To the Editor—We read with interest the recent article by Clement et al [1]. In this analysis of the veteran clinical case registry, statins were underutilized for primary or secondary prevention in patients living with human immunodeficiency virus (HIV), hepatitis C virus (HCV), and HIV/HCV coinfection. We wondered whether similar patterns of underutilization would be seen in a national clinical registry representing approximately 8% of the US population. Additionally, because the veteran clinical case registry analysis excluded women, we wished to explore gender differences in statin utilization in these cohorts.
We utilized Explorys, a large registry of US patients seen in the inpatient and outpatient settings in participating institutions (26 major healthcare systems, 317 000 providers, 50 million unique lives in 50 states). The database collects data from billing, International Classification of Diseases diagnosis codes, laboratory studies, and procedures, and are then de-identified and standardized [2].
Our cohort included nondeceased adults (aged 40–75 years), with diagnosis of HIV monoinfection, HCV monoinfection, or HIV/HCV coinfection who had active patient records between May 2015 and May 2016. Statin eligibility was defined as belonging to one of three 2013 American College of Cardiology/American Heart Association statin benefit groups: (1) low-density lipoprotein cholesterol >190 mg/dL, (2) diabetes, or (3) coronary artery disease. We were unable to calculate individual 10-year atherosclerotic cardiovascular disease risk scores; therefore, this statin-eligible group was excluded from our analysis.
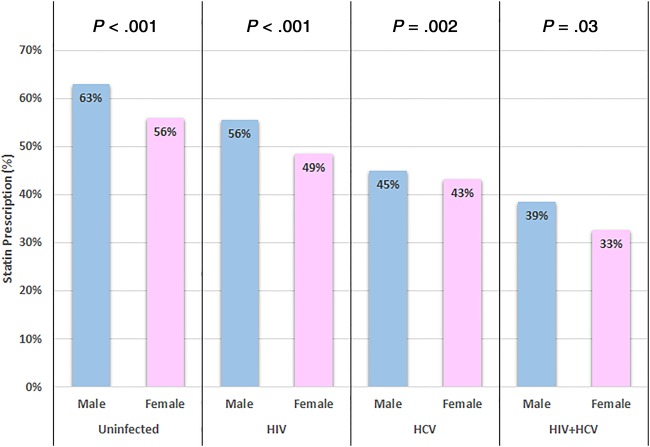
We identified 5700 patients with HIV (32% female), 31 740 with HCV (39% female), 1420 patients with HIV/HCV coinfection (32% female), and 1 486 510 (50% female) controls free of HIV and HCV. Statin prescription rate for eligible patients was highest in noninfected controls (60%), followed by HIV (53%) and HCV (44.3%), and was lowest in HIV/HCV (37%). For all 4 groups, the statin prescription rate was significantly higher in males than females (P < .05 for all comparisons; Figure 1). The gender gap was highest among patients with HIV (absolute difference 7%) and uninfected controls (7%), followed by HIV/HCV (6%), and was lowest in HCV (2%).
Figure 1.
Statin prescription rate in eligible patients. Abbreviations: HCV, hepatitis C virus; HIV, human immunodeficiency virus.
These findings confirm the underutilization of statins among those patients living with HIV and/or HCV who fall into the 3 least controversial statin benefit groups. We did not include the risk-based benefit group, for which controversy persists due to poor calibration of the pooled cohort equations in some populations. In a nonveteran real-world cohort, the statin underprescription may be higher than that described by Clement et al, and is in concordance with the data reported from the National Health and Nutrition Examination Survey [3]. We also highlight the gender gap in statin utilization, especially among those with HIV, which requires further investigation.
Notes
Financial support. This work was supported by the National Institutes of Health (grant number K23 HL123341 to C. T. L.).
Potential conflicts of interest. All authors: No reported conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Clement ME, Park LP, Navar AM et al. Statin utilization and recommendations among HIV- and HCV-infected veterans: a cohort study. Clin Infect Dis 2016; 63:407–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kaelber DC, Foster W, Gilder J, Love TE, Jain AK. Patient characteristics associated with venous thromboembolic events: a cohort study using pooled electronic health record data. J Am Med Inform Assoc 2012; 19:965–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mercado C, DeSimone AK, Odom E, Gillespie C, Ayala C, Loustalot F. Prevalence of cholesterol treatment eligibility and medication use among adults—United States, 2005–2012. MMWR Morb Mortal Wkly Rep 2015; 64:1305–11. [DOI] [PubMed] [Google Scholar]