Abstract
AIM
To describe the performance of 450 nm diode laser in oral surgery procedures.
METHODS
The case described consisted of the removal of a lower lip fibroma through a blue diode laser (λ = 450 nm).
RESULTS
The efficacy of this device, even at very low power (1W, CW), allows us to obtain very high intra and postoperative comfort for the patient, even with just topical anaesthesia and without needing suture. The healing process was completed in one week and, during the follow-up, the patient did not report any problems, pain or discomfort even without the consumption of any kind of drugs, such as painkillers and antibiotics. The histological examination performed by the pathologist showed a large area of fibrous connective tissue with some portions of epithelium-connective detachments and a regular incision with very scanty areas of carbonization.
CONCLUSION
The 450 nm diode laser proved of being very efficient in the oral soft tissue surgical procedures, with no side effects for the patients.
Keywords: Blue laser, Advantages, Oral surgery, Patient satisfaction
Core tip: In this work we described a single case consisting of the removal of a lower lip fibroma by means of a blue diode laser (λ = 450 nm), showing its efficacy even at very low power (1W, CW) and allowing us to obtain very high intra and postoperative comfort for the patient, even with just topical anaesthesia and without needing suture. The observed healing process after one week and the complete absence of pain during the follow-up without the consumption of any kind of drugs, such as painkillers and antibiotics, together with the perfect histological readability are very great advantages in favour of this surgical approach.
INTRODUCTION
In 1964 Goldman introduced laser technology in dentistry field[1] and, even if several authors in those years described several laser applications in dentistry[2-5], only Frame was the first who showed the absence of biological damage in a laser-assisted surgical intervention with CO2 laser[6].
Many papers described the advantages for laser-assisted oral surgery as the reduction of the surgical time, the absence of bleeding and consequently the good vision of the surgical site, the possibility to avoid infiltrative anaesthesia and suture with a greater compliance for the patient and the better and faster healing process[7-12].
Together with wavelengths specific for soft tissues, thanks to Hibst and Keller, since 1990, we can use also the Erbium laser (2940 nm) for decay removal in restorative dentistry[13,14].
Today, in addition to lasers working in infrared spectrum, for oral surgery we can use wavelengths working in the visible spectrum as Argon laser (435 nm) useful in oral surgery but also in restorative dental field, and KTP laser (532 nm) well working in oral surgery thanks to its characteristics at low parameters and with a good bleeding control[14-16].
Supercontinuum source is a device allowing to evaluate laser-tissue interactions, mainly transmission; an “ex vivo” recent study showed that the lowest transmission is in the blue and green portion of visible spectrum and in the infrared portion ranging from 1300 to 1400 nm[17]: These results could justify the utilisation of dental blue laser, considering also the demonstration, by Enwemeka et al[18] , of the of blue light capacity to neutralise some bacterial species also being effective on periodontal biofilm, as shown in several in vitro studies[19-21] as well as in Photodynamic Therapy field on Streptococcus Mutans cultures, as described by Merigo et al[22].
Blue light has been evaluated also for its biomodulatory properties, with laser or LED devices, showing positive effects[23-26].
Even if blue laser was previously proposed in dentistry field for composite resin polymerization, while argon laser showed its efficacy, diode lasers apparently are not proposed as useful for this use[27-31].
Lately, the combined treatment with blue laser and titanium oxide has been indicated for teeth whitening, but there are still no works describing the utilisation of this wavelength in oral surgery[32].
The purpose of this paper was to demonstrate the advantages of this wavelength in oral soft tissue surgery.
MATERIALS AND METHODS
The patient ML, a thirty-eight years old female, came to our clinic for the examination of a lesion in the margin of the lower lip. She reported that it had been present for a year and, in the last few months, she had noticed an enlargement of its size (Figures 1 and 2). She required the surgical removal for aesthetical reasons.
Figure 1.

Clinical appearence of the lower lip lesion with aesthetical impairment.
Figure 2.

Lower lip fibroma probably caused by a lip biting habit.
She had a medical history without significant diseases and the oral clinical examination did not reveal any suspicious aspect.
The clinical diagnosis was positive for fibroma, probably related to a lip biting habit. Based on the age of the patient, the anatomical area and the size of the lesion, it was decided to perform a laser-assisted surgery session for the lesion removing, so avoiding the complications related to the conventional surgery, such as the formation of post-operative scars and bleeding[33]. Regarding the choice of the wavelength, in order to limit the thermal elevation and, at the same time, to obtain a good sample for histological observation[34] and to offer the patient the most comfort during the healing process, it was decided to use the blue diode laser (Ermes Blue Diode, Gardalaser, Italy, λ = 450 nm) with this protocol: Power 1W in CW (Continuous Wave) with an optical fiber of 320 μm of diameter in contact mode at a speed of around 5 mm/s (Power density 1244 W/cm2, Total fluence: 95790 J/cm2).
The patient was informed about all the aspects of the intervention, and she signed the consensus for the surgical removal of the fibroma. The use of anaesthetic injection and the sutures apposition were avoided; only a topical anaesthetic was applied (EMLA, Astratech, Sweden) and the duration of the intervention was 77 s.
The patient was instructed on the need to record the intensity of the pain she felt through a visual analogue scale (VAS) and a numerical rating scale (NRS) every day after surgery beginning with the first day after surgery until the re-evaluation we performed seven days after surgery.
Clinical observations at 1 and 3 mo after surgery did not show any sign of recurrence.
RESULTS
During the whole duration of the intervention patient described the absence of pain or discomfort.
The site of the lesion, after the removal, did not show any bleeding and did not require any suture (Figure 3).
Figure 3.

Image of the surgical site immediately after surgery.
Both the site and the sample removed did not evidence any sign of carbonization (Figure 4) and the healing process was completed in seven days (Figure 5).
Figure 4.

Sample for histological analysis.
Figure 5.
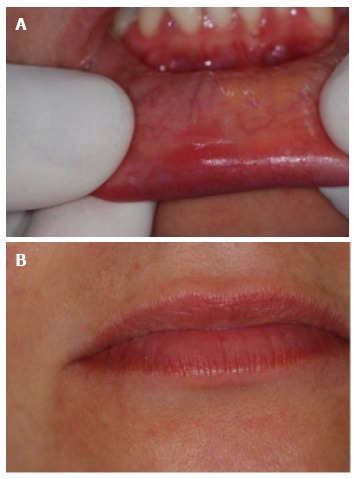
The healing process was completed in seven days. A: Surgical site seven days after surgery; B: Appearence of the lip seven days after surgery with a complete recovering of aesthetic aspect.
During the follow-up the patient did not take any drugs, such as painkillers and antibiotics, did not reveal any sign of oedema and/or infection and reported that she did not feel any form of pain (VAS and NRS were 0 in every record), discomfort or other problems.
The histological evaluation of the sample, performed by the pathologist, showed a large area of fibrous connective tissue with some portions of epithelium-connective detachments and a regular incision with very scanty areas of carbonization (Figure 6).
Figure 6.
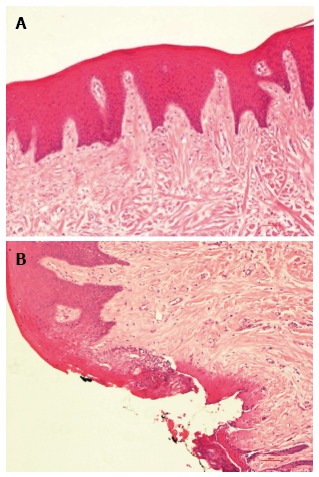
A large area of fibrous connective tissue with some portions of epithelium-connective detachments and a regular incision with very scanty areas of carbonization. A: Fibrous connective tissue without signs of inflammation; B: Regular incision with discrete signs of coagulations.
DISCUSSION
This report confirms the advantages of the utilization of 450 nm laser in oral surgery, showing undeniable benefits for its use at very low power. During the operative session it allows for the reduction of the time of the intervention, the avoidance of the anaesthetic injection and the control of the tissue bleeding. From the patient’s comfort point of view, it allows us to minimize the pain and avoid the use of suture. During the follow-up, the use of drugs is not requested, and pain, discomfort, oedema and infection are not present. The healing process is very fast and was completed in a week without side effects.
From the histological point of view, the sample removed shows significantly fewer zones of carbonization, so as avoiding the risk of the impossibility of not being able to make a correct diagnosis of the lesion. This technique may be considered a good approach in oral soft tissues surgery.
COMMENTS
Background
Many papers described the advantages for laser-assisted oral surgery as the reduction of the surgical time, the absence of bleeding and consequently the good vision of the surgical site, the possibility to avoid infiltrative anaesthesia and suture with a greater compliance for the patient and the better and faster healing process. Blue light has been evaluated for its biomodulatory properties, with laser or LED devices, and for its usefulness in dental bleaching procedures, showing positive effects.
Research frontiers
Actually there are still no works describing the utilisation of this wavelength in oral surgery. The purpose of this paper was to demonstrate the advantages of this wavelength in oral soft tissue surgery.
Innovations and breakthroughs
This report confirms the advantages of the utilization of 450 nm laser in oral surgery, showing undeniable benefits for its use at very low power. During the operative session it allows for the reduction of the time of the intervention, the avoidance of the anaesthetic injection and the control of the tissue bleeding. From the patient’s comfort point of view, it allows us to minimize the pain and avoid the use of suture. During the follow-up, the use of drugs is not requested, and pain, discomfort, oedema and infection are not present. The healing process is very fast and was completed in a week without side effects. From the histological point of view, the sample removed shows significantly fewer zones of carbonization, so as avoiding the risk of the impossibility of not being able to make a correct diagnosis of the lesion.
Applications
This technique may be considered a good approach in oral soft tissues surgery.
Terminology
CW or continuous wave is a working mode of laser devices. VAS or visual analogue scale and NRS or numerical rating scale are two methods to evaluate the discomfort or pain felt by the patient in the intra and postoperative period.
Peer-review
Interesting case report of the use of blue diode laser for the removal of oral and intraoral soft tissue benign tumors. The case report is well written with a comprehensive description of the application of the blue diode laser.
Footnotes
Institutional review board statement: N/A.
Informed consent statement: The described patient gave her informed consent prior to study inclusion.
Conflict-of-interest statement: Authors disclosed no potential financial conflict of interest with this study.
Manuscript source: Invited manuscript
Specialty type: Medicine
Country of origin: France
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
Peer-review started: February 16, 2016
First decision: March 25, 2016
Article in press: July 16, 2016
P- Reviewer: Ebid AA, Rapidis AD S- Editor: Qiu S L- Editor: A E- Editor: Lu YJ
References
- 1.Goldman L, Gray JA, Goldman J, Goldman B, Meyer R. Effect of laser beam impacts on teeth. J Am Dent Assoc. 1965;70:601–606. doi: 10.14219/jada.archive.1965.0260. [DOI] [PubMed] [Google Scholar]
- 2.Kinersly T, Jarabak JP, Phatak NM, Dement J. Laser effects on tissue and materials related to dentistry. J Am Dent Assoc. 1965;70:593–600. doi: 10.14219/jada.archive.1965.0268. [DOI] [PubMed] [Google Scholar]
- 3.Morrant GA. Lasers: an appraisal of their possible use in dentistry. Dent Pract Dent Rec. 1965;16:5–9. [PubMed] [Google Scholar]
- 4.Stern RH, Sognnaes RF. Laser effect on dental hard tissues. a preliminary report. J South Calif Dent Assoc. 1965;33:17–19. [PubMed] [Google Scholar]
- 5.Taylor R, Shklar G, Roeber F. The effects of laser radiation on teeth, dental pulp, and oral mucosa of experimental animals. Oral Surg Oral Med Oral Pathol. 1965;19:786–795. doi: 10.1016/0030-4220(65)90351-8. [DOI] [PubMed] [Google Scholar]
- 6.Basu MK, Frame JW, Rhys Evans PH. Wound healing following partial glossectomy using the CO2 laser, diathermy and scalpel: a histological study in rats. J Laryngol Otol. 1988;102:322–327. doi: 10.1017/s0022215100104852. [DOI] [PubMed] [Google Scholar]
- 7.Vescovi P, Del Vecchio A, Manfredi M, Fornaini C, Tenore G, Romeo U. The use of laser for treatment of oral mucosal diseases. Dental Cadmos. 2009;77:10. [Google Scholar]
- 8.Tuncer I, Ozçakir-Tomruk C, Sencift K, Cöloğlu S. Comparison of conventional surgery and CO2 laser on intraoral soft tissue pathologies and evaluation of the collateral thermal damage. Photomed Laser Surg. 2010;28:75–79. doi: 10.1089/pho.2008.2353. [DOI] [PubMed] [Google Scholar]
- 9.Fornaini C, Rocca JP, Bertrand MF, Merigo E, Nammour S, Vescovi P. Nd: YAG and diode laser in the surgical management of soft tissues related to orthodontic treatment. Photomed Laser Surg. 2007;25:381–392. doi: 10.1089/pho.2006.2068. [DOI] [PubMed] [Google Scholar]
- 10.Rocca JP. Les lasers en odontologie. France: Walters Kluwer; 2008. [Google Scholar]
- 11.Fornaini C. Case report: Use of Er: YAG and Nd: YAG lasers during orthodontic treatment. Journal of the Laser and Health Academy. 2014;1:47–54. [Google Scholar]
- 12.Fornaini C, Rocca JP. Oral Laserology. Italy: Monduzzi Editore, Bologna; 2015. [Google Scholar]
- 13.Hibst R, Keller U. Experimental studies of the application of the Er: YAG laser on dental hard substances: I. Measurement of the ablation rate. Lasers Surg Med. 1989;9:338–344. doi: 10.1002/lsm.1900090405. [DOI] [PubMed] [Google Scholar]
- 14.Majaron B, Plestenjak P, Lukac M. Thermo-mechanical laser ablation of soft tissue: modeling the micro-explosions. Appl Phys B. 1999;69:71–80. [Google Scholar]
- 15.Kelsey WP, Blankenau RJ, Powell GL. Application of the argon laser to dentistry. Lasers Surg Med. 1991;11:495–498. doi: 10.1002/lsm.1900110602. [DOI] [PubMed] [Google Scholar]
- 16.Fornaini C, Rocca JP, Merigo E, Meleti M, Manfredi M, Nammour S, Vescovi P. Low energy KTP laser in oral soft tissue surgery: A 52 patients clinical study. Med Oral Patol Oral Cir Bucal. 2012;17:e287–e291. doi: 10.4317/medoral.17428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fornaini C, Sozzi M, Merigo E, Poli F, Selleri S, Pasotti P, Cucinotta A: Different wavelengths absorption in different tissue kinds: ex vivo study with a supercontinuum broadband source. Las Surg Med. 2015;47:380–381. [Google Scholar]
- 18.Enwemeka CS. Antimicrobial blue light: an emerging alternative to antibiotics. Photomed Laser Surg. 2013;31:509–511. doi: 10.1089/pho.2013.9871. [DOI] [PubMed] [Google Scholar]
- 19.Bumah VV, Masson-Meyers DS, Cashin SE, Enwemeka CS. Wavelength and bacterial density influence the bactericidal effect of blue light on methicillin-resistant Staphylococcus aureus (MRSA) Photomed Laser Surg. 2013;31:547–553. doi: 10.1089/pho.2012.3461. [DOI] [PubMed] [Google Scholar]
- 20.de Sousa NT, Santos MF, Gomes RC, Brandino HE, Martinez R, de Jesus Guirro RR. Blue Laser Inhibits Bacterial Growth of Staphylococcus aureus, Escherichia coli, and Pseudomonas aeruginosa. Photomed Laser Surg. 2015;33:278–282. doi: 10.1089/pho.2014.3854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fontana CR, Song X, Polymeri A, Goodson JM, Wang X, Soukos NS. The effect of blue light on periodontal biofilm growth in vitro. Lasers Med Sci. 2015;30:2077–2086. doi: 10.1007/s10103-015-1724-7. [DOI] [PubMed] [Google Scholar]
- 22.Merigo E, Sozzi M, Ciociola T, Conti S, Fornaini C, Selleri S, Cucinotta A. Photodynamic therapy: a synergy between light and colors. Proceedings of the SPIE, Volume 9306, id. 93060A 8 pp. United States: Spie Bios; 2015. [Google Scholar]
- 23.Smith KC. Laser (and LED) therapy is phototherapy. Photomed Laser Surg. 2005;23:78–80. doi: 10.1089/pho.2005.23.78. [DOI] [PubMed] [Google Scholar]
- 24.Adamskaya N, Dungel P, Mittermayr R, Hartinger J, Feichtinger G, Wassermann K, Redl H, van Griensven M. Light therapy by blue LED improves wound healing in an excision model in rats. Injury. 2011;42:917–921. doi: 10.1016/j.injury.2010.03.023. [DOI] [PubMed] [Google Scholar]
- 25.Kushibiki T, Tajiri T, Ninomiya Y, Awazu K. Chondrogenic mRNA expression in prechondrogenic cells after blue laser irradiation. J Photochem Photobiol B. 2010;98:211–215. doi: 10.1016/j.jphotobiol.2010.01.008. [DOI] [PubMed] [Google Scholar]
- 26.Omi T, Bjerring P, Sato S, Kawana S, Hankins RW, Honda M. 420 nm intense continuous light therapy for acne. J Cosmet Laser Ther. 2004;6:156–162. doi: 10.1080/14764170410023785. [DOI] [PubMed] [Google Scholar]
- 27.Meniga A, Tarle Z, Ristic M, Sutalo J, Pichler G. Pulsed blue laser curing of hybrid composite resins. Biomaterials. 1997;18:1349–1354. doi: 10.1016/s0142-9612(97)00047-1. [DOI] [PubMed] [Google Scholar]
- 28.Fleming MG, Maillet WA. Photopolymerization of composite resin using the argon laser. J Can Dent Assoc. 1999;65:447–450. [PubMed] [Google Scholar]
- 29.Mirsasaani SS, Atai MM, Hasani-Sadrabadi MM. Photopolymerization of a dental nanocomposite as restorative material using the argon laser. Lasers Med Sci. 2011;26:553–561. doi: 10.1007/s10103-009-0699-7. [DOI] [PubMed] [Google Scholar]
- 30.Fornaini C, Lagori G, Merigo E, Rocca JP, Chiusano M, Cucinotta A. 405 nm diode laser, halogen lamp and LED device comparison in dental composites cure: an “in vitro” experimental trial. Laser Ther. 2015;24:265–274. doi: 10.5978/islsm.15-OR-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ro JH, Son SA, Park JK, Jeon GR, Ko CC, Kwon YH. Effect of two lasers on the polymerization of composite resins: single vs combination. Lasers Med Sci. 2015;30:1497–1503. doi: 10.1007/s10103-015-1753-2. [DOI] [PubMed] [Google Scholar]
- 32.Tano E, Otsuki M, Kato J, Sadr A, Ikeda M, Tagami J. Effects of 405 nm diode laser on titanium oxide bleaching activation. Photomed Laser Surg. 2012;30:648–654. doi: 10.1089/pho.2012.3273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yagüe-García J, España-Tost AJ, Berini-Aytés L, Gay-Escoda C. Treatment of oral mucocele-scalpel versus CO2 laser. Med Oral Patol Oral Cir Bucal. 2009;14:e469–e474. [PubMed] [Google Scholar]
- 34.Vescovi P, Merigo E, Fornaini C, Rocca JP, Nammour S. Thermal increase in the oral mucosa and in the jawbone during Nd: YAG laser applications. Ex vivo study. Med Oral Patol Oral Cir Bucal. 2012;17:e697–e704. doi: 10.4317/medoral.17726. [DOI] [PMC free article] [PubMed] [Google Scholar]


