Abstract
The association between physicians’ and patients’ racial attitudes and poorer patient–physician communication in racially discordant medical interactions is well-documented. However, it is unclear how physicians’ and patients’ racial attitudes independently and jointly affect their behaviors during these interactions. In a secondary analysis of video-recorded medical interactions between non-Black physicians and Black patients, we examined how physicians’ explicit and implicit racial bias and patients’ perceived past discrimination influenced their own as well as one another’s affect and level of engagement. Affect and engagement were assessed with a “thin slice” method. For physicians, the major findings were significant three-way interactions: physicians’ affect and engagement were influenced by their implicit and explicit racial bias (i.e., aversive racism), but only when they interacted with patients who reported any incidence of prior discrimination. In contrast, patients’ affect was influenced only by perceived discrimination. Theoretical and clinical implications of current findings are discussed.
Keywords: explicit bias, healthcare disparities, implicit bias, medical interactions, patient–physician communication, perceived discrimination, racial attitudes
The quality of patient–physician communication, which is a critical element of effective medical care (Epstein & Street, 2007), is generally lower in racially discordant than in racially concordant medical interactions (R. L. Johnson, Roter, Powe, & Cooper, 2004; Siminoff, Graham, & Gordon, 2006). The Institute of Medicine report, Unequal Treatment (Smedley, Stith, & Nelson, 2003), proposed that both physicians’ and patients’ racial attitudes (e.g., physician racial bias and patient perceived discrimination) may play a critical role in determining the quality of patient– physician communication, and thus ultimately in healthcare disparities. This proposal spawned considerable research on the association between physician racial bias and the quality of racially discordant interactions (Shavers et al., 2012). However, there is still limited understanding of how physician racial bias affects the dynamics of such interactions. Additionally, very few studies have empirically examined the role of Black patients’ perceived discrimination in determining the quality of racially discordant medical interactions. Even fewer studies have examined how non-Black physicians’ racial bias and Black patients’ perceived discrimination may simultaneously and/or reciprocally affect the dynamics of medical interactions. The present study addressed these gaps in the healthcare disparities literature by examining the effects of non-Black physicians’ and Black patients’ racial attitudes on their own as well as each other’s affect and level of active engagement during medical interactions.
Physician Racial Biases During Racially Discordant Medical Interactions
Racial biases play a significant role in shaping interracial social interactions (Shelton & Richeson, 2006). People have both explicit (conscious, deliberate) and implicit (nonconscious, spontaneous) racial biases (Wilson, Lindsey, & Schooler, 2000), which are only weakly correlated with one another (in the range of .15 to .25; Greenwald, Poehlman, Uhlmann, & Banaji, 2009; Hofmann, Gawronski, Gschwendner, Le, & Schmitt, 2005). Individuals are aware of their explicit racial bias; thus, explicit bias is relatively easy to monitor and self-regulate. In contrast, implicit bias is an automatically activated response that occurs often without conscious awareness (Wilson et al., 2000). Implicit bias is therefore relatively difficult to monitor and self-regulate. It appears that, in the context of medical interactions, the differences between explicit and implicit racial biases are of particular importance. Expressions of racial bias among healthcare providers are strongly condemned (Green et al., 2007). Consequently, physicians are likely to be strongly motivated and able to control their explicit racial bias—bias of which they are aware. However, physicians may not be aware of their implicit racial bias. Even if they were aware of their implicit racial bias, implicit bias plays a particularly influential role in determining nonverbal behaviors (e.g., eye contact, posture) and paraverbal behaviors (e.g., behaviors related to how speech is delivered), which are harder to monitor and self-regulate than verbal behaviors (i.e., the content of the speech; Dovidio, Kawakami, & Gaertner, 2002). Because physicians exhibit significant general implicit racial bias toward Blacks at a level comparable to the general U.S. population (Sabin, Nosek, Greenwald, & Rivara, 2009), their implicit racial bias likely affects the dynamics of racially discordant medical interactions.
An increasing, although still limited, number of studies provide evidence supporting such an argument. For example, physicians’ general implicit racial bias predicts how much physicians verbally dominate a medical interaction: Physicians with higher levels of general implicit racial bias talk more (Cooper et al., 2012; Hagiwara, Penner, Gonzalez, Eggly, et al., 2013) and faster (Cooper et al., 2012) than physicians with lower levels of implicit bias. Also, Hagiwara, Slatcher, Eggly, and Penner (in press) found a positive association between physician implicit bias and the number of anxiety-related words used in racially discordant medical interactions. Importantly, there is evidence that Black patients are sensitive to their physician’s level of general implicit racial bias and react more negatively to physicians with higher levels of implicit bias than to those with lower levels of implicit bias. For example, Cooper et al. (2012) found that Black patients reported lower levels of liking, respect for, and trust of non-Black physicians higher in general implicit racial bias. Blair et al. (2013) also found that Black patients had less trust of and felt treated less well by physicians with higher levels of general implicit racial bias. Schaa, Roter, Biesecker, Cooper, and Erby (2015) found comparable effects with clients of genetic counselors.
In contrast, as already noted, physician explicit racial bias does not appear to have a consistent direct effect on their communication with Black patients (e.g., Hagiwara, Penner, Gonzalez, Eggly, et al., 2013; Penner et al., 2010). However, Penner et al. (2010) found that physician explicit racial bias interacted with implicit racial bias to influence patient reactions to them. Specifically, Black patients who interacted with physicians with lower levels of explicit racial bias but higher levels of implicit racial bias reacted significantly less positively to these physicians than did patients who interacted with physicians who did not fit this low explicit–high implicit bias profile. These findings are consistent with the large literature on the construct of aversive racism. Aversive racists are individuals with low levels of explicit racial bias but high levels of implicit bias (Dovidio & Gaertner, 2004). At the explicit level, they reject racial bias and genuinely find it aversive; however, at the implicit level, they harbor negative feelings toward Blacks. Blacks often react quite negatively to aversive racists, perhaps because aversive racists often give Blacks mixed messages consisting of positive verbal behaviors that do not match their negative nonverbal and paraverbal behaviors (Dovidio et al., 2002).
Patient Perceived Discrimination During Racially Discordant Medical Interactions
The quality of the communication between non-Black physicians and Black patients depends, of course, not only on physicians’ racial bias but also on patients’ racial perceptions such as perceived discrimination. In general, members of socially disadvantaged groups are vigilant for signs of bias when they enter interactions with members of higher status groups (Shelton, Richeson, & Vorauer, 2006; Vorauer, 2006), and they expect to be the target of prejudice and/or discrimination (Bergsieker, Shelton, & Richeson, 2010; Shelton, 2003). These findings are consistent with Black patients’ perspectives on medical care. The majority of Black patients report that they are mistrustful of the medical community and experience discrimination in their medical encounters with White physicians (Dovidio et al., 2008; Halbert, Armstrong, Gandy, & Shaker, 2006; Malat & Hamilton, 2006).
Some researchers have examined how such feelings affect Black patients perceptions of medical interactions with non-Black physicians (e.g., Benkert, Hollie, Nordstrom, Wickson, & Bins-Emerick, 2009; Penner et al., 2009). However, research on how Black patients’ perceived discrimination actually affects their behaviors is relatively limited. One recent study of racially discordant medical interactions found that Black patients with higher levels of perceived discrimination talked more than those with lower levels of perceived discrimination (Hagiwara, Penner, Gonzalez, Eggly, et al., 2013). This finding suggests that Black patients’ racial perceptions and attitudes may affect their behaviors in racially discordant medical interactions
The Present Study
The present study adds to this growing literature on the racial dynamics of medical interactions in two significant ways. First, prior research has typically focused on how physicians’ racial bias and patients’ perceived discrimination affect their perceptions of one another, but the proximal causes of such reactions remain generally unknown. That is, it is not clear how physician racial bias and patient perceived discrimination are actually manifested in medical interactions. The present study addressed this issue by obtaining observers’ ratings of the affect (positive and negative) and level of engagement displayed by both physicians and patients in racially discordant medical interactions and assessing whether they are associated with racial bias and perceived discrimination, respectively. We focused on affect and engagement because they have been found to play important roles in determining the quality of patient–physician communication during the medical interactions (Mendez, Hogan, & Culhane, 2013; Roter & Larson, 2002). Second, rather than simply looking at how physicians’ racial bias or patients’ perceived discrimination influence their own behaviors, we examined how they jointly influence the behaviors that each person displays during real world racially discordant medical interactions.
The present study involved a secondary analysis of medical interactions between non-Black primary care physicians and Black patients at an inner-city primary care clinic in a predominantly Black, low SES neighborhood in a large Midwestern city (see Penner et al., 2009; Penner et al., 2010). The analysis was limited to interactions for which video-recordings and measures relevant to the goals of the present research (i.e., physician racial attitudes and patient perceived discrimination) were available.
Outcomes from the parent study, including elements such as patients’ perceptions of the physicians and the amount of time physicians and patients talked have been previously reported elsewhere (see Hagiwara, Penner, Gonzalez, Eggly, et al., 2013; Penner et al., 2010). The present study, however, focused on observable indicators of the participants’ affect and engagement during the interactions. To do this, we used a thin slice method. In the thin slice method, observers make judgments of target persons based on few brief excerpts of behaviors taken from a longer interaction. These excerpts, which can be anywhere between 2 seconds and 5 minutes (Ambady & Rosenthal, 1992), have been shown to convey information about affect and communication style through behaviors that are likely not consciously regulated, such as facial expression, gestures, and voice tone (Ambady, Koo, et al., 2002; Ambady, Laplante, et al., 2002; Rosenblum et al., 1994). A number of empirical studies and several meta-analyses have shown that judgments of affect and communication style in an interaction based on less than 30 seconds of observation are as accurate and valid as those based on observations of the entire interaction (Ambady, Bernieri, & Richeson, 2000; Murphy, 2005). We used the thin slice method in this study because it was a cost-effective, time-efficient, and valid way to collect the data.
Hypotheses
Previous research has shown that physicians with higher levels of implicit racial bias are rated more negatively by their Black patients than physicians with lower levels of implicit bias (Blair et al., 2013; Cooper et al., 2012). In his study of the same overall sample of physicians and patients who were analyzed in the present study, Penner et al. (2010) found a main effect for physician implicit bias on patient perceptions of physicians, which was further qualified by a significant interaction between implicit and explicit racial bias. Specifically, physicians who scored higher on implicit racial bias but lower on explicit racial bias (i.e., aversive racism) were rated more negatively by their Black patients than other physicians. In later analyses of the same data, Penner et al. (2013) found a similar pattern of the results for patient trust on the physicians 4 weeks after the interaction. These studies suggest that the racial attitudes of physicians who are characterized as an aversive racist were displayed in certain behaviors that were noticed by their patients. Thus, with regard to physician behaviors, we predicted that physician explicit and implicit biases would interact to affect physician affect. Specifically, we expected that physicians with lower levels of explicit racial bias and higher levels of implicit racial bias would display less positive affect and more negative affect than other physicians.
In addition to affect, we also examined the physician level of engagement. Previous healthcare disparities research has shown that non-Black physicians with higher levels of general implicit racial bias were more verbally engaged than those with lower levels of implicit bias (Cooper et al., 2012; Hagiwara, Penner, Gonzalez, Eggly, et al., 2013). These findings are consistent with social psychology research that showed paradoxical effects of Whites’ implicit racial bias on Blacks’ perceptions of Whites: Whites with higher levels of implicit racial bias tend to be perceived by Blacks as more engaged during interracial interactions. Some have speculated that this occurred because Whites higher in implicit bias are more likely to attempt to prevent or suppress expressions of their bias (Shelton, Richeson, Salvatore, & Trawalter, 2005). Because individuals who fit the aversive racist profile are more likely to try to prevent expressions of their bias (Dovidio & Gaertner, 2004), we predicted that aversive racist physicians would be more engaged than other physicians during the racially discordant medical interactions.
The present research also extends the previous work on the impact of racial attitudes on medical interactions by simultaneously exploring the effects of physicians’ racial bias and patients’ perceived discrimination on the dynamics of racially discordant medical interactions. As noted earlier, we are not aware of any prior work on the combined effects of physician racial bias and patient perceived discrimination. This limits our ability to make firm predictions about how they might independently and/or jointly affect their behaviors. However, extrapolating from prior research showing that even minor disagreements in interracial interactions can activate Whites’ implicit bias toward Blacks (Kunda, Davies, Adams, & Spencer, 2002), it seems reasonable to expect that physicians who fit the profile of an aversive racist would be especially sensitive to subtle behaviors displayed by Black patients. Black patients who, because of their own perceived discrimination, may express negative thoughts and feelings during medical interactions. This may, in turn, elicit higher levels of negative responses in aversive racist physicians than in other physicians who do not fit this profile. Thus, we anticipated that we would find a three-way interaction between physician explicit racial attitudes, implicit racial attitudes, and patient perceived discrimination that would affect physician affect and engagement.
In terms of patient behaviors, as already noted, prior research has found that Blacks who report higher levels of perceived discrimination tend to have more negative responses to specific interpersonal interracial encounters in which concerns about bias are aroused (J. D. Johnson, Ashburn-Nardo, Spicer, & Dovidio, 2008), such as medical encounters (Benkert et al., 2009; Penner et al., 2009). Additionally, and as already noted, it has been shown that Black patients who report higher levels of perceived discrimination are more verbally active in racially discordant medical interactions (Hagiwara, Penner, Gonzalez, Eggly, et al., 2013). These findings led us to predict that Black patients who reported higher levels of perceived discrimination would, relative to those who reported lower levels, display less positive and more negative affect and be more engaged in medical encounters.
We also expected a three-way interaction for patient affect and engagement. Prior research has shown that Blacks who report higher levels of perceived discrimination are more sensitive to subtle cues associated with bias than Blacks who report lower levels of perceived discrimination (Mendoza-Denton, Downey, Purdie, Davis, & Pietrzak, 2002). Thus, it is reasonable to expect that the effects of patient perceived discrimination on their affect and engagement may be particularly pronounced when they interact with non-Black physicians who fit the aversive racist profile.
Method
Participants
One-hundred thirteen interactions from the original study of 153 racially discordant medical interactions in a primary care clinic (see Penner et al., 2009) were used in this study. The 113 interactions were selected because: (a) there were video recordings of them, and (b) both the physician and the patient had completed measures of racial bias and perceived discrimination, respectively, prior to the interactions. In the present secondary study, the participants were 113 self-identified low-income (median annual household income less than $20,000) Black patients (77.0% women, Mage = 42.81, SD = 13.73) who interacted with 13 non-Black primary physicians. (11 Asians, two Whites; 53.8% women; Mage = 30.50, SD = 2.51). The demographic and professional characteristics of this subsample did not differ in any meaningful ways from the larger sample. The racial/ethnic distribution of the physicians, although skewed toward Asians, is typical for primary clinics that serve low-income, residentially segregated minority patient populations in the United States (Hing & Lin, 2009; Mertz, Jain, Breckler, Chen, & Grumbach, 2007).
Procedure
In the parent study, physicians were recruited first. Physicians who agreed to participate signed a consent form and completed a baseline questionnaire, which included measures of implicit and explicit bias. Next, patients of those physicians were recruited as they came to their scheduled appointment. Patients who agreed to participate in the study were asked to sign both informed consent and the Health Insurance Portability and Accountability Act (HIPAA) release forms and then completed a baseline questionnaire that included a measure of perceived discrimination. Immediately following the baseline, patients met with their physicians for a scheduled visit, and these interactions were video-recorded. More complete descriptions of the procedure for the original study are reported elsewhere (see Penner et al., 2009; Penner et al., 2010). The original study was approved by Karmanos Cancer Institute Protocol Review and Monitoring Committee and the Wayne State University Institute of Review Board (WSU IRB). The present secondary analysis of data from the original study was approved by both the Virginia Commonwealth University and Wayne State University’s IRBs.
To create “thin slices,” we first measured the total amount of time both a physician and a patient were in the room together. Then, we subtracted the first minute and the last minute of the interaction from the total amount of time because the beginning and the end of medical interactions generally followed a similar pattern of scripted interactions (e.g., greeting and introduction, description of the prescribed medication). Next, the total amount of time was divided into three equal-length segments. Finally, the first 30 seconds were picked from each of the three segments to create “thin slices.” We ensured that each “thin slice”: (a) had both the physician and the patient appearing within the video frame; (b) had either a physician or a patient talking; and (c) included no physical exam. If an excerpt from the first 30 seconds of a given segment did not meet these criteria, we shifted the starting point of the thin slice until we found a 30-second slice that met all criteria.
Next, these “thin slices” were presented in a random order to 19 naïve female undergraduate observers (10 Black, nine White), paid to serve as research assistants for this study. We recruited only female naïve coders because research has shown that women tend to show better judgment accuracy than men (Ambady & Rosenthal, 1992; Weisbuch & Ambady, 2011). Studies that use the thin slice method for affect and communication style judgments do not usually formally train observers (Ambady, Hallahan, & Rosenthal, 1995; Ambady, Koo, Rosenthal, & Winograd, 2002) because research has shown that overthinking and overreasoning can often disrupt the judgment accuracy and that people usually make better judgments when they do not try to explain their judgments (Ambady & Rosenthal, 1992; Weisbuch & Ambady, 2011). Thus, the observers in the present study were simply instructed to: (a) provide their ratings based on their impressions; and (b) use the full scale when reporting their perceptions. Approximately half of the raters were asked to focus only on the patients while they watched the randomly presented “thin slices” one at a time on a computer screen and provide their ratings on 13 items concerning physician/patient affect and engagement (see following lines for more details). Once they provided their ratings for all patients, they were then instructed to look at the slices again and complete the same tasks but this time focusing only on the physicians. The other half of the raters were given the opposite order (physicians first, patients second). All the instructions and “thin slices’ were administered on computer screens using MediaLab software (Jarvis, 2012).
Measures
Physician explicit racial bias
Explicit racial bias toward Blacks was assessed using 25 items that were taken from the Attitudes Toward Blacks Scale (Brigham, 1993) and Modern Racism Scale (McConahay, 1986). Higher numbers indicate more explicit racial bias toward Blacks (α = .89).
Physician implicit racial bias
Implicit racial bias against Blacks was assessed using the computer-based race Implicit Association Test (IAT; Greenwald, McGhee, & Schwartz, 1998). In this task, participants respond to items that are to be classified into four categories: two representing social groups (e.g., White vs. Black) and two representing valence (positive vs. negative), which are presented in pair. The premise is that response times are faster when two categories are paired together for responding (i.e., White–Good or Black–Bad) than when the opposite categories are paired together (i.e., White–Bad or Black–Good). The difference in response time is considered to indicate that these categories are more strongly implicitly associated with one another. IAT responses were scored to compute a D measure (Greenwald, Nosek, & Banaji, 2003). Higher numbers indicate more implicit pro-White/anti-Black bias attitudes.
Patient perceived discrimination
Perceived discrimination was assessed using a modified version of Brown’s measure of perceived past discrimination (Brown, 2001). Participants were asked to indicate whether they had ever experienced unfair treatment in each of seven social domains: jobs, education, medical treatments,1 job applications, police encounters, housing, and dealing with neighbors. Thus, the scale ranged between 0 and 7, with higher numbers indicating greater perceived discrimination. The scale’s odd-even reliability with Spearman-Brown correction = .74.
Affect and engagement
Raters used 9-point rating scales to measure affect and engagement, with higher scores indicating more of a given characteristic. Positive affect was assessed with five items (cheerful, friendly, getting along, relaxed, warm; α = .97); negative affect was assessed with five items (annoyed, cold, hostile, nervous, stressed; α = .84); and engagement was assessed with three items (active, attentive, engaged; α = .97). Interrater reliability was assessed by computing intraclass correlations (ICCs) using the two-way mixed model and a mean of 19 observers, that is, ICC(3,19) for positive affect, negative affect, and engagement separately for patients and physicians. Interrater reliability across the 19 observers was very high (ICCs = .90–.96).
Due to a programming error, there were no observer ratings of cheerful and stressed for the first 27 patients. Thus, the positive and negative affect composite scores for those 27 patients were computed without these items.2
Analysis Overview
An analysis conducted in the previous study using the data from the same parent study (Hagiwara, Penner, Gonzalez, & Albrecht, 2013) showed that patient perceived discrimination had a zero-inflated Poisson distribution. This means that the distribution on the measure of this discrimination consists of two parts (Cameron & Trivedi, 1998): “binary” (whether or not patients reported experiencing any discrimination in the past) and “count” (if the “binary” part was yes, then how many different social domains they report experiencing discrimination in). Initial analyses showed that only the binary part of patient perceived discrimination (i.e., patients who reported no prior discrimination vs. patients who reported any incidence of prior discrimination) was associated with the variables of interest. Thus, the count part was not included in the analyses reported here.
We tested our hypotheses for physicians and patients separately, resulting in a total of six separate analyses (i.e., three outcomes for each group: positive affect, negative affect, and engagement). We used multilevel modeling because patients were nested within physicians. In the full model, grand-mean centered physician implicit bias, grand-mean centered physician explicit bias, and dummy-coded patient perceived discrimination (0 = report of no prior discrimination, 1 = report of any incidence of prior discrimination), as well as all possible interaction terms among these variables were entered as predictors. When higher order interactions were nonsignificant but lower order effects were significant, we removed the nonsignificant higher order interactions from the full model (and in essence placed them in the error term) and reexamined the significance of lower order effects. This step-down procedure is suggested by Aiken and West (1991) when there are no strong theoretical grounds for expecting certain higher order interactions.
Results
Table 1 presents the means, standard deviations, and correlations among all variables. Positive affect, negative affect, and engagement were highly correlated with one another. These associations were stronger within persons (i.e., among physicians or among patients) than between physicians and patients.
Table 1.
Means, standard deviations, and correlations among all variables.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Physician explicit bias | – | ||||||||
| 2. Physician implicit bias | .50** | – | |||||||
| 3. Patient perceived discrimination binary | .17 | .08 | – | ||||||
| 4. Physician positive affect | −.03 | .17† | −.16† | – | |||||
| 5. Physician negative affect | .04 | −.02 | .16† | −.89** | – | ||||
| 6. Physician engagement | −.02 | .14 | −.11 | .87** | −.80** | – | |||
| 7. Patient positive affect | −.19* | −.07 | −.28** | .44** | −.42** | .20* | – | ||
| 8. Patient negative affect | .18† | .03 | .26** | −.39** | .42** | −.17† | −.88** | – | |
| 9. Patient engagement | −.18† | −.11 | −.16† | .17† | −.12 | −.02 | .86** | −.71** | – |
| M | 2.04 | −0.16 | n/a | 6.22 | 1.88 | 7.17 | 5.98 | 2.18 | 6.88 |
| SD | 0.42 | 0.29 | n/a | 0.61 | 0.27 | 0.57 | 0.78 | 0.49 | 0.74 |
Note. N = 113.
p < .10.
p < .05.
p = .01.
Non-Black Physicians
Table 2 presents the estimates of fixed effects for non-Black physicians’ positive affect, negative affect, and engagement. In all three analyses, there were significant main effects for patient perceived discrimination. Physicians displayed less positive affect, more negative affect, and less engagement when they interacted with patients who reported any (as opposed to no) incidence of prior discrimination. There were also significant two-way interactions between: (a) physician explicit bias and patient perceived discrimination and (b) physician implicit bias and patient perceived discrimination for all three measures. However, these main effects and two-way interactions were all qualified by the significant three-way interactions between physician implicit bias, physician explicit bias, and patient perceived discrimination. To better understand the significant three-way interactions, we assessed the simple slopes of physician explicit bias at different levels of physician implicit bias (±1 SD from the mean) separately for patients who report no prior discrimination in the past and those who reported any incidence of prior discrimination (Cohen, Cohen, West, & Aiken, 2003).
Table 2.
Estimates of fixed effects predicting physician behaviors.
| Physicians |
||||||
|---|---|---|---|---|---|---|
| Positive affect |
Negative affect |
Engagement |
||||
| B | SE | B | SE | B | SE | |
| Intercept | 6.28 | 0.16 | 1.82 | 0.07 | 7.18 | 0.15 |
| Physician explicit bias | −0.44 | 0.72 | 0.25 | 0.31 | −0.17 | 0.59 |
| Physician implicit bias | 0.49 | 0.67 | −0.18 | 0.24 | 0.24 | 0.57 |
| Patient perceived | −0.30** | 0.09 | 0.19** | 0.05 | −0.23* | 0.10 |
| discrimination | ||||||
| Exp x Discrim | 1.22* | 0.48 | −0.75** | 0.21 | 1.06* | 0.43 |
| Imp x Discrim | −0.91** | 0.27 | 0.60** | 0.16 | −0.80* | 0.32 |
| Exp x Imp | −0.50 | 0.99 | 0.50 | 0.48 | 0.20 | 0.73 |
| Exp x Imp x Discrim | 3.70** | 1.29 | −2.85** | 0.69 | 3.52* | 1.41 |
Note.
p < .10.
p < .05.
p < .01.
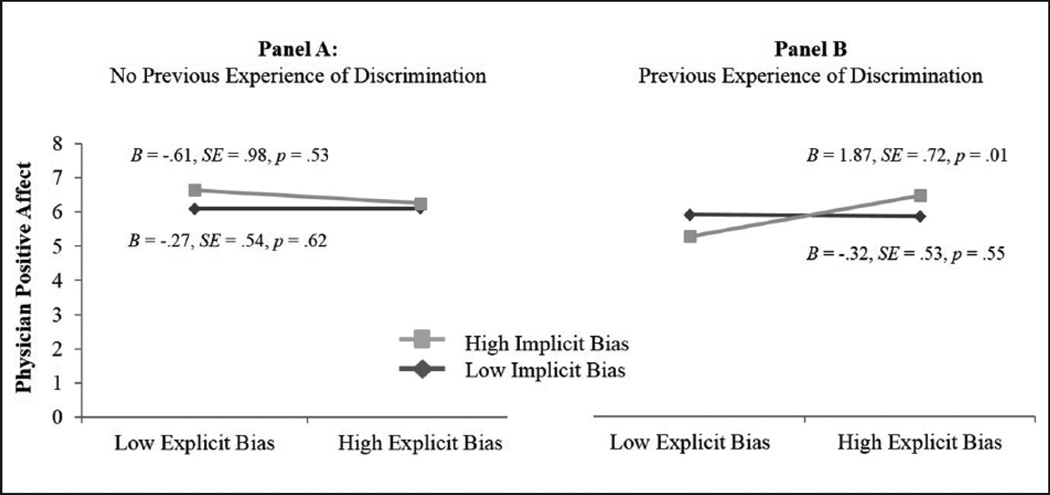
Positive affect
Figure 1 presents the significant three-way interaction involving physician positive affect. The analyses revealed that, when physicians interacted with Black patients who reported no prior discrimination (Panel A in Figure 1), the two-way interaction between explicit and implicit bias was not significant (B = −0.50, SE = 0.99, p = .61). Specifically, the simple main effect of explicit bias was nonsignificant whether physicians displayed lower (B = −0.27, SE = 0.54, p = .62) or higher (B = −0.61, SE = 0.98, p = .53) levels of implicit bias.
Figure 1.
A three-way interaction between physician explicit racial bias, physician implicit racial bias, and patient perceived discrimination predicting physician positive affect.
In contrast, when physicians interacted with patients who reported any incidence of prior discrimination (Panel B), the effects of physicians’ explicit bias on their positive affect differed depending on the level of implicit racial bias (B = 3.19, SE = 1.31, p < .05). That is, the level of positive affect for physicians who fit the aversive racist profile differed from the physicians who did not fit this profile. Specifically, for physicians with lower levels of implicit bias, there was no effect of explicit bias (B = −0.32, SE = 0.53, p = .55). In contrast, for physicians with higher levels of implicit bias, lower levels of explicit bias (i.e., aversive racists) were associated with significantly lower levels of positive affect (B = 1.87, SE = 0.72, p < .01). Thus, consistent with our predictions, when physicians who fit the aversive racist profile interacted with Black patients who reported any incidence of prior discrimination, they were rated by the observers as displaying less positive affect than the other physicians.
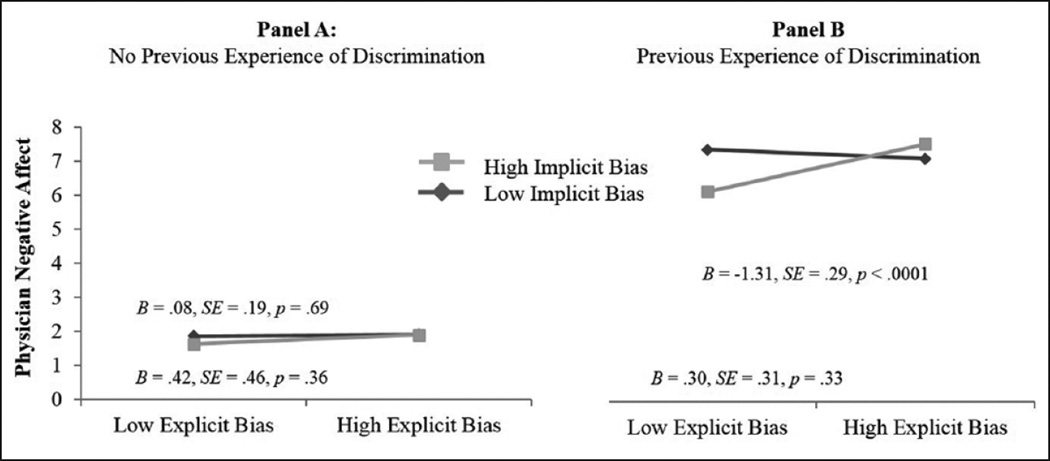
Negative affect
Figure 2 presents the significant three-way interaction predicting physician negative affect. The results showed that when the physicians interacted with patients who reported no prior discrimination (Panel A), aversive racist physicians did not differ from the other physicians. That is, the two-way interaction between physician implicit and explicit bias was not significant (B = 0.50, SE = 0.48, p = .30). Inspection of the individual slopes showed that physicians’ explicit bias did not have any effect on their negative affect, regardless of whether they reported lower (B = 0.08, SE = 0.19, p = .69) versus higher (B = 0.42, SE = 0.46, p = .36) levels of implicit bias.
Figure 2.
A three-way interaction between physician explicit racial bias, physician implicit racial bias, and patient perceived discrimination predicting physician negative affect.
In contrast, when physicians interacted with patients who reported any incidence of prior discrimination (Panel B), the two-way interaction was significant (B = −2.35, SE = 0.72, p < .001). Again, the interaction showed that aversive racists differed from the other physicians. Specifically, the effects of physician explicit bias on their negative affect differed depending on the levels of implicit bias. For physicians with lower levels of implicit racial bias, there was no effect of explicit bias (B = 0.30, SE = 0.31, p = .33). However, for physicians with higher levels of implicit bias, lower levels of explicit bias were associated with significantly higher levels of negative affect (B = −1.31, SE = 0.29, p < .0001).
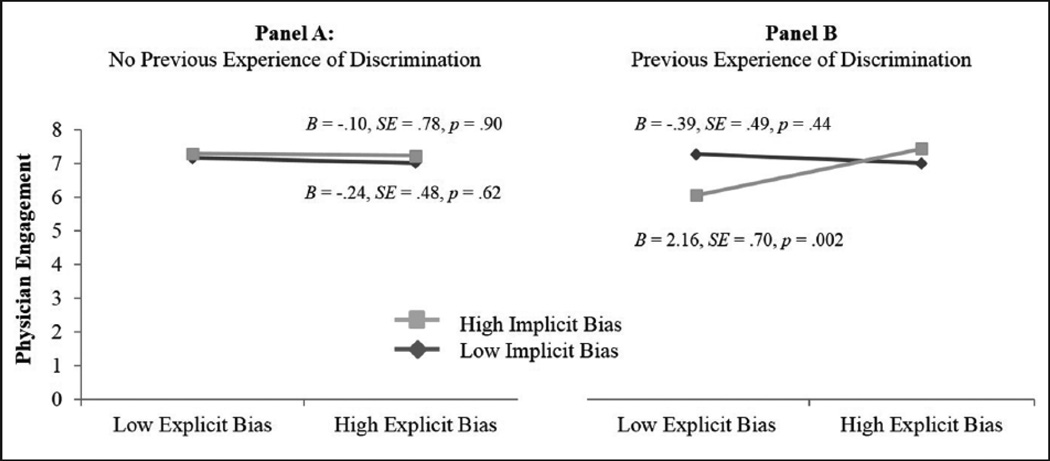
Engagement
Figure 3 presents the significant three-way interaction for physician engagement. When physicians interacted with the patients who reported no prior discrimination (Panel A), the simple interaction between physician explicit and implicit bias was not significant (B = 0.20, SE = 0.74, p = .78). Specifically, there was no effect of explicit bias on physician engagement, regardless of the levels of implicit bias (lower levels: B = −0.24, SE = 0.48, p = .62; higher levels: B = −0.10, SE = 0.78, p = .90).
Figure 3.
A three-way interaction between physician explicit racial bias, physician implicit racial bias, and patient perceived discrimination predicting physician engagement.
However, when physicians interacted with the patients who reported any incidence of prior discrimination (Panel B), the effects of physician explicit bias on their level of active engagement differed depending on the level of implicit bias (B = 3.72, SE = 1.40, p < .01). For physicians with lower levels of implicit bias, there was no association between their explicit bias and level of active engagement (B = −0.39, SE = 0.49, p = .44). In contrast, for physicians with higher levels of implicit bias, lower levels of explicit racial bias was associated with significantly lower levels of active engagement (B = 2.16, SE = 0.70, p < .01). That is, contrary to our predictions, when physicians who fit the aversive racist profile interacted with patients who reported any incidence of prior discrimination, they were rated as less engaged during the racially discordant medical interactions.
Black Patients
Contrary to our predictions, none of the higher order interactions were significant in the full models that examined patient affect and engagement. This lack of higher order interactions suggest that, unlike the findings with physician affect and engagement, patient perceived discrimination did not interact with physician racial bias to influence patient affect and engagement. However, some lower order main effects were significant in the full models. Thus, following Aiken and West’s (1991) suggestion, we conducted follow-up analyses in order to examine whether these significant lower order effects would remain significant after removing the nonsignificant higher order interaction terms from the full model. Table 3 presents only the estimates of fixed main effects that remained significant in these follow-up analyses.
Table 3.
Estimates of fixed effects predicting patient behaviors.
| Patients |
||||
|---|---|---|---|---|
| Positive affect |
Negative affect |
|||
| B | SE | B | SE | |
| Intercept | 6.21 | 0.10 | 2.04 | 0.04 |
| Physician explicit bias | −0.41† | 0.25 | 0.28† | 0.16 |
| Physician implicit bias | 0.06 | 0.20 | −0.10 | 0.12 |
| Patient perceived discrimination | −0.40* | 0.17 | 0.23* | 0.10 |
Note.
p ≤ .10.
p < .05.
Positive affect
The main effect of patient perceived discrimination was significant (B = −0.40, SE = 0.17, p < .05). Specifically, Black patients who reported any incidence of prior discrimination were rated as displaying significantly less positive affect than Black patients who reported no prior discrimination.
Negative affect
The main effect of patient perceived discrimination was also significant (B = 0.23, SE = 0.10, p < .05). Specifically, Black patients who reported any incidence of prior discrimination were rated as displaying significantly more negative affect than Black patients who reported no prior discrimination.
Engagement
Contrary to our predictions, there was no effect of patient perceived discrimination (B = −0.17, SE = 0.18, p = .37).
Discussion
It is now well-documented that both non-Black physicians’ racial bias and Black patients’ perceived discrimination are associated with the quality of racially discordant medical interactions. However, few studies have systematically investigated how they individually and jointly affect the behaviors of physicians and patients during such interactions. The present study addressed this gap in the literature by investigating the effects of physician racial bias and patient perceived discrimination on their own as well as one another’s behaviors.
Physician racial bias influenced their affect and engagement as rated by the observers. However, the effects are best understood by examining the significant three-way interactions that included physician explicit bias, physician implicit bias, and patient perceived discrimination. These interactions revealed that physicians’ racial bias had no significant effects on their affect and engagement when physicians interacted with patients who reported no prior discrimination. However, when physicians interacted with patients who reported any incidence of prior discrimination, physicians who fit the aversive racist profile (i.e., low explicit racial bias, high implicit racial bias) were rated by independent coders as displaying significantly less positive affect and more negative affect than physicians who did not fit this profile, including even those who were high in both explicit and implicit bias. This finding is conceptually consistent with Penner et al.’s (2010) findings that Black patients were least satisfied with their medical interactions with physicians who were classified as aversive racists compared to other physicians.
The present findings extend prior research on physician racial bias in racially discordant medical interactions in important ways. First, Black patients’ negative reactions to physicians with higher levels of bias that have been consistently reported in research have led researchers to assume that physician racial bias affects the manner in which physicians interact with their Black patients. The present research is the first, to the best of our knowledge, to study physician behaviors in racially discordant behaviors. We found that naïve observers could reliably detect changes in the valence of the affect certain physicians displayed as a function of the nature of the physicians’ racial attitudes. More importantly, however, the present findings provide much more precise information about when physician racial bias may affect their behaviors in racially discordant medical interactions. The three-way interactions among physician implicit racial bias, physician explicit racial bias, and patient perceived discrimination strongly suggest it is when their Black patients also have negative racial orientations related to some degree of perceived discrimination. This indicates that Black patients are not passive participants in racially discordant medical interactions, but rather may behave in ways that influence physicians’ affect. However, this is most likely to occur among physicians who fit the aversive racist profile.
The results obtained in this highly consequential real-world setting are quite consistent with experimental research on aversive racism. Aversive racists do not believe they are biased or racist individuals. However, according to theories of contemporary racial bias (Crandall & Eshleman, 2003; Dovidio & Gaertner, 2004), aversive racists are more likely to express their bias in contexts where there is an alternative, nonracial explanation for the negative behaviors toward Blacks. In the context of the present study, acting negatively toward a patient who is also acting negatively would not represent an obvious instance of racial bias to independent observers, or more importantly the physician him/herself. Thus, in essence, patients might have given the physicians who fit the aversive racist profile “license” to react more negatively.
Our hypotheses about the impact of Black patients’ perceived discrimination on their own positive and negative affect were also supported. That is, independent observers rated the patients who reported any incidence of prior discrimination as displaying less positive affect and more negative affect than patients who did not report any prior discrimination. However, in contrast to the results for physicians, no joint effects of physician racial bias and patient perceived discrimination on patient affect were observed. This may potentially be due to rather pervasive mistrust of the healthcare system among Black patients. Irrespective of specific experiences with discrimination, Black patients tend to mistrust the healthcare system and non-Black physicians (Benkert, Peters, Clark, & Keves-Foster, 2006; Dovidio et al., 2008; Halbert et al., 2006). Because of pervasive mistrust among Black patients, it may have been harder for the physicians to change the valence of the feelings the Black patients brought with them to the interaction. That is, even when their physicians were displaying positive affect, Black patients’ general levels of mistrust may have made their affective state during the interaction less context dependent.
There were other unexpected or null findings. In terms of physicians, contrary to our predictions, the physicians who fit the aversive racist profile were rated as less engaged than the other physicians when they interacted with the patients who reported any incidence of prior discrimination. One explanation is that engagement and affect were conflated. Note the measures of engagement and positive affect are strongly, positively correlated (rs = .87 and .86 for physicians and patients, respectively), whereas the measures of engagement and negative affect are strongly, negatively correlated (rs = −.80 and −.71 for physicians and patients, respectively). Thus, our measure of engagement may actually have been simply another aspect of affect. Another tentative explanation is predicated on research that finds that attempts made by Whites with higher levels of implicit racial bias to prevent or suppress expressions of their bias place increased demand on individuals’ executive function (Pearson, Dovidio, Phills, & Onyeador, 2013; Trawalter & Richeson, 2006). This could have produced lower levels of social engagement among the aversive racist physicians, who are particularly motivated to suppress their prejudice (Dovidio & Gaertner, 2004).
With respect to patients, we did not observe any significant effects of physician implicit or explicit racial bias on their engagement. This null effect was not expected: Perceiving higher levels of past discrimination has been found to be associated with higher levels of Black patients’ participation in clinical interactions (Cooper et al., 2012; Hagiwara, Penner, Gonzalez, Eggly, et al., 2013). Given the significant results for physicians’ engagement, this null effect is not easily attributable to the insensitivity of our measure of engagement. However, it is possible that our measure of engagement may not sufficiently consider the different ways physicians and patients manifest engagement. For example, members of socially disadvantaged groups often exert their influence more indirectly than members of socially advantaged groups and those high in situational power (Dovidio, Brown, Keating, Heltman, & Ellyson, 1988; Keltner, van Kleef, Chen, & Kraus, 2008). Thus, future research might assess engagement in more nuanced ways, perhaps distinguishing between different forms of engagement.
Limitations
One potential limitation of this study is that the majority of the non-Black physicians in the current study self-identified as Asian, as is typical of the racial/ethnic distribution of physicians in primary clinics in low-income, residentially segregated communities in the United States (Hing & Lin, 2009; Mertz et al., 2007). However, we do not think this reduces the importance or generalizability of the current findings. First, prior research has shown that the level of implicit bias toward Blacks is comparable among White, Asian, and Hispanic physicians (Sabin et al., 2009). Second, Cooper et al. (2012) found that the effects of physicians’ racial bias toward Blacks on their own verbal dominance and patient ratings of their interpersonal care were similar for White and Asian physicians. Third, the findings of the previous studies using this sample of physicians (Hagiwara, Penner, Gonzalez, Eggly, et al., 2013; Penner et al., 2010) are highly consistent with the results of studies that have used predominantly White samples of physicians (e.g., Blair et al., 2013; Cooper et al., 2012). Finally, and perhaps most importantly, the associations between the physicians’ racial bias and their behaviors were reliably detected by naïve non-Asian observers. We certainly would not discount the potential racial/cultural impacts on when and how affect is expressed. However, the fact remains that the observers were able to reliably identify the affect that was displayed in a manner that was consistent with prior work on the ways aversive racism is manifested during interracial interactions. Still, generalizability is an empirical question, and future studies with larger numbers of physicians who self-identify as White are encouraged.
A related limitation is the absence of racially concordant medical interactions involving non-Black patients in the sample. Without such comparison group, we cannot rule out the possibility that the present results reflect non-race-related factors which may covary with racial bias, such as social dominance orientation or right-wing authoritarianism (Esses & Hodson, 2006; Pratto, Sidanius, Stallworth, & Malle, 1994). That is, the results could be due to general social orientation rather than racial bias. We note, however, that other studies of physician general implicit racial bias have found that physicians’ general implicit racial bias has quite different effects on Black and White patients (Blair et al., 2013; Cooper et al., 2012; Schaa et al., 2015). For example, Cooper et al. (2012) reported:
In contrast to consistent negative findings for Blacks, the effect of implicit race attitudes for White patients is largely, although not exclusively, positive. As implicit race bias increases, White patients report being more respected and liked, and as implicit compliance stereotyping increases, coders rate the communication in their visits as more patient centered, less verbally dominant, and higher in clinician positive affect. (p. 983)
The only negative influences of physician bias common to both White and Black patients Cooper et al. reported was greater physician verbal dominance and less involvement of patients in treatment decisions. However, neither Blair et al. (2013) nor Schaa et al. (2015) found this latter effect of racial bias with White patients.
Next potential limitation concerns the measure of perceived discrimination. Patients completed it before the interactions. Thus, the measure may have served to prime feelings of discrimination among some patients, which may not have normally been present in medical interactions. We acknowledge this possibility, but we believe that giving the measure before the interactions was preferable to giving it afterwards, which have raised serious questions about causality. Further, we note the seven-item perceived discrimination measure was embedded in a 90-item baseline questionnaire, which makes such priming unlikely.
Another limitation is that the significant patient effects were found for a binary part of the measure of their perceived discrimination (i.e., report of no prior discrimination vs. report of any incidence of prior discrimination) but not for a continuous part. In trying to understand this difference, we first note that the continuous part of the perceived discrimination measure contained fewer cases, and thus there was much less power in the analyses, especially in the three-way interactions. However, beyond these statistical explanations, differences in the psychological meaning of the two parts of the measure may account for their different degree of impact. Whether or not people perceived themselves as a target of discrimination has been found to play a significant role in how they perceive others and themselves (e.g., Crocker & Major, 1989; Hatzenbuehler, 2009; Vorauer, 2006). That is, the distinction between perceiving that one has or has not been victimized by racial discrimination (i.e., the binary part of the perceived discrimination measure) may fundamentally affect Black patients’ behavior toward non-Black physicians, whom as a group may be perceived to be perpetuators of discrimination. In contrast, the continuous part may represent mainly gradations in the degree to which discrimination has been experienced. This post hoc explanation might be tested in future research that identifies the correlates of the two aspects of perceived discrimination.
Another limitation in the present study is that observers were able to see both physicians and patients in the video clips even though they were instructed to only focus on either the physician or the patient within a given video clip when they were rating affect and communication style. Thus, the observers had access to the patient’s behaviors when they were rating physicians’ behaviors, and vice versa. This might have resulted in the overestimated level of interdependence between physicians and patients in the present study. However, it should be noted that the joint effect of physician racial bias and patient perceived discrimination was observed only in the ratings of physician affect and engagement. No such effects were found for patient affect and engagement. If the observers were taking both dyad members’ behaviors into account when rating one member’s affect and communication style, the perception of such interdependence should have been also manifested in the ratings of patient affect and communication style. Nonetheless, it is important to empirically examine whether the present findings can be replicated in a future study in which observers can only see either physicians or patients in video clips when rating affect and communication style.
Finally, it is still unclear exactly what kinds of specific behaviors are contributing to ratings of affect and engagement because the thin slice method relies on raters’ global ratings. From both theoretical and clinical perspectives, it is important to identify which specific macro and/or micro behaviors are related to the displays of affect in interracial interactions. This will further basic researchers’ understanding of the dynamics of interactions between members of different racial/ethnic groups. Such understanding will, in turn, give researchers opportunities to develop interventions that could improve patient–physician communication during racially discordant medical interactions by targeting specific physician and patient behaviors.
Despite these potential limitations, we believe that the current study contributes substantially to a further understanding of racial disparities in healthcare. First, the present study demonstrated that physicians’ racial bias and patients’ perceived discrimination affect the dynamics of racially discordant medical interactions at least partially through their impact on behaviors that reflect positive and negative affect. Second, this is the first study, to our knowledge, to demonstrate the joint effects of physician racial bias and patient perceived discrimination on physician behaviors during racial discordant medical interactions. The present study, thus, clearly documents that physician racial bias and patient perceived discrimination individually and jointly influence the dynamics of racially discordant medical interaction. These dynamics can play a significant role in healthcare disparities and ultimately the health of racial/ethnic minority group members.
Acknowledgments
Funding
This research was supported by an National Institute of Nursing Research (NINR) grant (1R03NR013249– 01) to the first author, an National Institute of Child Health and Human Development (NICHD) grant (1R21HD050445001A1) to the last author, and a National Cancer Institute (NCI) grant (U01CA114583) to the Karmanos Cancer Institute, Wayne State University.
Footnotes
Twenty-three out of 113 patients (20.4%) reported experiencing unfair treatment in a medical setting. The results did not change even after excluding the patients who reported incidence of unfair treatment in the medical setting.
To ensure that the exclusion of these two items from the composite measures of positive and negative affect for the first 27 patients did not somehow bias the results, we did ancillary analyses in which “cheerful” and “stressed” were excluded from all observers’ ratings of patients and new estimates were computed and subjected to analyses. The results remained the same after excluding these items from the composites. Thus, we report findings for all patients.
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA: Sage; 1991. [Google Scholar]
- Ambady N, Bernieri FJ, Richeson JA. Toward a histology of social behavior: Judgmental accuracy from thin slices of the behavioral stream. In: Zanna MP, editor. Advances in experimental social psychology. Vol. 32. San Diego, CA: Academic Press; 2000. pp. 201–272. [Google Scholar]
- Ambady N, Hallahan M, Rosenthal R. On judging and being judged accurately in zero-acquaintance situations. Journal of Personality and Social Psychology. 1995;69:518–529. [Google Scholar]
- Ambady N, Koo J, Rosenthal R, Winograd C. Physical therapists’ nonverbal communication predicts geriatric patients’ health outcomes. Psychology and Aging. 2002;17:443–452. doi: 10.1037/0882-7974.17.3.443. [DOI] [PubMed] [Google Scholar]
- Ambady N, Laplante D, Nguyen T, Rosenthal R, Chaumeton N, Levinson W. Surgeons’ tone of voice: A clue to malpractice history. Surgery. 2002;132:5–9. doi: 10.1067/msy.2002.124733. [DOI] [PubMed] [Google Scholar]
- Ambady N, Rosenthal R. Thin slices of expressive behavior as predictors of interpersonal consequences: A meta-analysis. Psychological Bulletin. 1992;111:256–274. [Google Scholar]
- Benkert R, Hollie B, Nordstrom CK, Wickson B, Bins-Emerick L. Trust, mistrust, racial identity and patient satisfaction in urban African American primary care patients of nurse practitioners. Journal of Nursing Scholarship. 2009;41:211–219. doi: 10.1111/j.1547-5069.2009.01273.x. [DOI] [PubMed] [Google Scholar]
- Benkert R, Peters RM, Clark R, Keves-Foster K. Effects of perceived racism, cultural mistrust and trust in providers on satisfaction with care. Journal of the National Medical Association. 2006;98:1532–1540. [PMC free article] [PubMed] [Google Scholar]
- Bergsieker HB, Shelton JN, Richeson JA. To be liked versus respected: Divergent goals in interracial interactions. Journal of Personality and Social Psychology. 2010;99:248–264. doi: 10.1037/a0018474. [DOI] [PubMed] [Google Scholar]
- Blair IV, Steiner JF, Fairclough DL, Hanratty R, Price DW, Hirsh HK, Havranek EP. Clinicians’ implicit ethnic/racial bias and perceptions of care among Black and Latino patients. Annals of Family Medicine. 2013;11:43–52. doi: 10.1370/afm.1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brigham JC. College students’ racial attitudes. Journal of Applied Social Psychology. 1993;23:1933–1967. [Google Scholar]
- Brown TN. Measuring self-perceived racial and ethnic discrimination in social surveys. Sociological Spectrum. 2001;21:377–392. [Google Scholar]
- Cameron AC, Trivedi PK. Regression analysis of count data. Cambridge, UK: Cambridge University Press; 1998. [Google Scholar]
- Cohen J, Cohen PC, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3rd. Mahwah, NJ: Lawrence Erlbaum; 2003. [Google Scholar]
- Cooper LA, Roter DL, Carson KA, Beach MC, Sabin JA, Greenwald AG, Inui TS. The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. American Journal of Public Health. 2012;102:979–987. doi: 10.2105/AJPH.2011.300558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crandall CS, Eshleman A. A justification-suppression model of the expression and experience of prejudice. Psychological Bulletin. 2003;129:414–446. doi: 10.1037/0033-2909.129.3.414. [DOI] [PubMed] [Google Scholar]
- Crocker J, Major B. Social stigma and self-esteem: The self-protective properties of stigma. Psychological Review. 1989;96:608–630. [Google Scholar]
- Dovidio JF, Brown CE, Keating CF, Heltman K, Ellyson SL. Power displays between women and men in discussions of gender-linked tasks: A multichannel study. Journal of Personality and Social Psychology. 1988;55:580–587. doi: 10.1037//0022-3514.54.2.233. [DOI] [PubMed] [Google Scholar]
- Dovidio JF, Gaertner SL, editors. Aversive racism. San Diego, CA: Academic Press; 2004. [Google Scholar]
- Dovidio JF, Kawakami K, Gaertner L. Implicit and explicit prejudice and interacial interaction. Journal of Personality and Social Psychology. 2002;82:62–68. doi: 10.1037//0022-3514.82.1.62. [DOI] [PubMed] [Google Scholar]
- Dovidio JF, Penner LA, Albrecht TL, Norton WE, Gaertner SL, Shelton JN. Disparities and distrust: The implications of psychological processes for understanding racial disparities in health and health care. Social Science & Medicine. 2008;67:478–486. doi: 10.1016/j.socscimed.2008.03.019. [DOI] [PubMed] [Google Scholar]
- Epstein RM, Street RL. Patient-centered communication in cancer care: Promoting healing and reducing suffering. Bethesda, MD: National Cancer Institute; 2007. [Google Scholar]
- Esses VM, Hodson G. The role of lay perceptions of ethnic prejudice in the maintenance and perpetuation of ethnic bias. Journal of Social Issues. 2006;62:453–468. [Google Scholar]
- Green AR, Carney DR, Pallin DJ, Ngo LH, Raymond KL, Iezzoni LI, Banaji MR. Implicit bias among physicians and its predictions of thrombolysis decisions for Black and White patients. Journal of General Internal Medicine. 2007;22:1231–1238. doi: 10.1007/s11606-007-0258-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwald AG, McGhee DE, Schwartz JLK. Measuring individual differences in implicit cognition: The Implicit Association Test. Journal of Personality and Social Psychology. 1998;74:1464–1480. doi: 10.1037//0022-3514.74.6.1464. [DOI] [PubMed] [Google Scholar]
- Greenwald AG, Nosek BA, Banaji MR. Understanding and using the Implicit Association Test: I. An improved scoring algorithm. Journal of Personality and Social Psychology. 2003;85:197–216. doi: 10.1037/0022-3514.85.2.197. [DOI] [PubMed] [Google Scholar]
- Greenwald AG, Poehlman TA, Uhlmann E, Banaji MR. Understanding and using the Implicit Association Test: III. Meta-analysis of predictive validity. Journal of Personality and Social Psychology. 2009;97:17–41. doi: 10.1037/a0015575. [DOI] [PubMed] [Google Scholar]
- Hagiwara N, Penner LA, Gonzalez R, Albrecht TL. Within-group health disparities among Blacks: The effects of Afrocentric features and unfair treatment. Cultural Diversity and Ethnic Minority Psychology. 2013;19:477–480. doi: 10.1037/a0032566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagiwara N, Penner LA, Gonzalez R, Eggly S, Dovidio JF, Gaertner SL, Albrecht TL. Racial attitudes, physician-patient talk time ratio, and adherence in racially discordant medical interactions. Social Science & Medicine. 2013;87:123–131. doi: 10.1016/j.socscimed.2013.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagiwara N, Slatcher R, Eggly S, Penner LA. Physician racial bias and word use during racially discordant medical interactions. Health Communication. doi: 10.1080/10410236.2016.1138389. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halbert CH, Armstrong K, Gandy OH, Shaker L. Racial differences in trust in health care providers. Archives of Internal Medicine. 2006;166:896–901. doi: 10.1001/archinte.166.8.896. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML. How does sexual minority stigma get “under the skin”? A psychological mediation framework. Psychological Bulletin. 2009;135:707–730. doi: 10.1037/a0016441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hing E, Lin S. Role of international medical graduates providing office-based medical care: United States, 2005–2006 (NCHS Data Brief No. 13) 2009 Retrieved from http://www.cdc.gov/nchs/data/databriefs/db13.pdf. [PubMed]
- Hofmann W, Gawronski B, Gschwendner T, Le H, Schmitt M. A meta-analysis on the correlation between the Implicit Association Test and explicit self-report measures. Personality and Social Psychology Bulletin. 2005;31:1369–1385. doi: 10.1177/0146167205275613. [DOI] [PubMed] [Google Scholar]
- Jarvis BG. MediaLab (Version 2012) New York, NY: Empirisoft Corporation; 2012. [Google Scholar]
- Johnson JD, Ashburn-Nardo L, Spicer CV, Dovidio JF. The role of Blacks’ discriminatory expectations on prosocial orientations towards Whites and Blacks. Journal of Experimental Social Psychology. 2008;44:1498–1505. [Google Scholar]
- Johnson RL, Roter D, Powe NR, Cooper LA. Patient race/ethnicity and quality of patient-physician communication during medical visits. American Journal of Public Health. 2004;94:2084–2090. doi: 10.2105/ajph.94.12.2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keltner D, van Kleef GA, Chen S, Kraus M. A reciprocal influence model of social power: Emerging principles and lines of inquiry. Advances in Experimental Social Psychology. 2008;40:151–192. [Google Scholar]
- Kunda Z, Davies PG, Adams BD, Spencer SJ. The dynamic time course of stereotype activation: Activation, dissipation, and resurrection. Journal of Personality and Social Psychology. 2002;82:283–299. doi: 10.1037//0022-3514.82.3.283. [DOI] [PubMed] [Google Scholar]
- Malat J, Hamilton MA. Preference for same-race health care providers and perceptions of interpersonal discrimination in health care. Journal of Health and Social Behavior. 2006;47:173–187. doi: 10.1177/002214650604700206. [DOI] [PubMed] [Google Scholar]
- McConahay JB. Modern racism, ambivalence, and the Modern Racism Scale. In: Dovidio JF, Gaertner SL, editors. Prejudice, discrimination, and racism. San Diego, CA: Academic Press; 1986. pp. 91–125. [Google Scholar]
- Mendez DD, Hogan VK, Culhane JF. Institutional racism, neighborhood factors, stress, and preterm birth. Ethnicity & Health. 2013;19:479–499. doi: 10.1080/13557858.2013.846300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendoza-Denton R, Downey G, Purdie VJ, Davis A, Pietrzak J. Sensitivity to status-based rejection: Implications for African American students’ college experience. Journal of Personality and Social Psychology. 2002;83:896–918. doi: 10.1037//0022-3514.83.4.896. [DOI] [PubMed] [Google Scholar]
- Mertz E, Jain R, Breckler J, Chen E, Grumbach K. Foreign versus domestic education of physicians for the United States: A case study of physicians of South Asian ethnicity in California. Journal of Health Care for the Poor and Underserved. 2007;18:984–993. doi: 10.1353/hpu.2007.0100. [DOI] [PubMed] [Google Scholar]
- Murphy NA. Using thin slices for behavioral coding. Journal of Nonverbal Behavior. 2005;29:235–246. [Google Scholar]
- Pearson AR, Dovidio JF, Phills CE, Onyeador IN. Attitude-goal correspondence and interracial interaction: Implications for executive function and impression formation. Journal of Experimental Social Psychology. 2013;49:907–914. [Google Scholar]
- Penner LA, Dovidio JF, Edmondson D, Dailey RK, Markova T, Albrecht TL, Gaertner SL. The experience of discrimination and Black-White health disparities in medical care. Journal of Black Psychology. 2009;35:180–203. doi: 10.1177/0095798409333585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penner LA, Dovidio JF, West TV, Gaertner SL, Albrecht TL, Dailey RK, Markova T. Aversive racism and medical interactions with Black patients: A field study. Journal of Experimental Social Psychology. 2010;46:436–440. doi: 10.1016/j.jesp.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penner LA, Gaertner S, Dovidio JF, Hagiwara N, Porcerelli J, Markova T, Albrecht TL. A social psychological approach to improving the outcomes of racially discordant medical interactions. Journal of General Internal Medicine. 2013;28:1143–1149. doi: 10.1007/s11606-013-2339-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pratto F, Sidanius J, Stallworth LM, Malle BF. Social dominance orientation: A personality variable predicting social and political attitudes. Journal of Personality and Social Psychology. 1994;67:741–763. [Google Scholar]
- Rosenblum ND, Wetzel M, Platt O, Daniels S, Crawford J, Rosenthal R. Predicting medical student success in a clinical clerkship by rating students’ nonverbal behavior. Archives of Pediatrics & Adolescent Medicine. 1994;148:213–219. doi: 10.1001/archpedi.1994.02170020099020. [DOI] [PubMed] [Google Scholar]
- Roter D, Larson S. The Roter interaction analysis system (RIAS): Utility and flexibility for analysis of medical interactions. Patient Education and Counseling. 2002;46:243–251. doi: 10.1016/s0738-3991(02)00012-5. [DOI] [PubMed] [Google Scholar]
- Sabin JA, Nosek BA, Greenwald AG, Rivara FP. Physicians’ implicit and explicit attitudes about race by MD race, ethnicity, and gender. Journal of Health Care for the Poor and Under-served. 2009;20:896–913. doi: 10.1353/hpu.0.0185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaa KL, Roter DL, Biesecker BB, Cooper LA, Erby LH. Genetic counselors’ implicit racial attitudes and their relationship to communication. Health Psychology. 2015;34:111. doi: 10.1037/hea0000155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shavers VL, Fagan P, Jones D, Klein WM, Boyington J, Moten C, Rorie E. The state of research on racial/ethnic discrimination in the receipt of health care. American Journal of Public Health. 2012;102:953–966. doi: 10.2105/AJPH.2012.300773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shelton JN. Interpersonal concerns in social encounters between majority and minority group members. Group Processes & Intergroup Relations. 2003;6:171–185. [Google Scholar]
- Shelton JN, Richeson JA. Interracial interactions: A relational approach. Advances in Experimental Social Psychology. 2006;38:121–181. [Google Scholar]
- Shelton JN, Richeson JA, Salvatore J, Trawalter S. Ironic effects of racial bias during racially discordant interactions. Psychological Science. 2005;16:397–402. doi: 10.1111/j.0956-7976.2005.01547.x. [DOI] [PubMed] [Google Scholar]
- Shelton JN, Richeson J, Vorauer JD. Threatened identities and interethnic interactions. European Review of Social Psychology. 2006;17:321–358. [Google Scholar]
- Siminoff LA, Graham GC, Gordon NH. Cancer communication patterns and the influence of patient characteristics: Disparities in information-giving and affective behaviors. Patient Education and Counseling. 2006;62:355–360. doi: 10.1016/j.pec.2006.06.011. [DOI] [PubMed] [Google Scholar]
- Smedley BD, Stith AY, Nelson AR. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- Trawalter S, Richeson JA. Regulatory focus and executive function after interracial interactions. Journal of Experimental Social Psychology. 2006;42:406–412. [Google Scholar]
- Vorauer JD. An information search model of evaluative concerns in intergroup interaction. Psychological Review. 2006;113:862–886. doi: 10.1037/0033-295X.113.4.862. [DOI] [PubMed] [Google Scholar]
- Weisbuch M, Ambady N. Thin slice vision. In: Adams JRB, Ambady N, Nakayama K, Shimojo S, editors. Social vision. Oxford, UK: Oxford University Press; 2011. pp. 228–247. [Google Scholar]
- Wilson TD, Lindsey S, Schooler TY. A model of dual attitudes. Psychological Review. 2000;107:101–126. doi: 10.1037/0033-295x.107.1.101. [DOI] [PubMed] [Google Scholar]