Abstract
Lithium is frequently used in the management of bipolar affective disorders. It has a narrow therapeutic index and can cause acute or chronic intoxication. Toxic symptoms may be present even when concentrations are within the recommended therapeutic range. We believe that lithium intoxication is a very important issue for a physician. In this report, we aimed to evaluate the pathophysiological view of two chronic lithium intoxication cases accompanied by hyponatremia.
Keywords: Hyponatremia, intoxication, lithium
Introduction
Lithium is frequently used in the management of bipolar affective disorders. It has a narrow therapeutic index, between 0.6 and 1.5 mmol L−1 (1). Lithium intoxication can occur acutely or chronically and toxic symptoms may be present even when concentrations are within the recommended therapeutic range. We aimed to evaluate the pathophysiological view of two chronic lithium intoxication cases accompanied by hyponatremia.
Case Presentation
After informed consents were obtained, two chronic lithium intoxication cases were reported. The first case is of a 56-year-old woman who had used lithium (300 mg capsules four times a day) for the treatment of bipolar affective disorder for 15 years. She was admitted to emergency unit with a loss of appetite, nausea, vomiting, confusion, myoclonic twitches and unexpected aimless behaviour. Her vital values were normal. The routine laboratory workout showed the following serum concentrations: lithium, 2.7 mmol L−1; sodium, 129 mmol L−1; blood urea nitrogen (BUN), 67 mg dL−1 and creatinine, 1.71 mg dL−1. The patient was admitted to the intensive care unit (ICU) with the diagnosis of lithium intoxication, acute renal failure and hyponatremia. Lithium was stopped and volume resuscitation was started with normal saline, and haemodialysis was carried out for 4 h. After haemodialysis, her confusion and myoclonic twitches decreased, the concentration of serum lithium dropped to 1.09 mmol L−1. On the second day, her cooperation was perfect and myoclonic twitches recovered. The laboratory tests showed the following serum concentrations: lithium, 1.3 mmol L−1; sodium, 134 mmol L−1; BUN, 27 mg dL−1 and creatinine, 1 mg dL−1. On the third day, she was completely normal, and the serum lithium concentration was 1.1 mmol L−1. On the fourth day the serum lithium concentration was 0.8 mmolL−1 and serum sodium concentration was 140 mmol L−1 (Figure 1). She was discharged from the hospital for a follow up with a psychiatrist.
Figure 1.
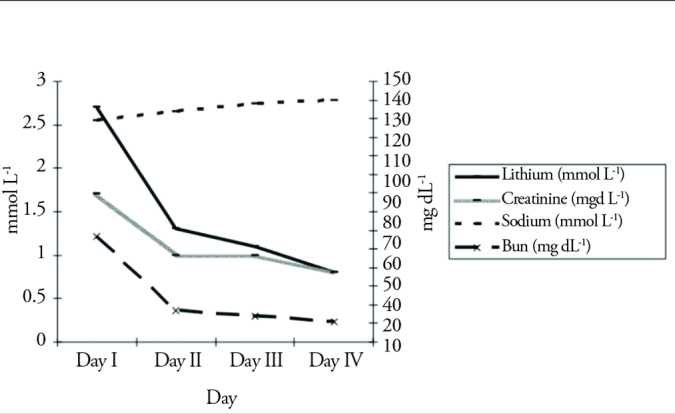
The laboratory values of the first patient
The second case is of a 39-year-old man who had used lithium (300 mg capsules three times a day) for the treatment of bipolar affective disorder for 6 years. He was admitted to the emergency unit with nausea, vomiting and confusion. The routine laboratory tests showed the following serum concentrations: lithium, 2.0 mmol L−1 and sodium, 131 mmol L−1. Other laboratory tests were normal. He was admitted to the ICU with the diagnosis of lithium intoxication and hyponatremia. Lithium was stopped and volume resuscitation was started with normal saline. On the second day, his lithium and sodium levels were 1.4 and 135 mmol L−1, respectively, and clinical symptoms had recovered. On the third day, he was discharged from the hospital for a follow up with a psychiatrist.
Discussion
Under normal physiological conditions the sodium (Na+)/hydrogen (H+) exchange protein is responsible for lithium transport into cells, the transport rate is 2-fold slower for lithium than sodium, and it is present in many cells in the body e.g. proximal tubules (2–4). Lithium transport into cells is a kind of a facilitated transport; however, lithium transport out of cells needs active transport involving the assistance of the Na+-potassium (K+) ATPase pump. The pathways for transporting lithium out of cells are more limited, resulting in intracellular lithium accumulation (5). All these mechanisms show that hyponatremia facilitates lithium intoxication. The long term use of lithium salts might have influenced the sodium levels of our patients, and the hyponatremic blood level may have caused lithium intoxication (6).
Volume depletion also increases renal lithium reabsorption and serum lithium levels (6). Concomitant medications such as diuretics, angiotensin-converting enzyme inhibitors and nonsteroidal anti-inflammatory drugs that alter glomerular filtration rates may cause lithium accumulation in the body (7). It has been documented that interactions between lithium and psychotropic medications such as thioridazine, chlorpromazine, clozapine and risperidone (7). There were no co-morbid diseases and used medications in our patients.
Besides other vital parameters, blood pressure and electrocardiography should be monitored in lithium intoxication. Cardiac arrhythmias of bradycardia, ventricular dysfunction, asystole and myocardial infarction are known adverse effects of lithium intoxication (8). Our patients did not present any cardiac side effect.
Volume resuscitation with normal saline has to be the first treatment step of chronic lithium intoxication, and hemodialysis should be performed in any patient with lithium intoxication who present with coma, convulsions, respiratory failure, deteriorating mental status or renal failure (9). The presence of coma with hyponathremia behave us to be with an approach of hemodialysis in the first patient. Lithium has a relatively small molecular weight, and thus, can be easily removed with standard or high-flux haemodialysis. The sequential use of haemodialysis followed by hemofiltration results in the further elimination of lithium in the extended-release lithium intoxication (10, 11). Renal replacement therapy should be continued until the symptoms of the central nervous system recover and lithium levels reduce to the recommended therapeutic range (9). After initiating haemodialysis, lithium levels must be frequently checked. We checked serum lithium levels after haemodialysis and daily intervals. Gastric lavage and whole bowel irrigation with polyethylene glycol are other treatment options for acute and extended-release lithium intoxication due to continued lithium absorption from the gastrointestinal tract (9).
Another side effect of lithium is nephrogenic diabetes insipidus, with an estimated prevalence of 20%–70% (9). These patient present polyuria, polydipsia, inability to concentrate their urine and hypernatremia. Choosing of the right replacement fluid in chronic lithium intoxication with diabetes insipidus should be performed according to serum sodium levels (9).
Conclusion
Chronic lithium intoxication is a life threatening, severe situation. Hyponatremia is a facilitating factor of lithium intoxication. Serum sodium levels should be regularly checked with serum lithium.
Footnotes
Informed Consent: Written informed consent was obtained from patient who participated in this case.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - Ö.K.D., İ.H., A.E., M.B.; Design - Ö.K.D., İ.H., A.E., M.B.; Supervision - Ö.K.D., İ.H., A.E., M.B.; Resources - M.B.; Data Collection and/or Processing - Ö.K.D., İ.H., A.E., M.B.; Analysis and/or Interpretation - Ö.K.D., İ.H., A.E., M.B.; Writing Manuscript - Ö.K.D.; Critical Review - M.B.; Other - Ö.K.D., İ.H., A.E., M.B.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Decker BS, Goldfarb DS, Dargan PI, Friesen M, Gosselin S, Hoffman RS, et al. Extracorporeal Treatment for Lithium Poisoning: Systematic Review and Recommendations from the EXTRIP Workgroup. Clin J Am Soc Nephrol. 2015;10:875–87. doi: 10.2215/CJN.10021014. http://dx.doi.org/10.2215/CJN.10021014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alsady M, Baumgarten R, Deen PM, de Groot T. Lithium in the Kidney: Friend and Foe? J Am Soc Nephrol. 2016;27:1587–95. doi: 10.1681/ASN.2015080907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Holstein-Rathlou NH. Lithium transport across biological membranes. Kidney Int Suppl. 1990;28:S4–9. [PubMed] [Google Scholar]
- 4.Greger R. Possible sites of lithium transport in the nephron. Kidney Int Suppl. 1990;28:S26–30. [PubMed] [Google Scholar]
- 5.Rej S, Herrmann N, Shulman K. The effects of lithium on renal function in older adults--a systematic review. J Geriatr Psychiatry Neurol. 2012;25:51–61. doi: 10.1177/0891988712436690. http://dx.doi.org/10.1177/0891988712436690. [DOI] [PubMed] [Google Scholar]
- 6.Bennett WM. Drug interactions and consequences of sodium restriction. Am J Clin Nutr. 1997;65:678S–81S. doi: 10.1093/ajcn/65.2.678S. [DOI] [PubMed] [Google Scholar]
- 7.Chen KP, Shen WW, Lu ML. Implication of serum concentration monitoring in patients with lithium intoxication. Psychiatry Clin Neurosci. 2004;58:25–9. doi: 10.1111/j.1440-1819.2004.01188.x. http://dx.doi.org/10.1111/j.1440-1819.2004.01188.x. [DOI] [PubMed] [Google Scholar]
- 8.Puhr J, Hack J, Early J, Price W, Meggs W. Lithium overdose with electrocardiogram changes suggesting ischemia. J Med Toxicol. 2008;4:170–2. doi: 10.1007/BF03161196. http://dx.doi.org/10.1007/BF03161196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Timmer RT, Sands JM. Lithium intoxication. J Am Soc Nephrol. 1999;10:666–74. doi: 10.1681/ASN.V103666. [DOI] [PubMed] [Google Scholar]
- 10.van Bommel EF, Kalmeijer MD, Ponssen HH. Treatment of life-threatening lithium toxicity with high-volume continuous venovenous hemofiltration. Am J Nephrol. 2000;20:408–11. doi: 10.1159/000013627. http://dx.doi.org/10.1159/000013627. [DOI] [PubMed] [Google Scholar]
- 11.Meyer RJ, Flynn JT, Brophy PD, Smoyer WE, Kershaw DB, Custer JR, et al. Hemodialysis followed by continuous hemofiltration for treatment of lithium intoxication in children. Am J Kidney Dis. 2001;37:1044–7. doi: 10.1016/s0272-6386(05)80022-8. http://dx.doi.org/10.1016/S0272-6386(05)80022-8. [DOI] [PubMed] [Google Scholar]


