Abstract
Purpose of the Study:
To facilitate replication, we examined delivery characteristics, acceptability, and depression outcomes of a home-based intervention, Get Busy Get Better, Helping Older Adults Beat the Blues (GBGB). GBGB, previously tested in a randomized trial, reduced depressive symptoms and enhanced quality of life in African Americans.
Design and Methods:
A total of 208 African Americans aged above 55 years with Patient Health Questionnaire (PHQ-9) scores ≥5 on two subsequent screenings were randomized to receive GBGB immediately or 4 months later. GBGB involves up to 10 home sessions consisting of care management, referral/linkage, depression education/symptom recognition, stress reduction, and behavioral activation. Interventionists recorded delivery characteristics (dose, intensity) and perceived acceptability of sessions. Baseline and post-tests were used to characterize participants and examine associations between dose/intensity and depression scores. Participant satisfaction and perceived benefits were examined at 8 months.
Results:
Of 208 participants, 181 (87%, mean age = 69.6) had treatment data. Of these, 165 (91.2%) had ≥3 treatment sessions (minimal dose). Participants had on average 8.1 sessions (SD = 2.6) for an average of 65.4min (SD = 18.3) each. Behavioral activation and care management were provided the most (average of six sessions for average duration = 17.9 and 22.2min per session respectively), although all participants received each treatment component. GBGB was perceived as highly acceptable and beneficial by interventionists and participants. More sessions and time in program were associated with greater symptom reduction.
Implications:
GBGB treatment components were highly acceptable to participants. Future implementation and sustainability challenges include staffing, training requirements, reimbursement limitations, competing agency programmatic priorities, and generalizability to other groups.
Keywords: Treatment implementation, Depression care, Home care, Behavioral activation
Depressive disorders are highly prevalent and debilitating conditions in later life (Cuijpers, Beekman, & Reynolds, 2012). Even mild symptomatology has profound effects on quality of life and health (Areán, 2006; Glaser, Robles, Sheridan, Malarkey, & Kiecolt-Glaser, 2003; Lyness, Chapman, McGriff, Drayer, & Duberstein, 2009). Left untreated, depressive symptoms increase dementia risk, comorbidities, functional decline, and mortality (Cuijpers et al., 2012; Glaser et al., 2003; Lenze et al., 2001; Saczynski, Beiser, Seshadri, Auerbach, Wolf, & Au 2010). Although primary care is the main setting for depression detection and treatment, older adults, and particularly African Americans, are underdiagnosed and undertreated in that setting (Areán & Unützer, 2003; Tai-Seale, Mcguire, Colenda, Rosen, & Cook, 2007). This may be due to fiscal and time constraints on the part of health providers and cultural mistrust, and preference of patients for nonpharmacologic treatments requiring more time, knowledge, and skills than physician practices possess (Gitlin, Chernett, Dennis, & Hauck, 2012). As such, developing, testing, implementing, and replicating novel nonpharmacological approaches remains a public health priority (Bartels & Naslund, 2013; Alexopoulos & Bruce, 2009; Callahan & Hendrie, 2010) particularly for older African Americans (Jimenez, Bartels, Cardenas, Dhaliwal, & Alegría, 2012).
Recent studies show that a wide range of home and community-based nonpharmacological interventions (e.g., yoga, exercise, problem-solving) are effective in reducing depressive symptoms in older adults (Gitlin, 2014). These programs tend to focus on the “here and now” and seek to ameliorate immediate stress and/or modifiable factors in people’s living environments that impinge on mood. Few tested programs however, target African Americans, report delivery characteristics or examine the extent to which participants find the intervention acceptable (Casado et al., 2008; Fuentes, & Aranda, 2012). Specifying delivery characteristics such as dose (number of sessions attended) and intensity (time in treatment) and level of receptivity to treatment by participants can inform the replication potential of proven interventions and overcome the “black box” of implementation or the unknowns associated with how programs are provided (Hodgson & Gitlin, in press). Examining delivery characteristics of a proven intervention also provides an indication of treatment fidelity or whether an intervention was delivered as intended (Gitlin & Parisi, in press; Washington et al., 2014).
This study describes the delivery characteristics and acceptability of a home-based depression treatment program, Get Busy Get Better, Helping Older Adults Beat the Blues (GBGB, formerly known as Beat the Blues). GBGB builds upon and extends previously tested approaches (Casado et al., 2008; Ciechanowski, Wagner, & Schmaling, 2004; Quijano et al., 2007). It reflects a collaborative effort between a senior center, serving mostly older African Americans, and a research center. Trial decision making including intervention design and content and study procedures were shared between the two sites with the senior center leading recruitment efforts, screening of potential study participants, and clinical supervision of interventionists.
Senior centers are an underutilized community resource for depression care (detection and treatment). As they serve over 9 million older adults, their capacity for outreach and connectivity to aging individuals, many of whom have limited resources and access to treatment, is unmatched (Dal Santo, 2009). Their partnership in this study provides insight as to their potential critical role in developing, testing, and implementing depression programs.
As reported elsewhere, GBGB was evaluated in a randomized controlled trial with 208 African Americans. At 4 months, compared to a wait-list group, participants in the initial treatment group reported reduced depressive symptoms, anxiety, and functional disability and improved depression knowledge/symptom recognition and behavioral activation levels (ps < .01; Gitlin et al., 2013). Follow-up analyses revealed that all participants (men vs women, individuals with low vs high education and with and without financial strain) benefited similarly (Gitlin et al., 2013, Szanton et al., 2014). Additionally, upon receiving GBGB after the 4-month follow-up, wait-list control group participants showed similar benefits at 8 months as the initial treatment group; and the initial treatment group sustained benefits afforded at 4 to 8 months (Gitlin et al., 2013).
Given these positive outcomes, we sought to understand the delivery of GBGB and participant receptivity and posed four descriptive questions: (a) What was the dose (number of treatment sessions) and intensity (time spent) delivered for GBGB overall and for each of its treatment components? (b) Were participants receptive to each treatment component and engaged in treatment? (c) Were participants satisfied with GBGB and did they perceive it as beneficial? and (d) Was dose and intensity associated with reductions in depression scores?
Our study was guided conceptually by Normalization Process Theory (NPT; Murray, et al., 2010). NPT identifies four factors that can affect replication which should be considered when evaluating the characteristics of an intervention. One factor, “coherence” or “sense-making,” refers to whether interventionists understand and value the intervention such that it is delivered as intended; here we used as an indicator the dose and intensity by which treatment components were delivered (e.g., did all participants receive the intended treatment components?). A second factor, “cognitive participation,” refers to whether participants consider the program a good idea. Here we consider the level of participant engagement in each session as perceived by interventionists as well as participant ratings of their satisfaction with the program. The third factor, “collective work,” or how the program affects agency staff and work flow was not directly evaluated in this study. The fourth consideration, “reflexive monitoring,” refers to how users perceive the program overall. For this we evaluated whether participants perceived benefits to the program and if greater participation was associated with better depression outcomes.
Methods
Study Sample and Procedures
As reported elsewhere (Gitlin, 2014; Gitlin et al., 2013), participants reflected a convenience sample. Recruitment sources included a short-term in-home support program for medically compromised individuals served by the participating senior center, the community at-large using media announcements and presentations at local events and social agencies. The 208 African Americans enrolled in the trial were aged 55 years or older, English speaking, cognitively intact Mini-Mental State Examination (MMSE > 24), and scored ≥5 on the Patient Health Questionnaire (PHQ-9), a measure of depressive symptoms, on two sequential testing occasions over 2 weeks. Individuals with a history of serious mental illness, life-limiting illnesses, enrolled in another depression trial, or living in assisted living or nursing home facilities were ineligible. Antidepressant medication use did not preclude study participation. Those eligible and willing to participate in the trial provided written consent using an approved Institutional Review Board (IRB) form, completed a baseline home interview, were randomized to receive GBGB program immediately (treatment condition) or 4-months later (wait-list control), and were reassessed at 4 and 8 months at home using the same interview battery conducted by assessors masked to participant group allocation.
At 4 months, the wait-list control group received GBGB in its entirety.
Data for this study included three sources. First, following each treatment session, interventionists documented time spent in intervention (dose/intensity), the treatment components implemented and time spent on each, and level of participant engagement. Second, baseline sample characteristics and 4- and 8-month depression severity outcomes were obtained by blinded interviewers. Third, a telephone survey conducted 2 weeks after the final 8-month interview by a staff member not previously involved in the study was conducted to obtain participants’ perceptions of program benefits and satisfaction.
Intervention
GBGB was based upon a broad social ecological and behavioral understanding of depression which suggests that situational factors may provide low levels of positive reinforcement and minimal control, and negatively affect mood. GBGB sought to help individuals break a negative behavior-mood cycle by providing strategies to enhance control over behavior event-contingencies, mitigate negative environmental circumstances (e.g., difficulty traveling to physician’s office, finance strain) infringing on mood and participation in positive activities, identify personal activity goals and achievable steps to accomplish them, and reengage participants in activities that provide positive feedback, reinforcement, and pleasant experiences. Each treatment component supports the other with the overarching goal to help participants become behaviorally activated to break the behavior-mood cycle. There is strong empirical support for activation techniques (Cuijpers, van Straten, & Warmerdam, 2007) with component analyses suggesting that this approach performs equally well with and independent of cognitive therapies (Jacobson et al., 1996).
GBGB was delivered by licensed social workers and involved up to ten 1-hr home sessions over 4 months. Sessions included five treatment components tailored to individual needs: care management, referral and linkage, stress reduction techniques, education in depression knowledge and symptom detection/management, and a simplified behavioral activation strategy (Agarwal, Hamilton, Crandell, & Moore, 2010; Cooper et al., 2003; Hopko, Lejuez, Ruggiero, & Eifert, 2003). Interventionists began by building rapport and conducting a needs assessment followed by enactment of a care plan to address unmet needs and including referrals and linkages. Ongoing education was provided about depression, treatment options, how to talk to doctors and those of a different race or culture about symptoms, how to recognize one’s symptoms, and manage symptoms through activity engagement. Also provided was education about chronic stress and instruction in simple stress reduction techniques such as deep breathing, listening to music or simple counting. Finally, although there are various approaches to behavioral activation (Manos, Kanter, & Busch, 2010), we used a three-step process; interventionists worked with participants to identify their daily routines and activities and associated moods, identify pleasant activities that the participant does or does not do but would like to, and to identify an activity the participant would like to do and the specific steps to achieve it (Quijano et al., 2007). Participants were then encouraged to introduce pleasant activities in their daily routines, to be sensitive to their mood throughout the day, and work towards accomplishing small steps to reach their activity goal. Participants in need of further counseling, psychotherapy, or other depression treatments were also referred to other mental health services.
Sessions were spaced to allow opportunities for participants to follow-up with recommendations, referrals, and enactment of activity goals. We anticipated that care management and behavioral activation would occur in most treatment sessions with the other treatment components being provided more up front (sessions 1–4) and then briefly reinforced in subsequent treatment sessions. We reasoned a priori that a minimum of three sessions were needed to receive minimum exposure to each of the five treatment components.
Of six interventionists, one delivered the intervention to 5 participants, 1 to 9 participants, 1 to 22 participants, 1 to 24 participants, 1 to 57 participants, and 1 to 64 participants. Each interventionist stayed with a participant for duration of the intervention. Fidelity was monitored through audiotaping randomly selected sessions, which were subsequently listened to by the investigative team and rated using investigator-designed monitoring forms, group case presentation sessions and troubleshooting, one-on-one supervision in which documentation was reviewed, and direct observation of randomly selected sessions.
Measures
Basic background characteristics included: age, sex, marital status, number of current health conditions, and financial difficulties (0 = not at all to 3 = very much). The main trial outcome was depression severity as measured by the PHQ-9, a brief, psychometrically sound 9-item self-report measure (Kroenke, Spitzer, & Williams, 2001). A total severity score was calculated by summing responses across nine items rated as occurring not at all (0), several days (1), more than half the days (2), or nearly every day (3). Possible scores ranged from 0 to 27 with higher scores indicating greater severity (Cronbach’s α = .78 for sample).
Dose and Intensity: During and immediately following each session, interventionists documented the delivery of each session including start and stop times, which treatment components were delivered, and amount of time spent on those components delivered. Summary indices were developed as follows: (a) total number of sessions conducted (dose); (b) total time spent in all sessions (intensity); (c) number of sessions in which each treatment component was introduced; and (d) time spent (intensity) on each component across sessions in which it was delivered.
Participant Receptivity to Treatment Components and Overall Engagement: For each treatment component delivered in a session, interventionists recorded their perceptions of participants’ receptivity (0 = not at all to 3 = very much). Summary scores for receptivity of each treatment component were derived that reflected the average score across those sessions in which the component was provided.
Also, interventionists were asked to rate the level of engagement of participants following the completion of each session using four items rated from 0 = not at all to 3 = very much. Items included the extent to which the: participant made interventionist feel welcomed and sought to continue participation; participant demonstrated engagement in session; participant indicated session was useful; and participant’s mood appeared better. The derived engagement index reflected the mean of each item across completed treatment sessions.
Participant Satisfaction and Perceived Benefits: Following the 8-month interview, a brief investigator-developed telephone survey modeled after evaluations used in other trials was conducted (Gitlin, Winter, Dennis, Hodgson, & Hauck, 2010). The survey included two areas: (a) satisfaction with study, consisting of five items (yes/no) and (b) perceived benefits consisting of nine items (1 = not at all to 3 = very much). Each item was examined separately (see Table 3 for items).
Table 3.
Participant Evaluation of Get Busy Get Better Program
| Item | N | Yes % (N) |
No % (N) |
||
|---|---|---|---|---|---|
| A. Satisfaction with Study | |||||
| 1. Was program clearly explained to you from the time we first contacted you? | 151 | 99.3% (150) | 0.7% (1) | ||
| 2. Do you feel that you were treated with proper respect during the course of this program? | 151 | 100.0% (151) | 0.0% (0) | ||
| 3. Did the social worker help develop activities that were important to you? | 151 | 85.4% (129) | 14.6% (22) | ||
| 4. Did the program require too much work or effort? | 151 | 4.0% (6) | 96.0% (145) | ||
| 5. Would you recommend this program to others in similar situations? | 150 | 96.0% (144) | 4.0% (6) | ||
| Item | N | Not at all | Some | A great deal |
|---|---|---|---|---|
| B. Perceived Benefits | ||||
| 1. Overall, how much do you think you benefited from participation in this program? | 150 | 0.7% (1) | 26.0% (39) | 73.3% (110) |
| 2. How much did participation in the program help you better understand feelings of sadness or distress you may have been experiencing? | 150 | 2.7% (4) | 33.3% (50) | 64% (96) |
| 3. How much did participation in the program help you better understand what you can do when you have feelings of sadness or distress? | 150 | 4.0% (6) | 30.7% (46) | 65.3% (98) |
| 4. How much did participation in this program help you feel more confident in dealing with your feelings of sadness or distress? | 151 | 5.3% (8) | 37.1% (56) | 58.0% (87) |
| 5. How much did participation in the program help make connections for you with community resources to help with concerns such as transportation, housing, and finances? | 151 | 23.8% (36) | 43.1% (65) | 33.1% (50) |
| 6. How much did participation in the program enhance your ability to discuss feelings of sadness or distress with your doctor or therapist or counselor? | 151 | 9.9% (15) | 36.4% (55) | 53.6% (81) |
| 7. How much did participation in the program help manage feelings of stress? | 151 | 6.6% (10) | 43.7% (66) | 49.7% (75) |
| 8. How much did participation in the program help you identify activities to improve your mood? | 151 | 8.0% (12) | 38.4% (58) | 53.6% (81) |
| 9. How helpful were those activities in improving your mood? | 129 | 3.9% (5) | 30.2% (39) | 65.9% (85) |
Note: Values are % (n).
Statistical Analyses
Descriptive data included sociodemographic characteristics, dose and intensity, participant receptivity and engagement level, and participant satisfaction and perceived benefit.
Summary statistics were presented as means (SD) and as frequencies for categorical data.
Initial treatment and wait-list control group participant’s characteristics were compared using chi-square for categorical variables and t tests for continuous variables. Exploratory analyses were performed to evaluate whether greater exposure to treatment (e.g., more sessions and time spent in intervention) were associated with lower depressive symptoms scores at follow-up. Separate fixed-effects models with change in PHQ-9 score (baseline minus 4-month PHQ-9 scores for initial treatment group; 4-month minus 8-month PHQ-9 scores for wait-list control group) as the dependent variable and either number of sessions or total time in intervention as the independent variable were fit. Statistical significance was based on a value of p < .05.
Results
Sample Characteristics
Of 208 study participants, documentation of treatment sessions by interventionists was available for 181 (87.0%). A comparison of those with treatment data and those without (n = 27) revealed no differences except for one: more men had less treatment data available (22%) than women (10%; χ2 = 4.3, p = .037). Missing documentation was due to loss-to-follow-up.
Participants were on average 69.6 (SD = 8.8) years old. Most were female (80.7%), not married (86.7%), not working (90.6%), and indicated financial strain (65.8%). Participants had an average of 6.4 health conditions and scored in the moderate range of depressive symptomatology (mean = 13.0, SD = 4.9). Less than a third were on antidepressant (n = 38, 21.1%) or anti-anxiety (n = 32, 17.9%) medications. There were no statistically significant differences at baseline between initial treatment and wait-list control groups on background characteristics except for living arrangement. More control group participants lived alone than in the treatment group. (Table 1)
Table 1.
Baseline Characteristics of Study Participants With Delivery Treatment Data (N = 181)
| Demographics | Control (n = 82) | Treatment (n = 99) | Total (N = 181) | Min–Max | χ 2 | t | p |
|---|---|---|---|---|---|---|---|
| Gender (%) | 0.1048 | .746 | |||||
| Male | 15 (18.3) | 20 (20.2) | 35 (19.3) | ||||
| Female | 67 (81.7) | 79 (79.8) | 146 (80.7) | ||||
| Age (M, SD)a | 70.1 (8.8) | 69.3 (8.9) | 69.6 (8.8) | 55.6–96.1 | 0.60 | .550 | |
| Financial difficulty (%) | 5.7809 | .123 | |||||
| Not difficult at all | 23 (28.1) | 15 (15.2) | 38 (21.0) | ||||
| Not very difficult | 9 (11.0) | 15 (15.2) | 24 (13.3) | ||||
| Somewhat difficult | 31 (37.8) | 36 (36.4) | 67 (37.0) | ||||
| Very difficult | 19 (23.2) | 33 (33.3) | 52 (28.7) | ||||
| Employment status (%) | 5.7916 | .016 | |||||
| Unemployed | 79 (96.3) | 85 (85.9) | 164 (90.6) | ||||
| Employed | 3 (3.7) | 14 (14.1) | 17 (9.4) | ||||
| a N = 180 | |||||||
| Marital status (%) | 1.6000 | .206 | |||||
| Not married | 74 (90.2) | 83 (83.8) | 157 (86.7) | ||||
| Married/living as married | 8 (9.8) | 16 (16.2) | 24 (13.3) | ||||
| Education (%) | 2.2256 | .329 | |||||
| <HS | 17 (20.7) | 19 (19.2) | 36 (19.9) | ||||
| HS | 28 (34.2) | 25 (25.3) | 53 (29.3) | ||||
| >HS | 37 (45.1) | 55 (55.6) | 92 (50.8) | ||||
| Living arrangement (%) | 9.7151 | .002 | |||||
| Alone | 57 (69.5) | 46 (46.5) | 103 (56.9) | ||||
| With others | 25 (30.5) | 53 (53.5) | 78 (43.1) | ||||
| Recruitment source (%)a | 0.5502 | .458 | |||||
| IHSP | 21 (25.6) | 30 (30.6) | 51 (28.3) | ||||
| Other | 61 (74.4) | 68 (69.4) | 129 (71.7) | ||||
| Number of health conditions (M, SD) | 6.4 (3.2) | 6.4 (2.8) | 6.4 (3.0) | 0–19 | 0.04 | .971 | |
| Medications (%) | |||||||
| Depression medicationa | 15 (18.5) | 23 (23.2) | 38 (21.1) | 0.5944 | .441 | ||
| Anxiety medicationb | 14 (17.3) | 18 (18.4) | 32 (17.9) | 0.0355 | .851 | ||
| Depression level (PHQ-9; %) | 0.9397 | .815 | |||||
| Minimal/no depression (0–4) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||||
| Mild depression (5–9) | 24 (29.3) | 29 (29.3) | 53 (29.3) | ||||
| Moderate depression (10–14) | 29 (35.4) | 34 (34.3) | 63 (34.8) | ||||
| Moderately severe depression (15–19) | 21 (25.6) | 22 (22.2) | 43 (23.8) | ||||
| Severe depression (≥20) | 8 (9.8) | 14 (14.1) | 22 (12.2) | ||||
| PHQ-9 (M, SD) | 12.8 (4.7) | 13.1 (5.1) | 13.0 (5.0) | 5–25 | -0.41 | .683 |
Note: PHQ = Patient Health Questionnaire.
a N = 180.
b N = 179.
Dose and Intensity for Intervention Overall and Treatment Components
Of 181 participants, 91.2% (n = 165) had three or more treatment sessions (e.g, .8% (n = 16) had less than 3 sessions. Participants had on average 8.1 sessions (SD = 2.6) for an average of 65.4min (SD = 18.3) each. Behavioral activation and care management were provided in an average of six sessions at an average duration of 17.9 and 22.2min per session respectively. Stress reduction and depression education/symptom recognition were provided in an average of four sessions for an average of 7.34 and 6.18min per session respectively; lastly, referral and linkage was provided in an average of three sessions, for an average of 5.41min (Table 2).
Table 2.
Number of Sessions, Time in Minutes per Treatment Component and Receptivity
| Treatment component | Mean no. of sessions (SD) | Mean time in minutes (SD) | Mean receptivity (SD) |
|---|---|---|---|
| Care management | 5.75 (3.13) | 22.19 (14.61) | 2.36 (0.51) |
| Referral and linkage | 3.43 (2.19) | 5.41 (4.83) | 1.99 (0.79) |
| Stress reduction | 4.27 (2.87) | 7.34 (4.10) | 2.19 (0.66) |
| Behavioral activation | 6.25 (3.07) | 17.90 (7.66) | 2.25 (0.57) |
| Depression education | 3.74 (2.42) | 6.18 (3.43) | 2.03 (0.71) |
Note: N for mean number of sessions is 181 for all treatment components. For mean time in minutes per session, N = 180 for Care Management and Depression Education, N = 174 for Referral and Linkage and Behavioral Activation, and N = 164 for Stress Reduction. Mean time in minutes per session was calculated based on subjects with at least one session in the respective component.
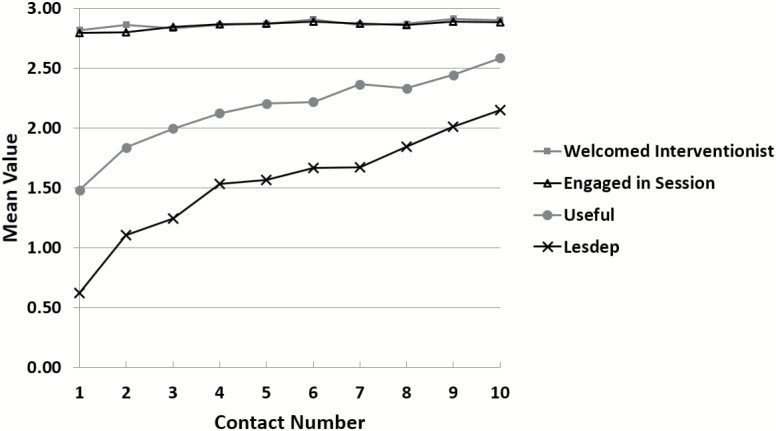
Figure 1 shows the percentage of participants who received a given treatment component at any one session. All components were introduced for most participants in session one with behavioral activation and care management occurring for most participants in subsequent sessions, with a slight decline in the inclusion of the other three components each subsequent session as was anticipated in the design of GBGB. Each treatment component was provided to at least a quarter of the sample at any one session suggesting that although all participants received each component, their delivery in each session unfolded slightly differently based on participant need as was intended.
Figure 1.
Percent of participants receiving a given treatment component by session number. Note: CM = care management; SR = stress reduction; RL = referral and linkage; Deped = depression education/symptom reduction; BA = behavioral activation.
Participant Receptivity to Treatment Components and Overall Engagement
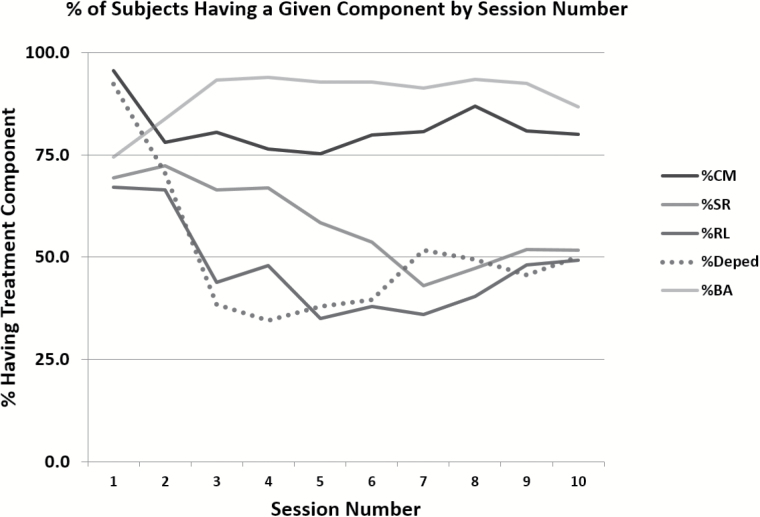
Each treatment component was rated by interventionists to be on average moderately to very well received by participants (Table 2). Interventionists also perceived that participants made them feel very welcomed and were very engaged in each treatment session. With each subsequent session, interventionists perceived that participants moved from viewing treatment sessions from “a little” to “moderately” useful. Similarly, on each subsequent session, interventionists viewed participants’ mood as improving (Figure 2).
Figure 2.
Mean values of participant engagement rated by interventionists for each treatment session (N = 181). Note: Session 1, N = 180 except for less depressed item in which N = 174; Session 2, N = 173 except for less depressed item in which N = 172; Session 3, N = 164; Session 4, N = 147 except for useful and depression item in which N = 148; Session 5, N = 138; Session 6, N = 125; Session 7, N = 115; Session 8, N = 91; Session 9, N = 79; and Session 10, N = 60.
Participant Satisfaction and Perceived Benefits
All participants believed they were treated respectfully in the study; all but one (99.3%) believed the study was clearly explained; 96.6% believed the study did not require too much work or effort, 96.0% would recommend GBGB to others in a similar situation; and 85.4% indicated the interventionist helped to identify meaningful activities, indicators of high program satisfaction.
Most participants expressed the highest level (“a great deal”) of benefit from the program (73.3%), as well as for obtaining a better understanding of depression (64.0%), better understanding of what to do when distressed (65.3%), confidence managing distress (58.0%), better ability to discuss feelings of sadness with health professionals (53.6%), better management of stress (49.7%), better ability to identify activities to improve mood (53.6%), and that those activities resulted in improved mood (65.9%). Referral and linkage appeared to be the weakest enacted treatment component such that only 33.1% indicated that GBGB helped them make connections with needed community resources “a great deal” (Table 3).
Relationship of Dose and Intensity to Depression Outcomes
We also examined the relationship between the number of sessions and time spent in intervention to depression scores (4 months for initial treatment group, 8 months for wait-list control group). Change in PHQ-9 as a function of the number of sessions (dose) was −0.41 units per session (95% CI of −0.75 to −0.06), with t = −2.33 (p = .021). This suggests that each completed session resulted in an estimated effect of decreasing a participant’s PHQ-9 score by about 0.4 points. Change in PHQ-9 score as a function of total hours (intensity) was −0.31 units per hour (95% CI of −0.57 to −0.06), with t = −2.43 (p = .016). This suggests that for each added hour of treatment, there was an estimated mean decrease in PHQ-9 score of about 0.3 points. These are consistent with session length targeted for about 1hr.
Discussion
This study continues to build evidence for GBGB and its implementation potential. GBGB provided care management and referrals and linkages to address modifiable situational stressors, training in stress reduction techniques to manage state anxiety, knowledge about depression and how to recognize symptoms, and activation strategies to reengage in self-identified activity goals and modulate mood.
Findings suggest high implementation potential using NPT indicators. As to “coherence,” participants received each treatment component with greater dose and intensity devoted to care management and behavioral activation as intended. As the average number of sessions were eight of 10, it is possible that GBGB could be shortened, saving costs without compromising outcomes. The average number of sessions and time spent for each treatment component in this study also provides guidance for future implementation. For example, an average of four of 10 sessions included stress reduction with each session averaging only 7 min to this component.
“Cognitive participation” also appeared to be strong: interventionists reported participants welcomed them, an indicator of obtaining a positive therapeutic alliance, and that participant engagement levels increased each subsequent session. Furthermore, participants reported high satisfaction with the program overall.
As to “reflexive monitoring,” most participants reported a great deal of benefit from each of the five treatment components, except for referral and linkage with only about a third finding it helpful. Finally, exploratory analyses revealed that more exposure to treatment was associated with better depression outcomes; that is, more sessions and time spent in intervention were associated with greater reductions in depression severity.
Testimonies from study participants further demonstrated that participants were able to clearly articulate derived benefits and also link benefits to specific program components. For example, Mr. L (age 80) indicated “I never realized I was depressed and learned a great deal about depression. I have a new outlook on life and think more positively about things,” reflecting the value to him of the depression education and symptom recognition component of the intervention. Ms. J (age 61) stated, “You not only helped me to recognize that I had symptoms of depression and that having those feelings was a problem, but how to get myself out of it,” reflecting the value of the behavioral activation component. Mr. B (age 75) indicated, “I have a positive outlook for the future, have become more active, and my self-esteem has improved,” highlighting the multiple benefits derived from the program.
Taken together, these findings suggest that GBGB has high implementation potential: it was delivered as intended, highly acceptable, and perceived as beneficial as observed by interventionists and reported by participants.
Why is GBGB acceptable to study participants? Acceptability may have been enhanced by participation of the senior center in both screening on-site and delivery of GBGB in homes. The senior center is a highly trusted community-based agency providing services to over 6,000 individuals, most of whom are African American. Another reason may be that sessions occurred in homes. Although adding cost, this may minimize stigma, reduce challenges including transportation to clinical settings, and enhance willingness to participate (Pizzi et al., 2014). A survey of 153 older African Americans (25% with depression) found that 74.8% endorsed the home as a preferred setting for mental health services although most also endorsed physician and therapist offices as well (Gitlin, Chernett, Dennis, & Hauck, 2012). It also cannot be discounted that our approach was well received due to factors that were not measured. For example, a strong therapeutic alliance, active listening, acknowledgement of a person’s challenges, and providing hope could also have been active ingredients as in other therapeutic programs (Marmar, Gaston, Gallagher, & Thompson, 1989).
As no studies to our knowledge have reported delivery characteristics for home-based depression programs targeting African Americans (Gitlin, 2014), it is not possible to compare our findings to others. In Healthy IDEAS, the primary intervention informing GBGB, only 19 (20%) of 94 participants were African American and a different delivery approach was used. Case managers screened for depression and then offered the 94 cases with symptoms different treatment elements based on their need and willingness to participate. Of the 94, 81 (86.2%) received depression education, 53 (56.4%) received referrals and linkages and 42 (44.7%) received behavioral activation (Casado et al., 2008). Those who chose to participate reported reduced depressive symptoms; however, Healthy IDEAS was not tested in a clinical trial (Quijano et al., 2007). Also, case managers reported many clients’ refused to engage in the intervention overall and in its different treatment components as evidenced by the varying levels of participation. This was especially the case for African American participants (Casado et al., 2008). In contrast, as shown in this study, all participants were exposed to all treatment components including behavioral activation and were moderately to highly receptive to each. We attribute the high level of participation in part to the senior center’s participation as a full study partner. Also, we separated screening activities, conducted by the senior center’s case managers, from treatment delivery activities, conducted by mental health professionals who were comfortable with and had the skills to deliver each treatment component.
A few study limitations should be noted. Interventionists rated participant engagement levels without independent confirmation of their ratings. As they were aware of the importance of keeping participants engaged and developing a positive therapeutic alliance, their ratings may be biased. Nevertheless, obtaining the interventionists’ perspective is one important source of insight as to how participants engaged. Also, as the PHQ-9 was administered at pre- and post-testing, only simple modeling was possible to detect a general linear trend between dose and intensity and depression outcomes. We were unable to determine at which session or time point improvements stopped occurring.
Implementation and Sustainability
Building the capacity of senior center staff nationally to systematically assess and then offer treatments such as GBGB in the homes of those they serve could have important benefits both for staff, by improving their knowledge and skills, and the community, by addressing unmet mental health needs. As supporting positive mental health is the expressed mission of senior centers, GBGB squarely fits within their mission.
Nevertheless, financial viability, sustainability, and staff training needs present as significant challenges for implementing and sustaining GBGB in senior centers or other community-based agencies. As there are no clear payment mechanisms to support the delivery of GBGB, rebudgeting of already tight budgets and the need to establish new work flows with possibly more skilled staff than senior centers have available, may make the program out-of-reach for some community-based centers. How the program affects the work of agency staff, the NPT factor of “collective work” that we did not evaluate in this study, needs careful consideration in this regard. As most senior centers or community-based agencies do not currently have capacity to engage in depression care, GBGB would require a modification of work practices and flow. Changes might need to include the establishment of screening, referral, and follow-up mechanisms and procedures, and protocols for handling suicidal ideation and major depression. Mechanisms for providing ongoing and booster staff training of case managers and intake coordinators would be critical to assure sustainability of depression detection and referral to the home program.
Although we tested GBGB with interventionists who were master’s degree social workers, with the right supervisory structure, we believe the program could be delivered by other health professionals such as nurses, occupational therapists, counselors, psychologists, or public health educators who may (or may not) be more available to senior centers.
Also, although we tested GBGB in the home, it may be possible to provide some if not all sessions on-site at a senior center. This would reduce the need to travel and associated costs, which represent the most costly aspect of its delivery (Pizzi et al., 2014). Nevertheless, assuring participant receptivity to engaging in some or all sessions on-site at a senior center or community agency needs careful evaluation. In the survey of 153 African Americans discussed earlier, less than half (48.3%) indicated they would favor receiving depression care on-site in a senior center.
As senior centers address a wide range of needs of older adults and tend to offer varied programs, attending to depression detection and treatment in a focused, skilled, and evidentiary-based approach may compete with other priorities and programmatic needs of the communities served. Such competing demands without a funding stream for depression care threaten the implementation potential of GBGB.
As to funding support for this approach, the Mental Health Parity Act of 2008 requires insurers to apply benefits to cover mental health disorders similar to other medical benefits. However, most senior centers and community-based agencies are not set up to participate in the delivery of Medicare-supported services. Partnering with Accountable Care Organizations may provide a unique opportunity for long-term viability of its delivery to a growing aging population that remains undertreated and underserved in mental health care.
Yet another challenge for sustainability concerns referral. As depression care (detection and treatment) chiefly resides in primary care, the integration of community-based agencies in mental health care is challenging. The U.S. health care system lacks an adequate infrastructure to support referrals and payment for nonpharmacological depression care (Bodenheimer, 2008).
Finally, although GBGB was tested using clinical trial methodology, evaluations with larger numbers and older adults from other race and ethnic groups would be important to widen its potential reach, impact and generalizability to other populations. The GBGB approach may resonate with other populations and for those in which cognitive and problem-solving therapies may not be as effective or preferred. There are also unknowns that would be important to address in future research; it is not clear whether participants need booster sessions after eight months and whether activation is continued independently and if so, for how long.
In conclusion, GBGB offers senior centers and other community agencies a promising nonpharmacological approach that appeals to and benefits older African Americans and which has been rigorously evaluated. While replication with other communities and diverse race/ethnic groups is important, the evidence to date supports moving forward with integrating its delivery by community-based agencies and solving its implementation and sustainability challenges.
Acknowledgments
The study reported in this manuscript was supported by the National Institute of Mental Health (RO1 MH079814). Clinicaltrials.gov: NCT00511680. Get Busy Get Better: Helping Older Adults Beat the Blues, was formerly referred to as Beat the Blues. We would like to acknowledge Nancy Wilson, MSW, for her consultation on this study.
References
- Agarwal M. Hamilton J. B. Crandell J. L., & Moore C. E (2010). Coping strategies of African American head and neck cancer survivors. Journal of Psychosocial Oncology, 28, 526–538. doi:10.1080/07347332.2010.498456 [DOI] [PubMed] [Google Scholar]
- Alexopoulos G. S., & Bruce M. L (2009). A model for intervention research in late-life depression. International Journal of Geriatric Psychiatry, 24, 1325–1334. doi:10.1002/gps.2287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Areán P. A. (2006). One in 10 elderly people with minor or subsyndromal depression develops major depression within a year. Evidence Based Mental Health, 9, 94–94. http://dx.doi.org/10.1136/ebmh.9.4.94 [DOI] [PubMed] [Google Scholar]
- Areán P. A., & Unützer J (2003). Inequities in depression management in low-income, minority, and old-old adults: a matter of access to preferred treatments? Journal of the American Geriatrics Society, 51, 1808–1809. doi:10.1046/j.1532-5415.2003.51569.x [DOI] [PubMed] [Google Scholar]
- Bartels S. J., & Naslund J. A (2013). The underside of the silver tsunami — Older adults and mental health care. New England Journal of Medicine, 368, 493–496. doi:10.1056/NEJMp1211456 [DOI] [PubMed] [Google Scholar]
- Bodenheimer T. (2008). Coordinating care — A perilous journey through the health care system. New England Journal of Medicine, 358, 1064–1071. doi:10.1056/NEJMhpr0706165 [DOI] [PubMed] [Google Scholar]
- Callahan C. M., & Hendrie H. C (2010). Mental health services research: moving from academia to the community. American Journal of Geriatric Psychiatry, 18, 460–463. doi:10.1097/JGP.0b013e3181db6d9a [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casado B. L. Quijano L. M. Stanley M. A. Cully J. A. Steinberg E. H., & Wilson N. L (2008). Healthy IDEAS: Implementation of a depression program through community-based case management. The Gerontologist, 48, 828–838. doi:10.1093/geront/48.6.828 [DOI] [PubMed] [Google Scholar]
- Ciechanowski P. Wagner E., & Schmaling K (2004). Community-integrated home-based depression treatment in older adults: A randomized controlled trial. JAMA: The Journal of the American Medical Association, 291, 1569–1577. doi:10.1001/jama.291.13.1569 [DOI] [PubMed] [Google Scholar]
- Cooper L. A. Gonzales J. J. Gallo J. J. Rost K. M. Meredith L. S. Rubenstein L. V., … Ford D. E (2003). The acceptability of treatment for depression among African-American, Hispanic, and White primary care patients. Medical Care, 41, 479–489. doi:10.1097/01.MLR.0000053228.58042.E4 [DOI] [PubMed] [Google Scholar]
- Cuijpers P. Beekman A. T., & Reynolds C. F. III (2012). Preventing depression: A global priority. Journal of the American Medical Association, 307, 1033–1034. doi:10.1001/jama.2012.271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P. van Straten A., & Warmerdam L (2007). Behavioral activation treatments of depression: A meta-analysis. Clinical Psychology Review, 27, 318−326. doi:10.1016/j.cpr.2006.11.001 [DOI] [PubMed] [Google Scholar]
- Dal Santo T. S., & California Commission on Aging. (2009). Senior center literature review: Reflecting & responding to community needs. Sacramento, CA: California Commission on Aging. [Google Scholar]
- Fuentes D., & Aranda M. P (2012). Depression interventions among racial and ethnic minority older adults: A systematic review across 20 years Retrieved from http://readinglists.lib.monash.edu/items/81D2CB0F-9DCC-2BC4-7F4E-5E65FFB74D02.html
- Gitlin L. N. (2014). The role of community and home-based interventions in late life depression. In Richards C. S., & O’Hara M. W. (Eds.). The Oxford handbook of depression and comorbidity (pp. 511–527). London: Oxford University Press; doi:10.1093/oxfordhb/9780199797004.013.035 [Google Scholar]
- Gitlin L. N. Chernett N. L. Dennis M. P., & Hauck W. W (2012). Identification of and beliefs about depressive symptoms and preferred treatment approaches among community-living older African Americans. The American Journal of Geriatric Psychiatry, 20, 973–984. doi:10.1097/JGP.0b013e31825463ce [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gitlin L. N. Harris L. F. Mccoy M. C. Chernett N. L. Pizzi L. T. Jutkowitz E., … Hauck W. W (2013). A home-based intervention to reduce depressive symptoms and improve quality of life in older African Americans. Annals of Internal Medicine, 159, 243. doi:10.7326/0003-4819-159-4-201308200-00005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gitlin L. N., & Parisi J. M (in press, projected publication date, 2016). Are treatment effects real? The role of fidelity. In Gitlin L. N., & Czaja S. J. (Eds.), Behavioral intervention research: Designing, evaluating and implementing. New York: Springer. [Google Scholar]
- Gitlin L. N. Winter L. Dennis M. P. Hodgson N., & Hauck W. W (2010). A biobehavioral home-based intervention and the well-being of patients with dementia and their caregivers: The COPE randomized trial. The Journal of the American Medical Association, 304, 983–991. doi:10.1001/jama.2010.1253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glaser R. Robles T. F. Sheridan J. Malarkey W. B., & Kiecolt-Glaser J. K (2003). Mild depressive symptoms are associated with amplified and prolonged inflammatory responses after influenza virus vaccination in older adults. Archives of General Psychiatry, 60, 1009–1014. doi:10.1001/archpsyc.60.10.1009 [DOI] [PubMed] [Google Scholar]
- Hodgson N. A., & Gitlin L. N, (in press, projected publication date 2016). The role of implementation science in behavioral intervention research. In Gitlin L. N., & Czaja S. J. (Eds.), Behavioral intervention research: designing, evaluating and implementing. New York: Springer Publishers. [Google Scholar]
- Hopko D. R. Lejuez C. W. Ruggiero K. J., & Eifert G. H (2003). Contemporary behavioral activation treatments for depression: Procedures, principles, and progress. Clinical Psychology Review, 23, 699–717. doi:10.1016/S0272-7358(03)00070-9 [DOI] [PubMed] [Google Scholar]
- Jimenez D. E. Bartels S. J. Cardenas V. Dhaliwal S. S., & Alegría M (2012). Cultural beliefs and mental health treatment preferences of ethnically diverse older adult consumers in primary care. American Journal of Geriatric Psychiatry, 20, 532–542. doi:10.1097/JGP.0b013e318227f876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson N. S., Dobson K. S., Truax P. A., Addis M. E., Koerner K., Gollan J. K., Prince S. E. (1996). A component analysis of cognitive behavioral treatment for depression. Journal of Consulting and Clinical Psychology, 64, 295−304. doi:10.1037/0022-006X.70.2.288 [DOI] [PubMed] [Google Scholar]
- Kroenke K. Spitzer R. L., & Williams J. B (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–613. doi:jgi01114 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenze E. J. Rogers J. C. Martire L. M. Mulsant B. H. Rollman B. L. Dew M. A., … Reynolds C. F. 3rd (2001). The association of late-life depression and anxiety with physical disability: A review of the literature and prospectus for future research. American Journal of Geriatric Psychiatry, 9, 113–135. doi:10.1097/00019442-200105000-00004 [PubMed] [Google Scholar]
- Manos R. C. Kanter J. W., & Busch A. M (2010). A critical review of assessment strategies to measure the behavioral activation model of depression. Clinical Psychology Review, 30, 547–561. doi:10.1016/j.cpr.2010.03.008 [DOI] [PubMed] [Google Scholar]
- Marmar C. R. Gaston L. Gallagher D., & Thompson L. W (1989). Alliance and outcome in late-life depression. Journal of Nervous and Mental Disease, 177, 464–472. doi:10.1097/00005053-198908000-00003 [DOI] [PubMed] [Google Scholar]
- Lyness J. M. Chapman B. P. McGriff J. Drayer R., & Duberstein P. R (2009). One-year outcomes of minor and subsyndromal depression in older primary care patients. International Psychogeriatrics/IPA, 21, 60–68. doi:10.1017/S1041610208007746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray E. Treweek S. Pope C. MacFarlane A. Ballini L. Dowrick C. Finch T., … May C (2010). Normalisation process theory: A framework for developing, evaluating and implementing complex interventions. BMC Medicine, 8, 63. doi:10.1186/1741-7015-8-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pizzi L. T. Jutkowitz E. Frick K. D. Suh D. Prioli K. M., & Gitlin L. N (2014). Cost-effectiveness of a community-integrated home-based depression intervention in older African Americans. Journal of the American Geriatrics Society, 62, 2288–2295. doi:10.1111/jgs.13146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quijano L. M. Stanley M. A. Petersen N. J. Casado B. L. Steinberg E. H. Cully J. A., & Wilson N (2007). Healthy IDEAS: A depression intervention delivered by community-based case managers serving older adults. Journal of Applied Gerontology, 26, 139–156. doi:10.1177/0733464807299354 [Google Scholar]
- Saczynski J. S. Beiser A. Seshadri S. Auerbach S. Wolf P. A., & Au R (2010). Depressive symptoms and risk of dementia: The Framingham Heart Study. Neurology, 75, 35–41. doi:10.1212/WNL.0b013e3181e62138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tai-Seale M. Mcguire T. Colenda C. Rosen D., & Cook M. A (2007). Two-minute mental health care for elderly patients: Inside primary care visits. Journal of the American Geriatrics Society, 55, 1903–1911. doi:10.1111/j.1532-5415.2007.01467.x [DOI] [PubMed] [Google Scholar]
- Washington T. Zimmerman S. Cagle J. Reed D. Cohen L. Beeber A. S., & Gwyther L. P (2014). Fidelity decision making in social and behavioral research: Alternative measures of dose and other considerations. Social Work Research, 38, 154–162. doi:10.1093/swr/svu021 [DOI] [PMC free article] [PubMed] [Google Scholar]