Abstract
Aims
Octogenarians have the highest incidence of heart failure (HF) that is not fully explained by traditional risk factors. We explored whether lack of pneumococcal vaccination is associated with higher risk of incident HF among octogenarians.
Methods and results
In the Cardiovascular Health Study (CHS), 5290 community‐dwelling adults, ≥65 years of age, were free of baseline HF and had data on pneumococcal vaccination. Of these, 851 were octogenarians, of whom, 593 did not receive pneumococcal vaccination. Multivariable‐adjusted hazard ratios (aHR) and 95% confidence intervals (CI) for associations of lack of pneumococcal vaccination with incident HF and other outcomes during 13 years of follow‐up were estimated using Cox regression models, adjusting for demographics and other HF risk factors including influenza vaccination. Octogenarians had a mean (±SD) age of 83 (±3) years; 52% were women and 17% African American. Overall, 258 participants developed HF and 662 died. Lack of pneumococcal vaccination was associated with higher relative risk of incident HF (aHR, 1.37; 95% CI, 1.01–1.85; P = 0.044). There was also higher risk for all‐cause mortality (aHR, 1.23; 95% CI, 1.02–1.49; P = 0.028), which was mostly driven by cardiovascular mortality (aHR, 1.45; 95% CI, 1.06–1.98; P = 0.019). Octogenarians without pneumococcal vaccination had a trend toward higher risk of hospitalization due to pneumonia (aHR, 1.34; 95% CI, 0.99–1.81; P = 0.059). These associations were not observed among those 65–79 years of age.
Conclusions
Among community‐dwelling octogenarians, lack of pneumococcal vaccination was associated with a significantly higher independent risk of incident HF and mortality, and trend for higher pneumonia hospitalization.
Keywords: Octogenarians, Pneumococcal vaccination, Heart failure, Mortality
Introduction
Octogenarians are among the fastest growing segments of the US population, and they also have the highest incidence of heart failure (HF).1, 2, 3 However, traditional risk factors for incident HF do not appear to explain this incidence as their impact appears to attenuate with ageing.4, 5, 6, 7 For example, in the Cardiovascular Health Study (CHS), among those <78 years of age, 18% and 13% of those with and without isolated systolic hypertension (ISH) developed new HF, respectively, which corresponded with a 44% higher relative risk for those with ISH.4 In contrast, among those ≥78 years of age, 24% and 25% of those with and without ISH developed new HF. Similarly, isolated diastolic hypertension was associated with a 33% significantly higher independent risk of incident HF, which was only observed among those <75 years of age.5
Thus, there is a need to identify non‐traditional risk factors for incident HF among the oldest old who have the highest incidence of HF that is not well explained by traditional risk factors. In this context, we conducted an exploratory analysis to determine if lack of pneumococcal vaccination is associated with higher risk of incident HF. Although pneumococcal infection is a major cause of cardiovascular morbidity,8 it has been suggested that pneumococcal vaccination may reduce the risk of cardiovascular events.9, 10 Therefore, in the current study, we examined whether lack of pneumococcal vaccination is associated with higher risk of incident HF in community‐dwelling octogenarians.
Methods
Data source and study participants
We used de‐identified copies of the CHS data obtained from the National Heart, Lung and Blood Institute (NHLBI), which also sponsored the study. The rationale and design of the CHS have been previously reported.11 The CHS is an ongoing, prospective, community‐based epidemiologic study based on 5888 Medicare‐eligible community‐dwelling older adults, aged 65 year and older, from Forsyth County, North Carolina; Sacramento County, California; Washington County, Maryland; and Pittsburgh, Pennsylvania. An initial cohort of 5201 participants was recruited between 1989 and 1990, and a second cohort of 687 African Americans was recruited between 1992 and 1993. Of the 5888 CHS participants, 5795 consent to be included in the public‐use copy of the data. Of these, 240 without data on baseline pneumococcal vaccination and 265 with baseline prevalent HF were excluded. Of the remaining 5290, 851 were 80 years and older and 4439 were 65 to 79 years of age at baseline. Data on pneumococcal vaccination were collected at baseline by asking the questions: ‘Have you ever had a shot to prevent pneumonia (pneumovax)?’12 Additional data on socio‐demographic characteristics, health behaviours, self‐rated health and vaccination history, comorbid conditions, medications, vital signs, markers of inflammation, and other biochemical covariates were collected at baseline and have been previously described in details.11 Missing values for variables were imputed based on values predicted by age, sex, and race.
Outcomes
Primary outcomes for the current analysis were incident HF and all‐cause mortality during 13 years of follow‐up. Incident HF was centrally adjudicated by the CHS Events Committee, which has been well described in literature.13 The process began with self‐reports of physician‐diagnosed HF, which were then confirmed by review of medical records for symptoms, signs, medications, and other evidence of HF.4, 5, 6, 7 The CHS criteria for HF diagnosis have been shown to be more stringent than those used in the Framingham Heart Study.14 Secondary outcomes of interest were cardiovascular and non‐cardiovascular mortality, as well as all‐cause hospitalization and hospitalization due to pneumonia.
Statistical analysis
For descriptive analyses, we used Pearson's χ2 for categorical variables and analysis of variance for continuous variables. Kaplan Meier survival analysis was used to determine the association of pneumococcal vaccination with outcomes during 13 years of follow‐up. Unadjusted and multivariable‐adjusted Cox regression models were used to estimate the association of lack of pneumococcal vaccination with outcomes. All statistical tests were two‐sided, and tests with P‐value <0.05 were considered significant. spss for Windows (Version 18) was used for data analysis. We repeated our analysis in participants 65 to 79 years of age.
Results
Baseline characteristics
Octogenarians had a mean (±SD) age of 83 (±3) years; 52% were female, and 17% were African American. The distribution of baseline characteristics between participants receiving or not receiving pneumococcal vaccination was generally balanced (Table 1). A greater proportion of octogenarians receiving pneumococcal vaccination also received influenza vaccination and had higher prevalence of chronic obstructive pulmonary disease and pneumonia.
Table 1.
Baseline characteristics by pneumococcal vaccination in CHS
| Variables mean (±SD) or n (%) | Age ≥80 years (n = 851) | Age 65–79 years (n = 4439) | ||||
|---|---|---|---|---|---|---|
| Pneumococcal vaccination | P‐value | Pneumococcal vaccination | P‐value | |||
| No (n = 593) | Yes (n = 258) | No (n = 3273) | Yes (n = 1166) | |||
| Age, years | 83 (±3) | 83 (±3) | 0.447 | 71 (±4) | 72 (±3) | <0.001 |
| Female | 298 (50%) | 144 (56%) | 0.136 | 1943 (59%) | 688 (59%) | 0.830 |
| African American | 111 (19%) | 31 (12%) | 0.016 | 521 (16%) | 134 (12%) | <0.001 |
| Married | 300 (51%) | 145 (56%) | 0.132 | 2293 (70%) | 805 (69%) | 0.515 |
| Education college or higher | 252 (43%) | 125 (48%) | 0.108 | 1335 (41%) | 566 (49%) | <0.001 |
| Income ≥$25K | 161 (27%) | 90 (35%) | 0.023 | 1201 (37%) | 519 (45%) | <0.001 |
| Smoke, pack years | 11 (±24) | 14 (±25) | 0.152 | 18 (±27) | 19 (±27) | 0.351 |
| Walk blocks last week | 25 (±40) | 25 (±36) | 0.939 | 41 (±57) | 44 (±57) | 0.212 |
| Body mass index, kg/m2 | 25.5 (±3.9) | 25.7 (±3.8) | 0.596 | 26.8 (±4.0) | 26.5 (±4.1) | 0.046 |
| Instrumental ADL | 0.5 (±0.9) | 0.7 (±1.0) | 0.050 | 0.3 (±0.6) | 0.31 (±0.6) | 0.073 |
| Centers for Epidemiologic Studies Depression (CES‐D) scale score | 5.0 (±4.5) | 5.4 (±4.9) | 0.253 | 4.5 (±4.5) | 4.5 (±4.3) | 0.918 |
| Mini‐Mental State Examination | 25.7 (±3.9) | 26.6 (±3.3) | 0.001 | 27.8 (±2.4) | 28.1 (±2.2) | 0.001 |
| Flu vaccination | 225 (38%) | 201 (78%) | <0.001 | 979 (30%) | 905 (78%) | <0.001 |
| Medical history | ||||||
| Coronary heart diseases | 124 (21%) | 58 (23%) | 0.608 | 506 (16%) | 223 (19%) | 0.004 |
| Acute myocardial infarction | 61 (10%) | 18 (7%) | 0.126 | 240 (7%) | 98 (8%) | 0.236 |
| Hypertension | 409 (69%) | 176 (68%) | 0.827 | 1816 (56%) | 680 (58%) | 0.094 |
| Diabetes | 92 (16%) | 32 (12%) | 0.237 | 515 (16%) | 182 (16%) | 0.916 |
| Stroke | 37 (6%) | 14 (5%) | 0.646 | 99 (3%) | 54 (5%) | 0.010 |
| Atrial fibrillation | 20 (3%) | 11 (4%) | 0.524 | 48 (2%) | 31 (3%) | 0.008 |
| LVH by electrocardiogram | 46 (8%) | 19 (7%) | 0.843 | 122 (4%) | 40 (3%) | 0.642 |
| LV systolic dysfunction | 66 (11%) | 25 (10%) | 0.532 | 214 (7%) | 80 (7%) | 0.704 |
| Left bundle branch block | 73 (12%) | 29 (11%) | 0.659 | 240 (7%) | 101 (9%) | 0.143 |
| COPD | 46 (8%) | 49 (19%) | <0.001 | 329 (10%) | 230 (20%) | 0.094 |
| Pneumonia | 110 (19%) | 97 (38%) | <0.001 | 765 (23%) | 436 (37%) | <0.001 |
| Laboratory data | ||||||
| Serum creatinine, g/dL | 1.09 (±0.4) | 1.04 (±0.4) | 0.093 | 0.9 (±0.4) | 0.9 (±0.5) | 0.902 |
| Serum C‐reactive protein, mg/L | 5.1 (±9.1) | 4.0 (±5.7) | 0.072 | 4.6 (±7.8) | 4.8 (±9.1) | 0.473 |
CHS, Cardiovascular Health Study; ADL, activities of daily living; COPD, chronic obstructive pulmonary disease; LVH, left ventricular hypertrophy.
Incident heart failure
During 13 years of follow‐up, among octogenarians, a non‐receipt of pneumococcal vaccination at baseline was associated with significantly higher risk of incident HF [adjusted hazard ratio (aHR), 1.37; 95% confidence interval (CI), 1.01–1.85; Figure 1 and Table 2). In contrast, among those 65–79 years, a non‐use of pneumococcal vaccination was not associated with incident HF (aHR, 0.88; 95% CI, 0.74–1.04; Table 2).
Figure 1.
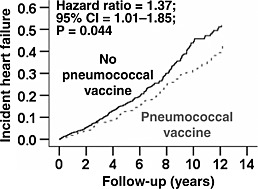
Multivariable‐adjusted risk for incident heart failure among Cardiovascular Health Study participants aged 80 years or older (Hazard ratio when non‐use of pneumococcal vaccination is compared with their use).
Table 2.
Association of lack of pneumococcal vaccination with outcomes in octogenarians in the CHS
| Events (%) | Hazard ratio* (95% confidence interval); P‐value | |||
|---|---|---|---|---|
| Pneumococcal vaccination | ||||
| No (n = 593) | Yes (n = 258) | Unadjusted | Multivariable‐adjusted† | |
| Incident heart failure | 183 (31%) | 75 (29%) | 1.21 (0.92–1.58); P = 0.165 | 1.37 (1.01–1.85); P = 0.044 |
| All‐cause mortality | 474 (80%) | 188 (73%) | 1.29 (1.09–1.53); P = 0.003 | 1.23 (1.02–1.49); P = 0.028 |
| Cardiovascular | 201 (34%) | 68 (26%) | 1.50 (1.14–1.98); P = 0.004 | 1.45 (1.06–1.98); P = 0.019 |
| Non‐cardiovascular | 272 (46%) | 120 (47%) | 1.16 (0.94–1.44); P = 0.168 | 1.10 (0.87–1.40); P = 0.426 |
| All‐cause hospitalization | 530 (89%) | 236 (92%) | 1.01 (0.87–1.18); P = 0.919 | 1.04 (0.87–1.24); P = 0.643 |
| Pneumonia | 184 (31%) | 75 (29%) | 1.20 (0.92–1.57); P = 0.183 | 1.35 (1.00–1.82); P = 0.051 |
CHS, Cardiovascular Health Study.
Hazard ratio, when non‐use of pneumococcal vaccination was compared with their use.
Adjusted for age ≥85 years, sex, race, married, education college or higher, income ≥$25K, smoking ≥32 pack‐years, walk blocks last week ≥10, body mass index ≥25 kg/m2, instrumental activities of daily living ≥1, Centers for Epidemiologic Studies Depression (CES‐D) scale score, Mini‐mental state examination (30 item), influenza vaccination, coronary heart diseases, hypertension, diabetes, stroke, acute myocardial infarction, atrial fibrillation, left ventricular hypertrophy, left ventricular systolic dysfunction, left bundle branch block, chronic kidney disease, chronic obstructive pulmonary disease, pneumonia, serum C‐reactive protein ≥2.4 mg/L.
Mortality
Compared with octogenarians who received pneumococcal vaccination, non‐receipt of pneumococcal vaccination was associated with significantly higher risk of all‐cause mortality (aHR, 1.23; 95% CI, 1.02–1.49), CV mortality (aHR, 1.45; 95% CI, 1.06–1.98), but not of non‐CV mortality (aHR, 1.10; 95% CI, 0.87–1.40; Table 2). Pneumococcal vaccination had no association with mortality among those 65–79 years of age (Table 3).
Table 3.
Association of lack of pneumococcal vaccination with outcomes in those 65–79 years of age in the CHS
| Events (%) | Hazard ratio* (95% confidence interval); P‐value | |||
|---|---|---|---|---|
| Pneumococcal vaccination | ||||
| No (n = 3273) | Yes (n = 1166) | Unadjusted | Multivariable‐adjusted† | |
| Incident heart failure | 568 (17%) | 247 (21%) | 0.78 (0.67–0.91); P = 0.001 | 0.88 (0.74–1.04); P = 0.126 |
| All‐cause mortality | 1182 (36%) | 468 (40%) | 0.87 (0.78–0.97); P = 0.009 | 0.96 (0.85–1.08); P = 0.480 |
| Cardiovascular | 485 (15%) | 187 (16%) | 0.89 (0.75–1.06); P = 0.181 | 0.96 (0.79–1.16); P = 0.667 |
| Non‐ cardiovascular | 692 (21%) | 281 (24%) | 0.85 (0.74–0.97); P = 0.017 | 0.95 (0.81–1.10); P = 0.512 |
| All‐cause hospitalization | 2650 (81%) | 994 (85%) | 0.85 (0.79–0.92); P < 0.001 | 0.94 (0.86–1.02); P = 0.111 |
| Pneumonia | 577 (18%) | 246 (21%) | 0.80 (0.69–0.93); P = 0.003 | 0.89 (0.75–1.06); P = 0.182 |
CHS, Cardiovascular Health Study.
Hazard ratio, when non‐use of pneumococcal vaccination was compared with their use.
Adjusted for age ≥70 years, sex, race, married, education college or higher, income ≥$25K, smoking ≥32 pack‐years, walk blocks last week ≥10, body mass index ≥25 kg/m2, instrumental activities of daily living ≥1, Centers for Epidemiologic Studies Depression (CES‐D) scale score, Mini‐mental state examination (30 item), influenza vaccination, coronary heart diseases, hypertension, diabetes, stroke, acute myocardial infarction, atrial fibrillation, left ventricular hypertrophy, left ventricular systolic dysfunction, bundle branch block, advance chronic kidney disease, chronic obstructive pulmonary disease, pneumonia, serum C‐reactive protein ≥2.4 mg/L
Hospitalization
Among octogenarians, non‐receipt of pneumococcal vaccination had no association with all‐cause hospitalization (aHR, 1.04; 95% CI, 0.87–1.40), but there was a trend toward higher risk of hospitalization due to pneumonia (aHR, 1.35; 95% CI, 1.00–1.82; Table 2). None of these associations were significant among those 65–79 years of age(Table 3).
Discussion
Findings from the current study demonstrated that among community‐dwelling octogenarians, the lack of a prior pneumococcal vaccination was associated with higher risk of incident HF and cardiovascular mortality. We also observed that there was a trend toward higher risk of hospitalization due to pneumonia. Lack of pneumococcal vaccination, however, had no association with these outcomes among older adults 65 to 79 years of age. These findings are hypothesis generating and suggest that pneumococcal infections may be a non‐traditional risk factor for incident HF among octogenarians, and that pneumococcal vaccination may lower the risk of HF among octogenarians.
The association of lack of pneumococcal vaccination and higher incident HF is unlikely to be confounded by other major HF risk factors such as prior myocardial infraction, hypertension, diabetes, and left ventricular systolic dysfunction as they were similarly distributed at baseline between octogenarians with and without prior pneumococcal vaccination and we adjusted for those in our multivariable model. They are also unlikely to be explained by chronic obstructive pulmonary disease and pneumonia as fewer octogenarians not receiving pneumococcal vaccination had these conditions, likely explained by the fact that they were potential indications for pneumococcal vaccination.12 Findings from animal studies suggest that human C‐reactive protein (CRP) may protect mice from pneumococcal infection15 and pneumococcal vaccination is often associated with higher CRP levels.16 Octogenarians without a prior pneumococcal vaccination had higher CRP levels, and although adjusted for in our multivariable model, residual bias is possible. Influenza vaccination has been shown to be associated with lower cardiovascular events.17, 18, 19, 20 Octogenarians without pneumococcal vaccination were less likely to receive influenza vaccination. Although this was adjusted for, residual bias is possible. It is also possible that lack of vaccination was a marker of less healthy life style for octogenarians with no prior vaccination, which may have contributed to their poor cardiovascular outcomes. However, there was no difference in other markers of healthy life style such body mass index between the two groups suggesting a healthy life style cannot fully explain our findings.
We used very similar risk‐adjustment models for both octogenarians and those 65–79 years of age. Further, between‐group prevalence of major HF, risk factors were also similar for both octogenarians and those 65–79 years of age. Yet, despite a larger sample size and higher number of events in those 65–79 years of age, pneumococcal vaccination had no association with incident HF or mortality. This may suggest that the associations observed among the octogenarians are due to chance. However, prior studies have reported that pneumococcal vaccination to be associated with better CV outcomes.9, 10 In one study, the use of pneumococcal vaccination was associated with higher risk of CV outcomes among those <65 years of age, while there was no such association among those ≥65 years of age.21, 22 Taken together with the findings from our study, these findings suggest that there might exist a potential age‐related variation in the benefit of pneumococcal vaccination. Oxidized low‐density lipoproteins play an important role in atherogenesis, and antibodies against them may cause regression of atherosclerosis.23, 24 In laboratory animals, pneumococcal vaccination has been shown to decrease atherosclerotic lesion.25 Preliminary findings from human studies suggest that pneumococcal vaccination may induce antibodies against oxidized low‐density lipoproteins.26 Although oxidized low‐density lipoproteins are not known HF risk factors, they have been shown to be associated with other cardiovascular events.27
Pneumococcal disease is common among older adults, specifically among octogenarians,28, 29 and pneumococcal vaccination is recommended for all adults ≥65 years of age.30 Findings from the current study suggest that this vaccination might also lower the risk of HF and CV mortality among octogenarians. Prospective studies of pneumococcal vaccination in octogenarians would be unethical as it would require delaying vaccination until that age. However, if these findings can be replicated in other octogenarian populations, this might provide an inexpensive tool for improving the health and outcomes of the fastest growing segment of the US population. It will also provide additional rationale to increase the utilization of pneumococcal vaccination, which remains low, about 60% among adults ≥65 years of age in 2010.8
Our study has several limitations. As discussed earlier, an important limitation of any observational study is the potential for bias due to unmeasured confounders, and ours is no exception. We had no data on the time of pneumococcal vaccination. The 23‐valent polysaccharide pneumococcal vaccine was licenced in 1977 and has been reimbursed by Medicare since 1981.31, 32 Although utilization of pneumococcal vaccination has improved over the years,8 use was low in 1989 when participants were enrolled in the CHS. Octogenarians are survivors, and the survival bias is likely to be more pronounced among those with prior pneumococcal vaccination. However, despite accumulation of higher proportion of susceptible patients, we observed a lower risk of incident HF and cardiovascular events among these patients. It is possible that some of the octogenarians in the unvaccinated group were vaccinated during follow‐up or that recollection of vaccination was inaccurate resulting in incorrect classification. However, this would be expected to result in regression dilution and underestimation of the true association.33 Finally, because findings of our study are hypothesis‐generating and do not provide mechanistic insights, they need to be interpreted with caution.
Conclusions
Among community‐dwelling octogenarians, lack of pneumococcal vaccination was associated with higher risk for incident HF and CV mortality, with a trend toward higher risk for hospitalization due to pneumonia. However, none of these associations were observed among those 65–79 years of age. If these hypothesis‐generating findings can be replicated in other octogenarian populations, it may provide a tool to lower the risk of HF among octogenarians, the fastest growing segment of the population in developing nations who also has the highest risk of HF.
Conflict of Interest
None declared.
Funding
Dr Ahmed was in part supported by the National Institutes of Health through grants (R01‐HL085561, R01‐HL085561‐S, and R01‐HL097047) from the National Heart, Lung, and Blood Institute.
Acknowledgements
The CHS was conducted and supported by the NHLBI in collaboration with the CHS investigators. This manuscript was prepared using a limited access dataset obtained by the NHLBI and does not necessarily reflect the opinions or views of the CHS Study or the NHLBI.
Ahmed, M. B. , Patel, K. , Fonarow, G. C. , Morgan, C. J. , Butler, J. , Bittner, V. , Kulczycki, A. , Kheirbek, R. E. , Aronow, W. S. , Fletcher, R. D. , Brown, C. J. , and Ahmed, A. (2016) Higher risk for incident heart failure and cardiovascular mortality among community‐dwelling octogenarians without pneumococcal vaccination. ESC Heart Failure, 3: 11–17. doi: 10.1002/ehf2.12056.
References
- 1. Rich MW, Kitzman DW. Heart failure in octogenarians: a fundamentally different disease. Am J Geriatr Cardiol 2000;9(suppl):97–104.11416547 [Google Scholar]
- 2. Gottdiener JS, Arnold AM, Aurigemma GP, Polak JF, Tracy RP, Kitzman DW, Gardin JM, Rutledge JE, Boineau RC. Predictors of congestive heart failure in the elderly: the Cardiovascular Health Study. J Am Coll Cardiol 2000;35:1628–1637. [DOI] [PubMed] [Google Scholar]
- 3. Kannel WB. Incidence and epidemiology of heart failure. Heart Fail Rev 2000;5:167–173. [DOI] [PubMed] [Google Scholar]
- 4. Ekundayo OJ, Allman RM, Sanders PW, Aban I, Love TE, Arnett D, Ahmed A. Isolated systolic hypertension and incident heart failure in older adults: a propensity‐matched study. Hypertension 2009;53:458–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Guichard JL, Desai RV, Ahmed MI, Mujib M, Fonarow GC, Feller MA, Ekundayo OJ, Bittner V, Aban IB, White M, Aronow WS, Love TE, Bakris GL, Zieman SJ, Ahmed A. Isolated diastolic hypotension and incident heart failure in older adults. Hypertension 2011;58:895–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Roy B, Pawar PP, Desai RV, Fonarow GC, Mujib M, Zhang Y, Feller MA, Ovalle F, Aban IB, Love TE, Iskandrian AE, Deedwania P, Ahmed A. A propensity‐matched study of the association of diabetes mellitus with incident heart failure and mortality among community‐dwelling older adults. Am J Cardiol 2011;108:1747–1753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bowling CB, Fonarow GC, Patel K, Zhang Y, Feller MA, Sui X, Blair SN, Alagiakrishnan K, Aban IB, Love TE, Allman RM, Ahmed A. Impairment of activities of daily living and incident heart failure in community‐dwelling older adults. Eur J Heart Fail 2012;14:581–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Centers for Disease Control and Prevention . Adult vaccination coverage—United States, 2010. MMWR Morb Mortal Wkly Rep 2012;61:66–72. [PubMed] [Google Scholar]
- 9. Eurich DT, Johnstone JJ, Minhas‐Sandhu JK, Marrie TJ, Majumdar SR. Pneumococcal vaccination and risk of acute coronary syndromes in patients with pneumonia: population‐based cohort study. Heart 2012;98:1072–1077. [DOI] [PubMed] [Google Scholar]
- 10. Lamontagne F, Garant MP, Carvalho JC, Lanthier L, Smieja M, Pilon D. Pneumococcal vaccination and risk of myocardial infarction. CMAJ 2008;179:773–777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fried LP, Borhani NO, Enright P, Furberg CD, Gardin JM, Kronmal RA, Kuller LH, Manolio TA, Mittelmark MB, Newman A, O'Leary DH, Psaty B, Rautaharju P, Tracy RP, Weiler PG. The Cardiovascular Health Study: design and rationale. Ann Epidemiol 1991;1:263–276. [DOI] [PubMed] [Google Scholar]
- 12. Jones LG, Zhang Y, Ahmed MI, Ekundayo OJ, Akhter S, Sawyer P, Aban I, Sims RV, Ahmed A. Understanding the reasons for the underuse of pneumococcal vaccination by community‐dwelling older African Americans. J Am Geriatr Soc 2010;58:2323–2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ives DG, Fitzpatrick AL, Bild DE, Psaty BM, Kuller LH, Crowley PM, Cruise RG, Theroux S. Surveillance and ascertainment of cardiovascular events. The Cardiovascular Health Study. Ann Epidemiol 1995;5:278–285. [DOI] [PubMed] [Google Scholar]
- 14. Schellenbaum GD, Rea TD, Heckbert SR, Smith NL, Lumley T, Roger VL, Kitzman DW, Taylor HA, Levy D, Psaty BM. Survival associated with two sets of diagnostic criteria for congestive heart failure. Am J Epidemiol 2004;160:628–635. [DOI] [PubMed] [Google Scholar]
- 15. Suresh MV, Singh SK, Ferguson DA, Jr. , Agrawal A. Human C‐reactive protein protects mice from Streptococcus pneumoniae infection without binding to pneumococcal C‐polysaccharide. J Immunol 2007;178:1158–1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Madhi SA, Kohler M, Kuwanda L, Cutland C, Klugman KP. Usefulness of C‐reactive protein to define pneumococcal conjugate vaccine efficacy in the prevention of pneumonia. Pediatr Infect Dis J 2006;25:30–36. [DOI] [PubMed] [Google Scholar]
- 17. Davis MM, Taubert K, Benin AL, Brown DW, Mensah GA, Baddour LM, Dunbar S, Krumholz HM, American Heart Association , American College of Cardiology . Influenza vaccination as secondary prevention for cardiovascular disease: a science advisory from the American Heart Association/ American College of Cardiology. Circulation 2006;114:1549–1553. [DOI] [PubMed] [Google Scholar]
- 18. Davis MM, Taubert K, Benin AL, Brown DW, Mensah GA, Baddour LM, Dunbar S, Krumholz HM, American Heart Association , American College of Cardiology , American Association of Cardiovascular Pulmonary Rehabilitation , American Association of Critical Care Nurses , American Association of Heart Failure Nurses , American Diabetes Association , Association of Black Cardiologists Inc , Heart Failure Society of America , Preventive Cardiovascular Nurses Association , American Academy of Nurse Practitioners , Centers for Disease Control and Prevention, the Advisory Committee on Immunization . Influenza vaccination as secondary prevention for cardiovascular disease: a science advisory from the American Heart Association/American College of Cardiology. J Am Coll Cardiol 2006;48:1498–1502. [DOI] [PubMed] [Google Scholar]
- 19. Phrommintikul A, Kuanprasert S, Wongcharoen W, Kanjanavanit R, Chaiwarith R, Sukonthasarn A. Influenza vaccination reduces cardiovascular events in patients with acute coronary syndrome. Eur Heart J 2011;32:1730–1735. [DOI] [PubMed] [Google Scholar]
- 20. Udell JA, Zawi R, Bhatt DL, Keshtkar‐Jahromi M, Gaughran F, Phrommintikul A, Ciszewski A, Vakili H, Hoffman EB, Farkouh ME, Cannon CP. Association between influenza vaccination and cardiovascular outcomes in high‐risk patients: a meta‐analysis. JAMA 2013;310:1711–1720. [DOI] [PubMed] [Google Scholar]
- 21. Tseng HF, Slezak JM, Quinn VP, Sy LS, Van den Eeden SK, Jacobsen SJ. Pneumococcal vaccination and risk of acute myocardial infarction and stroke in men. JAMA 2010;303:1699–1706. [DOI] [PubMed] [Google Scholar]
- 22. Kaczorowski J. Pneumococcal vaccination and cardiovascular events in men. JAMA 2010;304:742; author reply 743. [DOI] [PubMed] [Google Scholar]
- 23. Schiopu A, Frendeus B, Jansson B, Soderberg I, Ljungcrantz I, Araya Z, Shah PK, Carlsson R, Nilsson J, Fredrikson GN. Recombinant antibodies to an oxidized low‐density lipoprotein epitope induce rapid regression of atherosclerosis in apobec‐1(−/−)/low‐density lipoprotein receptor(−/−) mice. J Am Coll Cardiol 2007;50:2313–2318. [DOI] [PubMed] [Google Scholar]
- 24. Shoenfeld Y, Wu R, Dearing LD, Matsuura E. Are anti‐oxidized low‐density lipoprotein antibodies pathogenic or protective? Circulation 2004;110:2552–2558. [DOI] [PubMed] [Google Scholar]
- 25. Binder CJ, Horkko S, Dewan A, Chang MK, Kieu EP, Goodyear CS, Shaw PX, Palinski W, Witztum JL, Silverman GJ. Pneumococcal vaccination decreases atherosclerotic lesion formation: molecular mimicry between Streptococcus pneumoniae and oxidized LDL. Nat Med 2003;9:736–743. [DOI] [PubMed] [Google Scholar]
- 26. Suthers B, Hansbro P, Thambar S, McEvoy M, Peel R, Attia J. Pneumococcal vaccination may induce anti‐oxidized low‐density lipoprotein antibodies that have potentially protective effects against cardiovascular disease. Vaccine 2012;30:3983–3985. [DOI] [PubMed] [Google Scholar]
- 27. Holvoet P, Mertens A, Verhamme P, Bogaerts K, Beyens G, Verhaeghe R, Collen D, Muls E, Van de Werf F. Circulating oxidized LDL is a useful marker for identifying patients with coronary artery disease. Arterioscler Thromb Vasc Biol 2001;21:844–848. [DOI] [PubMed] [Google Scholar]
- 28. Sims RV, Boyko EJ, Maislin G, Lipsky BA, Schwartz JS. The role of age in susceptibility to pneumococcal infections. Age Ageing 1992;21:357–361. [DOI] [PubMed] [Google Scholar]
- 29. Huang SS, Johnson KM, Ray GT, Wroe P, Lieu TA, Moore MR, Zell ER, Linder JA, Grijalva CG, Metlay JP, Finkelstein JA. Healthcare utilization and cost of pneumococcal disease in the United States. Vaccine 2011;29:3398–3412. [DOI] [PubMed] [Google Scholar]
- 30. Sims RV, Steinmann WC, McConville JH, King LR, Zwick WC, Schwartz JS. The clinical effectiveness of pneumococcal vaccine in the elderly. Ann Intern Med 1988;108:653–657. [DOI] [PubMed] [Google Scholar]
- 31. Hinman AR, Orenstein WA, Rodewald L. Financing immunizations in the United States. Clin Infect Dis 2004;38:1440–1446. [DOI] [PubMed] [Google Scholar]
- 32. Butler JC, Shapiro ED, Carlone GM. Pneumococcal vaccines: history, current status, and future directions. Am J Med 1999;107:69S‐76S. [DOI] [PubMed] [Google Scholar]
- 33. Clarke R, Shipley M, Lewington S, Youngman L, Collins R, Marmot M, Peto R. Underestimation of risk associations due to regression dilution in long‐term follow‐up of prospective studies. Am J Epidemiol 1999;150:341–353. [DOI] [PubMed] [Google Scholar]


