Abstract
Introduction
Ultrasound (US) is the preferred imaging modality for evaluating appendicitis. Our purpose was to determine if including secondary signs (SS) improves diagnostic accuracy in equivocal US studies.
Methods
Retrospective review identified 825 children presenting with concern for appendicitis and with a right lower quadrant (RLQ) US. Regression models identified which SS were associated with appendicitis. Test characteristics were demonstrated.
Results
530 patients (64%) had equivocal US reports. Of 114 (22%) patients with equivocal US undergoing CT, those with SS were more likely to have appendicitis (48.6% vs 14.6%, p<0.001). Of 172 (32%) patients with equivocal US admitted for observation, those with SS were more likely to have appendicitis (61.0% vs 33.6%, p<0.001). SS associated with appendicitis included fluid collection (adjusted odds ratio (OR) 13.3, 95% Confidence Interval (CI) 2.1–82.8), hyperemia (OR=2.0, 95%CI 1.5–95.5), free fluid (OR=9.8, 95%CI 3.8–25.4), and appendicolith (OR=7.9, 95%CI 1.7–37.2). Wall thickness, bowel peristalsis, and echogenic fat were not associated with appendicitis. Equivocal US that included hyperemia, a fluid collection, or an appendicolith had 96% specificity and 88% accuracy.
Conclusion
Use of SS in RLQ US assists in the diagnostic accuracy of appendicitis. SS may guide clinicians and reduce unnecessary CT and admissions.
Keywords: pediatric surgery, appendicitis, secondary signs, ultrasound, quality improvement
1.0 Background
Despite appendicitis representing the leading cause of pediatric abdominal pain requiring emergent surgery, the clinical diagnosis remains challenging. Diagnostic imaging is often required, and its use has dramatically decreased the negative appendectomy rate1. Ultrasound (US) of the right lower quadrant (RLQ) is recommended by the American College of Radiology and the American Academy of Pediatrics as the initial imaging modality in evaluating pediatric appendicitis2,3; however, there is wide variation in the use of diagnostic imaging4–7. US provides a safe, non-invasive option that avoids radiation exposure while providing useful diagnostic information8–11. The user-dependency of US is reflected by a wide appendix visualization rate ranging from 40% to 89%12–16. Furthermore, differences in intra-institutional appendix visualization rates exist depending on whether the study is performed by a pediatric radiologist or a pediatric radiology technologist (75% vs 54%)17. When the appendix is visualized, US typically has a sensitivity (SN) ranging from 86% to 100% and specificity (SP) ranging from 88 to 98%1,10,13,18.
US studies that fail to fully visualize the appendix are considered equivocal and are often followed by computed tomography scans (CT) or hospital admissions for observation19. CTs are an accurate diagnostic tool with reports of SN ranging from 95 to 97% and SP ranging from 94 to 97%1. In addition to the expense of CTs, CTs expose children to ionizing radiation, increasing their risk of subsequent cancer development9,20–22. In effort to increase the diagnostic accuracy of US, investigators have proposed combining equivocal US studies with additional data such as laboratory values or sonographic secondary signs of appendicitis16,17,23–25. These results have not been widely validated, and the clinical utility of secondary signs has not been generally accepted. Secondary signs are sonographic descriptions of the anatomy of structures surrounding the appendix and include fluid collections, free fluid, echogenic fat, hyperemia, abnormal lymph nodes, abnormal adjacent bowel, bowel wall edema, and appendicoliths11,23. The purpose of our study is to evaluate if the use of secondary signs in equivocal US reports improves the diagnostic accuracy of US for pediatric appendicitis.
2.0 Methods
2.1 Patient Selection
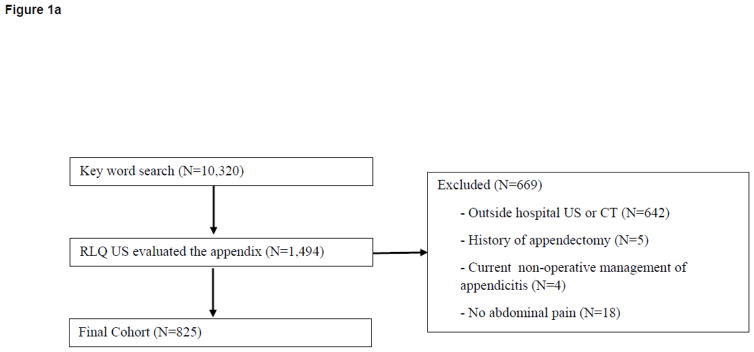
After obtaining approval from the Emory University Internal Review Board (#00077519), we performed a retrospective chart review for patients (ages 5–18 years) who presented to one of two pediatric emergency departments of a university-affiliated tertiary care facility between January 1, 2014 and December 31, 2014. The initial cohort was identified using language recognition software to examine the chief complaints as listed in the electronic medical record. Search terms included: “abd,” “appy,” “stomach,” “appendicitis,” and “rlq”. The key word search identified 10,320 visits. Patients were included if they had concern for appendicitis and received a RLQ US that evaluated the appendix. Patients were excluded if they underwent an US or CT for their abdominal pain at an outside hospital, if they had a history of an appendectomy, if they were currently being non-operatively managed for appendicitis, or if they did not have abdominal pain (Figure 1A).
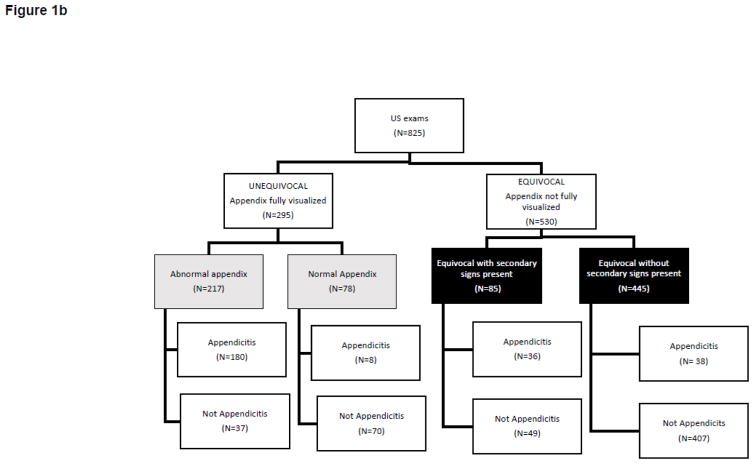
Figure 1.
(A) Inclusion and exclusion of patients being evaluated for appendicitis who underwent a right lower quadrant (RLQ) ultrasound (US) in 2014 at a tertiary care children’s referral center. (B) US classification and confirmed diagnosis of the patients in the included cohort.
2.2 Variables and outcome definitions
Final US reports were reviewed by two authors (KP, AP) for primary and secondary signs of appendicitis. The primary sign of appendicitis was a fully visualized appendix with a diameter greater than or equal to 6mm23. Secondary signs included fluid collections consistent with abscesses (fluid collections), a significant amount of abdominal free fluid (free fluid), hyperechogenicity of periappendiceal fat (echogenic fat), increased regional bowel vascularity (hyperemia), the presence of enlarged or supranumery mesenteric lymph nodes (abnormal lymph nodes), hypoperistalsis or dilation of adjacent bowel loops (abnormal adjacent bowel), bowel wall edema, and appendicoliths11,23. As has been previously described, US reports were classified into four categories: 1. Normal; 2. Equivocal without SS; 3. Equivocal with SS; and 4. Appendicitis23,24,26. Categories 1 and 4 included a fully visualized appendix and were collectively referred to as unequivocal. Categories 2 and 3 included US in which the appendix was not fully visualized and were collectively referred to as equivocal. The final diagnosis of each patient was recorded as either appendicitis or not appendicitis as shown in Figure 1B. Appendicitis was confirmed through review of operative reports, pathology results, and CT impressions when CT was performed. Each patient’s electronic medical record was examined for details regarding the clinical course and any re-admissions. For patients diagnosed as not having appendicitis, chart review ensured appendicitis was not diagnosed in the 30 days after the initial presentation. Based on our status as the pediatric referral center, patients were expected to return to our system if medical care was needed.
2.3 Reporting validation
Two pediatric radiologists (JL, KB) reviewed a sample of patients’ ultrasounds for the presence of SS. The sample included 5% of the patients with equivocal US that had no SS mentioned within radiologic reports. Furthermore, all patients with equivocal US that had no SS mentioned and were diagnosed with appendicitis had their initial US studies reviewed. If a SS was not mentioned in the report, then the SS was likely not present on the US as validation revealed that only 7% of SS were missed on the original reports as shown in Table 1. Of all the SS not mentioned in the original report but present on secondary review, echogenic fat and significant free fluid were the most likely to be present (18% and 21% respectively).
Table 1.
Validation of findings on ultrasound reports by re-review of source images by two attending radiologists through random selection of 50 studies. Secondary signs that were not mentioned in the radiologic reports were assumed to be absent. This assumption was challenged and accuracy is reported.
| Not Present | Present | % Missed | Accuracy | |
|---|---|---|---|---|
| Hyperemia | 42 | 2 | 4.76% | 95.24% |
| Echogenic fat | 38 | 7 | 18.42% | 81.58% |
| Appendicolith | 42 | 1 | 2.38% | 97.62% |
| Abnormal lymph nodes | 43 | 0 | 0.00% | 100.00% |
| Fluid collection | 34 | 0 | 0.00% | 100.00% |
| Free fluid | 19 | 4 | 21.05% | 78.95% |
| Abnormal adjacent bowel | 36 | 2 | 5.56% | 94.44% |
| Bowel wall edema | 33 | 3 | 9.09% | 90.91% |
|
| ||||
| Total | 287 | 19 | 6.62% | 93.38% |
2.4 Imaging techniques
All US examinations were performed by a certified ultrasound technician and were interpreted by an attending pediatric radiologist. A graded compression technique was performed in an attempt to locate the appendix using either a Philips iU22 or Philips Epiq with the Curved 5–1 array and Linear 9 array probes.
2.5 Data analysis
Descriptive statistics were calculated for all variables of interest and include means and standard deviations or frequencies and percentages, as appropriate. Statistical significance was assessed at the 0.05 level unless otherwise noted. Equivocal and unequivocal US patient demographics were compared using Chi-square and t-tests where applicable. For equivocal US studies (Categories 2 and 3) the association between final outcome of appendicitis and secondary signs was compared using Chi-square tests. Logistic regression was used to assess the adjusted association between appendicitis diagnosis and secondary signs. Individual secondary signs and demographic characteristics including race, sex, and age were included in the model. A separate logistic regression model was created to test the association between appendicitis diagnosis and number of secondary signs present. Race, sex, and age were also included in this model. Association between outcome and SS was quantified using odds ratios and corresponding 95% confidence intervals. Diagnostic test characteristics, including SN, SP, predictive values, and accuracy, were demonstrated for different test criteria. Criteria designating a positive test included ≥ 1 secondary sign present, ≥ 2 secondary signs present, 3 secondary signs present, and ≥ 1 of the three most highly associated secondary signs present. Statistical analyses were performed using SAS 9.4 (Cary, NC).
3.0 Theory
We hypothesized that among patients with an equivocal US, the presence of SS would increase the likelihood of patients having appendicitis. Furthermore, we hypothesized that specific SS and an increasing number of SS would be associated with a diagnosis of appendicitis.
4.0 Results
4.1 Ultrasound categories and outcomes
We identified 825 children who presented with concern for appendicitis and a RLQ US. Of the 825 patients, 295 (36%) had fully visualized appendices (referred to as unequivocal US) and 530 (64%) had equivocal US. The prevalence of appendicitis was 32% (262/830). Using ≥6mm as the maximal outer diameter of an abnormal appendix, the accuracy of unequivocal US was 85%. The patient demographics between the equivocal and unequivocal groups differed in that patients with equivocal US reports were more likely to be female and older (Table 2). Among the patients with equivocal US reports, 114 patients (22%) underwent CT and 172 patients (32%) were admitted for observation. Of the 114 patients with equivocal US undergoing CT, those with SS were more likely to have appendicitis (48.6% vs 14.6%, p<0.001). Of the 172 patients with equivocal US admitted for observation, those with SS were more likely to have appendicitis (61.0% vs 33.6%, p<0.001).
Table 2.
Characteristics of patients with high clinical suspicion for appendicitis based on equivocal or unequivocal right lower quadrant ultrasounds in 2014
| Characteristic | Overall (N = 825) | Equivocal US (N = 530) | Unequivocal US (N = 295) | p-value |
|---|---|---|---|---|
| Race | ||||
| White | 516 (62.6%) | 334 (63.0%) | 182 (61.7%) | 0.884 |
| Black | 214 (25.9%) | 137 (25.9%) | 77 (26.1%) | |
| Other | 95 (11.5%) | 59 (11.1%) | 36 (12.2%) | |
| Sex | ||||
| Male | 361 (36.8%) | 193 (36.4%) | 168 (57.0%) | <0.001* |
| Female | 464 (56.2%) | 337 (63.6%) | 127 (43.0%) | |
| Age, mean ± sd | 11.4 ± 3.6 | 11.7 ± 3.7 | 10.8 ± 3.4 | 0.001* |
| PAS Score, mean ± sd | 6.5 ± 1.8 | 6.2 ± 1.8 | 6.9 ± 1.7 | <0.001* |
| Imaging Pathway | ||||
| US with CT | 137 (16.6%) | 117 (22.1%) | 20 (6.8%) | <0.001* |
| US only | 688 (83.4%) | 413 (77.9%) | 275 (93.2%) | |
CT – computed tomography, PAS – pediatric appendicitis score, sd = standard deviation, US - ultrasound
4.2 Secondary signs association with appendicitis
On univariate analyses, all SS were associated with appendicitis except enlarged lymph nodes (Table 3). After fully adjusting for age, sex, race, and other SS, the SS that were associated with appendicitis included fluid collection (adjusted odds ratio (OR) 13.3, 95% Confidence Interval (95%CI) 2.1–82.8), hyperemia (OR 12.0, 95%CI 1.5 – 95.5), free fluid (OR 9.8, 95%CI 3.8 – 25.4), and appendicolith (OR 7.9, 95%CI 1.7 – 37.2). Bowel wall edema, abnormal adjacent bowel and echogenic fat were not associated with appendicitis in the fully adjusted model.
Table 3.
Demographic characteristics and presence of secondary signs in patients with equivocal ultrasound studies stratified by final diagnosis.
| Overall (N = 530) | Appendicitis (N = 74) | No Appendicitis (N = 456) | p-value | ORa | 95% CI | |
|---|---|---|---|---|---|---|
| Race | ||||||
| White | 334 (63.0%) | 52 (70.3%) | 282 (61.8%) | 0.291 | Ref | - |
| Black | 137 (25.9%) | 17 (23.0%) | 120 (26.3%) | 0.49 | (0.24, 1.02) | |
| Other | 59 (11.1%) | 5 (6.8%) | 54 (11.8%) | 0.30 | (0.09, 1.01) | |
| Sex | ||||||
| Male | 193 (36.4%) | 40 (54.0%) | 153 (33.5%) | 0.001* | Ref | - |
| Female | 337 (63.6%) | 34 (46.0%) | 303 (66.5%) | 0.43 | (0.23, 0.79) | |
| Age | ||||||
| 5–9 | 160 (30.2%) | 24 (32.4%) | 136 (29.8%) | 0.179 | 1.14 | (0.50, 2.60) |
| 10–14 | 223 (42.1%) | 36 (48.7%) | 187 (41.0%) | 1.25 | (0.58, 2.69) | |
| 15+ | 147 (27.7%) | 14 (18.9%) | 133 (29.2%) | Ref | - | |
| Abn bowel wall | ||||||
| Present | 23 (4.3%) | 11 (14.9%) | 12 (2.6%) | <0.001* | 1.61 | (0.47, 5.47) |
| Absent | 507 (95.7%) | 63 (85.1%) | 12 (2.6%) | Ref | - | |
| Abn adjacent bowel | ||||||
| Present | 8 (1.5%) | 4 (5.4%) | 4 (0.9%) | 0.016* | 1.66 | (0.30, 9.32) |
| Absent | 522 (98.5%) | 70 (94.6%) | 452 (91.1%) | Ref | - | |
| Free fluid | ||||||
| Present | 28 (5.3%) | 15 (20.3%) | 13 (2.9%) | <0.001* | 9.78 | (3.76, 25.44) |
| Absent | 502 (94.7%) | 59 (79.7%) | 443 (97.1%) | Ref | - | |
| Fluid collection | ||||||
| Present | 8 (1.5%) | 6 (8.1%) | 2 (0.4%) | <0.001* | 13.31 | (2.14, 82.76) |
| Absent | 522 (98.5%) | 68 (91.9%) | 454 (99.6%) | Ref | - | |
| Abn lymph nodes | ||||||
| Present | 26 (4.9%) | 6 (8.1%) | 20 (4.4%) | 0.239 | 1.11 | (0.35, 3.63) |
| Absent | 504 (95.1%) | 68 (91.9%) | 436 (95.6%) | Ref | - | |
| Appendicolith | ||||||
| Present | 12 (2.3%) | 9 (12.2%) | 3 (0.7%) | <0.001* | 7.86 | (1.66, 37.15) |
| Absent | 518 (97.7%) | 65 (87.8%) | 453 (99.3%) | Ref | - | |
| Echogenic fat | ||||||
| Present | 10 (1.9%) | 7 (9.5%) | 3 (0.7%) | <0.001* | 4.56 | (0.73, 28.40) |
| Absent | 520 (98.1%) | 67 (90.5%) | 453 (99.3%) | Ref | - | |
| Hyperemia | ||||||
| Present | 9 (1.7%) | 7 (9.5%) | 2 (0.4%) | <0.001* | 11.97 | (1.50, 95.49) |
| Absent | 521 (98.3%) | 67 (90.5%) | 454 (99.6%) | Ref | - | |
| SS Present | ||||||
| 0 | 446 (80.0%) | 38 (51.4%) | 408 (89.5%) | <0.001* | Ref | - |
| 1 | 57 (14.0%) | 17 (23.0%) | 40 (8.8%) | 4.31 | (2.19, 8.47) | |
| 2 | 15 (3.4%) | 10 (13.5%) | 5 (1.1%) | 19.07 | (5.91, 61.55) | |
| 3+ | 12 (2.6%) | 9 (12.2%) | 3 (0.7%) | 39.17 | (9.57, 160.36) | |
Adjusted odds ratio (OR) for “number of secondary signs present” is adjusted for race, sex, and age. All other variables are included in a separate model and are adjusted for other secondary signs present, race, sex, and age.
Abn – abnormal, Ref – reference value, SS – secondary signs
4.3 Test characteristics
In equivocal patients, secondary signs are highly specific for appendicitis, but have poor sensitivity (Table 4). Notably, there was no difference in accuracy between unequivocal US and equivocal US when SS were used. The presence of two SS improved the positive predictive value of appendicitis compared to the presence of a single SS. Very few patients had three or more secondary signs present precluding demonstration of value added by more than two signs. Equivocal US that included hyperemia, a fluid collection, or an appendicolith had a specificity of 96% and accuracy of 88%.
Table 4.
Test characteristics comparing appendix maximal outer diameter in patients with unequivocal ultrasound studies against secondary signs (SS) in patients with equivocal US.
| Test Characteristics | Unequivocal patients (N=295) | Equivocal patients with at least 1 SS (N=530) | Equivocal patients with at least 2 SS (N=530) | Equivocal patients with at least 3 SS (N=530) | Hyperemia, fluid collection, or appendicolith present (N=530) |
|---|---|---|---|---|---|
| Sensitivity | 95.7% | 48.7% | 25.7% | 12.2% | 35.1% |
| Specificity | 65.4% | 89.5% | 98.3% | 99.3% | 96.3% |
| PPV | 83.0% | 42.9% | 70.4% | 75.0% | 60.5% |
| NPV | 90.0% | 89.5% | 89.1% | 87.5% | 89.9% |
| Accuracy | 84.7% | 83.8% | 88.1% | 87.2% | 87.7% |
5.0 Discussion
There is potential to improve the diagnostic accuracy of US for pediatric appendicitis using secondary signs. Our study demonstrates that secondary signs noted on US are associated with appendicitis and improve the overall accuracy of equivocal US studies to that of unequivocal US studies. Our appendix visualization rate of 36% is similar to recently published rates11,12,16,17. With non-visualization of the appendix, an equivocal imaging report creates a diagnostic dilemma. Among children with an equivocal US, the lack of diagnosis results either in delay in diagnosis or overutilization of resources. Improving the accuracy of US is essential to changing the perception that US may be inadequate for diagnosing appendicitis. In the current study, we observed that 7% of patients with unequivocal US reads still underwent CT. This speaks to the persistent skepticism clinicians have with US for appendicitis and illustrates a major barrier to wide-spread adoption of US as the optimal first-line imaging modality. However, since US is not 100% SN and SP, there remains a role for the gestalt of a physician’s clinical reasoning. Of the 78 patients with unequivocal not appendicitis US reads, 6 underwent CT and 2 had appendicitis. Of the 217 patients with unequivocal appendicitis US reads, 15 underwent CT and 8 did not have appendicitis.
In effort to increase the diagnostic accuracy of equivocal US, investigations have proposed combining equivocal studies with additional data such as laboratory values or sonographic secondary signs of appendicitis16,17,23–25. Prior studies have evaluated if the presence or absence of SS in equivocal US studies could differentiate a positive and negative US23,24,26. Wiersma et al. developed a four-level categorization scheme that was adopted by Nielsen et al and that was used the current study23. They defined Categories 1 and 2 as negative US (not appendicitis) and Categories 3 and 4 as positive US (appendicitis) and reported 99% SN and 97% SP23. These extremely high SN and SP may be difficult to practically replicate as ultrasounds were performed by pediatric staff radiologists and not radiological technicians which likely contributed to their appendiceal visualization rate of 75%. Additionally, Wiersma et al. only included patients with less than two days of RLQ pain, guarding on exam, and leukocytosis23. These specific patient criteria are highly suggestive of appendicitis, and our study did not include the patients who had clinical presentations that were so highly suggestive of appendicitis that may not have undergone preoperative imaging.
There is not a consensus on what particular sonographic signs are associated with appendicitis17,23,24. Nielsen’s template included the same eight SS as the current study but did not include hyperemia, free fluid, wall thickness, lymphadenopathy, and appendicoliths in their analysis and did not explain the selective analysis. In fact, Wiersma and Nielsen only analyzed echogenic fat, fluid collections, and abnormal adjacent bowel. In the current study, echogenic fat and abnormal adjacent bowel were not found to be associated with appendicitis on multivariate analysis. Wiersma reported the presence of echogenic fat in 97% (69/71) of patients with appendicitis among equivocal and unequivocal US studies23. We found that after fully adjusting for age, sex, race, and other SS, echogenic fat was not associated with appendicitis (OR 4.56, 95%CI 0.73–28.40). Estey et al. evaluated the association between specific SS and appendicitis, as well as, the number of SS present and appendicitis16. In their analysis, they included periappendiceal free fluid, complex collections, abnormal lymph nodes, phlegmon, and echogenic fat. They reported the SP of moderate-to-large amounts of free fluid as 98%, phlegmon as 100%, echogenic fat as 98%, and any free fluids with abnormal lymph nodes as 81%. They also reported that the odds ratio of appendicitis was only significant for the presence of 3 or more SS. We found that the adjusted odds ratio of appendicitis was significant for the presence of 1, 2, and 3 SS.
Although there are some differences among the few studies that have evaluated SS, there is agreement that US is a reliable diagnostic tool and that SS can guide management of appendicitis for patients with equivocal US studies. Wiersma et al found that the absence of secondary signs in an equivocal US had a NPV of 99% and concluded that appendicitis can be ruled out23. The current study and others report NPV greater than 90%. In the current study, only 3% of patients with equivocal US reads without SS were selected for subsequent CT and had appendicitis, thus benefiting from the additional imaging. We agree that an equivocal US with no SS present has a very low probability of appendicitis and the patient could forgo further diagnostic imaging24,26. There is consensus that patients with an equivocal US and SS present are the most challenging to diagnose. Prior studies estimate the prevalence of this group to be 3% to 45%15,16,24,26. In the current study, such patients represented only 16% of the final cohort. Simply using the presence or absence of SS in equivocal US as a diagnostic test gives an accuracy of 84% similar to the reported accuracy range of 86%-96% in other studies23,24,29. In the current study, patients with an equivocal US that included hyperemia, a fluid collection, or an appendicolith had a specificity of 96% and accuracy of 88%. We propose that patients with an equivocal US and the presence of either hyperemia, a fluid collection, or an appendicolith undergo appendectomy without further imaging whereas patients with an equivocal US and the presence of less specific SS (free fluid, echogenic fat, abnormal lymph nodes, abnormal adjacent bowel, and bowel wall edema) represent the category of patients that would gain the most benefit from selective CT utilization. Our study includes several limitations including the fact that this work is a retrospective analysis of data collected from a single hospital system. Interestingly, our results may be more generalizable than prior reports as our system data includes representation from two physically separate campuses with variation in practice and resources including sonographer coverage, imaging preferences, and level of detail included in radiologic reporting. Furthermore, this study represents one of the largest assessments of secondary signs to date. Though retrospective, we carefully selected a cohort in which there was a high clinical suspicion for appendicitis by thoroughly examining emergency department notes and manually abstracted details from operative and pathology reports. For patients who were deemed not to have appendicitis, we tracked their clinical course to ensure they were not readmitted after discharge and found two patients that were re-admitted and diagnosed with appendicitis. Our study did not include the patients who had clinical presentations that were so highly suggestive of appendicitis that they did not undergo preoperative imaging. Despite this being a retrospective review, we attempted to ensure highly accurate data collection by using two reviewers to abstract the data and used two radiologists to review imaging.
6.0 Conclusions
There is potential to improve the diagnosis of appendicitis. When using SS, equivocal US are as accurate as unequivocal US. Among patients with an unequivocal US, the accuracy was 84.7%, but among patients with an equivocal US our accuracy was as high as 88.1% using the presence of SS in the diagnosis of appendicitis. Appropriate use of SS can guide clinicians and may reduce unnecessary CTs and admissions. We are using the knowledge gained from this and other studies to improve the US reporting at our institution. We plan to validate our findings by evaluating the implementation of a standardized template that includes the reporting of secondary signs.
Acknowledgments
This research is supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR000454. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. In addition, MVR is supported by the Emory+Children’s Pediatric Research Trust, Children’s Healthcare of Atlanta, and the Department of Surgery at Emory University.
Abbreviations
- CT
computed tomography
- NPV
negative predictive value
- PPV
positive predictive value
- RLQ
right lower quadrant
- SN
sensitivity
- SP
specificity
- SS
secondary signs
- US
ultrasound
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Rosendahl K, Aukland SM, Fosse K. Imaging strategies in children with suspected appendicitis. Eur Radiol. 2004;14(Suppl 4):L138–145. doi: 10.1007/s00330-003-2077-3. [DOI] [PubMed] [Google Scholar]
- 2.Smith MP, Katz DS, Lalani T, et al. ACR Appropriateness Criteria(R) Right Lower Quadrant Pain-Suspected Appendicitis. Ultrasound Q. 2015;31(2):85–91. doi: 10.1097/RUQ.0000000000000118. [DOI] [PubMed] [Google Scholar]
- 3.Pediatrics AAo. Choosing wisely. [Accesssed May 27, 2015];Ten Things Physicians and Patients Should Question. 2013 http://www.choosingwisely.org/doctor-patient-lists/american-academy-ofpediatrics/
- 4.Rice-Townsend S, Barnes JN, Hall M, Baxter JL, Rangel SJ. Variation in practice and resource utilization associated with the diagnosis and management of appendicitis at freestanding children's hospitals: implications for value-based comparative analysis. Ann Surg. 2014;259(6):1228–1234. doi: 10.1097/SLA.0000000000000246. [DOI] [PubMed] [Google Scholar]
- 5.Raval MV. Factors associated with imaging modality choice in children with appendicitis. The Journal of surgical research. 2012;177(1):131–136. doi: 10.1016/j.jss.2012.03.044. [DOI] [PubMed] [Google Scholar]
- 6.Kotagal M, Richards MK, Chapman T, et al. Improving ultrasound quality to reduce computed tomography use in pediatric appendicitis: the Safe and Sound campaign. Am J Surg. 2015 doi: 10.1016/j.amjsurg.2014.12.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tian Y, Heiss KF, Wulkan ML, Raval MV. Assessment of variation in care and outcomes for pediatric appendicitis at children's and non-children's hospitals. J Pediatr Surg. 2015;50(11):1885–1892. doi: 10.1016/j.jpedsurg.2015.06.012. [DOI] [PubMed] [Google Scholar]
- 8.Scheinfeld MH. Do clinical outcomes suffer during transition to an ultrasound-first paradigm for the evaluation of acute appendicitis in children? AJR, American journal of roentgenology. 2013:1348–1352. doi: 10.2214/AJR.13.10678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pershad J, Waters TM, Langham MR, Jr, Li T, Huang EY. Cost-effectiveness of diagnostic approaches to suspected appendicitis in children. J Am Coll Surg. 2015;220(4):738–746. doi: 10.1016/j.jamcollsurg.2014.12.019. [DOI] [PubMed] [Google Scholar]
- 10.Dilley A, Wesson D, Munden M, et al. The impact of ultrasound examinations on the management of children with suspected appendicitis: a 3-year analysis. J Pediatr Surg. 2001;36(2):303–308. doi: 10.1053/jpsu.2001.20702. [DOI] [PubMed] [Google Scholar]
- 11.Hahn HB, Hoepner FU, Kalle T, et al. Sonography of acute appendicitis in children: 7 years experience. Pediatr Radiol. 1998;28(3):147–151. doi: 10.1007/s002470050316. [DOI] [PubMed] [Google Scholar]
- 12.Hahn H, Macdonald E, Steinborn M. Sonographic detection of normal appendix in children andadolescents. Ultraschall in der Medizin (Stuttgart, Germany : 1980) 2008;29(3):281–285. doi: 10.1055/s-2008-1027322. [DOI] [PubMed] [Google Scholar]
- 13.Peletti AB, Baldisserotto M. Optimizing US examination to detect the normal and abnormal appendix in children. Pediatr Radiol. 2006;36(11):1171–1176. doi: 10.1007/s00247-006-0305-0. [DOI] [PubMed] [Google Scholar]
- 14.Kessler N, Cyteval C, Gallix B, et al. Appendicitis: evaluation of sensitivity, specificity, and predictive values of US, Doppler US, and laboratory findings. Radiology. 2004;230(2):472–478. doi: 10.1148/radiol.2302021520. [DOI] [PubMed] [Google Scholar]
- 15.Wiersma F, Sramek A, Holscher HC. US features of the normal appendix and surrounding area in children. Radiology. 2005;235(3):1018–1022. doi: 10.1148/radiol.2353040086. [DOI] [PubMed] [Google Scholar]
- 16.Estey A, Poonai N, Lim R. Appendix not seen: the predictive value of secondary inflammatory sonographic signs. Pediatr Emerg Care. 2013;29(4):435–439. doi: 10.1097/PEC.0b013e318289e8d5. [DOI] [PubMed] [Google Scholar]
- 17.Cohen B, Bowling J, Midulla P, et al. The non-diagnostic ultrasound in appendicitis: is a non visualized appendix the same as a negative study? J Pediatr Surg. 2015 doi: 10.1016/j.jpedsurg.2015.03.012. [DOI] [PubMed] [Google Scholar]
- 18.Kaiser S, Frenckner B, Jorulf HK. Suspected appendicitis in children: US and CT--a prospective randomized study. Radiology. 2002;223(3):633–638. doi: 10.1148/radiol.2233011076. [DOI] [PubMed] [Google Scholar]
- 19.Hernandez JAA. Imaging of acute appendicitis: US as the primary imaging modality. Pediatric radiology. 35(4):392–395. doi: 10.1007/s00247-004-1372-8. [DOI] [PubMed] [Google Scholar]
- 20.Miglioretti DL, Johnson E, Williams A, et al. The use of 46 computed tomography in pediatrics and the associated radiation exposure and estimated cancer risk. JAMA Pediatr. 2013;167(8):700–707. doi: 10.1001/jamapediatrics.2013.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Parker L, Nazarian LN, Gingold EL, Palit CD, Hoey CL, Frangos AJ. Cost and radiation savings of partial substitution of ultrasound for CT in appendicitis evaluation: a national projection. AJR Am J Roentgenol. 2014;202(1):124–135. doi: 10.2214/AJR.12.9642. [DOI] [PubMed] [Google Scholar]
- 22.Brenner D, Elliston C, Hall E, Berdon W. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol. 2001;176(2):289–296. doi: 10.2214/ajr.176.2.1760289. [DOI] [PubMed] [Google Scholar]
- 23.Wiersma F, Toorenvliet BR, Bloem JL, Allema JH, Holscher HC. US examination of the appendix in children with suspected appendicitis: the additional value of secondary signs. Eur Radiol. 2009;19(2):455–461. doi: 10.1007/s00330-008-1176-6. [DOI] [PubMed] [Google Scholar]
- 24.Nielsen JW, Boomer L, Kurtovic K, et al. Reducing computed tomography scans for appendicitis by introduction of a standardized and validated ultrasonography report template. J Pediatr Surg. 2015;50(1):144–148. doi: 10.1016/j.jpedsurg.2014.10.033. [DOI] [PubMed] [Google Scholar]
- 25.Anandalwar SP, Callahan MJ, Bachur RG, et al. Use of White Blood Cell Count and Polymorphonuclear Leukocyte Differential to Improve the Predictive Value of Ultrasound for Suspected Appendicitis in Children. J Am Coll Surg. 2015;220(6):1010–1017. doi: 10.1016/j.jamcollsurg.2015.01.039. [DOI] [PubMed] [Google Scholar]
- 26.Jaremko JL, Crockett A, Rucker D, Magnus KG. Incidence and significance of inconclusive results in ultrasound for appendicitis in children and teenagers. Can Assoc Radiol J. 2011;62(3):197–202. doi: 10.1016/j.carj.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 27.Baldisserotto M, Marchiori E. Accuracy of noncompressive sonography of children with appendicitis according to the potential positions of the appendix. AJR Am J Roentgenol. 2000;175(5):1387–1392. doi: 10.2214/ajr.175.5.1751387. [DOI] [PubMed] [Google Scholar]
- 28.Daly CP, Cohan RH, Francis IR, Caoili EM, Ellis JH, Nan B. Incidence of acute appendicitis in patients with equivocal CT findings. AJR Am J Roentgenol. 2005;184(6):1813–1820. doi: 10.2214/ajr.184.6.01841813. [DOI] [PubMed] [Google Scholar]
- 29.Gracey D, McClure MJ. The impact of ultrasound in suspected acute appendicitis. Clin Radiol. 2007;62(6):573–578. doi: 10.1016/j.crad.2006.12.008. [DOI] [PubMed] [Google Scholar]