Abstract
Objective
To evaluate the feasibility and safety of total mesopancreas excision (TMpE) in the treatment of pancreatic head cancer.
Methods
The clinical and pathological data of 120 patients with pancreatic head cancer who had undergone TMpE in our center from May 2010 to January 2014 were retrospectively analyzed.
Results
The mean operative time was (275.0±50.2) min and the average intra-operative blood loss was (390.0±160.5) mL. Post-operative complications were reported in 45 patients, while no peri-operative death was noted. The specimen margins were measured in three dimensions, and 86 patients (71.6%) achieved R0 resection.
Conclusions
TMpE is safe and feasible for pancreatic head cancer and is particularly helpful to increase the R0 resection rate.
Keywords: Pancreatic head carcinoma, mesopancreas, total mesopancreas excision (TMpE), R0 resection
Introduction
The post-operative 5-year survival rate is only around 20% in pancreatic cancer patients (1, 2). The local recurrence rate in the retroperitoneal space can reach 80% within the first post-operative year, with the relapse occurs most commonly to the soft tissue behind the pancreatic head (3, 4). With advances in pathological technology, it has been found that actually 20-86% of pancreatic head cancer patients do not actually reach the R0 resection after the surgical treatment (5-7). In recent year, along with the introduction of the concept of "mesopancreas" (8), the R1 resection in many pancreatic head cancer patients has been believed to be caused by the incomplete resection of the mesopancreas (9). Accordingly, the concept of "total mesopancreas excision (TMpE)" has been proposed and then applied in 52 patients, which had suggested that TMpE was helpful to increase the R0 resection rate and improve the prognosis (10-12). Our department was the first center in China to perform TMpE in pancreatic head cancer patients (13, 14). This article summarizes our experiences in conducting TMpE in 120 patients, with an attempt to evaluate the feasibility and safety of this procedure.
Materials and methods
General data
A total of 120 pancreatic head cancer patients (66 men and 54 women, with a median age of 62 years) received TMpE in our center from May 2010 to January 2014. The pre-operative total bilirubin (TB) was 10.3-368.9 μmol/L (x±s: 113.9±52.4 μmol/L). Preoperative biliary drainage was not conducted before surgery. Dual-source computed tomography (CT) and magnetic resonance imaging (MRI) of the abdomen, conventional chest x-ray examination, and examinations of major organ functions were performed before the surgery to rule out the corresponding surgical contraindications. Reconstruction of digestive tract was performed using the Child's operation, among which the residual pancreatic reconstruction was performed using the binding pancreaticoenterostomy, binding pancreaticogastrostomy, and end-to-side anastomosis of residual pancreas and jejunum (15-20). Pathological examination for the three dimensions of the surgical specimens was also performed.
Surgical methods
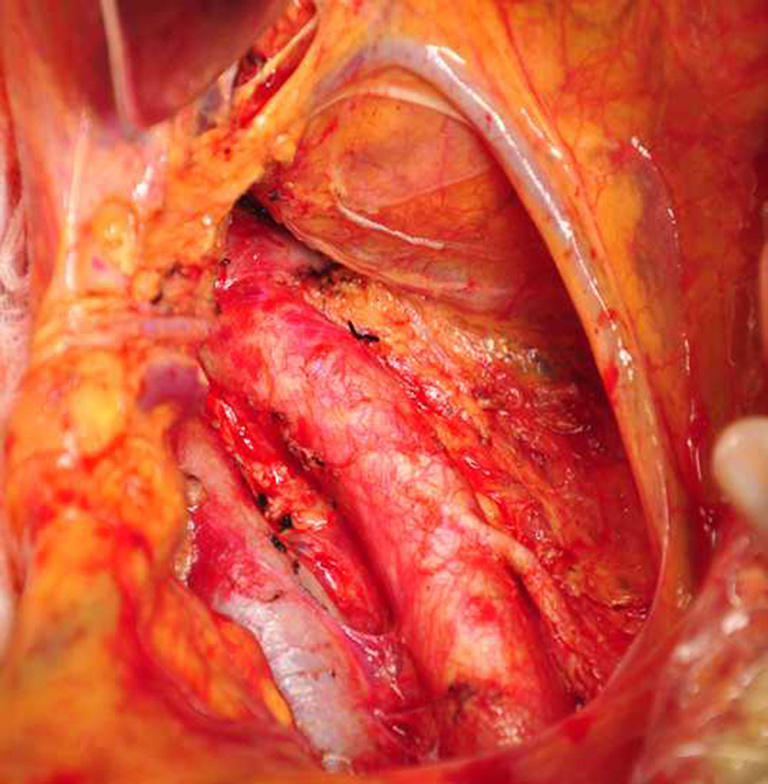
Isolation of the posterior edge of the mesopancreas using the Kocher's maneuver (Figure 1)
1.
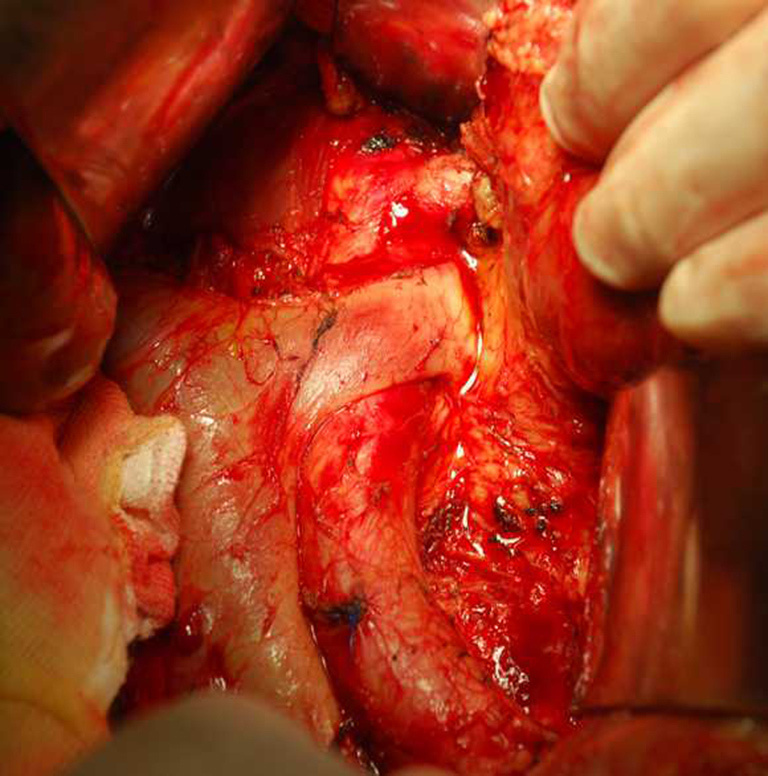
Isolation of the posterior edge of the mesopancreas using the Kocher's maneuver. With the Kocher's maneuver, the distal end of left renal vein and the root of the superior mesenteric artery were exposed leftwards to inspect whether the superior mesenteric artery was involved. Furthermore, expose the inferior vena cava and abdominal aorta towards the tail.abdominal aorta and those from the left side of the abdominal aorta to the inferior mesenteric vein and genital vein) can be safely performed under a clear vision via this approach.
Cut open the right anterior renal fascia along the external edge of the descendant duodenum. After the head of the pancreas and the duodenum were lifted to the left upper side by the assistant, the duodenal capsule was released and protected the hepatic flexure of the colon. Using the Kocher method, expose right renal vein, right genital vein, and inferior vena cava, and then leftwards expose and inspect the spaces behind the pancreatic head and portal vein. After the exposure of the distal end of left renal vein and the abdominal aorta leftwards, expose the root of superior mesenteric artery that is located above the cephalic aorta at the distal end of left renal vein and inspect whether the superior mesenteric artery has been involved. Furthermore, expose the inferior vena cava and abdominal aorta towards the caudal.
Resection of the anterior portion of the mesopancreas
From the hepatic flexure of colon to the middle colic vein, expose and ligate the right gastroepiploic vein, dissect the greater omentum and the anterior lobe of the transverse mesocolon till the lower edge of the pancreas; expose the superior mesenteric vein beneath the pancreatic neck, dissect the adjacent adipose and lymphoid tissues, and then partially expose the space behind pancreatic neck and in front of the portal vein-superior mesenteric vein at the lower edge of the pancreatic neck (Figure 2). Divide the greater omentum from the middle to the right side along the external side of the gastroepiploic arterial arch till the gastric antrum, during which the gastroepiploic arterial arch must be carefully protected. After the removal of the gallbladder, transect the common hepatic duct over the cystic duct, expose the hepatic artery and portal vein, skeletonize the hepatoduodenal ligament, and then expose and ligate the right gastric artery at the proximal end along the proper hepatic artery. Open the hepatogastric ligament along the lower edge of the left hepatic lobe till the distal end of the left gastric vein. Remove the lesser omentum from the distal end of the left gastric vein to the gastric antrum along the external side of the vascular arch of the gastric lesser curvature, during which the vascular arch must be carefully protected. Divide and ligate the gastroduodenal artery, followed by the exposure of the root of common hepatic artery and the abdominal aorta (Figure 3). Divide the gastric antrum using a stapler & cutter. After the portal vein and superior mesenteric vein were exposed at the upper and lower edge of the pancreatic neck, respectively, the space behind the pancreatic neck in front of the portal vein-superior mesenteric vein was further exposed, and then the pancreas was divided. Specimen from the pancreatic stump was sent for routine frozen pathology. Thus, the anterior portion of the mesopancreas was completely divided, and the head of the pancreas and pancreas uncinate process were still connected with the posterior portion of the mesopancreas (Figure 4).
2.
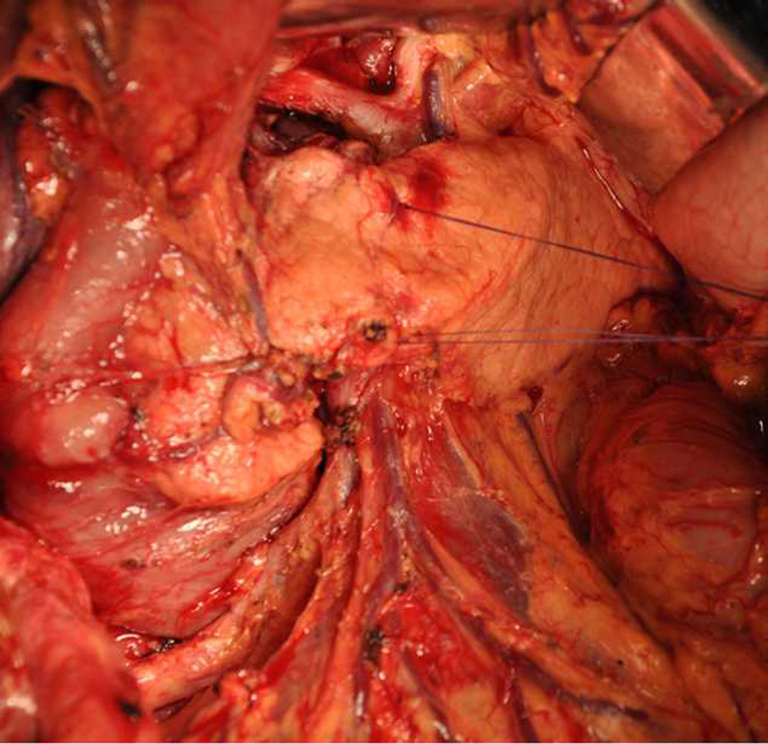
Resection of the anterior portion of the mesopancreas. From the hepatic flexure of colon to the middle colic vein, expose the superior mesenteric vein by peeling off the greater omentum and the anterior lobe of the transverse mesocolon, followed by the dissection of the surrounding adipose/lymphatic tissues. Cut open the hepatogastric ligament along the lower edge of the left hepatic lobe till the distal end of the left gastric vein, during which the vascular arch must be carefully protected.duodenum, and the anterior and posterior sections of the mesopancreas.
3.
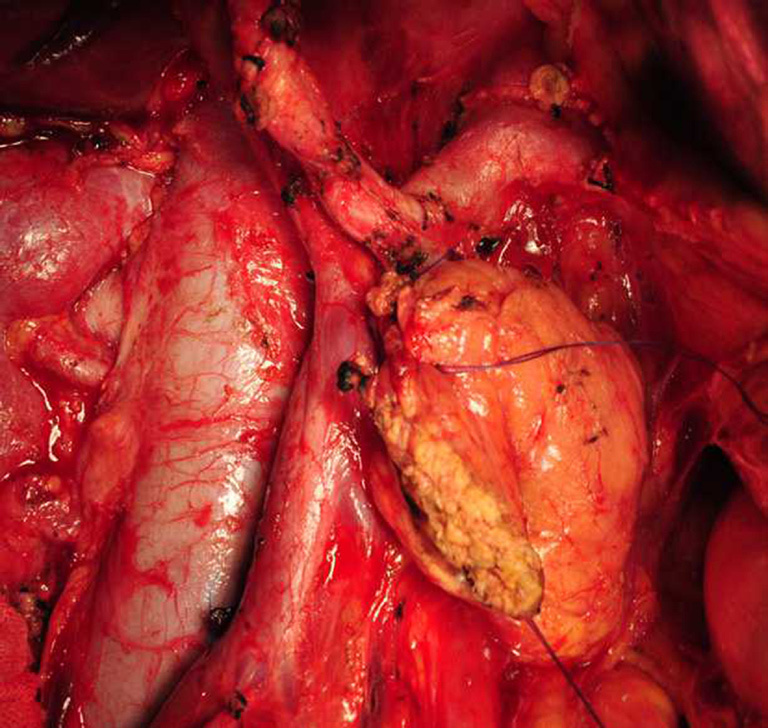
Resection of the anterior portion of the mesopancreas. Divide and ligate the gastroduodenal artery, followed by the exposure of the root of common hepatic artery and the abdominal aorta.
4.
Resection of the anterior portion of the mesopancreas. After the transection of pancreas, specimen was collected from the pancreatic stump frozen pathological examination. Thus, the anterior portion of the mesopancreas was completely divided, and the head of the pancreas and pancreas uncinate process were still connected with the posterior portion of the mesopancreas.
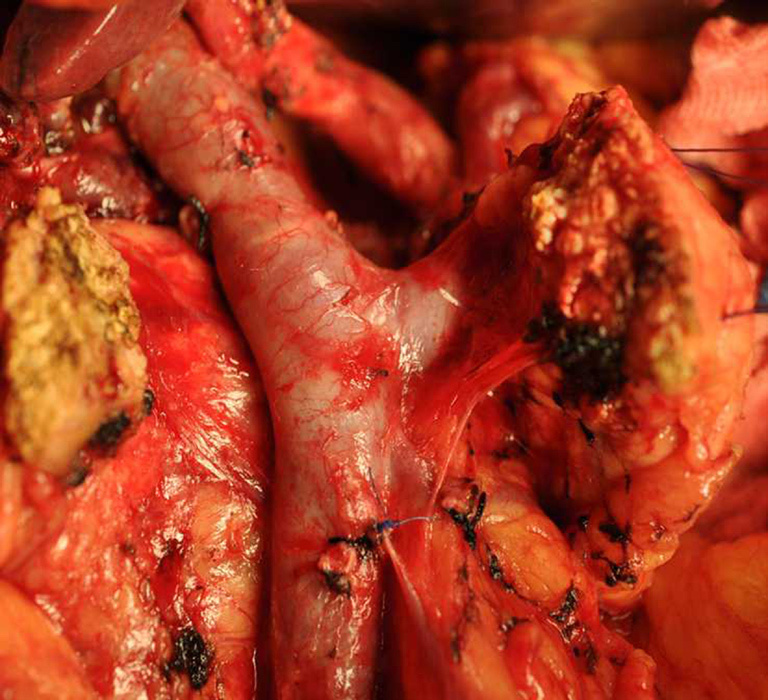
Resection of the posterior portion of the mesopancreas
Lift the transverse colon upwards to expose the inferior mesenteric vein. Open the retroperitoneum along the left edge of the inferior mesenteric vein. Thus, the posterior portion of the mesopancreas became visible (Figure 5). The level of inferior mesenteric artery was defined as the lower border of the resection of the posterior portion of the mesopancreas. After the dissection of the connective tissues around the superior mesenteric artery, the dissection continued upwards along the anterior side of the abdominal aorta till 2 cm above the root of celiac trunk, which was defined as the upper border of resection of the posterior portion of the mesopancreas. Then, the connective tissues around the celiac trunk were dissected. The connective tissue between the inferior vena cava and the abdominal aorta should be carefully dissected. Furthermore, the left genital vein was set as the left posterior border for the resection of mesopancreas and the inferior mesenteric vein as the left anterior border. After the jejunum was transected 15 cm away from the ligament of Treitz, the anterior and posterior sections of the mesopancreas had been completely divided; only the junction between the anterior and posterior sections (the head of the pancreas and the uncinate process of the pancreas) was connected with the superior mesenteric artery and vein. Divide and ligate the vessels in the uncinate process of the pancreas, and then dissociate the uncinate process. Pull away the uncinate process to expose the superior mesenteric artery at the left side of the superior mesenteric vein. Turn over the superior mesenteric artery in the first branch of jejunum to expose the right side of the superior mesenteric vein. Then, the lymphatic and nerve tissues around the superior mesenteric artery were dissected till its root. Separate and ligate the small blood vessels in the uncinate process to complete the en bloc resection of the head of the pancreas, duodenum, and the anterior and posterior sections of the mesopancreas; if necessary, resection and reconstruction of the vessels were also performed (Figure 6). After three-dimensional marking of the cutting edges, the surgical specimens were sent for pathology.
5.
Resection of the posterior portion of the mesopancreas. Cut open the retroperitoneum along the left edge of the inferior mesenteric vein to completely expose the posterior margin of the mesopancreas. The resection of the posterior mesopancreas from the inferior mesenteric artery to the left renal vein (in particular, the resection of tissues between the inferior vena cava and the abdominal aorta and those from the left side of the abdominal aorta to the inferior mesenteric vein and genital vein) can be safely performed under a clear vision via this approach.
6.
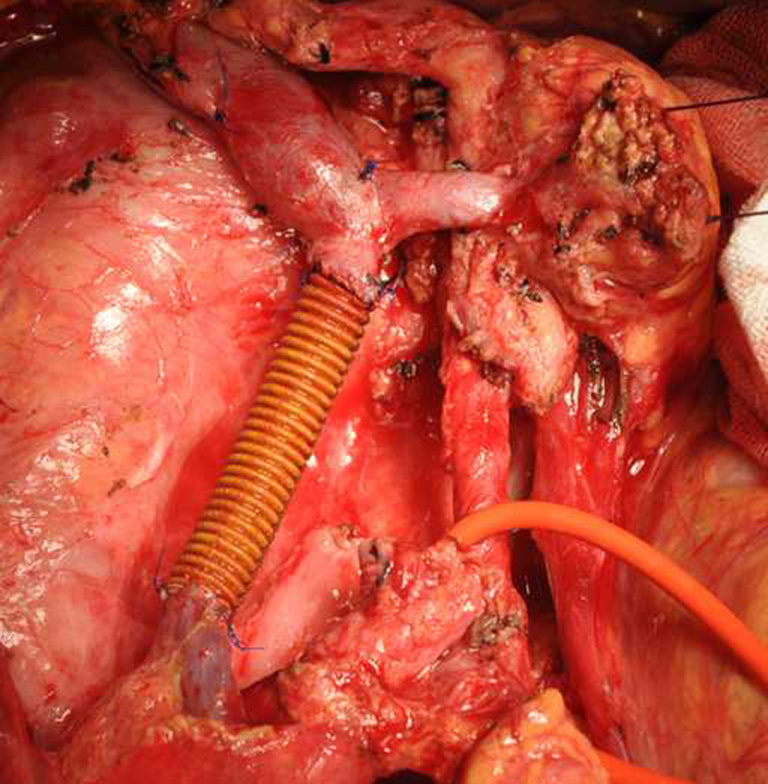
Resection and reconstruction of the vessels. Resection and reconstruction of the superior mesenteric vein was performed to complete the en cloc resection of the head of the pancreas, duodenum, and the anterior and posterior sections of the mesopancreas.
Results
Of these 120 patients who had undergone TMpE, 15 patients also received vascular resection and reconstruction, which included portal vein resection and reconstruction in nine cases and superior mesenteric vein resection and reconstruction in six cases. According to AJCC TNM staging for pancreatic cancer, 10 patients were in stage IB, 16 in stage IIA, 77 in stage IIB, and 17 in stage III. The specimen margins were measured in three dimensions, and 86 patients (71.6%) achieved R0 resection. The mean operative time was (275.0±50.2) min and the average intra-operative blood loss was (390.0±160.5) mL. Also, 45 patients (37.5%) suffered from postoperative complications (21), which were in grade I in 10 cases, grade II in 22 cases, grade III in 7 cases, and grade IV in 5 cases. No patient had a grade V complication.
Discussion
Adham et al. (12) firstly described the application of TMpE for the carcinoma of head of pancreas, which was based on the concept of total mesorectal excision (8). Due to its unique anatomic features, the connective tissues among the superior mesenteric vein, portal vein, and the root of superior mesenteric artery were collectively referred to as the mesopancreas, or known as the "mesopancreas triangle" (12). While this was only a theoretical inference, a rate (80.8%) of R0 resection was achieved in their series, which remarkably improved the 5-year survival rate (12). However, few studies have explored the role of TMpE for pancreatic head carcinoma in the coming years (22, 23). In our center, the relevant clinical study was initiated in 2010, and the findings from 75 cases were quite encouraging (13, 14). Preliminary results from a large number of clinical cases and autopsies in the past years have documented the feasibility of TMpE for the pancreatic head carcinoma.
Anatomically, the mesopancreas still cannot be easily described. In terms of pancreaticoduodenal resection, however, with an attempt to achieve the dissection of both lymphatic tissue and nerve tissue, we divide the mesopancreas at the pancreatic head into the anterior and posterior mesopancreas, which mainly refers to the lymphatic connective tissues that attach to the anterior side of the abdominal aorta and surround the superior mesenteric artery and vein and the celiac trunk. The anterior mesopancreas mainly refers to the anterior lobe of transverse mesocolon at the right side of the middle colic vein, the greater omentum besides the right gastroepiploic artery, the lesser omentum at the right side of left gastric vein, as well as the lymphatic/adipose tissues around the portal vein, hepatic artery, and hepatic artery; also, it includes stomach antrum, duodenum, common bile duct, and other nearby organs. Therefore, the resection of the anterior mesopancreas is mainly targeted at the dissection of lymphatic tissues. The inferior mesenteric artery is set as the lower margin of the posterior mesopancreas. After the dissection of the connective tissues around the superior mesenteric artery, the dissection continued upwards along the anterior side of the abdominal aorta till 2 cm above the root of celiac trunk, which was defined as the upper border of resection of the posterior portion of the mesopancreas. Then, the connective tissues around the celiac trunk were dissected. The connective tissue between the inferior vena cava and the abdominal aorta should be carefully dissected. Furthermore, the left genital vein was set as the left posterior border for the resection of posterior mesopancreas and the inferior mesenteric vein as the left anterior border. Since there are many nerve plexuses in the connective tissues behind the superior mesenteric artery and before the abdominal aorta and inferior vena cava, the resection of the posterior mesopancreas is mainly targeted at the dissection of nerve plexuses. Since the posterior mesopancreas covers the anterior side of the abdominal aorta (with its upper margin 2 cm above the celiac trunk and the lower margin at the level of the inferior mesenteric artery), it is anatomically justifiable to define the connective tissues around the major arteries (the celiac trunk, superior mesenteric artery, and inferior mesenteric artery) arising from the abdominal aorta as the mesopancreas at the head of the pancreas. We are currently carrying out autopsy-based studies on the mesopancreas, and further findings are expected. During the surgical operations, we have found that the posterior edge of the mesopancreas can be thoroughly exposed after cutting opening the retro peritoneum along the left edge of the inferior mesenteric vein. The resection of the posterior mesopancreas from the inferior mesenteric artery to the left renal vein (in particular, the resection of tissues between the inferior vena cava and the abdominal aorta and those from the left side of the abdominal aorta to the inferior mesenteric vein and genital vein) can be safely performed under a clear vision via this approach. The clear vision is particularly helpful to reduce intra-operative blood loss and improve the surgical safety and the quality of resection.
In our current study, we summarized the clinicopathological data of 120 patients with pancreatic head cancer, which demonstrated that TMpE was safe and feasible for this malignancy and could effectively increase the rate of R0 resection in these patients. However, the outcomes still warrant further validation in the subsequent follow-up.
Acknowledgments
Funding: Supported by Shanghai municipal hospital burgeoning and leading edge technology projects No. SHDC12014109.
Footnotes
The authors have no conflicts of interest to declare.
References
- 1.Liu YB, Wu WG. A preliminary investigation on the range of lymph node dissection for pancreatic cancer. Shanghai Yi Xue (in Chinese) 2010;33:986–8. [Liu YB, Wu WG. A preliminary investigation on the range of lymph node dissection for pancreatic cancer. Shanghai Yi Xue (in Chinese) 2010;33:986-8.] [Google Scholar]
- 2.Wagner M, Redaelli C, Lietz M, et al. Curative resection is the single most important factor determining outcome in patients with pancreatic adenocarcinoma. Br J Surg. 2004;91:586–94. doi: 10.1002/(ISSN)1365-2168. [Wagner M, Redaelli C, Lietz M, et al. Curative resection is the single most important factor determining outcome in patients with pancreatic adenocarcinoma. Br J Surg 2004;91:586-94.] [DOI] [PubMed] [Google Scholar]
- 3.Sperti C, Pasquali C, Piccoli A, et al. Recurrence after resection for ductal adenocarcinoma of the pancreas. World J Surg. 1997;21:195–200. doi: 10.1007/s002689900215. [Sperti C, Pasquali C, Piccoli A, et al. Recurrence after resection for ductal adenocarcinoma of the pancreas. World J Surg 1997;21:195-200.] [DOI] [PubMed] [Google Scholar]
- 4.Yermilov I, Bentrem D, Sekeris E, et al. Readmissions following pancreaticoduodenectomy for pancreas cancer: a population-based appraisal. Ann Surg Oncol. 2009;16:554–61. doi: 10.1245/s10434-008-0178-6. [Yermilov I, Bentrem D, Sekeris E, et al. Readmissions following pancreaticoduodenectomy for pancreas cancer: a population-based appraisal. Ann Surg Oncol 2009;16:554-61.] [DOI] [PubMed] [Google Scholar]
- 5.Esposito I, Kleeff J, Bergmann F, et al. Most pancreatic cancer resections are R1 resections. Ann Surg Oncol. 2008;15:1651–60. doi: 10.1245/s10434-008-9839-8. [Esposito I, Kleeff J, Bergmann F, et al. Most pancreatic cancer resections are R1 resections. Ann Surg Oncol 2008;15:1651-60.] [DOI] [PubMed] [Google Scholar]
- 6.Weitz J, Rahbari N, Koch M, et al. The “artery first” approach for resection of pancreatic head cancer. http://cn.bing.com/academic/profile?id=2144937441&encoded=0&v=paper_preview&mkt=zh-cn. J Am Coll Surg. 2010;210:e1–4. doi: 10.1016/j.jamcollsurg.2009.10.019. [Weitz J, Rahbari N, Koch M, et al. The “artery first” approach for resection of pancreatic head cancer. J Am Coll Surg 2010;210:e1-4.] [DOI] [PubMed] [Google Scholar]
- 7.Verbeke CS, Leitch D, Menon KV, et al. Redefining the R1 resection in pancreatic cancer. Br J Surg. 2006;93:1232–7. doi: 10.1002/(ISSN)1365-2168. [Verbeke CS, Leitch D, Menon KV, et al. Redefining the R1 resection in pancreatic cancer. Br J Surg 2006;93:1232-7.] [DOI] [PubMed] [Google Scholar]
- 8.Gockel I, Domeyer M, Wolloscheck T, et al. Resection of the mesopancreas (RMP): a new surgical classifica-tion of a known anatomical space. World J Surg Oncol. 2007;5:44. doi: 10.1186/1477-7819-5-44. [Gockel I, Domeyer M, Wolloscheck T, et al. Resection of the mesopancreas (RMP): a new surgical classifica-tion of a known anatomical space. World J Surg Oncol 2007;5:44.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gaedcke J, Gunawan B, Grade M, et al. The meso-pancreas is the primary site for R1 resection in pancreatic head cancer: relevance for clinical trials. Langenbecks Arch Surg. 2010;395:451–8. doi: 10.1007/s00423-009-0494-8. [Gaedcke J, Gunawan B, Grade M, et al. The meso-pancreas is the primary site for R1 resection in pancreatic head cancer: relevance for clinical trials. Langenbecks Arch Surg 2010;395:451-8.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Agrawal MK, Thakur DS, Somashekar U, et al. Meso-pancreas: myth or reality. http://cn.bing.com/academic/profile?id=2116325640&encoded=0&v=paper_preview&mkt=zh-cn. JOP. 2010;11:230–3. [Agrawal MK, Thakur DS, Somashekar U, et al. Meso-pancreas: myth or reality? JOP 2010;11:230-3.] [PubMed] [Google Scholar]
- 11.Popescu I, Dumitrascu T. Total meso-pancreas excision: key point of resection in pancreatic head adenocarcinoma. Hepatogastroenterology. 2011;58:202–7. [Popescu I, Dumitrascu T. Total meso-pancreas excision: key point of resection in pancreatic head adenocarcinoma. Hepatogastroenterology 2011;58:202-7.] [PubMed] [Google Scholar]
- 12.Adham M, Singhirunnusorn J. Surgical technique and results of total mesopancreas excision (TMpE) in pancreatic tumors. Eur J Surg Oncol. 2012;38:340–5. doi: 10.1016/j.ejso.2011.12.015. [Adham M, Singhirunnusorn J. Surgical technique and results of total mesopancreas excision (TMpE) in pancreatic tumors. Eur J Surg Oncol 2012;38:340-5.] [DOI] [PubMed] [Google Scholar]
- 13.Liu YB, Quan ZW, Peng SY. The idea and controversy of total mesopancreas excision (TMpE) in pancreatic head tumors. Zhongguo Shi Yong Wai Ke Za Zhi (in Chinese) 2013;33:856–8. [Liu YB, Quan ZW, Peng SY. The idea and controversy of total mesopancreas excision (TMpE) in pancreatic head tumors. Zhongguo Shi Yong Wai Ke Za Zhi (in Chinese) 2013;33:856-8.] [Google Scholar]
- 14.Wu WG, Wu XS, Li ML, et al. Total mesopancreas excision (TMpE) for pancreatic head tumors with 75 cases report. http://en.cnki.com.cn/article_en/cjfdtotal-zgwk201310022.htm. Zhongguo Shi Yong Wai Ke Za Zhi (in Chinese) 2013;33:859–62. [Wu WG, Wu XS, Li ML, et al. Total mesopancreas excision (TMpE) for pancreatic head tumors with 75 cases report. Zhongguo Shi Yong Wai Ke Za Zhi (in Chinese) 2013;33:859-62.] [Google Scholar]
- 15.Peng SY, Wang JW, Lau WY, et al. Conventional versus binding pancreaticojejunostomy after pancreaticoduodenectomy: a prospective randomized trial. Ann Surg. 2007;245:692–8. doi: 10.1097/01.sla.0000255588.50964.5d. [Peng SY, Wang JW, Lau WY, et al. Conventional versus binding pancreaticojejunostomy after pancreaticoduodenectomy: a prospective randomized trial. Ann Surg 2007;245:692-8.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu YB, Zhu JH, Wang JW, et al. Comparison of wound healing after pancreaticojejunostomy with three anastomotic methods in piglets. http://cn.bing.com/academic/profile?id=2416103774&encoded=0&v=paper_preview&mkt=zh-cn. Zhonghua Wai Ke Za Zhi (in Chinese) 2006;44:339–43. [Liu YB, Zhu JH, Wang JW, et al. Comparison of wound healing after pancreaticojejunostomy with three anastomotic methods in piglets. Zhonghua Wai Ke Za Zhi (in Chinese) 2006;44:339-43.] [PubMed] [Google Scholar]
- 17.Peng SY, Wang JW, Hong DF, et al. Binding pancreaticoenteric anastomosis: from binding pancrea-ticojejunostomy to binding pancreaticogastrostomy. Updates Surg. 2011;63:69–74. doi: 10.1007/s13304-011-0067-6. [Peng SY, Wang JW, Hong DF, et al. Binding pancreaticoenteric anastomosis: from binding pancrea-ticojejunostomy to binding pancreaticogastrostomy. Updates Surg 2011;63:69-74.] [DOI] [PubMed] [Google Scholar]
- 18.Liu YB, Wang JW, Fang HQ, et al. Effect of binding pancreaticojejunotomy in prevention of post-operational anastomotic leakage: a clinical study of 200 cases. http://cn.bing.com/academic/profile?id=2351257687&encoded=0&v=paper_preview&mkt=zh-cn. Zhonghua Yi Xue Za Zhi (in Chinese) 2004;83:997–9. [Liu YB, Wang JW, Fang HQ et al. Effect of binding pancreaticojejunotomy in prevention of post-operational anastomotic leakage: a clinical study of 200 cases. Zhonghua Yi Xue Za Zhi (in Chinese) 2004;83:997-9.] [PubMed] [Google Scholar]
- 19.Peng SY, Hong DF, Liu YB, et al. Binding pancrea-ticogastrostomy. Zhonghua Wai Ke Za Zhi (in Chinese) 2009;47:139–42. [Peng SY, Hong DF, Liu YB, et al. Binding pancrea-ticogastrostomy. Zhonghua Wai Ke Za Zhi (in Chinese) 2009;47:139-42.] [PubMed] [Google Scholar]
- 20.Peng SY, Li JT, Cao LP, et al. Binding pancreatic duct to mucosa anastomosis. http://cn.bing.com/academic/profile?id=2399086626&encoded=0&v=paper_preview&mkt=zh-cn. Zhonghua Wai Ke Za Zhi (in Chinese) 2011;49:834–8. [Peng SY, Li JT, Cao LP, et al. Binding pancreatic duct to mucosa anastomosis. Zhonghua Wai Ke Za Zhi (in Chinese) 2011;49:834-8.] [PubMed] [Google Scholar]
- 21.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13. doi: 10.1097/01.sla.0000133083.54934.ae. [Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205-13.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dumitrascu T, Popescu I. Total mesopancreas excision in pancreatic head adenocarcinoma: The same impact as total mesorectal excision in rectal carcinoma? Comment on article “surgical technique and results of total mesopancreas excision in pancreatic tumours” by Adham M and Singhirunnusorn J, Eur J Surg Oncol, 2012. Eur J Surg Oncol 2012;38:725; author reply 726.http://cn.bing.com/academic/profile?id=1975254951&encoded=0&v=paper_preview&mkt=zh-cn
- 23.Hong DF, Peng SY, Shen GL, et al. Total meso-pancreas excision on radical resection of pancreatic head carcinoma. Zhonghua Pu Tong Wai Ke (in Chinese) 2014;29:344–7. [Hong DF, Peng SY, Shen GL, et al. Total meso-pancreas excision on radical resection of pancreatic head carcinoma. Zhonghua Pu Tong Wai Ke (in Chinese) 2014;29:344-7.] [Google Scholar]


