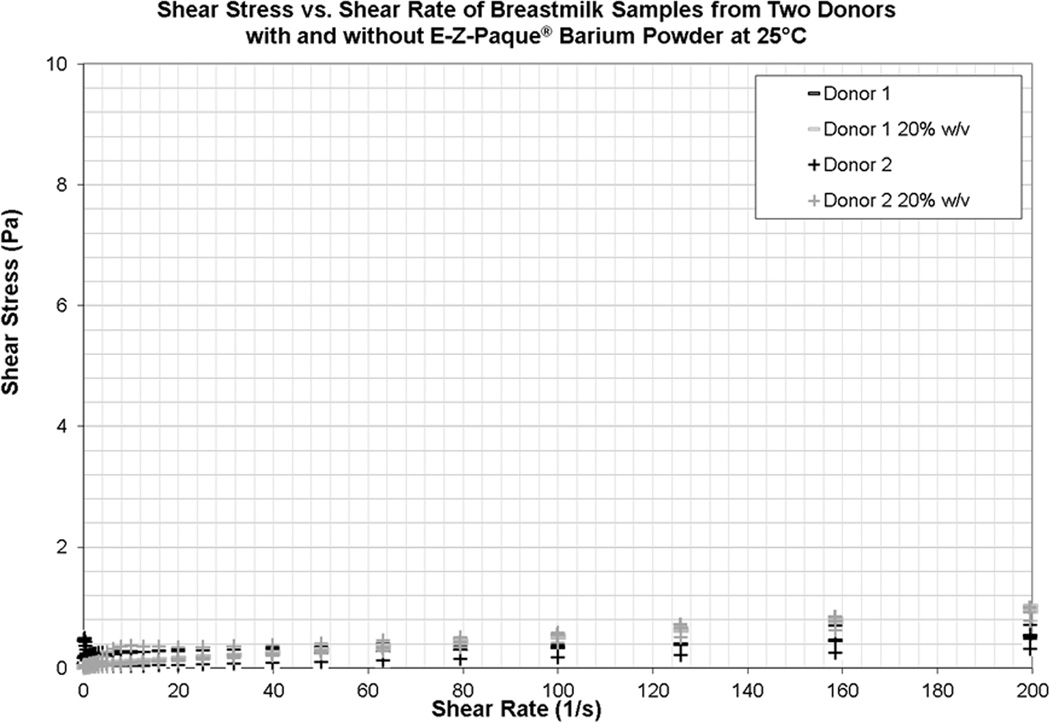
Viscosity measurements (mean, standard deviation) for all rheological tests are shown in millipascal seconds in Table 2 with grey shaded rows containing information about non-barium products and white shaded rows containing information about barium stimuli. Charts illustrating the viscosity of the different test stimuli across a shear rate range from 0.1–1000 reciprocal seconds are provided in Figures 1 a, b, c and d. These log-log plots show shear rate along the x-axis and apparent viscosity in mPa.s on the y-axis. Figure 1a illustrates the viscosities of the barium products. Figures 1 b, c and d each show a subset of the remaining stimuli (regular formulas, specialty formulas or breastmilk), with each plot showing both the non-barium liquid and the liquid plus 20% w/v barium stimulus. The comparison point of 50 reciprocal seconds is highlighted by a dashed black vertical line on each figure.
Table 2.
Viscosity measurements (Mean (SD) in mPa.s) at shear rates of 30, 50 and 100 reciprocal seconds
| Test Liquid | Shear Rate | NDD Classification |
||
|---|---|---|---|---|
| 30s−1 | 50s−1 | 100s−1 | ||
| Liquid E-Z-Paque® (60% w/v concentration) | 151 (7.28) | 112 (5.35) | 74 (3.29) | Nectar-thick |
| E-Z-Paque® Powder (60% w/v concentration) | 23 (0.89) | 20 (0.83) | 17 (0.88) | Thin |
| E-Z-Paque® Powder (diluted to 20% w/v concentration) | 4 (0.13) | 3 (0.17) | 3 (0.16) | Thin |
| Similac® 20 kcal | 3 (0.76) | 3 (0.52) | 3 (0.29) | Thin |
| Similac® 20 kcal plus E-Z-Paque® Powder (20% w/v concentration) | 6 (0.32) | 5 (0.18) | 5 (0.12) | Thin |
| Enfamil® 20 kcal | 3 (0.51) | 3 (0.45) | 2 (0.37) | Thin |
| Enfamil® 20 kcal plus E-Z-Paque® Powder (20% w/v concentration) | 8 (1.22) | 7 (0.77) | 6 (0.37) | Thin |
| Enfamil AR™ 20 kcal | 91 (19.17) | 76 (14.42) | 59 (10.59) | Nectar-thick |
| Enfamil AR™ 20 kcal plus E-Z-Paque® Powder (20% w/v concentration) | 34 (4.25) | 30 (3.58) | 25 (2.73) | Thin |
| Enfamil AR™ 24 kcal | 52 (35.88) | 44 (29.67) | 35 (22.29) | Thin |
| Enfamil AR™ 24 kcal plus E-Z-Paque® Powder (20% w/v concentration) | 68 (24.29) | 58 (20.5) | 46 (16.09) | Nectar-thick |
| Similac Sensitive for Fussiness and Gas® | 7 (0.2) | 6 (0.13) | 5 (0.06) | Thin |
| Similac Sensitive for Fussiness and Gas® plus E-Z-Paque® Powder (20% w/v concentration) |
11 (0.15) | 10 (0.12) | 9 (0.08) | Thin |
| Breastmilk: Donor 1 | 4 (1.78) | 3 (1.19) | 2 (0.65) | Thin |
| Breastmilk: Donor 1 plus E-Z-Paque® Powder (20% w/v concentration) | 7 (0.37) | 6 (0.31) | 5 (0.20) | Thin |
| Breastmilk: Donor 2 | 8 (4.81) | 5 (2.77) | 4 (1.91) | Thin |
| Breastmilk: Donor 2 plus E-Z-Paque® Powder (20% w/v concentration) | 8 (3.18) | 6 (1.81) | 5 (0.85) | Thin |
Figure 1.
a) Barium Stimuli
As shown in Table 3, the viscosities of 60% w/v E-Z-Paque® barium differ considerably depending on whether the pre-mixed liquid suspension is used or whether the powdered product is prepared with water. The pre-mixed Liquid E-Z-Paque® tested with an apparent viscosity > 100 mPa.s, well into the NDD nectar-thick range. This product was almost 6 times the viscosity of the corresponding 60% w/v suspension prepared from E-Z-Paque® barium powder. Thus, despite the similarity suggested by the same brand name, the liquid and powdered versions of E-Z-Paque® barium are quite different products. Dilution of the 60% w/v E-Z-Paque® powder product to a 20% w/v concentration resulted in a product with an 85% reduction in viscosity, with values falling below 5 mPa.s, at the bottom of the NDD thin range.
b) Infant Formulas
The standard formulas, all tested with viscosities at the low end of the NDD thin liquid range under 10 mPa.s. Notably, as shown in Figure 1c, both of the standard formulas display fairly stable viscosity across the shear rate range, suggesting Newtonian flow. This is in contrast to the other stimuli, where shear thinning characteristics are clearly seen. The two specialty anti-reflux Enfamil formulas had much higher viscosities, approximating or just crossing the NDD boundary (50 mPa.s) between thin and nectar-thick liquids.
c) Breastmilk
Figure 1d shows that both of the breastmilk samples displayed much greater variability in viscosity than the infant formula samples (Figure 1c). This is particularly true at low shear rates. At 50s−1, the viscosity of both breastmilk samples tested in the thin liquid range, under 10 mPa.s.
d) Formula or breastmilk plus barium
With the exception of the two Enfamil AR™ formulas, the addition of 20% w/v barium either to infant formula or breastmilk resulted in increased viscosity at all three shear rates listed in Table 2. On average, these increases were in the order of 3 mPa.s at 50s−1, with a range from a 0.2 to 1.3-fold increase relative to the non-barium product. Despite these increases, all of these 20% w/v stimuli remained at the low end of the thin range, below 12 mPa.s. There were no obvious differences in the behavior of the breastmilk samples compared to the infant formulas when barium was added.
The two Enfamil AR™ formulas showed different behaviors. The 20 kcal product showed an unusual pattern of thinner viscosity with the addition of 20% w/v barium, crossing back from the NDD nectar-thick range into the thin category. The 24 kcal product showed the opposite trend of thickening, and this was sufficient to place the barium product in the NDD nectar-thick range.
Discussion
The findings of this study underscore that clinicians should not rely on subjective impressions or assumptions regarding the viscosity or similarity in viscosity of infant dietary liquids or barium preparations [13–15]. Although none of these liquids had a viscosity of 1 mPa.s (viscosity of water) the majority of non-barium liquids in this study tested with viscosities at the low end (i.e. < 10 mPa.s) of the thin liquid range defined in the National Dysphagia Diet. Specifically, the two standard infant formulas displayed essentially Newtonian flow properties, similar to water. By contrast, the two specialty formulas tested were shown to have much higher viscosity than the standard formulas.
An unexpected and important result of the current study was the observation that pre-mixed Liquid E-Z-Paque® (in its non-diluted 60% w/v concentration) is much more viscous than a 60% w/v concentration barium made from powdered E-Z-Paque®. Although the similarity in brand name might lead a clinician to assume that these two barium products are equivalent, it is clear that the powdered product is different from the pre-mixed liquid suspension.
This study was primarily motivated by the clinical need to match viscosity between the liquids presented during an infant’s MBS and the viscosity of the infant’s typical diet. The findings provide assurance that several commercially available infant formulas (Similac® 20 kcal, Similac Sensitive for Fussiness and Gas®, and Enfamil® 20 kcal) fall within the NDD range for thin liquids in their non-barium form, and that the addition of 20% w/v E-Z-Paque® barium results in slight thickening, but not sufficient to reach the NDD nectar-thick liquids category. This provides reassurance that when barium is prepared for infant videofluoroscopies using a ratio of 1 part E-Z-Paque® barium suspension (prepared in a 60% w/v concentration from the powdered product) to 2 parts of formula (Similac® 20 kcal, Similac Sensitive for Fussiness and Gas®, or Enfamil® 20 kcal), the resulting barium will have a thin viscosity that is similar to the non-barium liquids. Clinicians can, therefore, have greater confidence in clinical recommendations regarding safety with these formulas that are made on the basis of observing swallowing with the corresponding barium stimuli. Similar results were seen with the two breastmilk samples, suggesting that the addition of 20% w/v barium should not dramatically alter the viscosity of breastmilk. However, given previous evidence that breastmilk can be highly variable in its composition; this interpretation should be made with caution.
The data showed much higher viscosity measures for Enfamil AR™ 20 kcal and Enfamil AR™ 24 kcal, with mean rheological test values falling between 44 and 76 mPa.s at 50s−1, both of which are close to the NDD boundary between thin and nectar thick liquids, 50mPa.s. Both the Enfamil AR™ 20 and 24 kcal also displayed greater variations in viscosity as shown by larger standard deviations across rheological trials (see Table 2). These specialty formulas showed greater changes in viscosity with the addition of 20% w/v barium. The variations observed suggest some instability in the product for reasons that are unknown. However, recent studies have shown that the viscosity of milk products varies based on protein and fat content [16, 17]. Given fact that the Enfamil AR™ specialty formulas involve elements designed to reduce acid reflux and/or provide caloric fortification, it is tempting to speculate that protein or fat content may be contributing to increased viscosity. Certainly, clinicians cannot assume that specialty formulas have a thin liquid viscosity, either in their natural state or following the addition of barium.
Limitations
In this study, the question of similarity or differences between the viscosities of different stimuli has been interpreted with reference to the liquid flow categories proposed in the National Dysphagia Diet [4, 5]. It must be highlighted that these categorical boundaries for consistencies are consensus based. To date, there are no specific value boundaries in viscosity that have been demonstrated to result in clear, measurable differences in swallowing behavior [12]. Furthermore, the clinical relevance of systematic or statistically significant differences in viscosity between liquids, is not known, particularly when these differences are small. Future research to establish the magnitudes of difference in viscosity or other rheological characteristics that lead to clinical changes in flow or swallowing safety is needed.
Breastmilk
Breastmilk samples were included in the current study due to the important role they play in infant nutrition worldwide, but this aspect of the study should be treated with caution and considered very preliminary. As mentioned in the introduction, the literature suggests that breastmilk can be highly variable in its composition across women and related to factors such as time post-partum, diet, and breast fullness. As such, samples from only two donors, for whom detailed information regarding these factors was not available, cannot be considered adequate for representing the diversity in breastmilk composition that exists, and which plausibly would affect viscosity. There is certainly a need for future studies to investigate this issue thoroughly so that clinicians can be better informed regarding the impact of variations in breastmilk properties on swallowing function in infants with dysphagia.
Yield Stress and Density
Previous literature regarding the rheological and material characteristics of items used in dysphagia management has pointed out that there are other parameters, in addition to viscosity, which may be relevant [12, 18–20]. Among these, yield stress (i.e., a stress threshold that must be surpassed before flow begins) and density have been proposed as important. These characteristics were not measured in the current study. However, post-hoc explorations of possible yield stress were conducted by examining shear stress vs. shear rate plots, which can be found in Figures 2a, b, c and d. These plots suggest negligible yield stress overall, with flow for most stimuli beginning at or very close to the 0 Pa level on the y-axis. A slightly elevated threshold is seen for the 60% w/v Liquid E-Z-Paque® product (Figure 2a).
Figure 2.
Conclusion
In conclusion, this study supports the idea that barium stimuli used in pediatric videofluoroscopy should be carefully prepared to promote the closest possible match in flow properties to liquids in the infant’s diet. The data show that different dietary liquids vary in their flow properties, and that similarity cannot be assumed. Instrumental measures of viscosity, density, and yield stress are technically complex, time consuming, costly, and not readily available to the broader clinical population. This study highlights the need for accurate and practical methods of testing the clinically relevant aspects of liquid consistency, while still remaining objective. This is particularly critical in the pediatric population when uses of familiar dietary products in assessment are known to facilitate optimal participation and maximize confidence that the MBS represents the child’s typical swallow function. Confidence in the match between videofluoroscopy test stimuli and standard dietary liquids is required to minimize the risk of an inaccurate assessment of swallow function that may result in unnecessary intervention(s) or place an infant at risk for respiratory consequences.
Acknowledgments
The authors gratefully acknowledge assistance from Kimberly Ng and Dr. David James with the rheological testing conducted for this study. The authors also gratefully acknowledge Daniel Stool and Jared Fry from Intertek, without whose initial rheological testing this study would not have been possible.
Conflicts of Interest
The 4th and 5th authors (CEAB and CMS) acknowledge funding from Bracco Canada to develop resources for clinicians using barium products in clinical practice.
References
- 1.Popa Nita S, Murith M, Chisholm H, Engmann J. Matching the rheological properties of videofluoroscopic contrast agents and thickened liquid prescriptions. Dysphagia. 2013;28:245–252. doi: 10.1007/s00455-012-9441-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Steele CM, Molfenter SM, Peladeau-Pigeon M, Stokely S. Challenges in preparing contrast media for videofluoroscopy. Dysphagia. 2013;28:464–467. doi: 10.1007/s00455-013-9476-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cichero J, Nicholson T, Dodrill P. Liquid Barium is not Representative of Infant Formula: Characterisation of Rheological and Material Properties. Dysphagia. 2011;26(3):264–271. doi: 10.1007/s00455-010-9303-3. [DOI] [PubMed] [Google Scholar]
- 4.Felt P. The National Dysphagia Diet: The science and practice. Nutrition in Clinical Practice. 1999;14:S60–S63. [Google Scholar]
- 5.National Dysphagia Diet: Standardization for Optimal Care. Diana Faulhaber: American Dietetic Association; 2002. [Google Scholar]
- 6.Stuart S, Motz JM. Viscosity in infant dysphagia management: comparison of viscosity of thickened liquids used in assessment and thickened liquids used in treatment. Dysphagia. 2009;24:412–422. doi: 10.1007/s00455-009-9219-y. [DOI] [PubMed] [Google Scholar]
- 7.de Almeida MBM, de Almeida JAG, Moreira MEL, Novak FR. Adequacy of human milk viscosity to respond to infants with dysphagia: Experimental study. Journal of Applied Oral Science. 2011;19:554–559. doi: 10.1590/S1678-77572011000600003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kent JC, Mitoulas LR, Cregan MD, Ramsay DT, Doherty DA, Hartmann PE. Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics. 2006;117:e387–e395. doi: 10.1542/peds.2005-1417. [DOI] [PubMed] [Google Scholar]
- 9.McDaniel MR, Barker E, Lederer CL. Sensory characterization of human milk. J Dairy Sci. 1989;72:1149–1158. doi: 10.3168/jds.S0022-0302(89)79218-3. [DOI] [PubMed] [Google Scholar]
- 10.Baron J, Alexander T. Effects of powdered versus liquid barium on the viscosity of fluids used in modified swallow studies. Canadian Association of Radiologists Journal. 2003;54:152–155. [PubMed] [Google Scholar]
- 11.Fink TA, Ross JB. Are we testing a true thin liquid? Dysphagia. 2009;24:285–289. doi: 10.1007/s00455-008-9203-y. [DOI] [PubMed] [Google Scholar]
- 12.Steele CM, Alsanei WA, Ayanikalath S, Barbon CE, Chen J, Cichero JA, Coutts K, Dantas RO, Duivestein J, Giosa L, Hanson B, Lam P, Lecko C, Leigh C, Nagy A, Namasivayam AM, Nascimento WV, Odendaal I, Smith CH, Wang H. The influence of food texture and liquid consistency modification on swallowing physiology and function: a systematic review. Dysphagia. 2015;30:2–26. doi: 10.1007/s00455-014-9578-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brown A, Mills RH, Daubert CR, Casper ML. Establishing labels and standards for thickened liquids in the dysphagia diet. Consultant Dietitian. 1998;23:1–5. [Google Scholar]
- 14.Mills RH. Increasing the precision of the videofluoroscopic swallowing examination. In: Mills RH, editor. Evaluation of dysphagia in adults: Expanding the diagnostic options. Austin, TX: Pro-Ed; 2000. pp. 103–144. [Google Scholar]
- 15.Mills RH. Rheology Overview: Control of Liquid Viscosities in Dysphagia Management. Nutrition in Clinical Practice. 1999;14:S52–S56. [Google Scholar]
- 16.Hadde EK, Nicholson TM, Cichero JAY. Rheological characterisation of thickened fluids under different temperature, pH and fat contents. Nutrition & Food Science. 2015;45:270–285. [Google Scholar]
- 17.Hadde EK, Nicholson TM, Cichero JAY, Deblauwe C. Rheological characterisation of thickened milk components (protein, lactose and minerals) J Food Eng. 2015;166:263–267. [Google Scholar]
- 18.Cichero JAY, Hay G, Murdoch BE, Halley PJ. Videofluoroscopy fluids versus mealtime fluids: Differences in viscosity and density made clear. Journal of Medical Speech Language Pathology. 1997;5:203–215. [Google Scholar]
- 19.Steele CM, Van Lieshout PH, Goff HD. The rheology of liquids: a comparison of clinicians' subjective impressions and objective measurement. Dysphagia. 2003;18:182–195. doi: 10.1007/s00455-002-0104-1. [DOI] [PubMed] [Google Scholar]
- 20.Nicosia MA, Robbins JA. The fluid mechanics of bolus ejection from the oral cavity. Journal of Biomechanics. 2001;34:1537–1544. doi: 10.1016/s0021-9290(01)00147-6. [DOI] [PubMed] [Google Scholar]