Abstract
Objective:
This article measures the probability that out-of-pocket expenses in the United States exceed a threshold share of income. It calculates this probability separately by individuals’ health condition, income, and elderly status and estimates changes occurring in these probabilities between 2010 and 2013.
Data and Method:
This article uses nationally representative household survey data on 344,000 individuals. Logistic regressions estimate the probabilities that out-of-pocket expenses exceed 5% and alternatively 10% of income in the two study years. These probabilities are calculated for individuals based on their income, health status, and elderly status.
Results:
Despite favorable changes in both health policy and the economy, large numbers of Americans continue to be exposed to high out-of-pocket expenditures. For instance, the results indicate that in 2013 over a quarter of nonelderly low-income citizens in poor health spent 10% or more of their income on out-of-pocket expenses, and over 40% of this group spent more than 5%. Moreover, for Americans as a whole, the probability of spending in excess of 5% of income on out-of-pocket costs increased by 1.4 percentage points between 2010 and 2013, with the largest increases occurring among low-income Americans; the probability of Americans spending more than 10% of income grew from 9.3% to 9.6%, with the largest increases also occurring among the poor.
Conclusion:
The magnitude of out-of-pocket’s financial burden and the most recent upward trends in it underscore a need to develop good measures of the degree to which health care policy exposes individuals to financial risk, and to closely monitor the Affordable Care Act’s success in reducing Americans’ exposure to large medical bills.
Keywords: Out-of-pocket, insurance, financing equity, Affordable Care Act
Introduction
Studies show that greater out-of-pocket (OOP) requirements reduce the use of health care; some researchers also trace larger OOP payments to poorer health outcomes or more expensive alternatives, especially among the poor, elderly, and those in poor health.1–7 Large OOP expenses also commonly lead to financial difficulties and, in extreme cases, bankruptcy.8–11 It is for these reasons that a central goal of the Patient Protection and Affordable Care Act (ACA) has been to expand the coverage and improve the design of health insurance to decrease the incidence of large OOP medical expenses. This article provides a more complete and accurate appraisal of the current size and most recent trends in this incidence. It does this by examining very large, nationally representative cross-sectional samples of the United States’ civilian, non-institutionalized population in 2010 and 2013; by using robust measures of income; by restricting OOP to non-premium expenses; and by calculating the probability of high OOP expenses based on citizens’ elderly status, income, and health status. Using cohorts from two different years (2010 and 2013) allows the article to also investigate the most recent trends in these probabilities.
The article’s results provide one benchmark for assessing the future success of policy measures intended to improve Americans’ protection from large OOP medical expenses. According to the White House, the ACA has already begun limiting health care costs and improving Americans’ financial protection from large health care bills.12 Research has already detected expansions in insurance coverage traceable to the ACA provisions.13,14 Relatively strong income growth over the period 2010–2013 could also be expected to reduce Americans’ exposure to the financial strain of devoting large amounts of one’s income to medical bills. Using data from 2010 to 2013, the article both assesses current levels of financial burden and analyzes whether a downward trend is evident.
Our measure of the financial burden OOP expenses place on families is a retrospective one insofar as it measures the probability (or risk) of high expenses through actual expenditures. We thus estimate it by measuring how common it is for OOP expenses to require more than a threshold share of one’s income. A different approach would measure Americans’ exposure to large medical costs by assessing prospective health needs and evaluating the adequacy of one’s insurance policy (or lack thereof) to cover these needs.15,16 Developing a prospective measure is a more difficult conceptual undertaking with challenging data requirements.16 Such a prospective measure conveys the degree to which Americans potentially face high health care costs. By measuring this insecurity retrospectively, this article likely underestimates the true degree to which Americans are exposed to high health expenditures, and the economic insecurity that this creates.
In theory, health insurance reduces the risk of high health care expenditures by turning the unpredictable expense of medical care into predictable spending on premiums. OOP expenditures as a way to reduce the cost of insurance can help balance the competing objectives of providing financial protection and containing health care costs. A reliance on co-payments, co-insurance, and deductibles can help to reduce the potential for individuals to over usage health care when the additional cost to them of consuming it is near zero. OOP payment requirements can also shift what might be considered discretionary medical spending from the insured pool to the user. Of course for those without insurance, in theory, all consumption of medical goods and services must be paid OOP, although in practice the amount paid is typically much less.17
In the United States, roughly 12% of the nation’s total health care expenditures is paid OOP, with the other 88% paid by some combination of public and private insurance.18 It is this 12%, the portion of medical spending most difficult to plan for or predict, that we measure in this article. While paying for health insurance via taxes, insurance premiums, and lower wages can also place a financial burden on households, these expenses are predictable ones and do not (or should not) influence health care usage. OOP payments are much harder to predict and plan for, and this mode of payment can result in individuals underutilizing health care and having less favorable health outcomes.1–7
While some OOP spending can be justified on grounds of efficiency and equity, concern over it arises from the high financial burden it can place on households, low-income ones in particular. High OOP can reduce the use of medical services and weaken adherence to medication therapies, possibly resulting in poorer health outcomes or more expensive alternatives. Health care decisions are particularly sensitive to OOP requirements among the poor,2,19 elderly,2 and those with health problems.20,21
While researchers and policy makers do not agree on how best to assess the appropriateness of cost-sharing practices, the most common approach, replicated here, is to measure the extent to which they require citizens to devote a large share of their income to OOP costs22–27—although as discussed below, researchers do not all measure this the same way. This measure offers a straightforward gauge of citizens’ protection from the burden of large medical bills and the inequities in health care financing, access, and outcomes that can result. That medical expenses are an important contributing factor to the financial distress of families, as well as the frequency with which they declare bankruptcy,8 adds a separate reason why most researchers judge cost-sharing practices by the degree to which they cause people to devote a large share of their income to them.
This article adds to recent research on the burden OOP expenses place on Americans by analyzing more recent data. Several studies using the same data and a similar methodology rely on 2010 data.25,27 Others define OOP too broadly by including premium expenses.28–31 Including direct expenditures on premiums in a definition of OOP moves partially, but incompletely, in the direction of measuring the total burden health care financing places on households, an analysis that van Doorslaer et al.32 undertook in the 1990s. This article, by contrast, focuses exclusively on the variable portion of health care expenses that is those expenses occurring at the point of usage. Other recent research limits itself to particular demographic groups, most commonly the nonelderly adult population,28,29 the insured,24 or children.33 Several studies rely on phone call surveys with low response rates and relatively small samples of individuals, which raise concerns over their reliability.24,28 The results of any study of financial burden will depend on how income is measured, and this study offers a more precise definition and accurate measure of the amount of resources available to the households to meet their medical needs. Finally, in calculating the probability of high OOP expense, the article disentangles the confounding roles of income, age, and health status.
Data and methods
Data
This study employs logistic regression analysis using data from nationally representative households that provide information on both OOP spending and household income. These data are used to estimate the probability that those with different demographic characteristics have large medical bills, where “large” is defined relative to income. Separate probabilities are calculated for different demographic groups based on individuals’ income, elderly status, and health condition. By pooling annual cross-sectional household data from the US Census Bureau’s Current Population Survey’s Annual Social and Economic Supplement (CPS-ASEC) for both 2010 and 2013,34 the study estimates both current risk factors for different demographic groups and changes in this risk over a 3-year period. Rising income, stagnating health costs, and expanding insurance coverage suggest that, all else equal, Americans’ protection from high medical expenses should be diminishing.
The CPS-ASEC contains excellent household data on OOP spending, which Caswell and O’Hara35 show is comparable in quality to that contained in the Medical Expenditure Panel Survey (MEPS). The CPS-ASEC data also have an advantage over the MEPS in that it provides many more observations; in 2010, it includes data on 204,983 individuals, and in 2013, 139,415 individuals. Crucial for this study, the CPS-ASEC also has significantly better and more accurate data on household income. Previous studies of high OOP expenditures have often resulted in inconsistent estimates, at least partially because of differences in the accuracy of income or variation in how it is defined.
We use information on all individuals in the 2010 and 2013 CPS-ASEC waves, except for those with disposable income equal to or below zero (n = 1893), leaving 99.5% of the observations (n = 342,505). All estimates are based on weighted individual observations, where weights account for possible selection bias in the population sampled. Table 1 provides the summary statistics broken down by year.
Table 1.
Descriptive statistics.
| 2010 | 2013 | |
|---|---|---|
| Average income | $63,837 | $70,131 |
| Average equivalized income | $36,300 | $39,993 |
| Q1 boundary | $16,206 | $17,105 |
| Q2 boundary | $25,049 | $26,405 |
| Q3 boundary | $35,684 | $37,714 |
| Q4 boundary | $50,903 | $54,514 |
| Percent | ||
| Elderly | 12.8% | 14.2% |
| Poor health | 11.8% | 11.7% |
| OOP > 5% | 20.9% | 22.3% |
| OOP > 10% | 9.3% | 9.6% |
| Number of observations | 203,799 | 138,706 |
OOP: out-of-pocket; Q: quintile.
Income is household disposable income. Equivalized income is household disposable income divided by the square root of household size. Dollar amounts in current dollars.
Definitions
OOP expenses
We measure household OOP spending by the direct expenses incurred at the household level for health care, which includes deductibles, co-insurance requirements, co-payments, and all other health expenses not covered by insurance. For this article, we do not include spending on health insurance premiums, nor taxes devoted to funding public insurance. This is because our purpose is not to examine the entire incidence of health spending on individuals’ budgets, but rather the amount spent at the point of usage. OOP spending captures the unpredictable portion of health care spending and thus serves to gauge the degree of financial protection provided by (public or private) insurance. And unlike other health care spending, OOP spending occurs if and only if medical goods or services are consumed and thus has the potential to deter usage, thereby contributing to inequities in access to health care.
Income
To capture resources available to meet OOP expenses, we use household disposable income, which is a measure of the income available to meet the household’s economic needs. Disposable income is calculated as all earned income derived from labor and capital, adjusted for the amount paid in taxes as well as the value of all cash and near-cash payments received from the government. Household income is generally a better measure of income than is family income because it is less selective in who it counts.
High medical expenses
This article defines high medical expenses as occurring when household OOP expenses exceed a certain share of its disposable income. Researchers typically use a 5% or 10% threshold,22–27 and this article measures “high spending” based separately on each of these two thresholds. All individuals in the same household received the same spending ratio and thus each has the same indicator (either 1 or 0) for high medical expenses. This binary indicator for high spending is the dependent variable used in the logistic regressions described below.
Independent variables
To measure the probability of high OOP spending for individuals within different demographic groups, we distinguish individuals by their income, health status, and elderly standing and estimate separate probabilities for those with different combinations of these three characteristics. We then compare the probability of high expenses between 2010 and 2013 for those with identical combinations of these traits. In this way, the study provides a more precise comparison over time because it accounts for changes in risk factors (health, income, age) among the population that occur over time.
Categorizing individuals based on their income is problematic, though, since income is measured at the household level. To account for differences in household size, we modify household income by assigning a portion of aggregated household income to each individual in the household; specifically, we assign each individual in the two years (2010 and 2013) an equivalized value of their household’s disposable income (disposable income divided by the square root of household size). This allows us to categorize each individual into a year-specific income quintile based on the amount of their equivalized household income. Since all members of the same household receive identical values of equivalized household disposable income, all are assigned to the same income quintile. Because income rose over the period 2010–2013, those in a particular quintile in 2013 on average have higher income relative to those in the same quintile 3 years earlier (see Table 1).
We identify elderly individuals as those aged 65 and older, indicated by an elderly dummy variable. In 2010, the elderly comprised 12.8% of the population, while in 2013 they made up 14.2% (Table 1). The health status of individuals is similarly captured by a “poor health” dummy variable, where individuals are labeled in poor health (value of 1) if in the CPS-ASEC they self-identify (or identify a household member) as either in poor or fair health (where the other three options were good, very good, and excellent health, indicated by the health dummy assuming a value of 0). By this criteria, 11.8% of the population in 2010 were in poor health and 11.7% were in 2013 (Table 1).
Method
The dependent variable, high health expenses, is a binary variable. Logistic regressions estimate the probability of this taking the value of 1 based on an individual’s health status, elderly standing, and income quintile, with the outcome of high OOP spending regressed on the three demographic characteristics. We measure high OOP spending alternatively as exceeding 5% and 10% of disposable income. Each of the two regressions (5% and 10%) uses all observations for both years, and each independent variable is entered twice: once for all observations, and a second time interacted with a 2013 dummy variable so that observations assume the value of zero if they are from 2010. These interaction variables allow us to determine if the probability of high expenses in 2013 for a distinct demographic group differed from the probability we estimate for 2010.
The probability of high expenses (P) for those in demographic group i is calculated (separately for each of the two measures of high spending) based on the estimated β coefficients resulting from the logistic regression. This permits distinguishing probabilities among each demographic group in 2010 and again in 2013. The exact formula for estimating the probability P is36
| (1) |
In equation (1), i represents the number of different demographic groups, Q1–Q5 are dummy variables for the five income quintiles (with Q1 the lowest and Q3 the reference quintile, and as such is excluded), Eld is an indicator variable for those 65 and older, and PH is a second indicator variable for those in poor health. A 2013 subscript indicates the variable takes the value of zero for individuals in the 2010 sample and takes its observed for those in the 2013 sample. In this study, all variables in equation (1) are indicator variables and thus take the value of 1 or 0. Hence, from equation (1), a nonelderly person in 2010, in the first income quintile, and not in poor health has the estimated probability of large health expenses of
| (2) |
Individuals with the same characteristics in 2013 have an estimated probability of
| (3) |
Any difference between equations (3) and (2) provides a gauge of whether the burden of high expenses for members of this demographic group changed between 2010 and 2013.
Results
First, we estimate the β coefficients from logistic regressions where the outcome indicator (high OOP expenses) is regressed on the individual’s characteristics (health status, elderly status, income) and the year. Table 2 presents these estimated β coefficients.
Table 2.
Estimated β coefficients and standard errors.
| OOP > 5% | SE | OOP > 10% | SE | |
|---|---|---|---|---|
| Eld | 0.468 | 0 | 0.485 | 0 |
| Eld-2013 | −0.025 | 0.001 | −0.059 | 0 |
| Q1 | 0.253 | 0 | 0.678 | 0 |
| Q1-2013 | 0.128 | 0 | 0.109 | 0 |
| Q2 | 0.099 | 0 | 0.279 | 0 |
| Q2-2013 | 0.093 | 0 | 0.038 | 0 |
| Q4 | −0.315 | 0 | −0.531 | 0 |
| Q4-2013 | 0.109 | 0 | 0.005 | 0 |
| Q5 | −0.976 | 0 | −1.35 | 0 |
| Q5-2013 | 0.092 | 0.001 | −0.118 | 0 |
| PH | 0.635 | 0 | 0.653 | 0 |
| PH-2013 | −0.071 | 0.001 | −0.053 | 0 |
| Constant | −1.35 | 0 | −2.458 | 0 |
Source: Author estimates, see text.
Eld: elderly (65 and over); Q: quintile; PH: poor health; OOP: out-of-pocket; SE: standard error.
We now convert Table 2’s coefficients into probabilities using equation (1). Table 3 presents these estimations—columns 1 and 2 for the probability of spending in excess of 5% of disposable income, and columns 3 and 4, 10%. The shaded values in the 2013 columns (2 and 4) indicate that the calculated probability is higher in 2013 than in 2010. All differences highlighted in Table 3 are significant at the 1% level of significance. As Table 1 shows, compared with 2010, in 2013 an additional 1.4% of the population had OOP expenses exceeding 5% of their income, and an additional 0.3% had OOP expenses in excess of 10% of their income. Table 3 decomposes these levels and changes to them, by demographic group. As shown, the percent in a broad range of groups spending in excess of 5% of their income grew between 2010 and 2013, while increases at the 10% threshold over this time period occurred primarily among poorer citizens.
Table 3.
Probability of health expenditures exceeding a threshold share of income, by demographic group and year.
| 5% Threshold |
10% Threshold |
|||
|---|---|---|---|---|
| 2010 (%) | 2013 (%) | 2010 (%) | 2013 (%) | |
| Elderly in poor health | ||||
| Q1 | 50.1 | 50.9 | 34.5 | 34.4 |
| Q2 | 46.3 | 46.2 | 26.1 | 24.7 |
| Q3 | 43.9 | 41.5 | 21.1 | 19.3 |
| Q4 | 36.3 | 36.6 | 13.6 | 12.4 |
| Q5 | 22.7 | 22.7 | 6.5 | 5.2 |
| Nonelderly in poor health | ||||
| Q1 | 38.7 | 40.0 | 24.5 | 25.5 |
| Q2 | 35.1 | 35.6 | 17.9 | 17.6 |
| Q3 | 32.8 | 31.3 | 14.1 | 13.5 |
| Q4 | 26.3 | 27.1 | 8.8 | 8.4 |
| Q5 | 15.6 | 15.8 | 4.1 | 3.5 |
| Elderly in good health | ||||
| Q1 | 34.8 | 37.1 | 21.5 | 22.4 |
| Q2 | 31.4 | 32.8 | 15.5 | 15.3 |
| Q3 | 29.3 | 28.8 | 12.2 | 11.6 |
| Q4 | 23.2 | 24.7 | 7.6 | 7.2 |
| Q5 | 13.5 | 14.3 | 3.5 | 2.9 |
| Nonelderly in good health | ||||
| Q1 | 25.0 | 27.5 | 14.4 | 15.8 |
| Q2 | 22.3 | 23.9 | 10.2 | 10.5 |
| Q3 | 20.6 | 20.6 | 7.9 | 7.9 |
| Q4 | 15.9 | 17.4 | 4.8 | 4.8 |
| Q5 | 8.9 | 9.7 | 2.2 | 1.9 |
Q: quintile.
All differences are significant at the 1% level of significance. Shaded numbers indicate that the probability in 2013 was higher than in 2010.
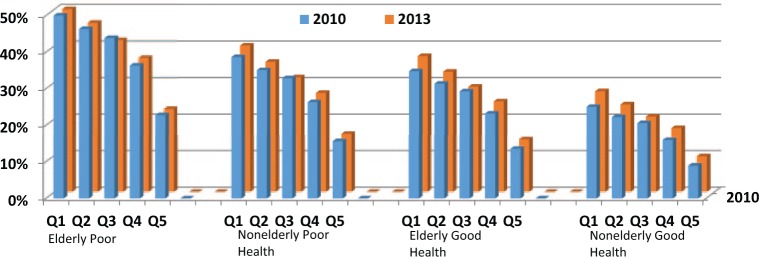
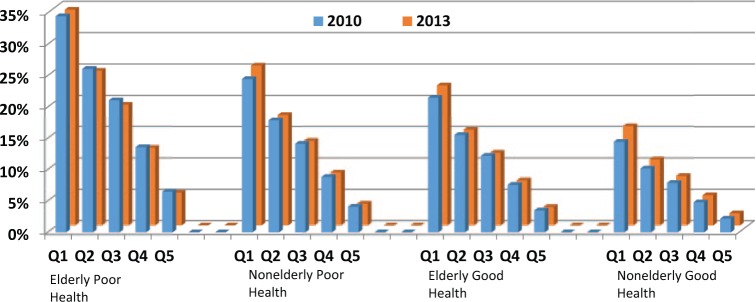
Table 3 also shows that the burden of high OOP expenses is highest among the poor (first quintile), the elderly, and those in poor health. Among those with all three characteristics, one in two had OOP expenses exceeding the 5% threshold in both 2010 and 2013, and more than one in three in both years using the 10% threshold. Not surprisingly, all probabilities decline as income increases, as health improves, and as one moves from an elderly to nonelderly status. Yet even among those not in poor health, not elderly, and with income in the middle quintile, 20.6% spent more than 5% of their disposable income on OOP expenses, and 7.9% devoted at least 10% of their income to these expenses (Table 3). Figures 1 and 2 visually summarize all the estimates by demographic group for both 2010 and 2013.
Figure 1.
Probability of out-of-pocket expenses exceeding 5% of income, by demographic characteristics.
Figure 2.
Probability of out-of-pocket expenses exceeding 10% of income, by demographic characteristics.
As Figure 1 and Table 3 show, nearly all demographic groups had a slightly higher probability in 2013 than 2010 of spending at least 5% of their income on OOP expenses. Moreover, this probability grew the most among the poor where the probability was already the highest. For instance, among the elderly population in good health and with disposable income in the bottom quintile, the likelihood that OOP costs would exceed 5% of disposal income grew from 34.8% to 37.1% between 2010 and 2013.
More modest trends are evident in the percent with OOP spending in excess of 10% of income (Table 1). Table 3 shows that among those in poor health, only nonelderly Americans in the bottom quintile had a higher probability of high OOP expenses in 2013 (25.5%) than they did in 2010 (24.5%). Among those not in poor health, the probability of large expenses grew or remained about the same for those in the bottom two quintiles. On the other hand, the probability of large expenses declined for those in the top 60% of incomes.
Overall, we see some improvement in the incidence of high OOP expenses when measured at this higher threshold, although the improvement is most pronounced at the top of the income distribution where high OOP costs occur less frequently. Yet for those at the bottom of the income distribution—those who already face a high probability of large OOP expenses—the probability of high expenses in 2013 remained similar to or slightly above levels in 2010.
Discussion
This article measures the percentage and trends in that percentage of Americans paying a larger share of their income OOP for medical expenses and does this by accounting for the individuals’ age, health status, or income level. While the results provide more recent and robust estimates than previously published, the approach has several limitations. For one, the article retrospectively estimates the probabilities of high expenses using data on actual household expenditure. This approach is distinct from a prospective measurement of the risk of high expenses, such as recently undertaken by Abramowitz et al.15 Unlike a prospective measurement, a retrospective analysis does not take into account the quality of insurance that individuals have. It is theoretically possible that the insurance coverage of Americans between 2010 and 2013 improved, even though this improvement might not be revealed by measures of the incidence of high OOP expenses. It is similarly possible that the opposite holds true as well. For this reason, the ideal measure would combine both retrospective and prospective indicators of risk, as the recent report by the National Research Council16 recommends.
A second limitation of the retrospective measure used here is that it treats all OOP expenses as equal. If one wishes to measure the element of spending that is difficult to plan for, then clearly not all OOP spending is equal—expenditures corresponding to a high deductible plan are more predictable than is a 20% co-pay requirement for an extended hospital stay, for instance. The article’s measure is also limited insofar as “high expenses” is based on a single year’s expenses; unusually high medical expenses in 1 year are much more affordable than are high expenses that persist year after year. Using an annual measure, the article does not distinguish between households with a one-time incidence of high expenses and those that consistently have high expenses that perhaps may not always reach this article’s annual “high” threshold.
The article’s use of a 5% and alternatively a 10% threshold as an indicator of high medical expenses represent somewhat artificial thresholds. We choose them not because they represent any objective measure but because they are commonly used benchmarks for making comparisons across demographic groups, across time, and across countries. Different metrics could be used to measure the phenomenon, such as ones capturing the distribution of expenditures.37 However, the threshold measure is straightforward to interpret and apply.
A final limitation of this study is that it does not include in the “high spending” category those who fall below the “high” threshold only because they forgo needed medical services and products. This omission could significantly underestimate the degree to which medically related costs expose households to economic insecurity.38
Conclusion
Rising incomes, slower growth in health care expenditures, and an expansion in insurance coverage offer propitious signs that the financial burden created by OOP requirements may be declining. Over the period 2010 and 2013, however, the article finds that the probability of individuals spending more than 5% of their income on medical care has modestly increased, and this is true of just about every demographic groups. The probability of spending more than 10% of income has slightly increased, although this increase is most noticeable among those with low incomes. While the article does not seek to explain these trends, one reason why more Americans may be spending at least 5% of their income on OOP expenses could be because they are switching to higher deductible insurance plans, where individuals exchange lower premiums for higher OOP requirements.24,39 The mixed results regarding the likelihood of high spending based on the 10% threshold is likely at least partly attributable to the fact that income growth has been more robust at the top end of the income distribution, which makes high OOP expenses more affordable for this group. For those in the bottom two quintiles, the probability of high OOP expenses in 2013 either remained similar to levels in 2010 or grew. To capture future risks (including that of under consumption) as well as past burdens, we need new gauges of OOP’s burden, which requires first tackling the numerous conceptual difficulties that come with such measurements, as outlined in a recent National Research Council and Institute of Medicine report.16
A key purpose of the ACA is to improve citizens’ protection from the risk of large medically related expenditures. With the complete implementation of the ACA, we should soon see its full potential to provide this greater financial protection. The ACA’s maximums on OOP expenditures should significantly reduce the probability of catastrophic health care costs,40 as should the expansion of Medicaid.41 However, the ACA will still permit the running-up of large medical bills, amounts which could exceed 20% of poor and middle-class incomes.42–44 Moreover, as Caswell et al.41 show, the risk of high expenses varies by state and is likely to continue to vary into the future due to state-specific policy differences. This study establishes a benchmark of the burden OOP requirements place on different populations. The frequency of high financial burdens revealed here, coupled with some doubts over the ACA’s ability to dramatically reduce poorer Americans’ exposure to large medical bills, underscore the importance of developing good means to monitor the nation’s progress in improving the manner in which we distribute health care’s financial burden.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Eaddy MT, Cook CL, O’Day K, et al. How patient cost trends affect adherence and outcomes. PT 2012; 37(1): 45–55. [PMC free article] [PubMed] [Google Scholar]
- 2. Tamblyn R, Laprise R, Hanley JA, et al. Adverse events associated with prescription drug cost sharing among poor and elderly persons. JAMA 2001; 285: 421–429. [DOI] [PubMed] [Google Scholar]
- 3. Soumerai SB, McLaughlin TJ, Ross-Degnan D, et al. Effects of a limit on Medicaid drug-reimbursement benefits on the use of psychotropic agents and acute mental health services by patients with schizophrenia. N Engl J Med 1994; 331(10): 650–655. [DOI] [PubMed] [Google Scholar]
- 4. Goldman DP, Jena AB, Lakdawalla DN, et al. The value of specialty oncology drugs. Health Serv Res 2010; 45(1): 115–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chandra A, Gruber J, McKnight R. Patient cost-sharing and hospitalization offsets in the elderly. Am Econ Rev 2010; 100(1): 193–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Heisler M, Choi H, Rosen AB, et al. Hospitalizations and deaths among adults with cardiovascular disease who underuse medications because of cost: a longitudinal analysis. Med Care 2010; 48(2): 87–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Soumerai SB, Ross-Degnan D, Avorn J, et al. Effect of Medicaid drug-payment limits on admission to hospitals and nursing homes. N Engl J Med 1991; 325: 1072–1077. [DOI] [PubMed] [Google Scholar]
- 8. Himmelstein D, Thorne D, Warren E, et al. Medical bankruptcy in the United States, 2007: results of a national study. Am J Med 2009; 122(8): 741–746. [DOI] [PubMed] [Google Scholar]
- 9. Kogan MD, Newacheck PW, Blumberg SJ, et al. Underinsurance among children in the United States. N Engl J Med 2010; 363(9): 841–851. [DOI] [PubMed] [Google Scholar]
- 10. Commonwealth Fund. Why not the best? Results from the national scorecard on U.S. health system performance. New York: Commonwealth Fund, http://www.commonwealthfund.org/~/media/files/publications/fund-report/2011/oct/1500_wntb_natl_scorecard_2011_web_v2.pdf, 2011 [Google Scholar]
- 11. Cunningham PJ. Explaining the increase in family financial pressures from medical bills between 2003 and 2007: do affordability thresholds change over time? Med Care Res Rev 2011; 68(3): 352–366. [DOI] [PubMed] [Google Scholar]
- 12. White House. Trends in health care cost growth and the role of the Affordable Care Act. Washington, DC: White House, https://www.whitehouse.gov/sites/default/files/docs/healthcostreport_final_noembargo_v2.pdf, 2013 [Google Scholar]
- 13. Scott JW, Sommers BD, Tsai TC, et al. Dependent coverage provision led to uneven insurance gains and unchanged mortality rates in young adult trauma patients. Health Aff 2014; 34(1): 125–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sommers BD, Buchmueller T, Decker SL, et al. The Affordable Care Act has led to significant gains in health insurance and access to care for young adults. Health Aff 2014; 32(1): 165–174. [DOI] [PubMed] [Google Scholar]
- 15. Abramowitz J, O’Hara B, Morris D. Risking life and limb: estimating a measure of medical care economic risk and considering its implications. Health Econ. Epub ahead of print 16 February 2016. DOI: 10.1002/hec.3325. [DOI] [PubMed] [Google Scholar]
- 16. National Research Council and Institute of Medicine. Medical care economic risk: measuring financial vulnerability from spending on medical care: panel on measuring medical care risk in conjunction with the new supplemental income poverty measure. Washington, DC: The National Academies Press, 2012. [PubMed] [Google Scholar]
- 17. Agency for Healthcare Research and Quality. Total health services—mean and median expenditures per person with expense and distribution of expenses by source of payment: United States, 2013 (Medical Expenditure Panel Survey Household Component Data), http://meps.ahrq.gov/mepsweb
- 18. OECD. Health expenditure and financing: health expenditure indicators, OECD Health Statistics (database), http://dx.doi.org/10.1787/data-00349-en, 2015
- 19. Chernew M, Gibson TB, Yu-Isenberg K, et al. Effects of increased patient cost sharing on socioeconomic disparities in health care. J Gen Intern Med 2008; 23(8): 1131–1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tambor M, Pavlova M, Rechel B. The inability to pay for health services in Central and Eastern Europe. Eur J Public Health 2014; 24: 378–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lee JC, Hasnain-Wynia R, Lau DT. Delay in seeing a doctor due to cost. Health Serv Res 2012; 47: 698–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Law MR, Daw JR, Cheng I, et al. Growth in private payments for health care by Canadian households. Health Policy 2013; 110: 141–146. [DOI] [PubMed] [Google Scholar]
- 23. Sanmartin C, Hennessy D, Lu Y, et al. Trends in out-of-pocket health care expenditures in Canada, by household income, 1997–2009. Health Rep 2014; 25(4): 13–17. [PubMed] [Google Scholar]
- 24. Collins SR, Rasmussen PW, Doty MM, et al. Too high a price: out-of-pocket health care costs in the United States. New York: Commonwealth Fund, http://www.commonwealthfund.org/publications/issue-briefs/2014/nov/out-of-pocket-health-care-costs, 2014. [PubMed] [Google Scholar]
- 25. Baird K. The incidence of high medical expenses by health status in seven developed countries. Health Policy 2016; 120(1): 26–34. [DOI] [PubMed] [Google Scholar]
- 26. Abramowitz J, O’Hara B. The financial burden of medical spending: estimates and implications for evaluating the impact of ACA reforms. Med Care Res Rev 2015; 72(2): 187–199. [DOI] [PubMed] [Google Scholar]
- 27. Baird K. High out-of-pocket medical spending among the poor and elderly in nine developed countries. Health Serv Res. Epub ahead of print 22 January 2016. DOI: 10.1111/1475-6773.12444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Schoen C, Doty MM, Robertson RH, et al. Affordable Care Act reforms could reduce the number of underinsured US adults by 70 percent. Health Aff 2011; 30(9): 1762–1771. [DOI] [PubMed] [Google Scholar]
- 29. Banthin JS, Cunningham P, Bernard DM. Financial burden of health care, 2001–2004. Health Aff 2008; 27(1): 188–195. [DOI] [PubMed] [Google Scholar]
- 30. Cunningham PJ. Despite the recession’s effects on incomes and jobs, the share of people with high medical costs was mostly unchanged. Health Aff 2012; 31(11): 2563–2570. [DOI] [PubMed] [Google Scholar]
- 31. Desmond KA, Rice T, Cubanski J, et al. The burden of out-of-pocket health spending among older versus younger adults: analysis from the Consumer Expenditure Survey, 1998–2003 (Medicare Issue Brief). Menlo Park, CA: Kaiser Family Foundation, 2007. [Google Scholar]
- 32. van Doorslaer E, Wagstaff A, van der Burg H, et al. The redistributive effect of health care finance in twelve OECD countries. J Health Econ 1999; 18: 291–313. [DOI] [PubMed] [Google Scholar]
- 33. Smith J, O’Hara B. The financial burden of paying for non-premium medical expense for children. SEHSD Working Paper, 31 March–2 April 2011; Washington, DC: US Census Bureau. [Google Scholar]
- 34. Luxembourg Income Study Database (LIS). www.lisdatacenter.org (United States; June 2015. –January 2016). Luxembourg: LIS. [Google Scholar]
- 35. Caswell KJ, O’Hara B. Medical out-of pocket expenses and poverty. Washington, DC: US Bureau of the Census, 2010. [Google Scholar]
- 36. Long JS. Regression models for categorical and limited dependent variables. Thousand Oaks, CA: SAGE, 1997. [Google Scholar]
- 37. Gruber J, Levy H. The evolution of medical spending risk. J Econ Perspect 2009; 21(4): 25–48. [DOI] [PubMed] [Google Scholar]
- 38. Abraham JM, DeLeir T, Royalty AB. Moral hazard matters: measuring relative rates of underinsurance using threshold measures. Health Serv Res 2010; 45(3): 806–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Schoen C, Radley D, Collins S. State trends in the cost of employer health insurance coverage, 2003–2013. The Commonwealth Fund, January 2015, http://www.commonwealthfund.org/publications/issue-briefs/2015/jan/state-trends-in-employer-coverage [PubMed]
- 40. Gruber J, Perry I. Realizing health reform’s potential: Will the ACA make health care affordable? New York: Commonwealth Fund, 2011. [Google Scholar]
- 41. Caswell K, Waidmann T, Blumberg L. Financial burden of medical out-of-pocket spending by state and the implications of the 2014 Medicaid expansions. Inquiry 2013; 50(3): 177–201. [DOI] [PubMed] [Google Scholar]
- 42. Associated Press. Under Obamacare, out-of-pocket costs leave some “underinsured.” Arlington, VA: PBS News Hour, http://www.pbs.org/newshour/rundown/under-obamacare-out-of-pocket-costs-leave-some-underinsured/, 2014. [Google Scholar]
- 43. Goodnough A, Pear R. Unable to meet the deductible or the doctor. New York Times, 17 October 2014, http://www.nytimes.com/2014/10/18/us/unable-to-meet-the-deductible-or-the-doctor.html
- 44. Rosenthal E. Insured but not covered. New York Times, 8 February 2015, http://www.nytimes.com/2015/02/08/sunday-review/insured-but-not-covered.html?_r=0