Abstract
Background
Trauma patients who present to the hospital in extremis are attempted to be salvaged with emergency department thoracotomy (EDT). EDT allows for relief of cardiac tamponade, internal cardiac massage, and proximal hemorrhage control. Minimally invasive techniques, such as endovascular hemorrhage control (EHC) are available, but their non-inferiority to EDT remains unproven. Before adopting EHC, it is important to evaluate the current outcomes of EDT. We hypothesize EDT survival has improved during the last 4 decades, and outcomes stratified by pre-hospital cardio pulmonary resuscitation(CPR), and injury patterns will provide benchmarks for success-to-rescue and survival outcomes for patients in extremis.
Study Design
Consecutive trauma patients undergoing EDT from 1975–2014 were prospectively observed as part of quality improvement. Predicted probabilities of survival were adjusted for prehospital CPR, mechanism of injury, injury pattern, patient demographics, and time period of EDT using logistic regression. Success to rescue (STR) was defined as return of spontaneous circulation with blood pressure permissive for transfer to the operating room.
Results
1708 EDTs were included, with an overall 419 (24%) success to rescue and 106 survivors (6%). 1394 (79%) of these patients had pre-hospital CPR, 900 (54%) had penetrating wounds. The most common injury patterns were chest (29%), multi system with head (27%) and multisystem without head (21%). Penetrating injury was associated with higher survival than blunt trauma (9% vs 3% p<0.001). STR increased from 22% in 1975–1979 to 35% over the final 5 years (P<0.001); while survival increased from 5% to 14% (p<0.001).
Conclusions
EDT outcomes have improved over the past 40 years. In the last 5 years, STR was 35% and overall survival was 14%. This prospective observational data provides benchmarks to define the role of EHC as an alternative approach for patients arriving in extremis.
Introduction
Emergency department thoracotomy (EDT) has been employed for half a century to salvage trauma patients arriving in circulatory arrest. Early pioneers of this procedure from Ben Taub appreciated the therapeutic role of a thoracotomy for patient’s who develop circulatory arrest from penetrating chest trauma irrespective of location in the hospital(1). This concept was expanded to blunt trauma patients with reportedly high salvage rates in the late 1970’s(2). However, widespread adoption of this procedure in all trauma patients presenting to the emergency department in circulatory arrest was regarded as an “indiscriminate fire drill”; it was proposed that there should be specific indications(3). In 2000, a literature review of 4,000 trauma patient undergoing EDT reported a survival rate of 7.4% (4). A decade later, however, Passos et al (5) reported a dismal survival rate of 2.4% in their 17-year experience, and had concluded that this procedure was risky, expensive, and offered no survival benefit. Other investigators previously expressed concerns that the EDT risk and cost did not outweigh its potential benefits(6, 7). This negative opinion of EDT is reflective of the current status of this procedure at a national level. In an evaluation of five major level I trauma centers between 2006–2010, EDT was performed in only 13% of patients when indicated(8). Our analysis of the collective experience in the US indicates EDT survival rates vary from 35% for cardiac wounds, 14% for penetrating wounds, to 2% for blunt trauma(9).
There is a clear need for improving early hemorrhage control in trauma as this represents 40% of preventable deaths(10), and the median time to death in hypotensive patients is 2 hours from injury(11). The reported under utilization of EDT at level 1 trauma centers is concerning, as prehospital care, resuscitation, and operative interventions have improved. Hospitals that specialize in high-risk elective surgery such as cardiothoracic(12) and pancreatic(13) surgery have better outcomes when contrasted to low volume centers. An important component attributed to improved outcomes in these patients at high volume centers is that low volume centers have a higher rate of “failure to rescue” patients from postoperative complications(14). Trauma surgery has the reverse sequence; the patient must be rescued from circulatory arrest with an EDT before they can proceed to the operating room. This can be considered “success to rescue”. It has been argued that trauma level designation, based on hospital resources and not volume, determines outcomes in trauma surgery(15, 16). However, these studies do not account for success to rescue from circulatory arrest because most of these centers consider a trauma patient in circulatory arrest dead on arrival (DOA).
The clinical implementation of minimally invasive hemorrhage control through resuscitative endovascular balloon occlusion of the aorta (REBOA)(17), has introduced an alternative strategy to augment resuscitation in patients with circulatory arrest following trauma. REBOA, in theory, could improve resuscitation efforts in trauma centers that fear the risks of EDT or lack experience in the technique. However, before global adoption of this technique, it is essential to benchmark the outcomes of EDT at high volume level I trauma centers’ to identify the contemporary expected success to rescue patterns of trauma patients in circulatory arrest. We hypothesize that anatomic injury location and prehospital circulatory status are associated with markedly different success to rescue and survival rates in trauma patients undergoing EDT, and that overall survival rates have improved over time.
Methods
Patient Population
This prospective observational study includes continuously collected variables on all trauma patients presenting to our urban adult level I trauma center who underwent EDT from January 1975 to December 2014. Data acquisition was under the approval of the Colorado Multiple Institution Review Board. The purpose of this data collection was for quality improvement in refining the indication for this procedure to improve outcomes. The senior author (EEM) reviewed in real-time all patient prehospital characteristics and patient outcomes.
Patient Characteristics and Outcomes
Recorded patient demographics included age and sex. Prehospital variables included injury mechanism and anatomic location, in addition to detection of prehospital cardiac activity, and prehospital cardiopulmonary resuscitation (CPR). For this study, success to rescue was defined as return of spontaneous circulation (ROSC) and transfer of the patient to the operating room; by institutional protocol a systolic blood pressure greater than 70 mmHg was necessary. Outcomes reviewed included success to rescue and survival to hospital discharge. Neurologic outcome was scored using the Glasgow Outcome Score (GOS)(18) and was determined based on the most recent outpatient follow-up visit with rehabilitation if the patient left the hospital with neurologic impairment.
Statistical Analysis
SAS software version 9.4 (Cary, North Carolina) was used for statistical analysis. Continuous variables were described as medians with 25th to 75th percentile range (IQR) if the distribution was skewed or mean with standard deviation when data were normally distributed. Univariate analysis was performed using Kruskal-Wallis, Wilcoxon or Spearman correlation tests for continuous variables, and Chi-square or Fisher Exacts test for categorical variables. The Cochran-Armitage test was used to assess temporal trends. Multivariate analysis to determine predicted probability of survival used logistic regression to adjust for clinically relevant variables (prehospital CPR, blunt versus penetrating mechanism, age, sex, and five-year period during when injury occurred). Model performance was evaluated using the area under the receiver operating characteristics curve (AUROC) with 95% confidence intervals (discrimination) and the Hosmer-Lemeshow statistics (calibration, the larger the p-value, the better the fit).
Results
Patient Population and Injury Patterns
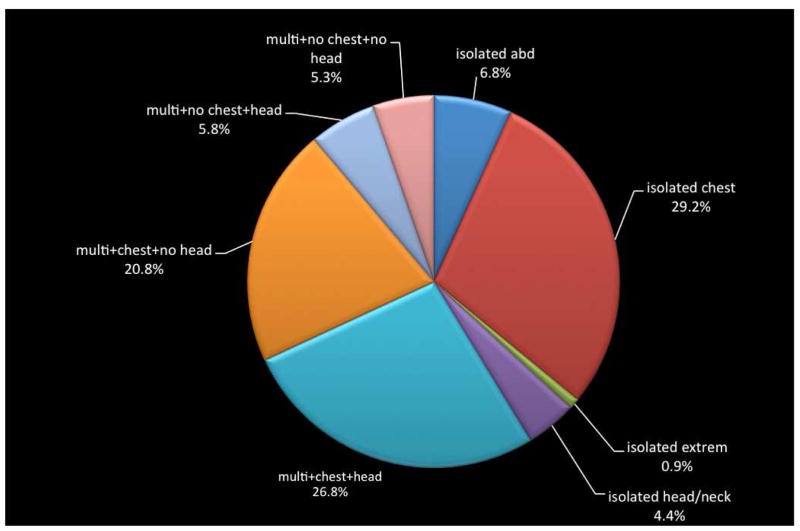
During the 40-year study period, 1,708 patients underwent an EDT at Denver Health Medical Center (DHMC). DHMC is an American College of Surgeons Committee on Trauma and state designated level 1 trauma center. The median age was 30 years (IQR 23–43); 81% of patients were men, and 79% underwent prehospital CPR. Temporal trends can be appreciated in table 1. Overall survival rate was 6.2%. Penetrating wounds occurred in 52% of patients and 59% of patients had multisystem trauma. The chest was the most common injury location (77%) followed by abdomen (49%), head/neck (37%) and extremity (37%). Isolated chest injuries represented nearly one-third of all patients, while isolated extremity was the least common in 0.8% (Figure 1).
Table 1.
Trends in Patient Demographics and Injury Patterns over Time
| 1975–1979 | 1980–1984 | 1885–1989 | 1990–1994 | 1995–1999 | 2000–2004 | 2005–2009 | 2010–2014 | |
|---|---|---|---|---|---|---|---|---|
| n | 252 | 258 | 287 | 194 | 184 | 192 | 164 | 177 |
| Demographics | ||||||||
| Median age, y | 28 | 29 | 32 | 30 | 29 | 31 | 28 | 34 |
| IQR | 22–41 | 23–39 | 22–45 | 22–42 | 21.5–43 | 23.5–42.5 | 22–42.5 | 24–47 |
| Male sex | ||||||||
| n | 198 | 209 | 221 | 150 | 151 | 166 | 138 | 131 |
| % | 78.6 | 81.0 | 77.0 | 77.3 | 82.1 | 86.5 | 84.7 | 87.3 |
| Injury characteristics | ||||||||
| Penetrating | ||||||||
| n | 146 | 116 | 122 | 113 | 105 | 108 | 107 | 88 |
| % | 57.9 | 45.0 | 42.5 | 58.3 | 57.1 | 56.3 | 65.2 | 49.7 |
| Treatment, pre-hospital CPR | ||||||||
| n | 209 | 203 | 227 | 156 | 144 | 143 | 130 | 120 |
| % | 82.9 | 78.7 | 79.7 | 80.8 | 78.3 | 74.5 | 79.8 | 79.0 |
Figure 1.
Distribution of injuries of patients undergoing emergency deparment thoracotomy during the study period. abd, abdominal injury; multi, multiple system trauma; extrem, extremity injury.
Temporal Trends
The average number of EDT per year decreased during the study period (Table 2). In the first five years of the study period, 50.4 patients per year underwent EDT compared to the last five years when EDT averaged 35 per year. The peak rate of EDT was during 1985–1989 when 57 patients per year received this procedure. This rate markedly dropped over the next five-year time frame to 39 patients per year.
Table 2.
Trends in Emergency Department Thoracotomy Outcomes over Time
| Quin-quennial, 5-y | EDT/y, average | Success-to-rescue, % | Survive OR, % | Penetrating survivors, % | Blunt survivors, % | Survivors per 5 y, n | Overall survival, % |
|---|---|---|---|---|---|---|---|
| 1975–79 | 50 | 23 | 6 | 8 | 1 | 12 | 5 |
| 1980–84 | 52 | 27 | 6 | 6 | 2 | 10 | 4 |
| 1985–89 | 57 | 19 | 6 | 7 | 3 | 13 | 5 |
| 1990–94 | 39 | 22 | 7 | 7 | 3 | 9 | 5 |
| 1995–99 | 37 | 17 | 7 | 9 | 3 | 11 | 6 |
| 2000–04 | 38 | 28 | 10 | 13 | 2 | 16 | 8 |
| 2005–09 | 33 | 30 | 10 | 8 | 4 | 11 | 7 |
| 2010–14 | 35 | 35 | 18 | 13 | 15 | 24 | 14 |
EDT, emergency department thoracotomy.
The percentage of men undergoing EDT significantly increased over time (p=0.003 table 1) from 78% during the first five years to 87% in the most recent five years. The percentage of patients undergoing prehospital CPR did not change significantly over time (p=0.219 table 1), but injury patterns of patients undergoing this procedure changed over time. Penetrating wounds tended to increase over time (p=0.052). Multisystem injuries were present in 68% of patients during the last five years compared to 49% in the first five years (p<0.001) and reflects an increase in the number of patients with thoracic (p<0.001), abdominal (p=0.004), and extremities injuries (p<0.001) but no difference in head injuries (p=0.835).
Outcomes
Success to rescue
There were 419 patients (24.5%) that had success to rescue. Of the 419 patients who arrived in the operating room, 147 (35%) survived to intensive care unit admission. Of the 147 who survived the OR 106 (72%) survived their hospitalization. The unadjusted success to rescue increased over time from 22% in 1975–79 to 35% in 2010–2014 (p=0.001). After adjusting for other predictors (pre-hospital CPR, age, sex, penetrating mechanism, and injury patterns), success to rescue during the study period increased (p<0.0001), especially in the last five years (OR=2.5, 95%CI: 1.5–4.2) compared to 1975–79. This model had good discrimination (AUROC 0.78 95% CI: 0.75–0.80) and calibration (H-L, p=0.3778). The percent of patients who survived the OR did not change over time (p=0.743). Among patients who survived the OR after EDT, there were no differences in age, sex, or pre-hospital CPR between those who survived the hospital stay and those who died in the intensive care unit.
Overall survival
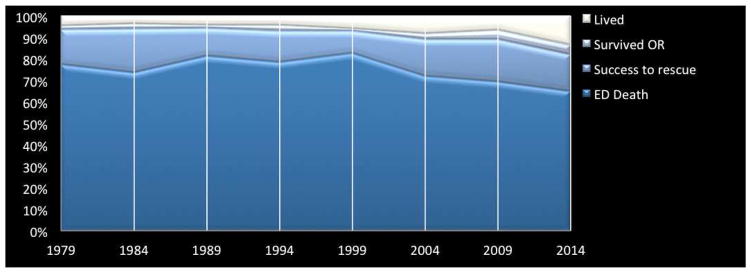
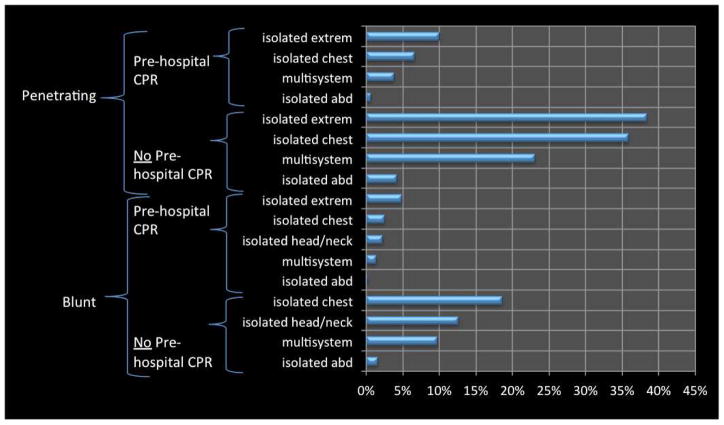
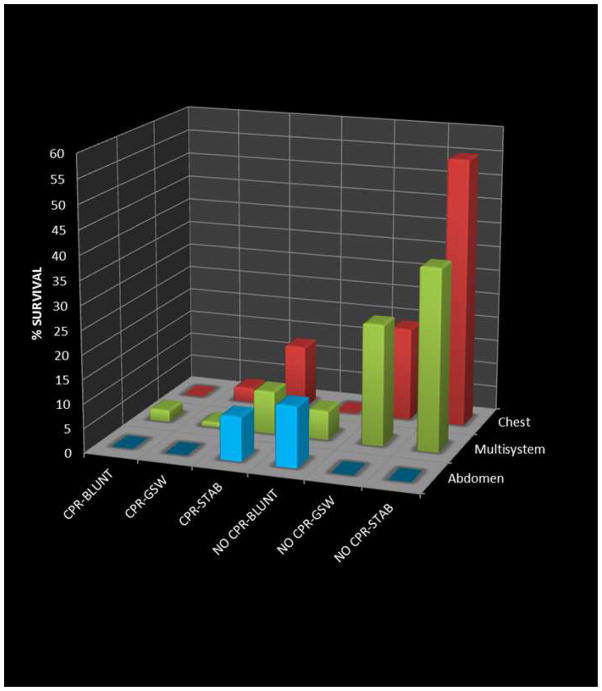
Survival significantly increased over time (p<0.001) from 5% in 1974–79 to 14% in 2010–2014 (Figure 2). Injury patterns and pre hospital had were associated with wide range of survival patterns (Figure 3). Patients that survived to leave the hospital, were significantly more likely to have a thoracic injury (with or without other injuries, p=0.004). Survival patterns for isolated abdominal trauma (p=0.885), and multisystem trauma (p=0.149) did not increase over time, while survivors with isolated chest injuries (p=0.002) improved overtime. Nevertheless, when controlling for presence of thoracic injuries survival significantly improved over time (p=0.019). The largest improvement in survival was observed in patients with blunt trauma over the last five years that surpassed survival rates in penetrating injuries (Table 2). With further stratification of the injury mechanism, patients with stab wounds had the highest survival rates (Figure 4).
Figure 2.
Changes in outcomes of emergency department thoracotomy over time. The percent of total patients per outcome are summed to 100% on the Y axis over 5-year intervals, which are displayed on the X axis and progress from the earliest study time point on the left to the most recent study period on the right. abd, abdomen; CPR, cardiopulmonary resuscitation; ED, emergency department; extrem, extremity injury; OR, operating room; Success-to-rescue, return of spontaneous circulation with systolic blood pressure of greater than 70 mmHg and transfer to operating room; Survived OR, survived first operative procedure and successfully transported to the intensive care unit postoperatively.
Figure 3.
Percent survival of patients based on injury pattern and blunt vs penetration trauma. CPR, cardiopulmonary resuscitation; extreme, extremity injury; abd, abdominal injury; multisystem, injuries to multiple body regions.
Figure 4.
Three-dimensional survival patterns based off of injury mechanism, location, and undergoing pre-hospital cardiopulmonary resuscitation (CPR). BLUNT includes: motor cycle crash, motor vehicle crash, and auto-pedestrian; GSW, gunshot wound; STAB, stab injury.
Defining benchmarks
Patients with prehospital CPR had a crude survival rate of 10% compared to patients without CPR who had a 3-fold improvement in survival at 34%. Survival improved over time, regardless of whether the patient underwent prehospital CPR (p=0.022) or not (p<0.001). Survival based on injury pattern and the effect modification of pre hospital CPR can be appreciated in Figure 3. The overall survival model had good discrimination (AUROC 0.80, 95%CI: 0.75–0.84) and calibration (Hosmer-Lemeshow statistics p=0.92).
Long-term outcome
Of the survivors, 68% had a no permanent neurologic deficits and 12% had mild neurologic disability based on GOS scoring(18). The remaining 20% were in a persistent vegetative state (n=17), died outside of the hospital (n=2) or were lost to follow-up (n=2).
Discussion
Emergency department thoracotomy for circulatory arrest from trauma remains a life saving procedure. In our high volume trauma center with routine performance of this procedure, survival has significantly improved over time. While the rate of EDT has decreased over time, suggesting improved patient selectivity, additional factors are likely responsible for the improvement in outcomes. There is a clear survival benefit of this procedure in patients with penetrating thoracic injuries. However, recovering from circulatory arrest for abdominal injuries remains a challenge. In addition to anatomic injury patterns, requiring prehospital CPR is associated with a significant decrease in survival. Interestingly, survival from blunt trauma has increased over the past 5 years. In the modern era of this procedure at our institution one in three patients is successfully resuscitated with a thoracotomy in the emergency department, and overall 14% of these patients survive with good neurologic outcomes.
The overall survival pattern in these patients is consistent with previously reported literature for penetrating chest injuries (4, 8, 19) and signs of life/no pre hospital CPR (6, 20–22). However, nearly 80% of trauma patients had CPR prior to EDT. It has been validated by our center(23) and in multicenter evaluation(24) that trauma patients with penetrating wounds undergoing less than 15 minutes of prehospital CPR can be salvaged with good neurologic outcomes. While EDT performed for isolated head/neck or extremity injury had high survival percentages (Figure 3), those patients that survived with isolated head injuries remained in persistent vegetative states. All of the patients with blunt isolated head/neck injuries had suspicion for polysystem trauma, which were confined to the head and neck after imaging or exploration in the operating room. While EDT performed for non torso trauma has previously been reported to be successful (25), the role in isolated head remains unclear; importantly, none of these patients had gun shot wounds. Interestingly blunt trauma improved during the last five years of this study. The largest change in patient care over the past five years has been related to early plasma and goal directed resuscitation(26). Prospectively data indicates that early plasma and not necessarily the ratio of blood products improves survival(27). Plasma has been shown in vitro to not only improve coagulation but buffer fibrinolysis and metabolic derangements(28), which are essential in a patient in extremis. While this hypothesis requires additional investigation, improvement in patient selection has also played a role.
Refining patient selection to improve the cost effectiveness of this procedure has been an ongoing emphasis in an effort to reduce health care cost (4, 7). In fact, our group was the first to raise this issue in 1979 (3), and again 15 years ago [28]; we suggested that optimizing EDT outcomes could be associated with a 32% reduction in procedures with the same number of survivors(29). In this previous report EDT rates were 41/yr over a 23-year period. This rate has dropped by 26% over the last 5 years compared to our prior publication, and there has been an associated increase in survival from 4.4% to 14%. A marked reduction in presumably futile EDT in the late 1980’s is illustrated in Figure 2 and Table 2. This selectivity also coincides with the increased concerns for risk of iatrogenic transmission of human immunodeficiency virus (HIV) from sharp instruments (30). The risks of iatrogenic self injury cannot be ignored with this procedure; the sero-conversion of blood borne pathogens from this procedure is estimated to be 1 in 1000 cases(31). Providers should be aware of this risk, and coordinated efforts to minimize accidental inflicted injuries including a pre-established role of care providers.
Regionalization of high-risk elective surgery has been shown to improve patient outcomes(12, 14). This should translate in trauma, however, it has been reported that trauma level status, and not trauma volume, correlates to outcome(15). The problem with this conclusion is that not all seriously injured patients are at high risk of death from hemorrhage. Injury severity does not take into consideration the patients physiologic status and active bleeding. It is important for a level I trauma center to be capable of gaining rapid hemorrhage control as 40% of trauma deaths are attributed to hemorrhage and considered to be the most common cause of preventable death(10). EDT and REBOA are complementary in achieving this goal, but should be applied to the appropriate patient for optimal outcomes.
Previous studies have not reported success to rescue from circulatory arrest as a potential outcome for quality measures. The importance of this marker on hospital performance is twofold: 1) reflective of the trauma surgeons ability to control life threatening hemorrhage and 2) provides a frame work for the future refinement of resuscitation strategies of patients with previously presumed lethal injuries which in the future may be amenable to advanced techniques such as extracorporeal circulatory support(32) or suspended animation(33). The EDT success to rescue rate has potential to be considered a benchmark for outcomes at level I trauma centers, and could assist in developing optimal trauma systems. Prospective studies are warranted to investigate if level 1 trauma centers should also be designated as a high preforming EDT center (based on success to rescue) to help guide EMS services triage critically injured patients for improving patient outcomes. These studies should include cost analysis, number of productive years lost, and survivor quality of life assessments. EDT performance has implication for policy reform. Trauma level designation at the state and national level of level I trauma centers could be set at a minimum requirement for success to rescue from circulatory arrest. This is particularly timely with the respect to ACS/COT position that level II trauma centers provide equivalent care to level I. Our recent geospatial analysis of Colorado indicates that there are too many high-level trauma centers.
In reality, if no patients in traumatic arrest underwent an EDT and were declared dead on arrival (DOA), there would be a reduction in cost to the hospital as well as valuable resources such as blood products, ED and OR time. However, in the modern era, if a high volume center can rescue 1 in 3 trauma patients from circulatory arrest and have an overall 14% survival rate, the cost is justified. As technology improves patients who survive to the OR are likely to have improved overall survival in the future. By forgoing this life saving procedure, advances in trauma will be limited to the most severely injured patients undergoing attempted resuscitation. Furthermore, there are potential benefits to society by providing viable organs for transplantation(34).
REBOA has been implemented as an alternative to EDT(17), but the precise role remains to be defined(35) REBOA is a rational approach for select patients, and success has been impressive, particularly with bleeding from major pelvic fractures (36). However, the technique must be learned systematically as complications reported from Japan(37) have been concerning. We believe it is imperative for all trauma surgeons in level 1trauma centers to be trained to perform REBOA as well as EDT. Future prospective studies contrasting EDT to REBOA with well-matched patients based on injury patterns and prehospital physiologic parameters are essential.
In conclusion, hemorrhage is the most common cause of preventable death of young individuals in the United States. Benchmarking trauma centers on success to rescue may help delineate high preforming centers and better define a needs base assessment of regional trauma systems. We submit EDT remains the gold standard for thoracic trauma and REBOA should be considered as an alternative approach for abdominal and pelvic injuries, however these indications need to be established by randomized control trials.
Acknowledgments
Support: This study was supported in part by National Institute of General Medical Sciences grants T32-GM008315 and P50-GM49222.
Footnotes
Disclosure Information: Dr Ernest Moore received grants to his institution for supplies and some salaries from Haemonetics and TEM research. All other authors have nothing to disclose.
Disclosures outside of the scope of this work: Dr Hunter Moore’s institution receives royalties from UpToDate; and Dr Fox is an unpaid clinical advisory board member of Prytime Medical Devices, Inc.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIGMS, or National Institutes of Health.
Presented at the Western Surgical Association 123rd Scientific Session, Napa Valley, CA, November 2015.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Beall AC, Jr, Diethrich EB, Cooley DA, DeBakey ME. Surgical management of penetrating cardiovascular trauma. Southern Med J. 1967;60:698–704. doi: 10.1097/00007611-196707000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Baker CC, Thomas AN, Trunkey DD. The role of emergency room thoracotomy in trauma. J Trauma. 1980;20:848–855. doi: 10.1097/00005373-198010000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Moore EE, Moore JB, Galloway AC, Eiseman B. Postinjury thoracotomy in the emergency department: a critical evaluation. Surgery. 1979;86:590–598. [PubMed] [Google Scholar]
- 4.Rhee PM, Acosta J, Bridgeman A, et al. Survival after emergency department thoracotomy: review of published data from the past 25 years. J Am Coll Surg. 2000;190:288–298. doi: 10.1016/s1072-7515(99)00233-1. [DOI] [PubMed] [Google Scholar]
- 5.Passos EM, Engels PT, Doyle JD, et al. Societal costs of inappropriate emergency department thoracotomy. J Am Coll Surg. 2012;214:18–25. doi: 10.1016/j.jamcollsurg.2011.09.020. [DOI] [PubMed] [Google Scholar]
- 6.Esposito TJ, Jurkovich GJ, Rice CL, et al. Reappraisal of emergency room thoracotomy in a changing environment. J Trauma. 1991;31:881–885. doi: 10.1097/00005373-199107000-00001. discussion 885–887. [DOI] [PubMed] [Google Scholar]
- 7.Brown SE, Gomez GA, Jacobson LE, et al. Penetrating chest trauma: should indications for emergency room thoracotomy be limited? Am Surg. 1996;62:530–533. discussion 533–534. [PubMed] [Google Scholar]
- 8.Shafi S, Barnes SA, Rayan N, et al. Compliance with recommended care at trauma centers: association with patient outcomes. J Am Coll Surg. 2014;219:189–198. doi: 10.1016/j.jamcollsurg.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 9.Burlew CC, Moore EE. Emergency Department Thoracotomy. 7. McGraw Hill; 2013. [Google Scholar]
- 10.Sauaia A, Moore FA, Moore EE, et al. Epidemiology of trauma deaths: a reassessment. J Trauma. 1995;38:185–193. doi: 10.1097/00005373-199502000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Tisherman SA, Schmicker RH, Brasel KJ, et al. Detailed description of all deaths in both the shock and traumatic brain injury hypertonic saline trials of the Resuscitation Outcomes Consortium. Ann Surg. 2015;261:586–590. doi: 10.1097/SLA.0000000000000837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gonzalez AA, Dimick JB, Birkmeyer JD, Ghaferi AA. Understanding the volume-outcome effect in cardiovascular surgery: the role of failure to rescue. JAMA Surg. 2014;149:119–123. doi: 10.1001/jamasurg.2013.3649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sosa JA, Bowman HM, Gordon TA, et al. Importance of hospital volume in the overall management of pancreatic cancer. Ann Surg. 1998;228:429–438. doi: 10.1097/00000658-199809000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ghaferi AA, Birkmeyer JD, Dimick JB. Hospital volume and failure to rescue with high-risk surgery. Medical Care. 2011;49:1076–1081. doi: 10.1097/MLR.0b013e3182329b97. [DOI] [PubMed] [Google Scholar]
- 15.Demetriades D, Martin M, Salim A, et al. The effect of trauma center designation and trauma volume on outcome in specific severe injuries. Ann Surg. 2005;242:512–517. doi: 10.1097/01.sla.0000184169.73614.09. discussion 517–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Margulies DR, Cryer HG, McArthur DL, et al. Patient volume per surgeon does not predict survival in adult level I trauma centers. J Trauma. 2001;50:597–601. doi: 10.1097/00005373-200104000-00002. discussion 603. [DOI] [PubMed] [Google Scholar]
- 17.Brenner ML, Moore LJ, DuBose JJ, et al. A clinical series of resuscitative endovascular balloon occlusion of the aorta for hemorrhage control and resuscitation. J Trauma Acute Care Surg. 2013;75:506–511. doi: 10.1097/TA.0b013e31829e5416. [DOI] [PubMed] [Google Scholar]
- 18.Wilson JT, Pettigrew LE, Teasdale GM. Structured interviews for the Glasgow Outcome Scale and the extended Glasgow Outcome Scale: guidelines for their use. J Neurotrauma. 1998;15:573–585. doi: 10.1089/neu.1998.15.573. [DOI] [PubMed] [Google Scholar]
- 19.Lustenberger T, Labler L, Stover JF, Keel MJ. Resuscitative emergency thoracotomy in a Swiss trauma centre. Br J Surg. 2012;99:541–548. doi: 10.1002/bjs.7706. [DOI] [PubMed] [Google Scholar]
- 20.Siram S, Oyetunji T, Johnson SM, et al. Predictors for survival of penetrating trauma using emergency department thoracotomy in an urban trauma center: the Cardiac Instability Score. J National Med Assoc. 2010;102:126–130. doi: 10.1016/s0027-9684(15)30500-9. [DOI] [PubMed] [Google Scholar]
- 21.Cera SM, Mostafa G, Sing RF, et al. Physiologic predictors of survival in post-traumatic arrest. Am Surg. 2003;69:140–144. [PubMed] [Google Scholar]
- 22.Roberge RJ, Ivatury RR, Stahl W, Rohman M. Emergency department thoracotomy for penetrating injuries: predictive value of patient classification. Am J Emerg Med. 1986;4:129–135. doi: 10.1016/0735-6757(86)90157-9. [DOI] [PubMed] [Google Scholar]
- 23.Powell DW, Moore EE, Cothren CC, et al. Is emergency department resuscitative thoracotomy futile care for the critically injured patient requiring prehospital cardiopulmonary resuscitation? J Am Coll Surg. 2004;199:211–215. doi: 10.1016/j.jamcollsurg.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 24.Moore EE, Knudson MM, Burlew CC, et al. Defining the limits of resuscitative emergency department thoracotomy: a contemporary Western Trauma Association perspective. J Trauma. 2011;70:334–339. doi: 10.1097/TA.0b013e3182077c35. [DOI] [PubMed] [Google Scholar]
- 25.Sheppard FR, Cothren CC, Moore EE, et al. Emergency department resuscitative thoracotomy for nontorso injuries. Surgery. 2006;139:574–576. doi: 10.1016/j.surg.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 26.Gonzalez E, Moore EE, Moore HB, et al. Goal-directed hemostatic resuscitation of trauma-induced coagulopathy: a pragmatic randomized clinical trial comparing a viscoelastic assay to conventional coagulation assays. Ann Surg. 2015 Dec 28; doi: 10.1097/SLA.0000000000001608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Holcomb JB, Tilley BC, Baraniuk S, et al. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial. JAMA. 2015;313:471–482. doi: 10.1001/jama.2015.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moore HB, Moore EE, Gonzalez E, et al. Plasma is the physiologic buffer of tissue plasminogen activator-mediated fibrinolysis: rationale for plasma-first resuscitation after life-threatening hemorrhage. J Am Coll Surg. 2015;220:872–879. doi: 10.1016/j.jamcollsurg.2015.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Branney SW, Moore EE, Feldhaus KM, Wolfe RE. Critical analysis of two decades of experience with postinjury emergency department thoracotomy in a regional trauma center. J Trauma. 1998;45:87–94. doi: 10.1097/00005373-199807000-00019. discussion -95. [DOI] [PubMed] [Google Scholar]
- 30.Kelen GD. Human immunodeficiency virus and the emergency department: risks and risk protection for health care providers. Ann Emerg Med. 1990;19:242–248. doi: 10.1016/s0196-0644(05)82037-2. [DOI] [PubMed] [Google Scholar]
- 31.Sikka R, Millham FH, Feldman JA. Analysis of occupational exposures associated with emergency department thoracotomy. J Trauma. 2004;56:867–872. doi: 10.1097/01.ta.0000082686.93669.10. [DOI] [PubMed] [Google Scholar]
- 32.Tseng YH, Wu TI, Liu YC, et al. Venoarterial extracorporeal life support in post-traumatic shock and cardiac arrest: lessons learned. Scand J Trauma Resuscitation Emergency Med. 2014;22:12. doi: 10.1186/1757-7241-22-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tisherman SA. Salvage techniques in traumatic cardiac arrest: thoracotomy, extracorporeal life support, and therapeutic hypothermia. Curr Opinion Crit Care. 2013;19:594–598. doi: 10.1097/MCC.0000000000000034. [DOI] [PubMed] [Google Scholar]
- 34.Schnuriger B, Inaba K, Branco BC, et al. Organ donation: an important outcome after resuscitative thoracotomy. J Am Coll Surg. 2010;211:450–455. doi: 10.1016/j.jamcollsurg.2010.06.012. [DOI] [PubMed] [Google Scholar]
- 35.Biffl WL, Fox CJ, Moore EE. The role of REBOA in the control of exsanguinating torso hemorrhage. J Trauma Acute Care Surg. 2015;78:1054–1058. doi: 10.1097/TA.0000000000000609. [DOI] [PubMed] [Google Scholar]
- 36.Moore LJ, Brenner M, Kozar RA, et al. Implementation of resuscitative endovascular balloon occlusion of the aorta as an alternative to resuscitative thoracotomy for noncompressible truncal hemorrhage. J Trauma Acute Care Surg. 2015;79:523–532. doi: 10.1097/TA.0000000000000809. [DOI] [PubMed] [Google Scholar]
- 37.Saito N, Matsumoto H, Yagi T, et al. Evaluation of the safety and feasibility of resuscitative endovascular balloon occlusion of the aorta. J Trauma Acute Care Surg. 2015;78:897–903. doi: 10.1097/TA.0000000000000614. discussion 904. [DOI] [PubMed] [Google Scholar]