Abstract
We used data from the 2002 to 2010 National Survey of Substance Abuse Treatment Services to describe changes in the supply of public and private outpatient substance use treatment facilities, and whether these trends had implications for the geographic availability of this infrastructure in racial minority counties. Between 2002 and 2010, the number of publicly owned facilities declined 17.2 percent, whereas number of private, for-profit facilities grew 19.1 percent. At baseline, counties with a very high percentage of black residents (i.e., more than one standard deviation above the mean) were more likely (p<0.01) than counties with less than the mean percentage of black residents to be served by public facilities and were thus disproportionately affected by the overall decline in the public sector. Furthermore, the public sector losses in these counties were not offset by an increased likelihood in gains in private for-profit or nonprofit facilities. Future research should examine the effect of Medicaid expansions on the supply of substance use treatment facilities, with particular attention to counties with a high percentage of black residents in states that do not opt into the expansion.
Keywords: Disparities, substance use disorders, safety-net systems
Substance use disorders (SUD), including abuse of and dependence on alcohol, illicit drugs, or both, are prevalent in the United States and undertreated.(1, 2) In recent years, national policies for substance use control have shifted away from punitive approaches and toward those that emphasize prevention and treatment.(3) Moreover, the implementation of the Mental Health Parity and Addiction Equity Act of 2008 and the Affordable Care Act of 2010 has led to improvements in health insurance coverage for those with a SUD.(4, 5) To raise treatment rates, this expanded coverage must be linked with geographically accessible outpatient services, especially given the chronic nature of many SUDs.(6) Treatment for SUDs is primarily provided by specialty facilities that are separate from both the general medical and mental health care sectors. (4)
Prior research using cross-sectional data reported that in 2009, more than three-tenths of US counties did not have any outpatient substance use treatment facilities.(7) Furthermore, these facilities were less likely to be located in counties with a greater percentage of black residents, after controlling for socioeconomic status and health insurance coverage. (7) However, little is known about changes in the SUD treatment infrastructure over time and the implications for black communities. A growing body of literature has reported that the decline of health care resources in other sectors is associated with community racial composition. More specifically, hospitals (8, 9), trauma centers (10, 11), and emergency departments (12) that serve black communities and populations are more likely to close, even after accounting for differences in socioeconomic resources. Yet, it is unknown whether communities with a higher percentage of black residents have similar vulnerabilities for loss of substance use treatment facilities.
There is reason to suspect that the supply of public and private nonprofit substance use treatment facilities may have been unstable since the turn of the century given that the majority of their revenue comes from government sources.(13) Between 2000 and 2010, funding for the Substance Abuse Prevention and Treatment Block Grant (an important source of federal funding for SUD treatment programs) lagged behind inflation.(4) After the economic downturn in 2008, state and local agencies experienced substantial budget reductions and had disproportionate cuts in spending for substance use treatment.(4) Consequently, public and nonprofit SUD treatment facilities that relied heavily on government resources may have faced increasing fiscal pressures to contract or close services, similar to what was reported in the mental health care system.(14) Publicly funded substance abuse treatment programs are an especially important resource for black clients, who constitute one-fifth of program admissions (15) despite having a similar underlying prevalence of SUD compared to whites, and despite accounting for only 13 percent of the US population.(16, 17)
At the same time, anecdotal reports have cited increased development of specialty SUD treatment services by private, for-profit corporations. Investors have identified the potential of this sector to offer growth opportunities and high margins of return in a large, untapped market where insurance coverage is expanding and treatment rates remain low.(18–20) However, it is unclear whether investors are looking to target underserved communities with gaps in the treatment infrastructure. If racial minority communities are less likely to have treatment facilities, these areas may be considered as opportunities with limited competition. On the other hand, profit-seeking firms may choose to locate in more affluent communities, which are less likely to have large proportions of racial minority residents. Studies have reported, for example, that growth in another outpatient for-profit sector – retail clinics – has been more likely to occur in communities with more economic resources, more favorable insurance coverage, and a lower percentage of black residents.(21, 22)
To date, however, there is no empirical evidence about recent trends in the supply of public and private SUD treatment facilities, and whether these trends have implications for the geographic availability of facilities in black communities. To address these gaps in the literature, we merged national data from several sources to achieve three study objectives. First, we describe trends in the ownership mix of SUD treatment facilities. Second, we describe changes in the geographic availability of outpatient SUD treatment facilities across US counties for public and private facilities. Finally, we examine whether the percentage of black residents in a county is associated with changes in the geographic availability of outpatient substance use treatment facilities.
Study Data And Methods
Data
Data come from the 2002 to 2010 National Survey of Substance Abuse Treatment Services (N-SSATS), an annual cross-sectional survey of public and private facilities that provide SUD treatment. The sampling frame was derived from the Inventory of Substance Abuse Treatment Services, which includes SUD treatment facilities that are licensed, certified, or otherwise approved by the state substance abuse agency (approximately 95 percent of facilities), as well as facilities that are not licensed or certified (approximately 5 percent of facilities). More than 13,000 facilities surveyed in each respective year, and response rates ranged from 91.4 percent to 96.5 percent.(23) We also aggregated facility-level data to the county-level and merged these data with measures from the 2011 and 2014 Area Healthcare Resources File (N=3,139 counties).(24) Of the 3,142 counties in all fifty states, we excluded three that were missing information on key demographic measures; this yielded a sample of 3,139 counties available for analysis.
Measures
Dependent Variables
We identified substance use treatment facilities that offered outpatient treatment and classified facilities by ownership status: public, private nonprofit, and private for-profit. Next, we aggregated facility-level data using the Federal Information Processing Standard (FIPS) code, which identifies counties and county equivalents, to create indicators for whether a county had any: outpatient substance use treatment facility in 2002; outpatient facility in 2010; net gain in outpatient facilities between 2002 and 2010; and net loss in outpatient facilities between 2002 and 2010. We created separate county-level indicators for all outpatient facilities and by facility ownership type.
County Racial Composition
We created a categorical measure of the percentage of black residents, using the mean (9.7 percent) and standard deviation (15.6 percent) to establish cut points that captured variation in the right tail of the distribution. More specifically, the percentage of black residents in the county was classified as: less than the mean ( or less than 10 percent of residents); high (from the mean to one standard deviation above the mean, or 10 percent to less than 25 percent); very high (between one and two standard deviations above the mean, or 25 percent to less than 41); and extremely high (at least two standard deviations above the mean, or at least 41 percent]).
County-level Control Variables
All regression models included measures to control for variation in social and demographic characteristics of the county that may be correlated with prevalence of SUDs and demand for substance use treatment. Using the most recent year of data available in the AHRF that preceded the baseline facility survey year, we derived measures of the percentage of residents that were: between the age of 15 and 44 [2000]; male [2000]; living below the federal poverty level [2001]; Hispanic [2001]; and living in an urban area [2000]. We also included the following measures of health insurance status, using the earliest year of data available in the AHRF that corresponded to the study period: percentage enrolled in Medicaid [2004]; and percentage uninsured [2005]. Finally, we controlled for the total county population [2001]. For regression models that examined the likelihood of having a facility in 2010 and changes in county-level access to facilities over time, we also created measures to capture changes in the social and demographic characteristics of these communities using the best available data in the AHRF that corresponded to the study period.
Analysis
Analyses were conducted using Stata version 13.1. We first examined descriptive information about the number of outpatient SUD treatment facilities in each year between 2002 and 2010 by ownership status. Next, we aggregated facility-level information to the county to examine county-level trends in access to outpatient SUD treatment.
To assess whether community racial composition was associated with changes in geographic availability of outpatient SUD treatment facilities, we examined the bivariate association between each dependent variable and county percentage of black residents using chi-squared tests. We subsequently estimated multivariate logistic regressions for the dependent variables assessing whether a county had any outpatient facility in 2002; any outpatient facility in 2010; net gain in outpatient facilities between 2002 and 2010; and net loss in outpatient facilities during this time. Each model was estimated for all outpatient facilities, then separately by ownership status. Net loss was estimated only for the subset of counties that had each respective type of outpatient SUD treatment facility at baseline (all facilities: N=2,211 counties; public facilities: N=941 counties; nonprofit facilities: N=1,660 counties; for-profit facilities: N=857 counties).
Regression models included census division indicators and controlled for the county-level social and demographic characteristics described above. Standard errors were clustered at the state level. We estimated marginal effects using the “margins” command at the reference category for our predictor of interest (percentage black residents). This output was used to generate graphs that present the adjusted percentage of counties with each type of facility at baseline and follow-up across the four categories of county racial composition.
Limitations
Several study limitations are noted. First, causality cannot be established in these associations. Second, although the NSSAT-S has been conducted in more recent years, this data was not available at the time of the study. Third, although response rates were high across years (greater than 91 percent), it is possible that the difference in the response rate between baseline and follow-up may have accounted for part of the estimated difference in overall supply of facilities. However, there is no reason to believe that differences in the response rates would have biased the findings associated with the trends in ownership mix or the geographic availability of facilities across racial minority communities. Finally, although the county is a meaningful unit of analysis for health resource planning purposes and has been used to understand the distribution of outpatient health care resources for vulnerable populations (25, 26), future research should examine the geographic availability of facilities using smaller units of analysis as data become available.
Results
Facility-level Trends
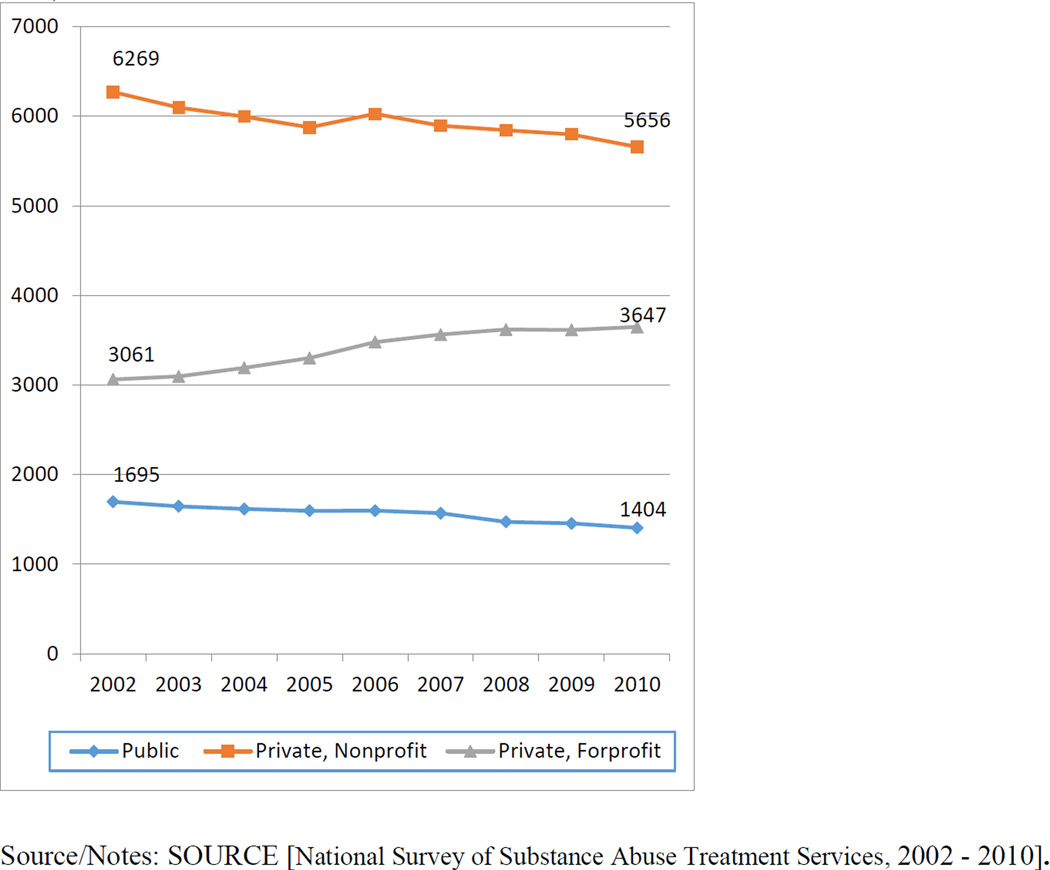
In 2002, more than half of the 11,025 outpatient SUD treatment facilities in the United States were private nonprofit entities (56.9 percent), more than one-fourth were for-profit entities (27.8 percent), and 15.4 percent were publicly owned (Exhibit 1). Between 2002 and 2010, the number of public and nonprofit facilities declined by 17.2 percent and 9.8 percent, respectively. However, there was a 19.1 percent increase in the number of private for-profit facilities. In supplemental analyses (Appendix Exhibit A1) (27), we examined these trends separately for states that have and have not opted into Medicaid expansion.(28) Notably, the relative decline in public facilities (25.2 percent) and increase in for-profit facilities (24.6 percent) were more pronounced in states that have not opted into the Medicaid expansion.
Exhibit 1.
Trends in the supply of public and private outpatient substance use treatment facilities (2002 – 2010)
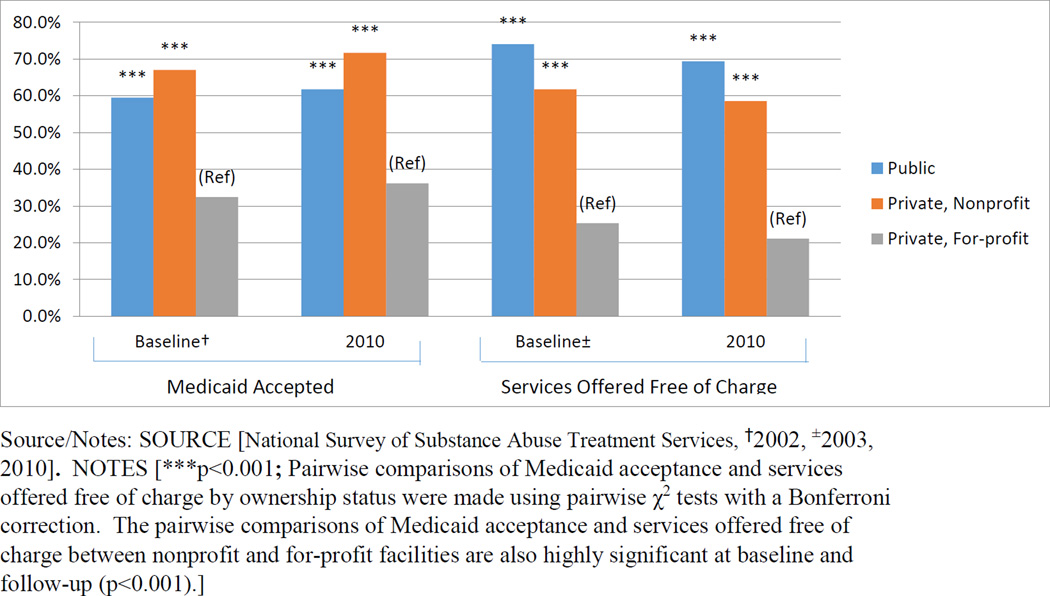
Declines in the public and nonprofit sectors have implications for access to services for low-income populations (Exhibit 2). At baseline and follow-up, public and nonprofit facilities were significantly more likely than for-profit facilities to accept Medicaid and offer services free-of charge to those who cannot afford to pay (p<0.001). Furthermore, public facilities were more likely than nonprofit facilities to offer services free-of-charge to those who cannot pay at baseline and follow-up (p<0.001).
Exhibit 2.
Percentage of outpatient substance use treatment facilities that accept Medicaid and offer services free of charge at baseline and follow-up, by ownership status
County-Level Availability Of SUD Treatment Facilities
Descriptive information about the social and demographic characteristics of the counties is provided in the online appendix (Appendix Exhibit A2, A3).(27)
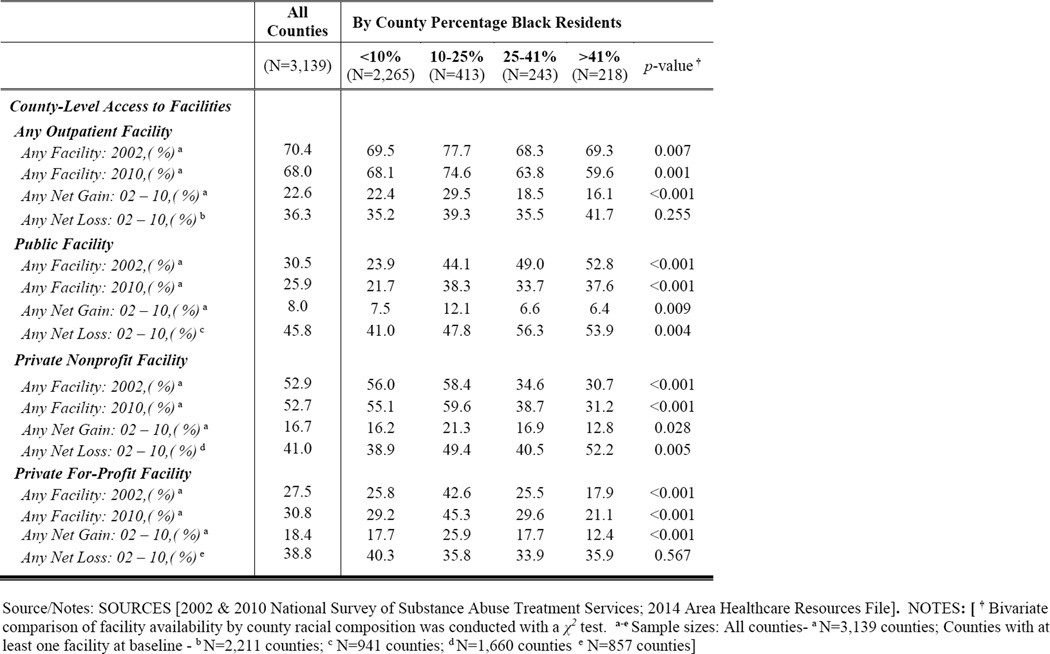
In 2002, more than half of US counties had at least one nonprofit facility (52.9 percent), 30.5 percent had at least one public facility, and 27.5 percent had at least one for-profit facility (Exhibit 3). Among counties with at least one public facility at baseline (N=941), nearly half experienced a net loss in the number of public facilities by 2010. When examining net gains, 18.4 percent of all US counties experienced a net gain in the number of for-profit facilities.
Exhibit 3.
County-level availability of outpatient substance use treatment facilities and sociodemographic characteristics, by county racial composition
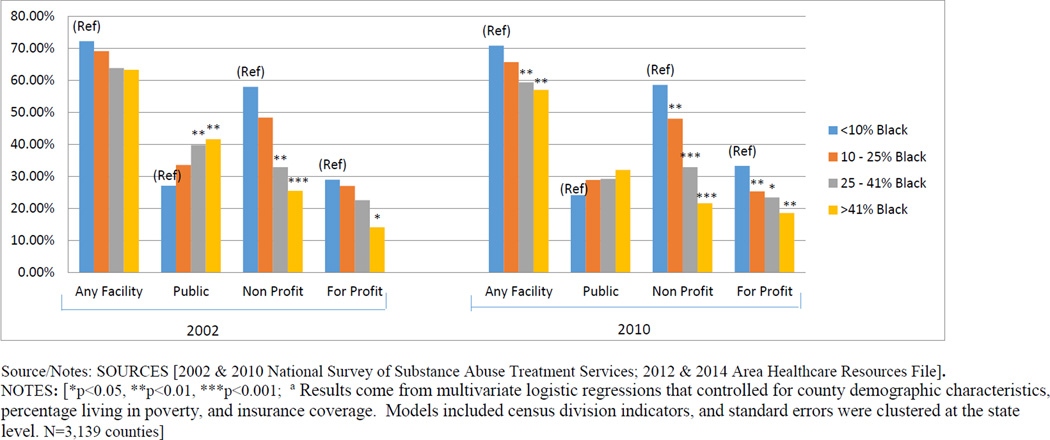
At baseline, results from the bivariate (Exhibit 3) and multivariate comparisons (Exhibit 4) indicate that public facilities were significantly more likely to be located in counties with a higher percentage of black residents. Private for-profit and nonprofit facilities were less likely to be located in these same communities. For example, results from the regression analysis indicated that the adjusted percentage of counties with at least one public facility was 14.6 percentage points higher (p<0.01) among counties with an extremely high percentage of black residents (>41 percent black residents), versus counties with less than the mean percentage of Black residents (<10 percent Black residents) (Appendix Exhibit A4).(27) Conversely, counties with an extremely high percentage of black residents were 14.9 percentage points less likely (p<0.05) to have a for-profit facility and 32.5 percentage points less likely (p<0.001) to have a nonprofit facility than counties with less than the mean percentage of black residents in the adjusted analyses. The increased likelihood of having a public facility compensated for the lower likelihood of having a private facility, resulting in no significant overall association between county percentage of black residents and having any outpatient facility at baseline after controlling for other county-level characteristics (Exhibit 4).
Exhibit 4.
Adjusted percentage of counties with any outpatient substance use treatment facility at baseline and follow-up, by county percentage of black residentsa
By 2010, counties with a very high or extremely high percentage of black residents were significantly less likely to have any outpatient facility, compared to counties with less than the mean percentage of black residents in the multivariate analysis (Exhibit 4). The emergence of this overall disparity in access to any facility may be explained by two phenomena. First, counties with a higher percentage of black residents were no longer more likely to have any public facility in 2010, after controlling for other county-level characteristics. Second, the negative relationship between county percentage of black residents and the likelihood of having any private nonprofit or for-profit facility became exacerbated in 2010, compared to the baseline association (Exhibit 4).
To better understand the changes across this time period, we also examined the association between county percentage of black residents and the likelihood that a county experienced a net gain or loss in each type of facility. Between 2002 and 2010, results from the multivariate regression analysis (Appendix Exhibit A7) (27) indicated that counties with an extremely high percentage of black residents were less likely to experience a net gain in private (nonprofit and for-profit) outpatient facilities than counties with less than the mean percentage of Black residents. Conversely, counties with a very high (p<0.01) or extremely high (p<0.05) percentage of black residents were more likely than counties with less than the mean percentage of black residents to experience a net loss in public facilities in bivariate pairwise comparisons (non shown), although these associations were not significant after controlling for other county-level characteristics (Appendix Exhibit A6).(27)
In addition to county racial composition, the percentage of residents living in poverty was also associated with changes in the geographic availability of substance use treatment facilities in the regression analyses. Counties with a higher percentage of residents living in poverty at baseline were less likely to experience a net gain in for-profit and nonprofit facilities (p<0.05) (Appendix Exhibit A7).(27) In addition, counties that experienced an increase in their poverty rate during the study period were significantly more likely to have a net loss in public facilities (p<0.01) (Appendix Exhibit A6).(27)
Discussion
Between 2002 and 2010, there was a decline in the number of public and private nonprofit outpatient substance use treatment facilities, but considerable growth in the number of private, for-profit facilities. Among counties with at least one public outpatient SUD treatment facility at baseline, nearly half experienced a net loss in the number of public facilities by 2010. Counties with a large percentage of Black residents were disproportionately burdened by the decline in public facilities, and these losses were not offset by an increased likelihood in gains in private for-profit or nonprofit facilities.
An overall decline in the supply of public and private, nonprofit facilities has important implications for vulnerable populations across all communities. Compared to private for-profit facilities, public and nonprofit facilities are less likely to turn away clients based on the ability to pay.(13) Although public facilities only constituted fifteen percent of the sample at the beginning of the study period, the decline in this sector is especially notable because these facilities were the most likely to provide services to those who cannot pay at baseline and follow-up, and prior research has reported that they serve a significantly higher percentage of clients unable to pay for services than private (for-profit and nonprofit) facilities.(13) Furthermore, public facilities are more likely than private facilities to offer important services such as HIV testing (29), and more likely than private for-profit facilities to offer comprehensive care including physical examinations and mental health treatment.(30, 31) Future research is needed to better understand the implications of these declines for the accessibility of outpatient care among low-income populations and for the availability of specific types of services.
The decline of public facilities has important implications for counties with a high percentage of black residents in particular. Nearly half of the counties with a public facility at baseline experienced a net loss in this resource, and counties with higher percentage of black residents were overrepresented among these communities. Although counties with a higher percentage of black residents had a similar probability of losing their public substance use treatment facility after controlling for other county-level characteristics, these communities were disproportionately affected by the overall downward trend in the public sector because they were more likely to be served by public facilities at baseline.
The net loss of public facilities in counties that had a higher percentage of Black residents was not offset by an increased likelihood in gains in private facilities. Instead, communities with an extremely high percentage of Black residents were less likely to gain a private (for-profit and nonprofit) facility after adjusting for other county-level social and demographic characteristics. Considered altogether, these results suggest that public facilities may help fill infrastructure gaps left by the private sector, and that losses of these providers may not necessarily draw in new investments from the private sector. As a consequence of the general decline in the public sector coupled with the lower likelihood that these communities experienced a net gain in private facilities, there was an overall disparity in the likelihood that counties with higher percentages of black residents had any outpatient facility by the end of the study period.
To address gaps in the specialty substance use treatment infrastructure for vulnerable communities and populations that result from the closure of public or non-profit facilities, policymakers can allocate resources to expand the availability of SUD treatment in the nearest safety-net facility – whether it is another substance use treatment facility, a community mental health center, or a community health center. In recent years, federal resources have been allocated as part of the Affordable Care Act and other initiatives to facilitate the expansion and integration of behavioral health services into primary care safety-net settings (32). For example, the Health Resources and Services Administration announced in July 2015 the availability of $100 million to enable more than 300 community health centers to expand the delivery of substance abuse treatment services (33). Of those counties that experienced a net loss in either public facilities or nonprofit facilities, more than three-fourths had at least one community health center; this figure was more than four-fifths among counties with higher than the mean percentage of Black residents. To best leverage these investments in expanded SUD services, policymakers may consider prioritizing funding for community health centers located in areas that have lost a public or nonprofit SUD treatment facility.
The expansion of Medicaid under the Affordable Care Act could have important implications for the trends in this sector, given that Medicaid financing constitutes a large and growing source of government funding for these facilities (4, 34). Because the majority of public and nonprofit facilities provide services free of charge to those who cannot pay, the fiscal environment for these facilities may have improved if Medicaid expansions reduced the volume of uncompensated care. As of January 2016, 31 states have opted to participate in the Medicaid expansion.(28) However, it is worth noting that the decline of public facilities was even more pronounced among states that are not participating in the Medicaid expansion. In addition, more than four-fifths of counties with higher than the mean percentage of black residents are located in states that have not expanded Medicaid. As newer data become available, research will be needed to understand the effect of Medicaid expansions on the trends in this sector, and whether the lack of Medicaid participation of many states has exacerbated disparities in availability of substance use treatment facilities in these communities.
Conclusion
This study provides the first empirical information about trends in the ownership mix of SUD treatment facilities since the turn of the century and the implications of these trends for counties with a high percentage of black residents. The general decline of the public sector, coupled with a reduced likelihood of gaining private facilities, resulted in an overall disparity in the geographic availability of SUD treatment facilities in counties with higher percentages of Black residents by 2010. As national policies for substance use control continue to shift towards prevention and treatment and away from more punitive approaches, it will be essential to ensure there is sufficient availability of treatment facilities across diverse communities.
Supplementary Material
Acknowledgments
Research reported in this publication was supported by the National Institute of Mental Health (K01MH095823). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Disclosures: The authors have no financial interests and no conflicts of interest to disclose.
REFERENCES
- 1.Center for Behavioral Health Statistics and Quality. Behavioral trends in the United States: Results from the 2014 Survey on Drug Use and Health. HHS Publication No. SMA 15-4927, NSDUH Series H-50. Rockville, MD: 2015. [Google Scholar]
- 2.Center for Behavioral Health Statistics and Quality. 2014 National Survey on Drug Use and Health: Detailed Tables. Rockville, MD: 2015. [Google Scholar]
- 3.Executive Office of the President. National Drug Control Strategy. Washington, DC: 2014. [cited 2015 November 1]. Available from: https://www.whitehouse.gov/sites/default/files/ndcs_2014.pdf. [Google Scholar]
- 4.Buck JA. The looming expansion and transformation of public substance abuse treatment under the Affordable Care Act. Health Aff (Millwood) 2011;30(8):1402–1410. doi: 10.1377/hlthaff.2011.0480. [DOI] [PubMed] [Google Scholar]
- 5.Garfield RL, Lave JR, Donohue JM. Health reform and the scope of benefits for mental health and substance use disorder services. Psychiatr Serv. 2010;61(11):1081–1086. doi: 10.1176/ps.2010.61.11.1081. [DOI] [PubMed] [Google Scholar]
- 6.McLellan AT, Lewis DC, O'Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284(13):1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- 7.Cummings JR, Wen H, Ko M, Druss BG. Race/ethnicity and geographic access to Medicaid substance use disorder treatment facilities in the United States. JAMA Psychiatry. 2014;71(2):190–196. doi: 10.1001/jamapsychiatry.2013.3575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ko M, Needleman J, Derose KP, Laugesen MJ, Ponce NA. Residential segregation and the survival of U.S. urban public hospitals. Med Care Res Rev. 2014;71(3):243–260. doi: 10.1177/1077558713515079. [DOI] [PubMed] [Google Scholar]
- 9.Whiteis DG. Hospital and community characteristics in closures of urban hospitals, 1980-87. Public Health Rep. 1992;107(4):409–416. [PMC free article] [PubMed] [Google Scholar]
- 10.Hsia RY, Shen YC. Rising closures of hospital trauma centers disproportionately burden vulnerable populations. Health Aff (Millwood) 2011;30(10):1912–1920. doi: 10.1377/hlthaff.2011.0510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hsia RY, Srebotnjak T, Kanzaria HK, McCulloch C, Auerbach AD. System-level health disparities in California emergency departments: minorities and Medicaid patients are at higher risk of losing their emergency departments. Ann Emerg Med. 2012;59(5):358–365. doi: 10.1016/j.annemergmed.2011.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shen YC, Hsia RY, Kuzma K. Understanding the risk factors of trauma center closures: do financial pressure and community characteristics matter? Med Care. 2009;47(9):968–978. doi: 10.1097/MLR.0b013e31819c9415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wheeler JR, Nahra TA. Private and public ownership in outpatient substance abuse treatment: do we have a two-tiered system? Adm Policy Ment Health. 2000;27(4):197–209. doi: 10.1023/a:1021357318246. [DOI] [PubMed] [Google Scholar]
- 14.Honberg R, Kimball A, Diehl S, Usher L, Fitzpatrick M. State Mental Health Cuts: The Continuing Crisis. Arlington, VA: National Alliance on Mental Illness; 2011. [cited 2015 October 22]. Available from: http://www.nami.org/ContentManagement/ContentDisplay.cfm?ContentFileID=147763. [Google Scholar]
- 15.National Institute on Drug Abuse, National Instittues of Health. Drug Facts: Treatment Statistics. Bethesda, Maryland: U.S. Department of Health and Human Services; 2011. [cited 2015 November 15]. Available from: http://www.drugabuse.gov/publications/drugfacts/treatment-statistics. [Google Scholar]
- 16.Substance Abuse and Mental Health Services Administration. Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings. HHS Publication No. (SMA) 13-4795, NSDUH Series H-46. Rockville, Maryland: Substance Abuse and Mental Health Services Administration; 2013. [Google Scholar]
- 17.United States Census Bureau. State & County QuickFacts. Washington D.C.: 2015. [cited 2015 October 26]. Available from: http://quickfacts.census.gov/qfd/states/00000.html. [Google Scholar]
- 18.Hill J. Behavioral Healthcare: Five Key Factors Are Driving Sector Consolidation. Edina, MN: Triple Tree; 2012. [cited 2014 August 1]. Available from: http://www.triple-tree.com/blog/2012/03/20/behavioral-healthcare-five-key-factors-are-driving-sector-consolidation/ [Google Scholar]
- 19.Kutscher B. Investors eye behavioral health: Market sees growth as more payers cover treatment. Modern Healthcare. 2013 Feb 15; [PubMed] [Google Scholar]
- 20.Knopf A. Special report: Addiction treatment growing as a financial investment. Alcoholism & Drug Abuse Weekly. 2012 Nov 5; [Google Scholar]
- 21.Pollack CE, Armstrong K. The geographic accessibility of retail clinics for underserved populations. JAMA Intern Med. 2009;169(10):945–949. doi: 10.1001/archinternmed.2009.69. discussion 50-3. [DOI] [PubMed] [Google Scholar]
- 22.Rudavsky R, Mehrotra A. Sociodemographic characteristics of communities served by retail clinics. J Am Board Fam Med. 2010;23(1):42–48. doi: 10.3122/jabfm.2010.01.090033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.United States Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. National Survey of Substance Abuse Treatment Services (N-SSATS) -- Concatenated, 1997 to 2010. ICPSR28544-v2. Ann Arbor, M: Inter-university Consortium for Political and Social Research [distributor]; 2012-06-07. [Google Scholar]
- 24.Area Health Resources File (ARF) Rockville, MD: US Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Professions; 2011-2012. pp. 2014–2015. [Google Scholar]
- 25.Cummings JR, Wen H, Ko M, Druss BG. Geography and the Medicaid mental health care infrastructure: implications for health care reform. JAMA Psychiatry. 2013;70(10):1084–1090. doi: 10.1001/jamapsychiatry.2013.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ko M, Cummings JR, Ponce NA. Changes in the Supply of US Rural Health Centers, 2000-2011: Implications for Rural Minority Communities. J Rural Health. 2015 doi: 10.1111/jrh.12147. [DOI] [PubMed] [Google Scholar]
- 27.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 28.The Henry J. State Health Facts: Status of State Action on the Medicaid Expansion Decision. Menlo Park, CA: 2016. [cited 2016 February 20]. Kaiser Family Foundation. Available from: http://kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/ [Google Scholar]
- 29.Pollack HA, D'Aunno T, Lamar B. Outpatient substance abuse treatment and HIV prevention: an update. J Subst Abuse Treat. 2006;30(1):39–47. doi: 10.1016/j.jsat.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 30.Friedmann PD, Lemon SC, Durkin EM, D'Aunno TA. Trends in comprehensive service availability in outpatient drug abuse treatment. J Subst Abuse Treat. 2003;24(1):81–88. doi: 10.1016/s0740-5472(02)00323-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.D'Aunno T. The role of organization and management in substance abuse treatment: Review and roadmap. J Subst Abuse Treat. 2006;31(3):221–233. doi: 10.1016/j.jsat.2006.06.016. [DOI] [PubMed] [Google Scholar]
- 32.Brolin M, Quinn A, Sirkin JT, Horgan CM, Parks J, Easterday J, et al. Financing of Behavioral Health Services within Federally Qualified Health Centers. Washington D.C.: Truven Health Analytics, Brandeis University; 2012. [Google Scholar]
- 33.Health Resources and Services Administration. FY 2016 Substance Abuse Service Expansion Technical Assistance. Rockville, MD: U.S. Department of Health and Human Services; 2016. [cited 2016 February 16]. Available from: http://bphc.hrsa.gov/programopportunities/fundingopportunities/substanceabuse/index.html. [Google Scholar]
- 34.The Pew Charitable Trusts, The John D. and Catherine T. MacArthur Foundation. Substance Use Disorders and the Role of the States. Philadelphia, PA: 2015. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.