Abstract
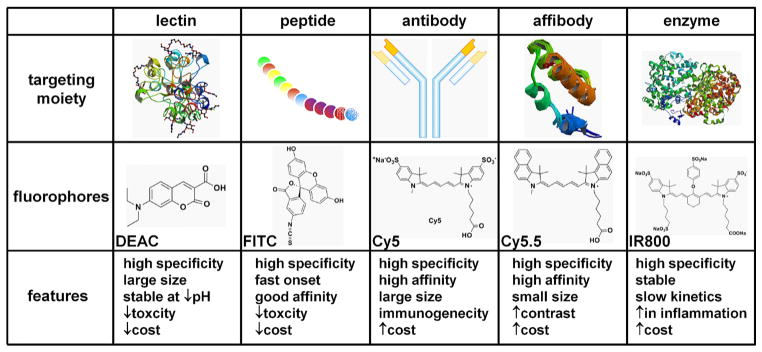
The rapid rise in incidence of oesophageal adenocarcinoma has motivated the need for improved methods for surveillance of Barrett’s oesophagus. Early neoplasia is flat in morphology and patchy in distribution and is difficult to detect with conventional white light endoscopy (WLE). Light offers numerous advantages for rapidly visualising the oesophagus, and advanced optical methods are being developed for wide-field and cross-sectional imaging to guide tissue biopsy and stage early neoplasia, respectively. We review key features of these promising methods and address their potential to improve detection of Barrett’s neoplasia. The clinical performance of key advanced imaging technologies is reviewed, including (1) wide-field methods, such as high-definition WLE, chromoendoscopy, narrow-band imaging, autofluorescence and trimodal imaging and (2) cross-sectional techniques, such as optical coherence tomography, optical frequency domain imaging and confocal laser endomicroscopy. Some of these instruments are being adapted for molecular imaging to detect specific biological targets that are overexpressed in Barrett’s neoplasia. Gene expression profiles are being used to identify early targets that appear before morphological changes can be visualised with white light. These targets are detected in vivo using exogenous probes, such as lectins, peptides, antibodies, affibodies and activatable enzymes that are labelled with fluorescence dyes to produce high contrast images. This emerging approach has potential to provide a ‘red flag’ to identify regions of premalignant mucosa, outline disease margins and guide therapy based on the underlying molecular mechanisms of cancer progression.
BARRETT’S OESOPHAGUS
Each year, >450 000 new cases of oesophageal cancer (EAC) are diagnosed worldwide, and >400 000 people die from this disease.1 Over the past three decades, the incidence of EAC has risen faster than any other cancer in developed countries.2,3 EAC has a poor prognosis, thus early detection is critical to relieve the burden of this cancer on society. Neoplasia is believed to arise from Barrett’s oesophagus (BE), a premalignant condition that is becoming more common as a result of a rapid rise in obesity and acid reflux.4–6 BE transforms into low-grade dysplasia (LGD) and progresses sequentially to high-grade dysplasia (HGD) and EAC.7 While dysplasia is a risk factor for cancer, its natural history is highly variable.8 In individual patients, the annual rate of BE transforming into EAC is estimated at between 0.07% and 0.82%.8–11 A diagnosis of HGD confers increased risk for progression to EAC of 12%–40%.12,13 LGD has an annual incidence of 0.54%–6.5% to progress to either HGD or EAC.14–16
Key messages.
Novel imaging technologies are needed to improve methods for early detection of oesophageal adenocarcinoma.
Light has a broad spectrum that can be developed to rapidly visualise oesophageal mucosa with improved resolution, contrast and depth.
Novel optical instruments for wide-field and cross-sectional imaging have been assessed in the clinic for improved detection of Barrett’s neoplasia.
Lectins, peptides, antibodies, affibodies and activatable enzymes are being developed as exogenous probes for detecting molecular targets overexpressed in Barrett’s neoplasia.
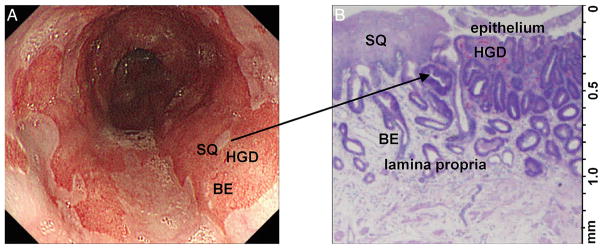
figure 1 shows that dysplasia can be flat in architecture and focal or patchy in distribution, thus difficult to detect on endoscopy. In the Seattle protocol, white light endoscopy (WLE) is performed with biopsies collected from visible mucosal abnormalities and at random in four-quadrants from every 1–2 cm in the BE segment using jumbo forceps. This method of surveillance has been validated and is recommended for BE patients every 2–5 years.17–19 Table 1 summarises the results of clinical studies performed using the Seattle protocol to detect Barrett’s neoplasia. However, this technique is labour-intensive, time-consuming and prone to sampling error and is not practiced widely by community physicians.20–22
Figure 1.
Imaging of Barrett’s oesophagus (BE). (A) Wide-field imaging is needed to localise neoplastic lesions, identify tumour margins and evaluate for cancer recurrence. White light image shows patches of squamous (SQ) in BE. An area of high-grade dysplasia (HGD) is not visibly distinct. (B) Cross-sectional imaging is needed to assess depth of early cancer invasion (T1a vs T1b). Histology (H&E) shows feature of both SQ and HGD.
Table 1.
Clinical performance for novel optical imaging technologies
| Imaging technology | Studies | Sensitivity | Specificity | Type of lesion | Level of evidence | References |
|---|---|---|---|---|---|---|
| High definition white light endoscopy (HD-WLE) | RCT | 40%–64% | 98%–100% | LGD/HGD/EAC | Ib | 33,59 |
| Chromoendoscopy | ||||||
| Methylene blue | RCT | 49%–51% | 48%–85% | LGD/HGD/EAC | Ib | 25,26 |
| Acetic acid | P | 96% | 81% | IIa | 28 | |
| Narrow band imaging (NBI) | RCT, P, MA | 47%–100% | 72%–100% | LGD/HGD/EAC | Ib | 31–34 |
| Autofluorescence imaging (AFI) | P, RCT | 42%–50% | 61%–92% | HGD/EAC | Ib | 36,38 |
| Endoscopic trimodal imaging (ETMI) | RCT | NA | NA | LGD/HGD/EAC | Ib | 40,41 |
| Optical coherence tomography (OCT) | P | 68%–83% | 75%–82% | LGD/HGD/EAC | IIa | 44,45 |
| Optical frequency domain imaging (OFDI) | P | NA | NA | LGD/HGD/EAC | IIa | 46,47 |
| Confocal laser endoscopy (CLE) | RCT, P, MA | 63%–100% | 70%–98% | LGD/HGD/EAC | Ib | 51,56–59 |
| Molecular imaging | P | 75% | 94% | HGD/EAC | IIa | 74 |
Performance and level of evidence for clinical studies performed using novel optical imaging technologies for BE surveillance.
Levels of evidence: Ib, evidence including at least one RCT; IIa, evidence including prospective, controlled, non-randomised studies.
BE, Barrett’s oesophagus; EAC, oesophageal cancer; HGD, high-grade dysplasia; LGD, low-grade dysplasia; MA, meta-analysis; NA, not available; P, prospective study; RCT, randomised control trial.
MOTIVATION FOR OPTICAL IMAGING METHODS
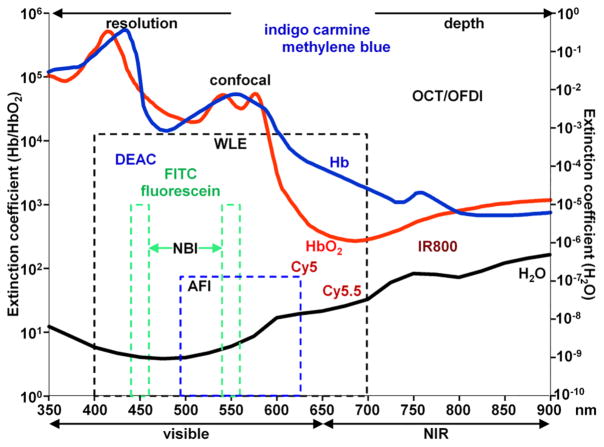
Improved imaging methods are needed to improve our ability to rapidly detect and assess Barrett’s neoplasia. Because light can rapidly interrogate tissue with high resolution over a broad range of wavelengths, a number of optical methods are being developed and fall into two main categories: (1) wide-field and (2) cross-sectional. Wide-field imaging techniques visualise large mucosal surface areas to localise suspicious regions for guiding tissue biopsy. Cross-sectional technologies image with subcellular resolution below the mucosal surface to assess depth of disease penetration.23 figure 2 shows important tradeoffs in the properties of light that are used to design instruments for either wide-field or cross-sectional imaging. Image resolution improves with reduced tissue depth at shorter wavelengths, and image penetration improves with reduced resolution at longer wavelengths. Haemoglobin (Hb) is a dominant absorber of light in the visible region (400–650 nm), while water absorption plays a small role in the infrared spectrum (>900 nm). The extinction coefficients for oxyhaemoglobin (HbO2), deoxyhaemoglobin (Hb) and water (H2O) vary over the visible and near infared (NIR) spectrum. Because fluorescence provides images with high contrast, bright dyes are being developed to label molecular probes that are specific for targets overexpressed in Barrett’s neoplasia to enhance visualisation of diseased areas and guide tissue biopsy. This emerging approach detects specific molecular changes that may have a direct effect on cancer progression. Figure 2 shows the spectral location of some contrast agents used in optical imaging. Imaging instruments that are sensitive to these fluorophores are being developed for both wide-field and cross-sectional imaging. Here, we discuss basic concepts and review emerging optical technologies for improved detection of Barrett’s neoplasia.
Figure 2.
Optical properties of tissue. Image resolution improves with shorter wavelengths, and tissue penetration increases with longer wavelengths. Haemoglobin (Hb) dominates absorption of light in the visible (400–700 nm). Water absorption plays a small role in the infrared (IR; >900 nm). The extinction coefficients for Hb (blue), oxyhaemoglobin (HbO2; red) and water (black) are shown. Fluorophores can be used to improve image contrast, and include Diethylaminocoumarin (DEAC), fluorescein, fluorescein isothiocyanate (FITC; derivative of fluorescein), Cyanine (CY) derivatives (Cy5, Cy5.5), and IR800. AFI, autofluorescence imaging; NBI, narrow band imaging; OCT, optical coherence tomography; OFDI, optical frequency domain imaging; WLE, white light endoscopy.
ADVANCES IN WIDE-FIELD ENDOSCOPY
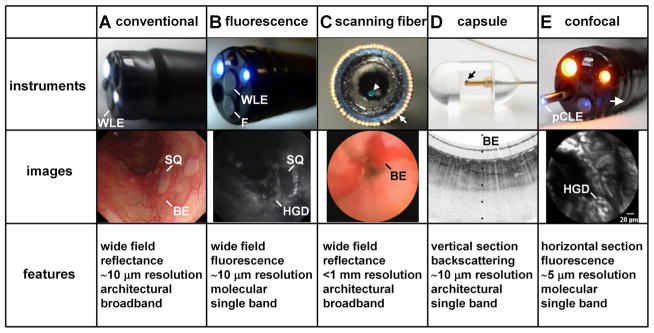
Conventional WLE is based on reflection of visible light from the mucosal surface to reveal the presence of structural abnormalities, such as nodularity, ulceration or oedema, that may harbour neoplasia. Images are collected with relatively low contrast compared with fluorescence, and disease is detected based on non-specific properties of tissue. Figure 3A shows a standard WLE used to visualise BE, which has a characteristic salmon pink colour. Recently, this technology has seen great improvement in resolution. High definition white light endoscopy (HD-WLE) use charge-coupled device detectors that have >106 pixels and can achieve resolution on the cellular scale (~10 μm).24
Figure 3.
Novel imaging instruments. (A) Conventional white light endoscopy(WLE) shows squamous (SQ) patches within Barrett’s oesophagus (BE). (B) Fluorescence (F) endoscope shows molecular images of high-grade dysplasia (HGD; high signal) next to SQ (low signal). (C) Scanning fibre endoscope inserted transnasally shows patches of BE. (D) Capsule endoscopy with tethered probe shows cross-sectional image of BE on optical coherence tomography (images courtesy of G. Tearney and M. Gora). (E) Confocal laser endomicroscope (CLE) passes through instrument channel of endoscope to shows optical cross-section of HGD on molecular imaging in vivo. pCLE, probe-based CLE.
Chromoendoscopy uses WLE with intravital dye, such as methylene blue (peak absorption at 670 nm) that is topically applied the mucosal surface to enhance visibility of microanatomical features.25,26 A prospective, randomised crossover study of 47 patients using chromoendoscopy with methylene blue reported detection of dysplasia with 51% sensitivity and 48% specificity.25 A later randomised control trial showed dysplasia or EAC detection with 49% sensitivity and 85% specificity.26 A meta-analysis of nine clinical studies totalling 450 patients using chromoendoscopy with methylene blue found no improvement in diagnostic yield for neoplasia compared with WLE alone using the Seattle protocol.27 Chromoendoscopy has also been performed with acetic acid to produce a transient whitening effect caused by protein acetylation and tissue oedema. Dysplasia regains colour faster than BE and squamous. Table 1 summarises the results of a prospective clinical study that used chromoendoscopy with acetic acid to detect Barrett’s neoplasia with 95.6% sensitivity and 81% specificity.28 However, a false-positive rate of 19.6% was observed, most likely from areas of inflammation. Compared with WLE, chromoendoscopy with acetic acid has been reported to increase the yield of neoplasia on biopsy by 6.5-fold with a 15-fold decrease in biopsies needed.29 This study was not randomised or blinded. Overall, chromoendoscopy with acetic acid is well tolerated and low in cost.
Narrow band imaging (NBI) uses a ‘narrowed’ illumination spectrum to enhance image contrast. The optical filters in the video processor produce blue (440–460 nm) and green (540–560 nm) light to match the absorption peaks of Hb.30 This approach improves visualisation of tissue capillary structures, subepithelial vessels and surface topography. Subtle mucosal irregularities are used to reveal the presence of dysplasia. Table 1 summarises the results of clinical studies using NBI to detect Barrett’s neoplasia.31–34 A large meta-analysis totalling 502 patients showed that NBI had 91% sensitivity and 95% specificity for identifying HGD and 91% sensitivity and 85% specificity for detecting BE.34 The use of NBI alone compared with WLE showed a non-significant difference for detection of Barrett’s neoplasia. However, NBI may reduce the number of biopsies needed to achieve a comparable diagnostic performance with WLE.33 Recent technological advances in NBI include an optical zoom for improved resolution of mucosal patterns. However, clinical data do not support an improvement in overall disease detection compared with standard WLE.
Autofluorescence imaging (AFI) uses blue light (λex=395–475 nm) to excite non-specific endogenous fluorophores, such as collagen and elastin, and collects fluorescence in the visible region (490–625 nm).35 In these images, squamous and BE appear green and neoplasia appears magenta in colour. A randomised clinical study of 187 patients showed that the use of AFI resulted in 1.5%–6.7% improvement in detection of HGD and EAC compared with conventional WLE.36 Technological improvements in AFI (gen II and III) resulted in a 44% improvement in detection of HGD and EAC compared with WLE.37 However, AFI has high-false positive rate of 86%, and its clinical use remains unclear.38 A meta-analysis of five prospective studies totalling 371 patients showed that AFI offers ~2% improvement over WLE for detecting Barrett’s neoplasia.39 AFI may be clinically useful in high-risk patients after either ablation or surgical resection to assess for residual disease. Endoscopic trimodal imaging (ETMI) combines WLE, NBI and AFI technologies.40,41 As with AFI, the clinical usefulness of ETMI remains unclear. The false-positive rate remained high. Prospective studies have shown no significant difference for detection of dysplasia compared with WLE.
Fluorescence endoscopes have been developed to perform wide-field imaging using custom filters for excitation and emission to match the spectral properties of fluorophores used to label molecular probes being developed for detection of specific biological targets. Figure 3B shows a fluorescence endoscope that provides a single blue excitation through a standard light guide to excite fluorescein isothiocyanate (FITC) to detect a single target. Figure 3C shows a scanning fibre endoscope that provides three excitation (blue, green and red) wavelengths delivered through a single optical fibre (arrow) to excite three dyes (DEAC, FITC and Cy5) that have distinct emission spectra and can be used to detect three targets simultaneously.42 These instruments provide reflectance images as well to produce an anatomical background to help with image interpretation.
ADVANCED CROSS-SECTIONAL ENDOSCOPY
Optical coherence tomography (OCT) uses a low coherence laser to measure differences in time delay in between light that backscatters from below the tissue surface and a reference beam. Cross-sectional images are collected in vivo with a view similar to that of histology but in real time. This approach is similar to ultrasound but uses NIR light instead to achieve much higher axial resolution (1–10 μm) at a tradeoff of reduced tissue depth (1–2 mm). Epithelial and subsquamous structures (blood vessels, glands, cysts and crypts) can be resolved.43 Table 1 summarises the results of a prospective clinical study of OCT in 33 patients that showed 68% sensitivity and 82% specificity for detection of Barrett’s neoplasia.44 A subsequent prospective clinical study showed that OCT could detect HGD and EAC with 83% sensitivity and 73% specificity.45 Limitations of OCT include images with low contrast and high interobserver and intraobserver variability for image interpretation and prediction of pathology.45 Optical frequency domain imaging (OFDI) uses advanced scanning technology to collect images based on the OCT mechanism at much higher speeds and can produce three-dimensional images. Clinically, OFDI can resolve long segments (>6 cm) of BE in <2 min.46 Results of a clinical study using OFDI showed 60% sensitivity and 80% specificity in assignment of squamous or columnar tissues.47 Figure 3D shows integration of OFDI imaging technology into a pill-sized capsule connected with a flexible optical fibre.48 A clinical study was performed in 13 patients to collect in vivo images of BE. However, the capsule does not have capability to perform tissue biopsy, and suspect mucosal regions may be difficult to locate on follow-up endoscopy. A validated classification system for correlating in vivo images with histology is needed before OCT/OFDI can be widely accepted for clinical use. Also, physicians will need specialised training to interpret these images in real time.
Confocal laser endomicroscopy (CLE) collects fluorescence to visualise ‘histology-like’ images in real-time. The instrument can achieve subcellular resolution (1–5 μm) at high magnifications (500–1000×). Figure 3E shows a probe-based (pCLE) instrument that passes through the biopsy channel of a standard medical endoscope. Images are collected with a small field of view (FOV) that ranges from 240×240 to 600×600 μm2 with frame rates that range from 8 to 12 per second. The working distance is fixed for each imaging probe and can range from 30 to 70 μm.49 An endoscope-based (eCLE) instrument integrates the optics and scanner into the distal end of the endoscope. Images with high lateral and axial resolution of 0.7 and 7 μm, respectively, can be collected with a FOV of 500×500 μm2 at 0.8–1.6 frames per second. The imaging depth can be manually adjusted from 0 to 250 μm.50 Both pCLE and eCLE use blue laser light (488 nm) to excite intravenously administrated fluorescein to generate image contrast. Fluorescein is Food and Drug Administration (FDA) approved for human use and is well tolerated.
CLE images are interpreted by evaluating the appearance of capillary structures and cellular architecture on fluorescence.51 Images of BE show organised morphology with distinct columnar-lined epithelial cells and structured capillaries. Figure 3E shows HGD with heterogeneous cellular features, ill-defined borders and irregular capillaries. Bright fluorescence can be seen in the lamina propria from leakage of the fluorescein contrast.51 A clinical study using CLE to image Barrett’s neoplasia has shown 92.9% sensitivity, 98.4% specificity and 98.4% negative predictive value (NPV). An interobserver and intraobserver agreement (κ) of 0.84 and 0.89, respectively, was found, suggesting that physicians could use imaging criteria to interpret the images and that the results are reproducible. Several studies have further investigated CLE classification criteria for real-time diagnosis of Barrett’s neoplasia.52–56 The Miami criteria has been widely accepted and has been validated in randomised controlled trials. This image classification system defines BE as having uniform villiform architecture and columnar epithelial cells with dark goblet cells.54 In HGD, villiform structures persist with irregularly shaped crypts and dilated capillary vessels. In EAC, a complete loss of crypt and villiform architecture is observed with irregular and dilated capillaries.
In clinical practice, confocal imaging may reduce the number of unnecessary biopsies during BE surveillance and may help to guide real-time endoscopic therapy of Barrett’s neoplasia. A meta-analysis of seven studies totalling 345 patients reports 86% sensitivity, 83% specificity and 96% NPV for detection of HGD/EAC with CLE.57 Randomized clinical studies have shown that combining either pCLE or eCLE with WLE can produce higher sensitivity for detecting Barrett’s neoplasia and can reduce up to 65% of the number of biopsies needed to achieve comparable diagnostic performance compared with WLE alone.58,59 Limitations of pCLE and eCLE include consistency in collecting interpretable images, an image FOV limited to a few hundred microns, special training needed for image interpretation, and potential for miss-registration of CLE images with histology. Also, intravenous fluorescein, a non-specific contrast agent, can extravasate and produce false positives.
MOLECULAR IMAGING
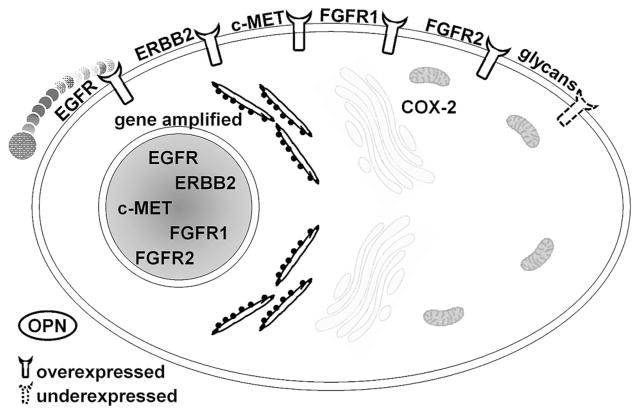
Advanced imaging technologies based on non-specific contrast mechanisms have not demonstrated a clear clinical advantage for improved detection of Barrett’s neoplasia. Molecular imaging is an emerging methodology that detects overexpressed targets specific for cancer that promises to overcome these limitations. The molecular mechanisms that drive progression of Barrett’s neoplasia are under intense investigation. Genetic instability,60 including chromosomal aberrations (aneuploidy/tetraploidy), loss of heterozygosity, changes in DNA methylation, abnormalities in tumour suppressor loci, changes in cell cycle regulation, dysregulation of cell signalling and focal gene amplifications and deletions are believed to play important roles in the initiation and progression of disease.61–64 Many of these changes have been identified by copy number variation on analysis with single nucleotide polymorphism arrays.65 High-frequency gene amplification can produce overexpression of protein targets on the cell surface, cytoplasm or extracellular matrix that are accessible to imaging. Figure 4 shows a number of promising imaging targets that can be developed for imaging of Barrett’s neoplasia. Epidermal growth factor receptor (EGFR), ErbB2, Fibroblast Growth Factor Receptor (FGFR)1/2 and c-MET are transmembrane tyrosine kinase receptors that stimulate epithelial cell growth, proliferation and differentiation.66–69 Glycans are cell surface glycoproteins that are under-expressed in Barrett’s neoplasia.70 Cyclooxygenase-2 (COX-2) is an intracellular enzyme that is absent in normal cells and found at increased levels in HGD and early EAC.64,71 Osteopontin is a secreted extracellular matrix protein that is highly overexpressed in EAC.72
Figure 4.
Targets for molecular imaging. Cell surface glycans are underexpressed with disease progression in oesophageal cancer (EAC), and can be detected with lectins. Protein targets (epidermal growth factor receptor (EGFR), ERBB2, c-MET, fibroblast growth factor receptors (FGFR) 1 and 2)) that are overexpressed in Barrett’s neoplasia are accessible to imaging with peptides and antibodies. Cyclooxygenase-2 (COX-2) is an intracellular enzyme that is absent in normal cells but increased in neoplasia. Osteopontin (OPN) is a secreted extracellular matrix protein that is highly overexpressed in EAC.
Because these targets are too small to be seen with endoscopy, even using HD-WLE, molecular probes are being developed that are labelled with bright fluorescent dyes as optical reporters. Figure 5 shows a number of different molecular probes that have been demonstrated in preclinical models of cancer with in vivo imaging and include lectins,70 peptides,73–75 antibodies,76–79 affibodies80,81 and activated enzymes.82,83 Topical application is a promising approach for delivery of these molecular probes for imaging of Barrett’s neoplasia because binding can occur rapidly and predictably within a few minutes. This time scale provides minimal interruption to the work flow for performing upper endoscopy in high volume procedure units. High contrast images can be achieved with minimal risk for toxicity and avoids undesired biodistribution of the molecular probe to other tissues. This is a major concern with systemic delivery.
Figure 5.
Molecular probe platforms. Various classes of molecular probes have been developed and demonstrated on imaging in vivo in preclinical models and in the clinic. Each class has unique strengths and weaknesses. Biochemical structures of commonly used fluorophores for molecular imaging are shown. FITC, fluorescein isothiocyanate.
Lectins are carbohydrate-binding proteins that bind specific-ally to glycans. In the progression of BE to neoplasia, cell surface glycans are lost, thus lectins show less binding. Wheat germ agglutinin is a lectin that has been fluorescein-labelled and shown to bind with high affinity and specificity to a subtype of glycans underexpressed in Barrett’s neoplasia.70 This imaging agent was topically applied to surgically resected specimens of BE and imaged with an AFI endoscope. Areas of neoplasia appeared dark, while squamous and BE regions avidly bind the lectin and were bright. Using blue excitation (λex=395–475 nm), images with areas of decreased fluorescence were found with a target-to-background ratio (T/B) ratio of 5.2. Lectins have several advantages for clinical translation, including low production costs, stability at low pH and low toxicity. However, in vivo studies are needed to further to investigate this approach.
Peptide probes are short sequences of amino acids that bind specifically to cell surface targets and have been used to detect early Barrett’s neoplasia in vivo.74,84 Single peptide sequences specific for neoplastic targets were selected using binding assays with a high diversity phage display library. Peptides have advantages for diagnostic imaging that include low manufacture costs, long-term stability, rapid binding kinetics and low dissociation rates. An FITC-labelled peptide specific for HGD/EAC was topically applied to oesophagus in human subjects, and images were collected in vivo with pCLE. A T/B ratio of 3.8 was found for early neoplasia with 75% sensitivity and 97% specificity.74 Additional clinical studies are needed to validate clinical performance. Ongoing trials are being performed to investigate use of peptides with wide-field fluorescence endoscopy to overcome the small image FOV of CLE and increase the practical use of this technology in the clinic to guide tissue biopsy. A limitation of topical molecular probe application is that neoplasia present under neosquamous reepithelialised oesophageal mucosa may evade detection. This may be problematic for BE patients after therapy with radiofrequency ablation.85,86
Antibodies are large proteins derived from the immune system that have high target specificity and binding affinity and are used primarily for therapy. Recently, they have been fluorescently labelled for diagnostic imaging in vivo in clinical studies. An anti-EGFR antibody has been labelled with AlexaFluor 488 to detect colorectal adenomas that overexpress EGFR using eCLE.76 Also, adalimumab, an antibody for tumour necrosis factor, has been fluorescein labelled and used to monitor therapeutic response in patients with Crohn’s disease using eCLE.77 An antibody specific for ErbB2 (HER2) was labelled with AlexaFluor 488 and used to image a rat model of EAC in vivo with pCLE.78 EAC showed a heterogeneous pattern of ErbB2 expression, and the fluorescence images had a mean T/B ratio of 1.6. Antibodies were also used with pCLE imaging to detect EGFR and survivin protein expressed in EAC.79 Widespread clinical use of antibodies for diagnostic imaging purposes may be limited by slow binding kinetics (>4 h), potential immunogenicity and high production costs. Affibodies consist of the binding region of antibodies and are over 20 times smaller in size. They have comparable binding kinetics and may have improved tumour penetrance, reduced immunogenicity and lower production costs.81
Activatable probes are optically dormant in the absence of disease and generate bright NIR fluorescence in the presence of proteolytic enzymes overexpressed in neoplasia. They can be ‘activated’ repeatedly to achieve high T/B ratios. NIR fluorescence endoscopy (λex=750 nm) has been used to detect cathepsin B activity in a mouse model of EAC.82 A cathepsin B-activated probe (Prosense750) was delivered intravenously into an orthotopic mouse model with human EAC cell implants. NIR images showed T/B ratios that was 3.6-fold to 4.5-fold greater in areas of neoplasia. In colon, in vivo fluorescence endoscopy (λex=465–500 nm) of colitis-associated neoplasia has been demonstrated using topical application of an activatable probe cleaved by γ-glutamyltranspeptidase. A T/B ratio of 7.0 was measured for dysplasia.83
CHALLENGES FOR MOLECULAR IMAGING
Molecular imaging of Barrett’s neoplasia is a promising direction but is at an early stage. The development of specific molecular probes is challenged by the rigours required for target validation. In addition, the regulatory path for FDA approval of a new imaging agent requires clinical studies to be performed under an Investigational New Drug application. Good manufacturing practices are needed for synthesis of the imaging agent, and Good laboratory practices are needed for the pharmacology/toxicological studies in animals to establish safety prior to clinical use. Also, target expression in Barrett’s neoplasia is characterised by molecular heterogeneity,87 thus imaging of multiple targets may be required for effective use in a diverse patient population. Multiplexed detection of several targets simultaneously may overcome this challenge. In vivo imaging with the scanning fibre endoscope using three peptides has been demonstrated in mouse colonic adenomas and is a promising direction.75 Further development of this optical technology is needed to perform in vivo imaging of Barrett’s neoplasia in clinical studies.
FUTURE OUTLOOK
Recently, the number of advanced imaging technologies being developed to improve surveillance of BE has undergone explosive growth. Optical methods take advantage of the broad spectrum of light to perform real-time imaging. WLE, chromoendoscopy, NBI, AFI and ETMI are wide-field approaches based on non-specific contrast mechanisms. Although the resolution of these instruments has improved, clinical studies have not shown significant improvement for detection of Barrett’s neoplasia. Imaging studies using AFI and ETMI have shown an overall increase in detection of neoplasia, but these technologies are limited by high false-positive rates. Chromoendoscopy using topically applied intravital dyes has unclear clinical utility in BE surveillance. OCTand OFDI are cross-sectional methods that provide imaging depth of 1–2 mm and may be useful for detection of subsurface neoplasia. These methods are limited by low contrast and variability in image interpretation. CLE is another cross-sectional technology that provides real-time ‘histology-like’ images for in vivo pathology and has been used to target biopsy of early neoplasia on molecular imaging. However, this approach is limited by a small FOV that is inadequate to evaluate the large surface areas of BE that need surveillance. Ultimately, there remains a clear unmet clinical need for a wide-field imaging method that rapidly and specifically identifies localised areas of neoplasia to guide physician intervention.
Many of the instruments being developed are sensitive to fluorescence and can also be used for molecular imaging. This approach identifies overexpressed biological targets that appear before mucosal changes become visible and is potentially transformative for BE surveillance. The current paradigm for medical decision making based on observation of structural lesions may soon be replaced by visualisation of molecular expression. The specific targets detected can also be used to guide appropriate therapy for individual patients. A number of molecular probe platforms are being developed and include lectins, peptides, antibodies, affibodies and activatable enzymes. These probes have already been demonstrated in vivo in preclinical imaging studies using fluorescence methods that provide high contrast. Some of these probes have also been studied in the clinic. This targeted approach will require further development of molecular probes and endoscopic instruments and will need to accelerate along the long and complex path for regulatory approval by the FDA. While molecular imaging is currently at an early stage, the potential for use of cancer biomarkers to perform early detection, stage T1a versus T1b lesions, guide choice of therapy and monitor therapeutic response is vast. The availability of optical tools that can significantly improve our ability to help patients with BE lies just over the horizon.
Acknowledgments
Funding U.S. Department of Health and Human Services-National Institutes of Health U54 CA163059
Footnotes
Contributors Drafting of the manuscript: MBS, TDW.
Competing interests None declared.
Patient consent Obtained.
Provenance and peer review Commissioned; externally peer reviewed.
References
- 1.Ferlay J, Soerjomataram I, Ervik M, et al. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11. Lyon, France: International Agency for Research on Cancer; 2013. http://globocan.iarc.fr. [Google Scholar]
- 2.American Cancer Society. Cancer facts & figures 2012. Atlanta: American Cancer Society; 2012. [Google Scholar]
- 3.Hur C, Miller M, Kong CY, et al. Trends in esophageal adenocarcinoma incidence and mortality. Cancer. 2013;119:1149–58. doi: 10.1002/cncr.27834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lagergren J, Bergström R, Lindgren A, et al. Symptomatic gastroesophageal reflux as a risk factor for esophageal adenocarcinoma. N Engl J Med. 1999;340:825–31. doi: 10.1056/NEJM199903183401101. [DOI] [PubMed] [Google Scholar]
- 5.Ryan AM, Duong M, Healy L, et al. Obesity, metabolic syndrome and esophageal adenocarcinoma: Epidemiology, etiology and new targets. Cancer Epidemiol. 2011;35:309–19. doi: 10.1016/j.canep.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 6.Pohl H, Wrobel K, Bojarski C, et al. Risk factors in the development of esophageal adenocarcinoma. Am J Gastroenterol. 2013;108:200–7. doi: 10.1038/ajg.2012.387. [DOI] [PubMed] [Google Scholar]
- 7.Schlemper RJ, Riddell RH, Kato Y, et al. The Vienna classification of gastrointestinal epithelial neoplasia. Gut. 2000;47:251–5. doi: 10.1136/gut.47.2.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.De Jonge PJF, Van Blankenstein M, Grady WM, et al. Barrett’s oesophagus: epidemiology, cancer risk and implications for management. Gut. 2014;63:191–202. doi: 10.1136/gutjnl-2013-305490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yousef F, Cardwell C, Cantwell MM, et al. The incidence of esophageal cancer and high-grade dysplasia in Barrett’s esophagus: a systematic review and meta-analysis. Am J Epidemiol. 2008;168:237–49. doi: 10.1093/aje/kwn121. [DOI] [PubMed] [Google Scholar]
- 10.Hvid-Jensen F, Pedersen L, Drewes AM, et al. Incidence of adenocarcinoma among patients with Barrett’s esophagus. N Engl J Med. 2011;365:1375–83. doi: 10.1056/NEJMoa1103042. [DOI] [PubMed] [Google Scholar]
- 11.Desai TK, Krishnan K, Samala N, et al. The incidence of oesophageal adenocarcinoma in non-dysplastic Barrett’s oesophagus: a meta-analysis. Gut. 2012;61:970–6. doi: 10.1136/gutjnl-2011-300730. [DOI] [PubMed] [Google Scholar]
- 12.Heitmiller RF, Redmond M, Hamilton SR. Barrett’s esophagus with high-grade dysplasia. An indication for prophylactic esophagectomy. Ann Surg. 1996;224:66–71. doi: 10.1097/00000658-199607000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Konda VJA, Ross AS, Ferguson MK, et al. Is the risk of concomitant invasive esophageal cancer in high-grade dysplasia in Barrett’s esophagus overestimated? Clin Gastroenterol Hepatol. 2008;6:159–64. doi: 10.1016/j.cgh.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 14.Sharma P, Falk GW, Weston AP, et al. Dysplasia and cancer in a large multicenter cohort of patients with Barrett’s esophagus. Clin Gastroenterol Hepatol. 2006;4:566–72. doi: 10.1016/j.cgh.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 15.Picardo SL, O’Brien MP, Feighery R, et al. A Barrett’s esophagus registry of over 1000 patients from a specialist center highlights greater risk of progression than population-based registries and high risk of low grade dysplasia. Dis Esophagus. 2015;28:121–6. doi: 10.1111/dote.12166. [DOI] [PubMed] [Google Scholar]
- 16.Singh S, Manickam P, Amin AV, et al. Incidence of esophageal adenocarcinoma in Barrett’s esophagus with low-grade dysplasia: a systematic review and meta-analysis. Gastrointest Endosc. 2014;79:897–909. doi: 10.1016/j.gie.2014.01.009. [DOI] [PubMed] [Google Scholar]
- 17.Spechler SJ, Sharma P, Souza RF, et al. American Gastroenterological Association. American Gastroenterological Association medical position statement on the management of Barrett’s esophagus. Gastroenterology. 2011;140:1084–91. doi: 10.1053/j.gastro.2011.01.030. [DOI] [PubMed] [Google Scholar]
- 18.Evans JA, Early DS, Fukami N, et al. The role of endoscopy in Barrett’s esophagus and other premalignant conditions of the esophagus. Gastrointest Endosc. 2012;76:1087–94. doi: 10.1016/j.gie.2012.08.004. [DOI] [PubMed] [Google Scholar]
- 19.Fitzgerald RC, di Pietro M, Ragunath K, et al. British Society of Gastroenterology guidelines on the diagnosis and management of Barrett’s oesophagus. Gut. 2014;63:7–42. doi: 10.1136/gutjnl-2013-305372. [DOI] [PubMed] [Google Scholar]
- 20.Peters FP, Curvers WL, Rosmolen WD, et al. Surveillance history of endoscopically treated patients with early Barrett’s neoplasia: nonadherence to the Seattle biopsy protocol leads to sampling error. Dis Esophagus. 2008;21:475–9. doi: 10.1111/j.1442-2050.2008.00813.x. [DOI] [PubMed] [Google Scholar]
- 21.Abrams JA, Kapel RC, Lindberg GM, et al. Adherence to biopsy guidelines for Barrett’s esophagus surveillance in the community setting in the United States. Clin Gastroenterol Hepatol. 2009;7:736–42. doi: 10.1016/j.cgh.2008.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kariv R, Plesec TP, Goldblum JR, et al. The Seattle protocol does not more reliably predict the detection of cancer at the time of esophagectomy than a less intensive surveillance protocol. Clin Gastroenterol Hepatol. 2009;7:653–8. doi: 10.1016/j.cgh.2008.11.024. [DOI] [PubMed] [Google Scholar]
- 23.Mashimo H. Subsquamous intestinal metaplasia after ablation of Barrett’s esophagus: frequency and importance. Curr Opin Gastroenterol. 2013;29:454–9. doi: 10.1097/MOG.0b013e3283622796. [DOI] [PubMed] [Google Scholar]
- 24.Kwon RS, Adler DG, Chand B, et al. ASGE Technology Committee. High-resolution and high-magnification endoscopes. Gastrointest Endosc. 2009;69(3 Pt 1):399–407. doi: 10.1016/j.gie.2008.12.049. [DOI] [PubMed] [Google Scholar]
- 25.Wo JM, Ray MB, Mayfield-Stokes S, et al. Comparison of methylene blue-directed biopsies and conventional biopsies in the detection of intestinal metaplasia and dysplasia in Barrett’s esophagus: a preliminary study. Gastrointest Endosc. 2001;54:294–301. doi: 10.1067/mge.2001.115732. [DOI] [PubMed] [Google Scholar]
- 26.Ragunath K, Krasner N, Raman VS, et al. A randomized, prospective cross-over trial comparing methylene blue-directed biopsy and conventional random biopsy for detecting intestinal metaplasia and dysplasia in Barrett’s esophagus. Endoscopy. 2003;35:998–1003. doi: 10.1055/s-2003-44599. [DOI] [PubMed] [Google Scholar]
- 27.Ngamruengphong S, Sharma VK, Das A. Diagnostic yield of methylene blue chromoendoscopy for detecting specialized intestinal metaplasia and dysplasia in Barrett’s esophagus: a meta-analysis. Gastrointest Endosc. 2009;69:1021–8. doi: 10.1016/j.gie.2008.06.056. [DOI] [PubMed] [Google Scholar]
- 28.Longcroft-Wheaton G, Duku M, Mead R, et al. Acetic acid spray is an effective tool for the endoscopic detection of neoplasia in patients with Barrett’s esophagus. Clin Gastroenterol Hepatol. 2010;8:843–7. doi: 10.1016/j.cgh.2010.06.016. [DOI] [PubMed] [Google Scholar]
- 29.Tholoor S, Bhattacharyya R, Tsagkournis O, et al. Acetic acid chromoendoscopy in Barrett’s esophagus surveillance is superior to the standardized random biopsy protocol: results from a large cohort study (with video) Gastrointest Endosc. 2014;80:417–24. doi: 10.1016/j.gie.2014.01.041. [DOI] [PubMed] [Google Scholar]
- 30.Lambert R, Kuznetsov K, Rey J-F. Narrow-band imaging in digestive endoscopy. ScientificWorldJournal. 2007;7:449–65. doi: 10.1100/tsw.2007.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sharma P, Bansal A, Mathur S, et al. The utility of a novel narrow band imaging endoscopy system in patients with Barrett’s esophagus. Gastrointest Endosc. 2006;64:167–75. doi: 10.1016/j.gie.2005.10.044. [DOI] [PubMed] [Google Scholar]
- 32.Singh M, Bansal A, Curvers WL, et al. Observer agreement in the assessment of narrowband imaging system surface patterns in Barrett’s esophagus: a multicenter study. Endoscopy. 2011;43:745–51. doi: 10.1055/s-0030-1256631. [DOI] [PubMed] [Google Scholar]
- 33.Sharma P, Hawes RH, Bansal A, et al. Standard endoscopy with random biopsies versus narrow band imaging targeted biopsies in Barrett’s oesophagus: a prospective, international, randomised controlled trial. Gut. 2013;62:15–21. doi: 10.1136/gutjnl-2011-300962. [DOI] [PubMed] [Google Scholar]
- 34.Song J, Zhang J, Wang J, et al. Meta-analysis of the effects of endoscopy with narrow band imaging in detecting dysplasia in Barrett’s esophagus. Dis Esophagus. 2014 doi: 10.1111/dote.12222. Published Online First: 24 Apr 2014. [DOI] [PubMed] [Google Scholar]
- 35.Song L-M, Banerjee S, Desilets D, et al. ASGE Technology Committee. Autofluorescence imaging. Gastrointest Endosc. 2011;73:647–50. doi: 10.1016/j.gie.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 36.Borovicka J, Fischer J, Neuweiler J, et al. Autofluorescence endoscopy in surveillance of Barrett’s esophagus: a multicenter randomized trial on diagnostic efficacy. Endoscopy. 2006;38:867–72. doi: 10.1055/s-2006-944726. [DOI] [PubMed] [Google Scholar]
- 37.Boerwinkel DF, Holz JA, Aalders MC, et al. Third-generation autofluorescence endoscopy for the detection of early neoplasia in Barrett’s esophagus: a pilot study. Dis Esophagus. 2014;27:276–84. doi: 10.1111/dote.12094. [DOI] [PubMed] [Google Scholar]
- 38.Giacchino M, Bansal A, Kim RE, et al. Clinical utility and interobserver agreement of autofluorescence imaging and magnification narrow-band imaging for the evaluation of Barrett’s esophagus: a prospective tandem study. Gastrointest Endosc. 2013;77:711–18. doi: 10.1016/j.gie.2013.01.029. [DOI] [PubMed] [Google Scholar]
- 39.Boerwinkel DF, Holz JA, Kara MA, et al. Effects of autofluorescence imaging on detection and treatment of early neoplasia in patients with Barrett’s esophagus. Clin Gastroenterol Hepatol. 2014;12:774–81. doi: 10.1016/j.cgh.2013.10.013. [DOI] [PubMed] [Google Scholar]
- 40.Curvers WL, Herrero LA, Wallace MB, et al. Endoscopic tri-modal imaging is more effective than standard endoscopy in identifying early-stage Neoplasia in Barrett’s esophagus. Gastroenterology. 2010;139:1106–14. doi: 10.1053/j.gastro.2010.06.045. [DOI] [PubMed] [Google Scholar]
- 41.Curvers WL, van Vilsteren FG, Baak LC, et al. Endoscopic trimodal imaging versus standard video endoscopy for detection of early Barrett’s neoplasia: a multicenter, randomized, crossover study in general practice. Gastrointest Endosc. 2011;73:195–203. doi: 10.1016/j.gie.2010.10.014. [DOI] [PubMed] [Google Scholar]
- 42.Lee CM, Engelbrecht CJ, Soper TD, et al. Scanning fiber endoscopy with highly flexible, 1-mm catheterscopes for wide-field, full-color imaging. J Biophotonics. 2010;3:385–407. doi: 10.1002/jbio.200900087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cobb MJ, Hwang JH, Upton MP, et al. Imaging of subsquamous Barrett’s epithelium with ultrahigh-resolution optical coherence tomography: a histologic correlation study. Gastrointest Endosc. 2010;71:223–30. doi: 10.1016/j.gie.2009.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Isenberg G, Sivak MV, Jr, Chak A, et al. Accuracy of endoscopic optical coherence tomography in the detection of dysplasia in Barrett’s esophagus: a prospective, double-blinded study. Gastrointest Endosc. 2005;62:825–31. doi: 10.1016/j.gie.2005.07.048. [DOI] [PubMed] [Google Scholar]
- 45.Evans JA, Poneros JM, Bouma BE, et al. Optical coherence tomography to identify intramucosal carcinoma and high-grade dysplasia in Barrett’s esophagus. Clin Gastroenterol Hepatol. 2006;4:38–43. doi: 10.1053/S1542-3565(05)00746-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Suter MJ, Vakoc BJ, Yachimski PS, et al. Comprehensive microscopy of the esophagus in human patients with optical frequency domain imaging. Gastrointest Endosc. 2008;68:745–53. doi: 10.1016/j.gie.2008.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Suter MJ, Gora MJ, Lauwers GY, et al. Esophageal-guided biopsy with volumetric laser endomicroscopy and laser cautery marking: a pilot clinical study. Gastrointest Endosc. 2014;79:886–96. doi: 10.1016/j.gie.2013.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gora MJ, Sauk JS, Carruth RW, et al. Tethered capsule endomicroscopy enables less invasive imaging of gastrointestinal tract microstructure. Nat Med. 2013;19:238–40. doi: 10.1038/nm.3052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jabbour JM, Saldua MA, Bixler JN, et al. Confocal endomicroscopy: instrumentation and medical applications. Ann Biomed Eng. 2012;40:378–97. doi: 10.1007/s10439-011-0426-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.De Palma GD. Confocal laser endomicroscopy in the “in vivo” histological diagnosis of the gastrointestinal tract. World J Gastroenterol. 2009;15:5770–5. doi: 10.3748/wjg.15.5770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kiesslich R, Gossner L, Goetz M, et al. In vivo histology of Barrett’s esophagus and associated neoplasia by confocal laser endomicroscopy. Clin Gastroenterol Hepatol. 2006;4:979–87. doi: 10.1016/j.cgh.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 52.Pohl H, Rosch T, Vieth M, et al. Miniprobe confocal laser microscopy for the detection of invisible neoplasia in patients with Barrett’s oesophagus. Gut. 2008;57:1648–53. doi: 10.1136/gut.2008.157461. [DOI] [PubMed] [Google Scholar]
- 53.Sharma P, Meining A, Coron E, et al. 1071 Detection of Neoplastic Tissue in Barrett’s Esophagus With In Vivo Probe-Based Confocal Endomicroscopy (DONT BIOPCE). Final Results of a Prospective International RCT: Image Guided Versus 4 Quadrant Random Biopsies? Gastroenterology. 2010;138(5, Supplement 1):S-155. [Google Scholar]
- 54.Wallace M, Lauwers GY, Chen Y, et al. Miami classification for probe-based confocal laser endomicroscopy. Endoscopy. 2011;43:882–91. doi: 10.1055/s-0030-1256632. [DOI] [PubMed] [Google Scholar]
- 55.Gaddam S, Mathur SC, Singh M, et al. Novel probe-based confocal laser endomicroscopy criteria and interobserver agreement for the detection of dysplasia in Barrett’s esophagus. Am J Gastroenterol. 2011;106:1961–9. doi: 10.1038/ajg.2011.294. [DOI] [PubMed] [Google Scholar]
- 56.Tofteland N, Singh M, Gaddam S, et al. Evaluation of the updated confocal laser endomicroscopy criteria for Barrett’s esophagus among gastrointestinal pathologists. Dis Esophagus. 2014;27:623–9. doi: 10.1111/dote.12121. [DOI] [PubMed] [Google Scholar]
- 57.Gupta A, Attar BM, Koduru P, et al. Utility of confocal laser endomicroscopy in identifying high-grade dysplasia and adenocarcinoma in Barrett’s esophagus: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2014;26:369–77. doi: 10.1097/MEG.0000000000000057. [DOI] [PubMed] [Google Scholar]
- 58.Sharma P, Meining AR, Coron E, et al. Real-time increased detection of neoplastic tissue in Barrett’s esophagus with probe-based confocal laser endomicroscopy: final results of an international multicenter, prospective, randomized, controlled trial. Gastrointest Endosc. 2011;74:465–72. doi: 10.1016/j.gie.2011.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Canto MI, Anandasabapathy S, Brugge W, et al. In vivo endomicroscopy improves detection of Barrett’s esophagus–related neoplasia: a multicenter international randomized controlled trial (with video) Gastrointest Endosc. 2014;79:211–21. doi: 10.1016/j.gie.2013.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Dulak AM, Schumacher SE, van Lieshout J, et al. Gastrointestinal adenocarcinomas of the esophagus, stomach, and colon exhibit distinct patterns of genome instability and oncogenesis. Cancer Res. 2012;72:4383–93. doi: 10.1158/0008-5472.CAN-11-3893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Maley CC, Galipeau PC, Finley JC, et al. Genetic clonal diversity predicts progression to esophageal adenocarcinoma. Nat Genet. 2006;38:468–73. doi: 10.1038/ng1768. [DOI] [PubMed] [Google Scholar]
- 62.Fitzgerald RC. Molecular basis of Barrett’s oesophagus and oesophageal adenocarcinoma. Gut. 2006;55:1810–20. doi: 10.1136/gut.2005.089144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Timmer MR, Sun G, Gorospe EC, et al. Predictive biomarkers for Barrett’s esophagus: so near and yet so far. Dis Esophagus. 2013;26:574–81. doi: 10.1111/dote.12015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chen M, Huang J, Zhu Z, et al. Systematic review and meta-analysis of tumor biomarkers in predicting prognosis in esophageal cancer. BMC Cancer. 2013;13:1–15. doi: 10.1186/1471-2407-13-539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gu J, Ajani JA, Hawk ET, et al. Genome-wide catalogue of chromosomal aberrations in Barrett’s esophagus and esophageal adenocarcinoma: a high-density single nucleotide polymorphism array analysis. Cancer Prev Res (Phila) 2010;3:1176–86. doi: 10.1158/1940-6207.CAPR-09-0265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cronin J, McAdam E, Danikas A, et al. Epidermal growth factor receptor (EGFR) is overexpressed in high-grade dysplasia and adenocarcinoma of the esophagus and may represent a biomarker of histological progression in Barrett’s esophagus (BE) Am J Gastroenterol. 2011;106:46–56. doi: 10.1038/ajg.2010.433. [DOI] [PubMed] [Google Scholar]
- 67.Varghese S, Lao–Sirieix P, Fitzgerald RC. Identification and Clinical Implementation of Biomarkers for Barrett’s esophagus. Gastroenterology. 2012;142:435–41. doi: 10.1053/j.gastro.2012.01.013. [DOI] [PubMed] [Google Scholar]
- 68.Tänzer M, Liebl M, Quante M. Molecular biomarkers in esophageal, gastric, and colorectal adenocarcinoma. Pharmacol Ther. 2013;140:133–47. doi: 10.1016/j.pharmthera.2013.06.005. [DOI] [PubMed] [Google Scholar]
- 69.Mokrowiecka A, Wierzchniewska-Lawska A, Smolarz B, et al. Amplification of Her-2/neu oncogene in GERD—Barrett’s metaplasia—dysplasia—adenocarcinoma sequence. Hepatogastroenterology. 2013;60:1063–6. doi: 10.5754/hge121343. [DOI] [PubMed] [Google Scholar]
- 70.Bird-Lieberman EL, Neves AA, Lao-Sirieix P, et al. Molecular imaging using fluorescent lectins permits rapid endoscopic identification of dysplasia in Barrett’s esophagus. Nat Med. 2012;18:315–21. doi: 10.1038/nm.2616. [DOI] [PubMed] [Google Scholar]
- 71.Wilson KT, Fu S, Ramanujam KS, et al. Increased expression of inducible nitric oxide synthase and cyclooxygenase-2 in Barrett’s esophagus and associated adenocarcinomas. Cancer Res. 1998;58:2929–34. [PubMed] [Google Scholar]
- 72.Miller CT, Lin L, Casper AM, et al. Genomic amplification of MET with boundaries within fragile site FRA7G and upregulation of MET pathways in esophageal adenocarcinoma. Oncogene. 2005;25:409–18. doi: 10.1038/sj.onc.1209057. [DOI] [PubMed] [Google Scholar]
- 73.Hsiung PL, Hardy J, Friedland S, et al. Detection of colonic dysplasia in vivo using a targeted heptapeptide and confocal microendoscopy. Nat Med. 2008;14:454–8. doi: 10.1038/nm1692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sturm MB, Joshi BP, Lu S, et al. Targeted imaging of esophageal neoplasia with a fluorescently labeled peptide: first-in-human results. Sci Transl Med. 2013;5:184ra61. doi: 10.1126/scitranslmed.3004733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Joshi BP, Miller SJ, Lee CM, et al. Multispectral endoscopic imaging of colorectal dysplasia in vivo. Gastroenterology. 2012;143:1435–7. doi: 10.1053/j.gastro.2012.08.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Liu J, Zuo X, Li C, et al. In vivo molecular imaging of epidermal growth factor receptor in patients with colorectal neoplasia using confocal laser endomicroscopy. Cancer Lett. 2013;330:200–7. doi: 10.1016/j.canlet.2012.11.044. [DOI] [PubMed] [Google Scholar]
- 77.Atreya R, Neumann H, Neufert C, et al. In vivo imaging using fluorescent antibodies to tumor necrosis factor predicts therapeutic response in Crohn’s disease. Nat Med. 2014;20:313–18. doi: 10.1038/nm.3462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Realdon S, Dassie E, Fassan M, et al. In vivo molecular imaging of HER2 expression in a rat model of Barrett’s esophagus adenocarcinoma. Dis Esophagus. 2015;28:394–403. doi: 10.1111/dote.12210. [DOI] [PubMed] [Google Scholar]
- 79.Nakai Y, Shinoura S, Ahluwalia A, et al. Molecular imaging of epidermal growth factor-receptor and survivin in vivo in porcine esophageal and gastric mucosae using probe-based confocal laser-induced endomicroscopy: proof of concept. J Physiol Pharmacol. 2012;63:303–7. [PubMed] [Google Scholar]
- 80.Lee SB, Hassan M, Fisher R, et al. Affibody molecules for in vivo characterization of HER2-positive tumors by near-infrared imaging. Clin Cancer Res. 2008;14:3840–9. doi: 10.1158/1078-0432.CCR-07-4076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lofblom J, Feldwisch J, Tolmachev V, et al. Affibody molecules: engineered proteins for therapeutic, diagnostic and biotechnological applications. FEBS Lett. 2010;584:2670–80. doi: 10.1016/j.febslet.2010.04.014. [DOI] [PubMed] [Google Scholar]
- 82.Habibollahi P, Figueiredo JL, Heidari P, et al. Optical imaging with a Cathepsin B activated probe for the enhanced detection of esophageal adenocarcinoma by dual channel fluorescent upper GI endoscopy. Theranostics. 2012;2:227–34. doi: 10.7150/thno.4088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Mitsunaga M, Kosaka N, Choyke PL, et al. Fluorescence endoscopic detection of murine colitis-associated colon cancer by topically applied enzymatically rapid-activatable probe. Gut. 2013;62:1179–86. doi: 10.1136/gutjnl-2011-301795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Sturm MB, Piraka C, Elmunzer BJ, et al. In vivo molecular imaging of Barrett’s esophagus with confocal laser endomicroscopy. Gastroenterology. 2013;145:56–8. doi: 10.1053/j.gastro.2013.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Biddlestone LR, Barham CP, Wilkinson SP, et al. The histopathology of treated Barrett’s esophagus: squamous reepithelialization after acid suppression and laser and photodynamic therapy. Am J Surg Pathol. 1998;22:239–45. doi: 10.1097/00000478-199802000-00013. [DOI] [PubMed] [Google Scholar]
- 86.Satodate H, Inoue H, Fukami N, et al. Squamous reepithelialization after circumferential endoscopic mucosal resection of superficial carcinoma arising in Barrett’s esophagus. Endoscopy. 2004;36:909–12. doi: 10.1055/s-2004-825830. [DOI] [PubMed] [Google Scholar]
- 87.Leedham SJ, Preston SL, McDonald SA, et al. Individual crypt genetic heterogeneity and the origin of metaplastic glandular epithelium in human Barrett’s oesophagus. Gut. 2008;57:1041–8. doi: 10.1136/gut.2007.143339. [DOI] [PMC free article] [PubMed] [Google Scholar]