Abstract
Recently, Eclipse treatment planning system (TPS) version 8.8 was upgraded to the latest version 13.6. It is customary that the vendor gives training on how to upgrade the existing software to the new version. However, the customer is provided less inner details about changes in the new software version. According to manufacturer, accuracy of point dose calculations and irregular treatment planning is better in the new version (13.6) compared to the old version (8.8). Furthermore, the new version uses voxel-based calculations while the earlier version used point dose calculations. Major difference in intensity-modulated radiation therapy (IMRT) plans was observed between the two versions after re-optimization and re-calculations. However, minor difference was observed for IMRT cases after performing only re-calculations. It is recommended TPS quality assurance to be performed after any major upgrade of software. This can be done by performing dose calculation comparisons in TPS. To assess the difference between the versions, 25 clinical cases from the old version were compared keeping all the patient data intact including the monitor units and comparing the differences in dose calculations using dose volume histogram (DVH) analysis. Along with DVH analysis, uniformity index, conformity index, homogeneity index, and dose spillage index were also compared for both versions. The results of comparative study are presented in this paper.
Key words: Conformity index, dose spillage index, dose volume histogram, homogeneity index, treatment planning version, uniformity index
Introduction
Aim
The aim of this study is to validate the new version (13.6) of Eclipse™ treatment planning for AAA algorithm after upgrading from old version (8.8).
From time to time, treatment planning system (TPS) users accept the vendor's latest version of treatment planning system. Most customers will not do any quality assurance (QA) to assess the performance of new version of TPS with respect to old version. Recently, Ojala et al.[1] quantified the dose difference between two versions of Acuros algorithms from AXB10 to AXB11 version (Varian Medical Systems, Palo Alto, CA). In their study, AXB11 was compared with AXB10 on the dose calculation accuracy. However, no general conclusion was made that the dose calculation accuracy of the AXB10 would be inferior to the AXB11, except in air cavities. The deviations between the two versions of the algorithm in the dose volume histogram (DVH) analysis were generally small. Performance of dose calculation in lung stereotactic body radiotherapy[2] was studied by Ojala et al. The American Association of Physicists in Medicine TG65[3] studied the tissue homogeneities for dose calculations. This protocol quantified the uncertainty of dose calculations ranging from 1% to 5%. Comparison of dose calculation algorithms for different materials and in various clinical situations was also reported.[4,5,6,7,8,9,10]
In the current study, the goal was to find differences and similarities between old (8.8) and new (13.6) versions of Eclipse TPS from Varian (Varian Medical Systems, Palo Alto, CA). Manufacturer stated that dose calculations for old version (8.8) were based on interpolation of point doses and for new version (13.6) were based on volumetric dose estimation. In addition, the operating system in 13.6 used 64-bit architecture compared to the version 8.8 which used 32-bit architecture. This difference was identified by us as a major software change. Furthermore, according to the manufacturer,[11] major additional features and advantages of new Eclipse version (13.6) over 8.8 are as follows.
Rapid plan
Rapid, knowledge-based planning is a comprehensive treatment planning tool that provides clinicians with models that are representative of their clinical practice.
New optimization dialog
Display of dose on a selected orthogonal plane during optimization. One can change the viewing direction between the three different orthogonal planes
Generalized equivalent uniform dose-based objectives
Automatic normal tissue objective and mean dose objectives are now supported for both volumetric modulated arc therapy and intensity-modulated radiation therapy (IMRT) plans
Second source inhomogeneity correction is now supported for static gantry IMRT optimization
Jaw tracking option for Varian machines is now following the actual multi-leaf collimator (MLC) aperture and not the target projection. In earlier versions, the collimator positions were always kept outside the target structure projection in MLC-plane even when the actual MLC aperture was closed. Now, the collimators can follow the MLC aperture inside the target projection if necessary
The two-dimensional view in the optimization dialog box shows an approximation of the dose. The dose is not transferred to external beam planning. The final dose calculation is performed after optimization in external beam planning
To delete an objective, click the “x” on the row of the objective in the objective table. Objectives can no longer be deleted from DVH view.
Controlled structure terminology
Eclipse contains structure dictionary. The use of structure dictionary allows identifying structure by assigning standardized label. The assigned label is uniquely matched to computer readable code enabling effective data mining and exchange of knowledge models between systems using different naming schemes.
Smart adapt
Deformable registrations can now be inverted using menu driven software tools.
Plan converter
Plan converter is a new optional software module in Eclipse external beam planning that adapts the plan to another treatment unit or treatment technique. This feature enables you to convert a plan from treatment machine A to another treatment machine B.
Image visualization improvements
Multiple enhancements have been made including adding a neutral gamma correction and a wider range of computed tomography window/level to improve image quality.
Digitally reconstructed radiography quality improvement
Digitally reconstructed radiography quality and sharpness have been improved with stronger sharpness filtering and increased interpolation.
Eclipse scripting
Users can now add favorite scripts to the Eclipse menus.
In our study, different indices such as uniformity index (UI), conformity index (CI), homogeneity index (HI), and spillage of dose index (R50%) were computed for five sites for both the versions. The overall study showed that there was no significant difference between old and new versions for planning target volume (PTV) coverage and sparing of normal structures.
Methods
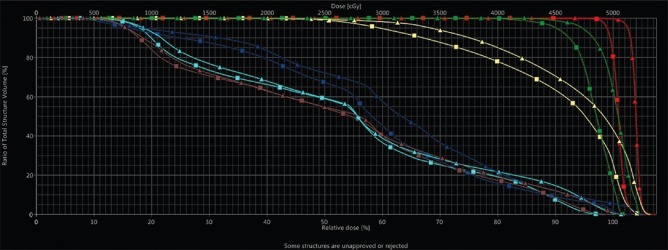
After the upgrade to the new software, some IMRT cases were evaluated and compared the DVH between the two versions. Major differences between the two versions were observed after performing re-optimization and re-calculations as can be seen from the following example shown in Figure 1. It was observed that the number of monitor units (MUs) got changed compared to the old version after re-optimization and re-calculation.
Figure 1.
Variations in doses for a case of cervix for both versions (8.8 and 13.6) - for IMRT technique (with re-optimization and re-calculations). ▴ Triangles are for version 13.6 and ▪ rectangles for version 8.8
To assess the difference between the versions, 25 clinical cases were studied comprising five sites, namely, head and neck, breast, lung, cervix, and stomach. Out of five sites, IMRT study was performed for cervix and head and neck and the three-dimensional conformal radiotherapy study was carried out for breast, lung, and stomach cases. While comparing the cases, the entire patient data were kept intact in both versions and then the differences in dose calculations using DVH were estimated. For IMRT cases, only dose calculations were done without re-optimization. All the 25 cases were already planned in old Eclipse version 8.8 planning system. These plans with same parameters (beam angle, number of beams, beam weights for each beam, prescribed dose, number of MUs, and other constraints) were kept constant and again dose calculations were performed in new version. The DVH data required for calculation of the indices (UI, CI, HI, R50%), defined below, were taken for both old and new versions of Eclipse TPS for each case. Further, to analyze the sparing of normal structures, data of mean, maximum doses for normal structures were taken wherever required. Since the dose differences were found to be very small compared to old version, planar dose distributions were not experimentally measured.
Brief definitions of the dose indices, uniformity index, conformity index, homogeneity index, and spillage of dose index
Conformity index
The CI was described by following formula[12]
CI = {TV95 /TV}{TV95 /V95}
where TV95 is the volume of target covered by 95% isodose line, TV is the total target volume, and V95 is the volume of tissue covered by the 95% isodose line. The value of CI varies between 0 and 1 and value close to unity is indicative of better conformity of dose to the PTV.
Uniformity index
The UI was defined as ratio of D5 to D95, where D5 and D95 are minimum doses to 5% and 95% of PTV as previously reported.[13,14,15]
The value of UI close to 1 signifies better uniformity of PTV dose.
Homogeneity index
HI was defined by a number of authors[16,17,18] as follows:
HI = (D5 − D95)/prescribed dose
Smaller the value of HI more is the homogeneous distribution in PTV.
Dose spillage index
R50%=50% isodose volume/PTV volume.
Lower R50% ratio indicates greater dose fall-off and better dose conformity around the PTV.
Results
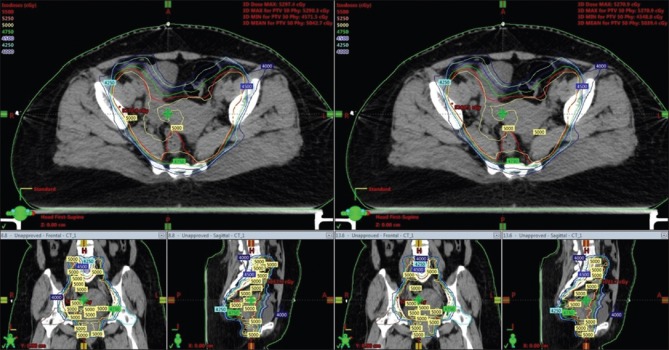
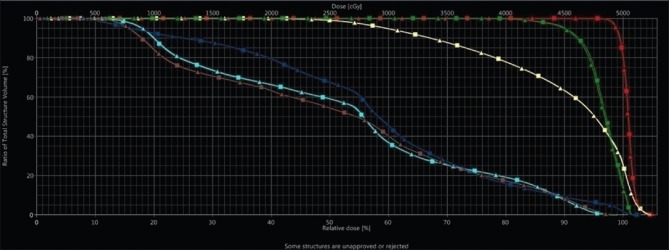
Table 1 shows the summary of mean values with standard deviation for calculated four indices for five sites for all 25 plans. From this, it can be observed that difference in four indices (CI, UI, HI, and R50%) for both versions is minimal for the five sites (lung, breast, stomach, cervix, and head and neck). Table 2 shows the mean values of doses to normal structures for both versions for all sites and the variation is <3% for all the organs. This shows that there is no significant difference in doses to normal organs even if you upgrade the version from 8.8 to 13.6. Figure 2 shows isodose curves on an axial slice at isocenter plane of versions 8.8 and 13.6 for a case of cervix. By comparing the isodose curves at different dose levels, change in PTV coverage is very small. This gives a similar result with minimal variation in coverage. Figure 3 shows the DVH for PTV and normal structures for a case of the cervix. It shows all DVH lines of PTV, bladder, rectum, both the femoral heads overlapping one over the other. This also shows that the both versions have resulted in similar dose distribution for estimating doses to PTV and different normal structures.
Table 1.
Summary of average values of DVH indices of 25 cases for 5 sites between the two Eclipse versions (8.8 and 13.6)
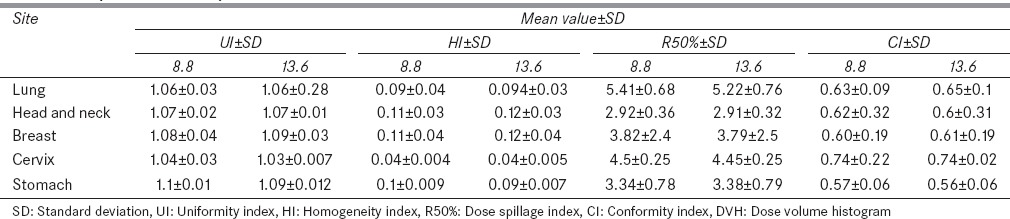
Table 2.
Summary of doses to normal structures for 25 clinical cases
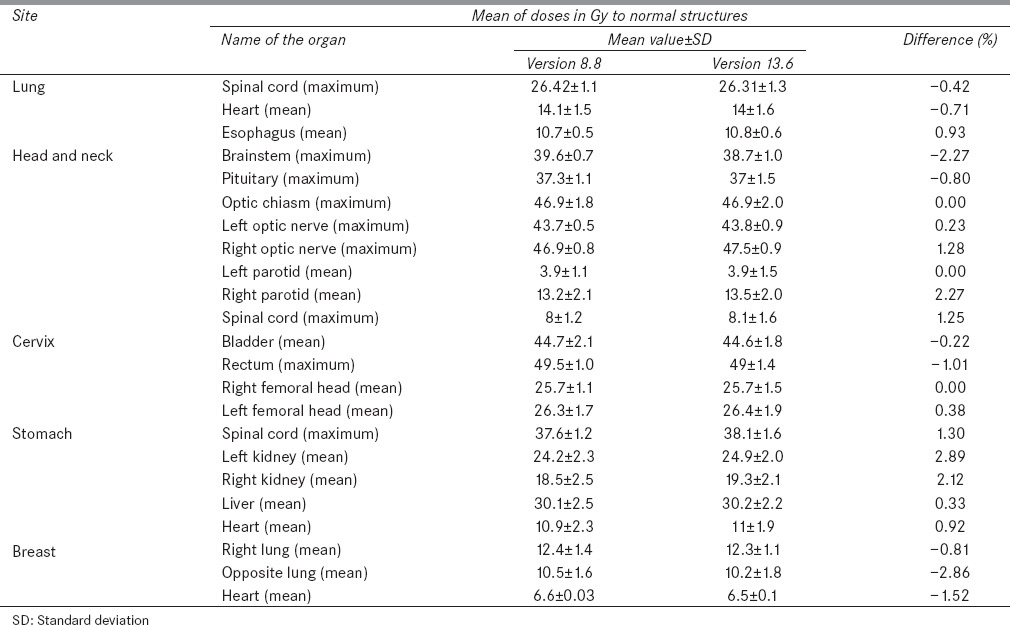
Figure 2.
Isodose curves on an axial slice at isocentre plane for a case of cervix between versions 8.8 and 13.6. Lower part of the figure shows the isodose distribution on coronal and sagittal plane of the corresponding slice
Figure 3.
Comparison of dose volume histogram curves of intensity-modulated radiation therapy plan of representative patient for planning target volume, rectum, bladder, left femoral head, and right femoral head for 8.8 and 13.6 version treatment planning system. ▴ Triangles are for version 13.6 and ▪ rectangles for version 8.8
Discussion
By performing dose calculations in both versions of the Eclipse planning system for five sites each of lung, breast, stomach, head and neck, and cervix, no significant difference in dose coverage was observed for the PTV or normal structures. This is evident from comparison of average values of the indices (UI, HI, CI, and R50%) for 25 cases for 5 sites, showing different clinical situations. With respect to all other organs at risk, sparing of normal structures is similar in both the versions. Although the methodology of the two versions is a major software change, there is no clinical significance to the dose calculation results. While evaluating the plans on both versions, we observed that the new version plans had run about 20% faster than the older version.
Conclusion
Whenever major software changes are made by the manufacturer, it is important that the users of the system should perform QA checks. In this paper, we have demonstrated such a study by making sure that both versions are operational before the new version is implemented in the clinic. We were able to compare several clinical plans using both the systems and determined that the new version 13.6 results in the same dose as the old version 8.8. This assured us that the new version maintained the plan quality. It is to be understood that normally version changes do not result in change in plan quality. However, QA of treatment planning could be performed along these guidelines whenever major software change takes place.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ojala JJ, Kapanen M. Quantification of dose differences between two versions of Acuros XB algorithm compared to Monte Carlo simulations – The effect on clinical patient treatment planning. J Appl Clin Med Phys. 2015;16:5642. doi: 10.1120/jacmp.v16i6.5642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ojala JJ, Kapanen MK, Hyödynmaa SJ, Wigren TK, Pitkänen MA. Performance of dose calculation algorithms from three generations in lung SBRT: Comparison with full Monte Carlo-based dose distributions. J Appl Clin Med Phys. 2014;15:4662. doi: 10.1120/jacmp.v15i2.4662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Papanikolau N, Battista JJ, Boyer AL, Boyer AL, Kappas C, Klein E, Mackie TR, et al. Report of Task Group No. 65 of the Radiation Therapy Committee of the American Association of Physicist in Medicine. AAPM Report No. 85. Madison, WI: Medical Physics Publishing; 2004. Tissue Inhomogeneity Corrections for Megavoltage Photon Beams. Available from: http://www.aapm.org/pubs/reports/rpt_85.pdf . [Google Scholar]
- 4.Knöös T, Wieslander E, Cozzi L, Brink C, Fogliata A, Albers D, et al. Comparison of dose calculation algorithms for treatment planning in external photon beam therapy for clinical situations. Phys Med Biol. 2006;51:5785–807. doi: 10.1088/0031-9155/51/22/005. [DOI] [PubMed] [Google Scholar]
- 5.Ojala J, Kapanen M, Sipilä P, Hyödynmaa S, Pitkänen M. The accuracy of Acuros XB algorithm for radiation beams traversing a metallic hip implant - Comparison with measurements and Monte Carlo calculations. J Appl Clin Med Phys. 2014;15:4912. doi: 10.1120/jacmp.v15i5.4912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ojala J. The accuracy of the Acuros XB algorithm in external beam radiotherapy – A comprehensive review. Int J Cancer Ther Oncol. 2014;2:020417. DOI: 10.14319/ijcto.0204.17. [Google Scholar]
- 7.Failla GA, Wareing T, Archambault Y, Thompson S. Clinical perspectives 2010. Palo Alto, CA: Varian Medical Systems; 2010. Acuros XB advanced dose calculation for the Eclipse treatment planning system. [Google Scholar]
- 8.Wareing TA, McGhee JM, Morel JE, Pautz SD. Discontinuous finite element SN methods on three-dimensional unstructured grids. Nucl Sci Eng. 2001;138:256–68. [Google Scholar]
- 9.Wareing TA, Morel JE, McGhee JM. Coupled electron-photon transport methods on 3-D unstructured grids. Trans Am Nucl Soc. 2000;83:240–2. [Google Scholar]
- 10.Vassiliev ON, Wareing TA, Davis IM, McGhee J, Barnett D, Horton JL, et al. Feasibility of a multigroup deterministic solution method for three-dimensional radiotherapy dose calculations. Int J Radiat Oncol Biol Phys. 2008;72:220–7. doi: 10.1016/j.ijrobp.2008.04.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Varian Medical Systems, Eclipse Treatment Planning Customer Release Note 13.6 MR 0.5. [Last accessed on 2015 Dec]. Available from: https://www.varian.com/sites/default/files/resource_attachments/ARIA_Minimum_Hardware_Specs_v13-6.pdf .
- 12.Feuvret L, Noël G, Mazeron JJ, Bey P. Conformity index: A review. Int J Radiat Oncol Biol Phys. 2006;64:333–42. doi: 10.1016/j.ijrobp.2005.09.028. [DOI] [PubMed] [Google Scholar]
- 13.Knöös T, Kristensen I, Nilsson P. Volumetric and dosimetric evaluation of radiation treatment plans: Radiation conformity index. Int J Radiat Oncol Biol Phys. 1998;42:1169–76. doi: 10.1016/s0360-3016(98)00239-9. [DOI] [PubMed] [Google Scholar]
- 14.Wang X, Zhang X, Dong L, Liu H, Gillin M, Ahamad A, et al. Effectiveness of noncoplanar IMRT planning using a parallelized multiresolution beam angle optimization method for paranasal sinus carcinoma. Int J Radiat Oncol Biol Phys. 2005;63:594–601. doi: 10.1016/j.ijrobp.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 15.Sheng K, Molloy JA, Larner JM, Read PW. A dosimetric comparison of non-coplanar IMRT versus Helical Tomotherapy for nasal cavity and paranasal sinus cancer. Radiother Oncol. 2007;82:174–8. doi: 10.1016/j.radonc.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 16.Nutting CM, Bedford JL, Cosgrove VP, Tait DM, Dearnaley DP, Webb S. A comparison of conformal and intensity-modulated techniques for oesophageal radiotherapy. Radiother Oncol. 2001;61:157–63. doi: 10.1016/s0167-8140(01)00438-8. [DOI] [PubMed] [Google Scholar]
- 17.Kataria T, Sharma K, Subramani V, Karrthick KP, Bisht SS. Homogeneity Index: An objective tool for assessment of conformal radiation treatments. J Med Phys. 2012;37:207–13. doi: 10.4103/0971-6203.103606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pezner RD, Liu A, Han C, Chen YJ, Schultheiss TE, Wong JY. Dosimetric comparison of helical tomotherapy treatment and step-and-shoot intensity-modulated radiotherapy of retroperitoneal sarcoma. Radiother Oncol. 2006;81:81–7. doi: 10.1016/j.radonc.2006.08.025. [DOI] [PubMed] [Google Scholar]
- 19.Merrow CE, Wang IZ, Podgorsak MB. A dosimetric evaluation of VMAT for the treatment of non-small cell lung cancer. J Appl Clin Med Phys. 2013;14:4110. doi: 10.1120/jacmp.v14i1.4110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Weyh A, Konski A, Nalichowski A, Maier J, Lack D. Lung SBRT: Dosimetric and delivery comparison of RapidArc, TomoTherapy, and IMR. J Appl Clin Med Phys. 2013;14:4065. doi: 10.1120/jacmp.v14i4.4065. [DOI] [PMC free article] [PubMed] [Google Scholar]