Abstract
In Brief This study investigates carbohydrate counting accuracy in patients using insulin through a multiple daily injection regimen or continuous subcutaneous insulin infusion. The average accuracy test score for all patients was 59%. The carbohydrate test in this study can be used to emphasize the importance of carbohydrate counting to patients and to provide ongoing education.
Carbohydrate counting has been used in diabetes care since the 1920s. The Diabetes Control and Complications Trial (1) used carbohydrate counting as one approach to meal planning that resulted in improved glycemic control and flexibility with food choices. The American Diabetes Association’s nutrition recommendations advocate the use of carbohydrate counting or experienced-based estimation of carbohydrate intake to improve glycemic control (2). One study (3) found a reduction in A1C and improved quality of life for adult patients trained to count carbohydrates compared to patients estimating premeal insulin doses. These patients were all diagnosed with type 1 diabetes, were naive to carbohydrate counting, and received insulin through continuous subcutaneous insulin infusion (CSII). Koontz et al. (4) developed the PedCarbQuiz to assess carbohydrate counting and calculate insulin doses in youth with type 1 diabetes. This study demonstrated that higher scores on the quiz correlated with lower A1C levels. A more recent meta-analysis (5) found that 24 of the 27 studies included demonstrated a decrease in A1C (0.2–1.2%) after starting carbohydrate counting. However, the statistical significance of the A1C reduction was not available for all of the studies. The studies in this meta-analysis included children, adolescents, and adults with type 1 diabetes, but more patients were using a multiple daily injection (MDI) regimen than were using CSII. The authors concluded that, although there is not sufficient evidence to support advanced carbohydrate counting for A1C reduction, it is preferred over other methods of dosing insulin.
During a typical follow-up appointment for diabetes, the majority of the time is spent correcting high and low blood glucose patterns, leaving little time for discussion of carbohydrate counting. Advanced carbohydrate counting requires patients to count carbohydrates to determine proper dosing for bolus insulin. Inaccurate carbohydrate counting can lead to elevated postprandial glucose levels or hypoglycemia. Postprandial hyperglycemia can contribute to poor glycemic control (A1C >7%) (6). On the other hand, episodes of hypoglycemia may force patients to consume unwanted calories.
What are patients really doing when it comes to carbohydrate counting? Numerous studies have looked at the accuracy of carbohydrate counting in children and adolescents, but little information exists regarding the accuracy of carbohydrate counting in adults using an MDI regimen or CSII. The carbohydrate test study was designed to investigate four questions: 1) how accurately do patients count carbohydrates, 2) does increased accuracy correlate with a lower A1C, 3) did A1C improve after education, and 4) what changes are patients willing to make?
Methods
Sample and Setting
The sample consisted of 61 patients receiving care at an endocrinology office in the southeastern region of the United States. The office staff includes two endocrinologists, one nurse practitioner (NP), and two certified diabetes educators (CDEs). Patients with type 1 or type 2 diabetes were eligible for the test if they were dosing insulin based on carbohydrates and using an MDI regimen or CSII. Table 1 describes the baseline characteristics for study participants. The sample included 32 women and 29 men ranging in age from 22 to 84 years (mean 53 years). Most (75%) had type 1 diabetes. One patient used an MDI regimen, whereas the rest used CSII. Sixty-seven percent of the sample had some college education, and 33% had completed high school or had less education. This study was approved by the research review board of Wingate University.
TABLE 1.
Characteristics of Study Participants
| Participants (n) | 61 |
| Age (years)* | 53 ± 15.3 |
| Type 1 diabetes (n [%]) | 46 (75) |
| Type 2 diabetes (n [%]) | 15 (25) |
| Insulin regimen (n) | |
| CSII | 60 |
| MDI | 1 |
| Sex (n [%]) | |
| Male | 29 (48) |
| Female | 32 (52) |
| Diabetes duration (years)* | 26 ± 13.3 |
| Baseline A1C (%)* | 7.4 ± 0.9 |
| Education (n [%]) | |
| High school or less | 17 (33) |
| Some college | 35 (67) |
Data are mean ± SD.
Instrumentation
The carbohydrate test was designed to assess how frequently a patient eats a particular food and how many carbohydrates are in each serving size. The test contained 18 different foods with a corresponding food model for each item, including fruits, vegetables, starches, snacks, combination foods, and drinks. The carbohydrate test is summarized in Table 2.
TABLE 2.
Carbohydrate Test
| Circle how frequently you eat these foods: N = never S = sometimes O = often | How many grams of carbohydrate are in this serving size of this food? | Office use only | |
| Fruit | |||
| Red delicious apple | N S O | ||
| Banana | N S O | ||
| Vegetables | |||
| Kidney beans | N S O | ||
| Baked beans | N S O | ||
| Kernel corn | N S O | ||
| Green peas | N S O | ||
| Baked potato | N S O | ||
| Starch | |||
| White rice | N S O | ||
| Spaghetti noodles | N S O | ||
| Cornflakes | N S O | ||
| Snacks | |||
| Popcorn | N S O | ||
| Combinations | |||
| Lasagna | N S O | ||
| Spaghetti and meatballs | N S O | ||
| Chili with beef/beans | N S O | ||
| Drinks | |||
| Skim milk | N S O | ||
| Chocolate milk | N S O | ||
| Orange juice | N S O | ||
Food models were purchased from Nasco Nutrition (Fort Atkinson, WI) and varied with regard to serving size. For example, instead of the standard 1/2-cup serving for peas or corn, the food model used for the test was a 1/4-cup size. Table 3 contains a list of serving sizes for the food items included on the test. Nasco Nutrition includes the serving size and carbohydrate content for each food model; however, this information was also reviewed by a registered dietitian. Patients’ age, sex, duration of diabetes, level of education, and insulin regimen were collected at the time of the test. The A1C recorded at baseline was an average of the previous two values, which accounted for other factors that could influence A1C, such as illness, steroid use, and stress. Post-intervention A1C levels were measured 3 months after the initial visit.
TABLE 3.
Food Model and Serving Sizes Used on the Carbohydrate Test and Number of Patients Reporting Eating the Items Never or Sometimes/Often
| Food Item | Serving Size of Food Model | Never (n) | Sometimes or Often (n) | P* |
| Apple | 6 oz | 11 | 50 | 0.265 |
| Banana | 1 banana | 9 | 52 | 0.578 |
| Kidney beans | 1/2 cup | 31 | 30 | 0.133 |
| Baked beans | 2/3 cup | 12 | 49 | 0.559 |
| Kernel corn | 1/4 cup | 10 | 51 | 0.753 |
| Green peas | 1/4 cup | 21 | 40 | 0.544 |
| Baked potato | 1 potato | 3 | 58 | 0.293 |
| White rice | 1/2 cup | 18 | 43 | 0.773 |
| Spaghetti noodles | 1 cup | 10 | 51 | 0.586 |
| Cornflakes | 3/4 cup | 31 | 30 | 0.133 |
| Popcorn | 1/2 cup | 13 | 48 | 0.699 |
| Lasagna | 1 slice (3” x 4”) | 16 | 45 | 0.384 |
| Thin-crust cheese pizza | 1 slice | 13 | 48 | 0.858 |
| Spaghetti and meatballs | 1 cup | 16 | 45 | 0.750 |
| Chili with beef/beans | 1 cup | 18 | 43 | 0.907 |
| Skim milk | 1 cup | 24 | 37 | 0.207 |
| Chocolate milk | 1 cup | 48 | 13 | 0.391 |
| Orange juice | 3/4 cup | 22 | 39 | 0.616 |
By t test.
Implementation
Unlike the assessment used by Koontz et al. (4), the 1-page carbohydrate test was designed to allow completion during a regular follow-up appointment. All patients using carbohydrate counting with CSII or MDI and followed by the NP between January and November 2013 were scheduled for a joint visit (with the CDE and NP). Patients completed the carbohydrate test at the beginning of the visit. The CDE was responsible for setting up the food models, administering the tests, grading them, and then reviewing results with patients. Correct answers for the carbohydrate test were based on the total amount of carbohydrates contained in each item and included a range or a single value. If the serving size of food included a range as the total amount of carbohydrate, correct answers included those within 3 g of the upper and lower range limit (e.g., if a 6 oz. red delicious apple serving size contains 20–25 g of carbohydrate, an answer was correct if the patient chose a number from 17 to 28 g). For foods with a single value as the total amount of carbohydrate, correct answers were given to those within 5 g of the single value (e.g., if 1 cup of spaghetti contains 45 g of carbohydrate, an answer was correct if the patient chose a number from 40 to 50 g).
The education intervention included a review of the food label and correct carbohydrate amounts for any items missed on the test. The majority of the time was spent reviewing incorrect items that patients indicated they ate “often” or “sometimes.” Upon completion of the review, every patient received a resource packet containing a food label handout, carbohydrate recommendations for each meal, a list of mobile device applications that provide nutritional information, and the CalorieKing book (a nutritional guide that includes calories, fat, and carbohydrate content). At the end of the visit, patients were asked if they were willing to change their current practice, and a dietitian referral was offered to all patients.
Statistical Analysis
A paired t test was employed to investigate the effect of the diabetes education intervention on A1C. Analysis of variance was used to examine the association between test scores and A1C levels. A t test was used to look at the potential relationship between level of education and carbohydrate test scores. A t test was also employed to analyze the effect of eating frequency and the ability of patients who reported “never” eating a given food to correctly answer a question about its carbohydrate content. Pearson correlation and analysis of variance were used to investigate the possible effect of diabetes duration on carbohydrate test scores. All P values were two-tailed, with statistical significance set at <0.05. Descriptive statistics were also used as appropriate. All analyses were performed using SYSTAT 13 (Systat Software, Inc., San Jose, CA).
Results
The average score for all patients was 44%. Of the 61 patients tested, 7 scored ≥66% on the carbohydrate test. Omitting the “never” answers increased the average score to 59%, with 19 patients scoring ≥72%.
Mean A1C at baseline was 7.4 ±0.9% (range 4.9–10%), and 49% of patients had a pre-intervention A1C between 7.1 and 8%. Pre- and post-intervention A1C values were analyzed for improvement after education, and there was no change (7.444 vs. 7.457, respectively). Patients were grouped into quartiles based on their carbohydrate test scores, as follows: Q1, lowest test scores; Q2–3, mid-range scores; and Q4, highest scores (Figure 1). Higher test scores appeared to be related to lower post-intervention A1C results, although statistical significance was not reached (P = 0.095).
FIGURE 1.
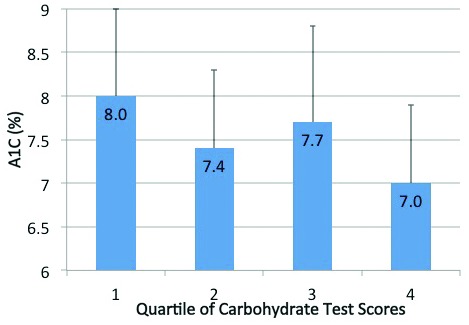
A1C (mean ± SD) by quartiles (Q) of carbohydrate test scores. The A1C of patients with the highest test scores (Q4) was lower than the A1C of patients with lower test scores (Q1), but did not reach statistical significance.
The highest score was 94% from a patient living with diabetes for 25 years who had an average A1C of 6.1%. Three other patients who scored 83% had diabetes for an average of 16 years and an average A1C of 7.1%. Overall, however, patients with a longer duration of diabetes did not score better than patients with a shorter duration of diabetes (P = 0.425). The level of education for participants was combined into two groups: any college or high school or less. The patients with a higher education level (67%) did not score better on the test than those with less education (P = 0.804).
Table 3 includes the number of patients reporting “never,” “sometimes,” or “often” eating food items. Only chocolate milk was reported more often to be “never” consumed. All of the other food items were reported consumed “sometimes” or “often” by at least half of the participants. This indicates that the carbohydrate test did reflect common food choices for the patient population. Patients who reported eating foods “sometimes” or “often” were not more likely to count carbohydrates accurately than those who reported “never” eating the item (P values shown in Table 3). Most patients (82%) overestimated the carbohydrate content for items on the test, and when they overestimated, it was by an average of 40%. Two patients overestimated every item on the test. When patients underestimated carbohydrate content, it was by an average of 12%.
At the end of the appointment, patients were asked two questions: 1) are you willing to change your current practice of carbohydrate counting? and 2) would you like more education (referral to a dietitian or CDE in the office)? Interestingly, 36% of patients were not willing to change their current practice because they reported using food labels or an electronic or printed resource for carbohydrate amounts. Among those who were willing to change (41%), three behaviors were documented for modification: paying closer attention to food labels, using a printed or online resource, and watching serving sizes. Only two patients accepted the referral to the dietitian.
Discussion
The providers and educators were surprised by and disappointed in the degree of carbohydrate counting accuracy among patients. Earlier studies demonstrated that carbohydrate counting inaccuracies are common in younger patients with type 1 diabetes (4,7–9). The results of the present study are consistent with Shapira et al. (10), who found inaccuracies in the estimation of carbohydrate for adult patients with type 1 diabetes using CSII. One previous study (4) documented that college-educated parents of children with type 1 diabetes scored higher than parents without a college degree for carbohydrate counting accuracy. Another study (8) demonstrated a lower A1C in youth with diabetes when college-educated parents estimated carbohydrate for meals. However, in the present study, having some college education did not correlate with an increase in carbohydrate counting accuracy.
The duration of diabetes for participants ranged from 2 to 63 years, with a mean of 26 years. No association was found between diabetes duration and carbohydrate counting accuracy, which is consistent with a study in adolescents that documented the same results (8). However, some patients who scored low on accuracy reported reading food labels or using an online or printed resource to obtain carbohydrate information, and these resources were not available for use on the test.
The education provided to each patient was a review of items missed on the test and resources to assist in improving the accuracy of carbohydrate counting. The importance of education for A1C reduction with carbohydrate counting has been documented in numerous studies and a meta-analysis. Bell et al. (11) identified five out of seven studies that showed a 0.64% reduction in A1C with carbohydrate counting in adults with type 1 diabetes. The carbohydrate counting included the use of grams, exchanges, portions, and fixed amounts of carbohydrate or exchanges per meal to calculate a bolus. All of the studies in the review also included some type of education. The amount of education varied from as little as one session with a dietitian to a 5-day course run by diabetes educators. Clearly, more intense education may be required, as reported in a study comparing carbohydrate counting to estimation in adult patients using CSII (3). In that study, the intervention group received four to five education sessions with a dietitian that focused on carbohydrate counting and using an insulin-to-carbohydrate ratio with a sensitivity factor. The control group did not use carbohydrates to estimate premeal insulin doses. After 24 weeks, the carbohydrate-counting group had lower A1C levels and better quality-of-life scores. Another study (8) looked at the effectiveness of a 90-minute education class and review of food records, which resulted in a reduction in A1C that was not statistically significant. In the current study, there was no change in A1C after education, but patients with higher scores on the carbohydrate test had lower A1C levels after the education intervention. Patients reported increased awareness of the importance of accurately counting carbohydrates. Providers found it helpful to know the tendency of patients to over- or underestimate carbohydrate content. Future education should focus on encouraging patients to continually check and evaluate serving sizes.
Our study has several strengths. First, the carbohydrate test and education were provided during a regular office visit and can be incorporated into the workflow of any clinic. Second, the use of nonstandard-sized food models reflected what patients encounter daily while trying to determine serving sizes. Many variables such as illness, stress, and medications can affect A1C; this was taken into account at baseline by using an average of patients’ past two A1C values. Finally, more focused education can be provided to patients who indicate that they are willing to change or improve their current practices with carbohydrate counting (in this study, 41% of participants). Modification of their current habits can be discussed at future visits.
One limitation of this study is the use of pre-selected foods, which did not always reflect patients’ everyday choices. Interestingly, nine of the foods included on the carbohydrate test were also used in one of the first carbohydrate assessment tools, but this was not intentional (7). A more comprehensive list would lengthen the test and make it impractical for use during an office visit because of time constraints. Second, patients were not able to use food labels or other resources during the test. This could be viewed as a strength in that it reflects a more real-world situation, but also as a weakness because so many resources are available to patients through the Internet, mobile devices, and printed materials. Before using the carbohydrate test at our clinic, the percentage of patients using online and printed resources was unknown. One study reported that the use of a food label did not increase accuracy (8). Thus, it is unclear whether the use of printed or online resources would have improved the accuracy of carbohydrate counting. Future research may incorporate the use of printed and online resources. Finally, we did not ask about previous carbohydrate- counting education, but patients are required to attend a carbohydrate- counting class before starting CSII at this office. Since the majority of the patients were insulin pump users, they most likely had previous education.
Carbohydrate counting is the preferred method of dosing mealtime insulin in patients with diabetes. Unfortunately, complex and challenging self-management requirements take precedence and often leave little time to focus on counting carbohydrates. Patients then begin over- and underestimating carbohydrate amounts, which is likely to result in hypo- or hyperglycemia.
The results of this study suggest that testing a patient’s ability to accurately count carbohydrates is beneficial because it can reveal patient behaviors that otherwise may go undocumented. For example, eating a banana every morning for breakfast without entering the carbohydrates was determined to be the cause of one patient’s elevated post-breakfast and pre-lunch blood glucose readings. Additionally, one patient who overestimated the carbohydrate content of all items on the test required a lower insulin-to-carbohydrate ratio to receive more insulin when carbohydrates were entered accurately. Consistent over- or underestimation of carbohydrates may not adversely affect overall glycemic control. However, it can be the cause of hypo- or hyperglycemia and therefore needs to be corrected during an office visit. Information from the carbohydrate test can help providers, dietitians, educators, and patients to make better decisions about carbohydrate ratios. Finally, the test emphasizes to patients the importance of carbohydrate counting in the management of diabetes.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
References
- 1.Delahanty LM, Halford BN. The role of diet behaviors in achieving improved glycemic control in intensively treated patients in the Diabetes Control and Complications Trial. Diabetes Care 1993;16:1453–1458 [DOI] [PubMed] [Google Scholar]
- 2.Evert AB, Boucher JL, Cypress M, et al. Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care 2013;36:3821–3842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Laurenzi A, Bolla AM, Panigoni G, et al. Effects of carbohydrate counting on glucose control and quality of life over 24 weeks in adult patients with type 1 diabetes on continuous subcutaneous insulin infusion. Diabetes Care 2011;34:823–827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koontz MB, Cuttler L, Palmert MR, et al. Development and validation of a questionnaire to assess carbohydrate and insulin dosing knowledge in youth with type 1 diabetes. Diabetes Care 2010;33:457–462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schmidt S, Schelde B, Norgaard K. Effects of advanced carbohydrate counting in patients with type 2 diabetes: a systematic review. Diabet Med 2014;31:886–896 [DOI] [PubMed] [Google Scholar]
- 6.American Diabetes Association : Glycemic targets. Sec. 5 in Standards of Medical Care in Diabetes—2016. Diabetes Care 2016;39(Suppl. 1):S39–S46 [DOI] [PubMed] [Google Scholar]
- 7.Bishop FK, Maahs DM, Spiegel G, et al. The Carbohydrate Counting in Adolescents with Type 1 Diabetes (CCAT) study. Diabetes Spectrun 2009;22:56–62 [Google Scholar]
- 8.Spiegel G, Bortsov A, Bishop FK, et al. Randomized nutrition education intervention to improve carbohydrate counting in adolescents with type 1 diabetes study: is more intensive education needed? J Acad Nutr Diet 2012;112:1736–1746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mehta SN, Quinn N, Volkening LK, Laffel LM. Impact of carbohydrate counting on glycemic control in children with type 1 diabetes. Diabetes Care 2009;32:1014–1016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shapira G, Yodfat O, HaCohen A, Feigin P, Rubin R. Bolus guide: a novel insulin bolus dosing decision support tool based on selection of carbohydrate ranges. J Diabetes Sci Technol 2010;4:893–902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bell KJ, Barclay AW, Petocz P, Colagiuri S, Brand-Miller JC. Efficacy of carbohydrate counting in type 1 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol 2014;2:133–140 [DOI] [PubMed] [Google Scholar]


