Abstract
Objective Sleep health is critical for children to adapt to evolving cognitive-socioemotional contexts. Given that sleep timing in early childhood is instituted under caregiver control, the family context likely has an influential role on children’s sleep. This study investigated links between maternal depressive symptoms and variability in children’s sleep, and whether household income moderated this relation. Method 90 children (Mage = 53 ± 9 months) wore actigraphs to objectively measure sleep for 4–16 days. Mothers reported income and depressive symptomatology. Results Higher maternal depressive symptoms were related to greater variability in 24-hr sleep duration. Income moderated this relation. Lower income, but not maternal depressive symptoms, was linked to greater variability in sleep onset time. Conclusions Findings demonstrate important relations between maternal depressive symptoms, income, and children’s sleep. Understanding distal and proximal family characteristics that may be related to children’s developing sleep schedules could help identify populations and strategies for promoting optimal sleep health.
Keywords: children, depression, family functioning, health behavior, sleep
Healthy sleep habits, such as consistent sleep schedules, are important for children’s concurrent and long-term functioning in cognitive, socioemotional, and behavioral domains (Bernier, Beauchamp, Bouvette-Turcot, Carlson, & Carrier, 2013; Kelly & El-Sheikh, 2014). For example, a recent study reported that children who had higher proportions of total sleep taking place at night (i.e., greater consolidation of sleep into the night period) during infancy performed better on executive tasks 4 years later (Bernier, Beauchamp, et al., 2013). Likewise, shorter sleep duration and worse sleep quality at 8 years of age are related to behavioral and emotional problems that persist into adolescence (Kelly & El-Sheikh, 2014).
Upholding a consistent sleep schedule is especially important at developmental transitions. During the preschool years, children are first introduced to formal schooling and to a more homogenous weekday schedule, including routine sleep times. It is recommended that preschoolers maintain a consistent sleep schedule such that bedtimes and wake times are not shifted by more than 1 hr across the week (Mindell, Meltzer, Carskadon, & Chervin, 2009; National Sleep Foundation, 2014). Inconsistent sleep patterns have been increasingly linked to adverse outcomes in typically developing children. For instance, 9-year-old children with more variable sleep schedules self-reported more internalizing symptoms 2 years later (El-Sheikh, Kelly, Buckhalt, & Benjamin Hinnant, 2010). Moreover, school-aged children whose parent-reported bedtime varied by >1 hr across the week had a significantly higher risk of behavior problems compared with those whose bedtime varied by <1 hr (Biggs, Lushington, van den Heuvel, Martin, & Kennedy, 2011). Variability in both sleep duration and bedtime predicts less positive and more negative adjustment behavior in preschool, as well as more family stress (Bates, Viken, Alexander, Beyers, & Stockton, 2002). Given the adverse outcomes associated with inconsistent sleep patterns, it is imperative to discern environmental factors that may contribute to variability in preschool-aged children’s sleep. Because bedtimes and sleep patterns are typically enforced and maintained by caregivers at this age, the family context is one such factor that warrants further consideration.
Accumulating evidence supports the role of the family context on children’s sleep. Specifically, a number of studies substantiate the longitudinal and concurrent links between maternal psychopathology and children’s sleep disturbances (see Seifer, 2011 for review). Among studies that have focused on normative variations in parental psychosocial functioning, findings suggest that child sleep problems are related to greater maternal depressive symptoms (Warren, Howe, Simmens, & Dahl, 2006), higher parenting stress (Meltzer & Mindell, 2007), and elevated family and marital stress (Kelly & El-Sheikh, 2011).
Multiple indicators of family socioeconomic status (SES) have also been linked to objectively and subjectively measured sleep, providing evidence that children from lower SES homes display greater variation in sleep and wake patterns and overall poorer sleep quality (Acebo et al., 2005; El-Sheikh et al., 2013). Additionally, a number of studies show that family SES moderates the connection between child sleep and outcomes. In particular, links between children’s sleep problems and cognitive-socioemotional outcomes are exacerbated for lower SES children (Buckhalt, El-Sheikh, Keller, & Kelly, 2009; El-Sheikh et al., 2010). However, unknown is whether family SES moderates links between children’s sleep and parental psychosocial functioning, and only recently have studies begun to address this question. For example, Bernier, Bélanger, Bordeleau, and Carrier (2013) found that higher maternal social support, higher paternal marital satisfaction, and lower paternal stress were related to greater sleep consolidation (i.e., longer uninterrupted bouts of nighttime sleep) in toddlers. Further, the degree to which these factors were related was more pronounced in lower SES families.
Importantly, the study by Bernier, Bélanger, et al. (2013) was limited in that it used only 3 days of sleep assessed subjectively. Given that parent reports underestimate night awakenings and overestimate time spent asleep, significant variation in child sleep behaviors may not have been captured (Sadeh, 1996; Tikotzky & Sadeh, 2001). Kelly and El-Sheikh (2011) used actigraphy across seven nights as an objective measure of sleep and found that links between marital conflict and child sleep disruptions were stronger in lower SES homes. However, it is still uncertain whether a similar pattern is evident using extensive sleep measures in the context of parental psychosocial functioning, specifically maternal depressive symptoms.
The current study examined the degree to which maternal depressive symptoms were related to variability in weekday sleep onset time and variability in weekday sleep duration in preschool children. To our knowledge, only one study has assessed associations between maternal depressive symptoms and children’s sleep problems using both objective and subjective sleep parameters; however, the study was focused on elementary school-aged children (9 years of age; El-Sheikh et al., 2012). Here, we focused on preschool-aged children, an important age for establishing a consistent sleep schedule given that sleep transitions from biphasic (composed of a nap and an overnight sleep bout) to monophasic (composed solely of overnight sleep) patterns during this period. We hypothesized that higher maternal depressive symptoms and/or lower income may be characteristic of an unstable, unpredictable environment; exposure to such an environment may be linked to variability in children’s sleep. As such, we predicted that higher levels of maternal depressive symptoms would be associated with greater weekday sleep variability in preschool children. We further predicted that this relation would be more pronounced for lower income dyads.
Method
Participants
Children were recruited as part of a larger study from 17 preschools, including Head Start and private nonprofit preschools that serve low-income families. All children were enrolled in formal preschool in center-based settings before and throughout data collection. Children were eligible to participate if they met the following criteria: (1) 33–71 months of age, (2) normal or corrected-to-normal vision and hearing, (3) no current or past diagnosis of a sleep disorder or developmental disability, (4) no recent illness or travel across time zones, and (5) not using sleep-affecting or psychotropic medications.
Biological mothers of 128 children completed the series of questionnaires (excluding cases for which the father, grandparent, or other caregiver completed forms) containing demographic items, a depressive symptomatology scale, and subjective measures of child and maternal sleep (discussed below). Participants were required to have at least three weeknights of usable actigraphy data to be included in analyses based on previous work using the same, or a less stringent, criteria (Nixon et al., 2008; Penpraze et al., 2006; Sadeh, 1996; Sadeh, Lavie, Scher, Tirosh, & Epstein, 1991). Of the 128 children, 38 were excluded for insufficient actigraphy data (owing to noncompliance wearing the actigraph, parent choosing not to have their child wear the actigraph, or actigraph malfunction) and were therefore excluded from present analyses. Thus, the final sample included 90 preschool children (48% female; Mage = 53 months, standard deviation [SD] = 9 months, and range = 34–69 months).
Independent samples t tests and χ2 analyses were used to identify differences between dyads with (included in the present study) and without (those excluded from the present study) actigraphy data. Results revealed that the samples did not differ in terms of child gender, ethnicity, maternal education, household income, maternal depressive symptoms, maternal sleep quality, or maternal report of child sleep difficulties (p’s > .05). However, children with sufficient actigraphy data were slightly older (53 vs. 49 months, t(126) = 2.279, p = .024).
Procedures
Data were collected as part of a larger study, with all procedures approved by the University institutional review board. Mothers provided written informed consent for their own and their child’s participation. On the first day of the 16-day study, research assistants were present in preschool classrooms to distribute actigraphs to participants. Children were fitted with an actigraph watch on their nondominant wrist, and parent and child were instructed to press an event marker at lights-off (time child was expected to try to fall asleep) and after waking for both daytime and nighttime sleep episodes. Mothers were asked to encourage their child to wear the watch continuously for 16 consecutive days (15 nights). Mothers were also given a daily sleep diary to record any naps, periods where the watch was taken off, time the child was in bed (asleep or not), time it took the child to fall asleep, and wake time to validate actigraphy assessments. When the child was in the preschool classroom, teachers recorded nap times. Additionally, mothers were asked to complete questionnaires to assess household income, maternal depressive symptoms, maternal sleep quality, and child sleep. After completing the study, mothers received monetary compensation for completing questionnaires, and children received an age-appropriate book in appreciation of their time and participation.
Measures
Household Income
Mothers reported annual household income as one of the following: (a) ≤$5,000; (b) $5,001–$10,000; (c) $10,001–$20,000; (d) $20,001–$40,000; (e) $40,001–$70,000; (f) $70,001–$100,000; (g) $100,001–$150,000; or (h) >$150,000. Household income was plotted using a normal probability plot, revealing its normal distribution, and was thus used as a continuous variable (1–8) in analyses.
Maternal Depressive Symptoms
Mothers completed the Center for Epidemiological Studies Depression Scale (CES-D; Radloff, 1977) as a self-reported measure of current depressive symptomatology. The CES-D contains 20 items assessing the frequency with which symptoms occurred during the preceding week. Items are rated on a 4-point scale: Rarely or none of the time (<1 day), Some of the time (1–2 days), Occasionally (3–4 days), and Most or all of the time (5–7 days). A summary score was calculated using all 20 items and ranged from 0 to 60, with higher scores reflecting greater symptomatology. A cutoff score of 16 is indicative of significant depressive symptomatology (Boyd, Weissman, Thompson, & Myers, 1982). The CES-D has well-established reliability (e.g., Cronbach’s alpha = .91; Miller, Anton, & Townson, 2008) and concurrent validity (e.g., r ≥ .60; Agrell & Dehlin, 1989) with clinical and self-report assessments of depressive symptoms (Radloff, 1977).
Subjective Measures of Maternal and Child Sleep
The Pittsburgh Sleep Quality Index (PSQI; Buysse, Reynolds, Monk, Berman, & Kupfer, 1989) was completed by mothers and used as a subjective measure of sleep during the preceding month. Given evidence that maternal sleep quality is related to both maternal depressive symptoms and child sleep (Meltzer & Mindell, 2007), the PSQI was included in the present study to examine relations between maternal sleep quality, maternal depressive symptoms, and child sleep. The PSQI consists of 18 items that assess an array of sleep characteristics including sleep duration, latency, and frequency of sleep difficulties (e.g., “Cannot get to sleep within 30 minutes,” “Have bad dreams”). Items are used to create seven component scores that are equally weighted on a 0–3 scale. The seven component scores are summed to generate an overall PSQI score ranging from 0 to 21, with higher scores indicating worse sleep quality. A score >5 reflects poor sleep quality (Buysse et al., 1989). The PSQI demonstrates high internal consistency (Cronbach’s alpha = .80) and construct validity (r ≥ .69; Carpenter & Andrykowski, 1998).
Mothers also completed the Child Sleep Habits Questionnaire (CSHQ; Owens, Spirito, & McGuinn, 2000) as a subjective measure of children’s sleep habits during a typical week. The CSHQ includes 33 items grouped into eight subscales; however, the current study inadvertently omitted three items (i.e., “Seems tired during the day”; “Falls asleep while watching TV”; “Falls asleep while riding in car”), resulting in a 30-item measure. Items are rated on a 3-point scale: Usually (5–7 days per week), Sometimes (2–4 days per week), and Rarely (0–1 day per week). Items are summed to yield a global CSHQ score, with higher scores reflecting more sleep difficulties. To account for missing data, sum scores were divided by the total number of items with a response, resulting in a possible range of 1–3. The CSHQ is a reliable measure of sleep problems in community and clinical samples (Cronbach’s alpha = .68 and .78, respectively; Owens et al., 2000) and has established clinical utility in preschool children (Goodlin-Jones, Sitnick, Tang, Liu, & Anders, 2008). However, given that the current study inadvertently omitted three items relating to daytime sleepiness, the reliability of the CSHQ was assessed in the current sample, which revealed a Cronbach’s alpha of .86.
Actigraph-Measured Child Sleep
Actigraphy is considered a reliable method for detecting sleep in children when compared with polysomnography (agreement rates = 85.1–88.6%; Hyde et al., 2007). Actigraphs used in this study were the Actiwatch Spectrum (Philips Respironics, Inc., Bend, OR), a water-resistant wrist-worn device with off-wrist detection and triaxial accelerometer to measure motion. Parents and children were instructed to press an event marker at lights-off and lights-on, and parents and teachers were asked to note lights-off and lights-on in a sleep diary. Data collected by the actigraph were stored in the internal memory of the device, downloaded to a computer, and analyzed using Actiware software (Philips Respironics, Inc., Bend, OR). Fifteen-second epochs were scored for sleep or wake based on activity levels. Diary and event marker data were used to corroborate actigraphy data. Standard scoring rules were applied to each sleep episode: sleep onset was defined as the first of three consecutive minutes of sleep, and wake onset was the last of five consecutive minutes of sleep (LeBourgeois et al., 2013; Nixon et al., 2008). Sleep episodes were excluded if the actigraph was off-wrist or not working for all or part of the sleep episode. Variables derived for analysis from this scoring technique are described below.
To examine children’s sleep duration and timing, data were evaluated for daytime and nighttime sleep intervals separately. Given the inconsistency in weekend sleep schedules that may not be representative of children’s typical sleep patterns, weekday data alone were used, consistent with previous work (Ward, Gay, Anders, Alkon, & Lee, 2008). Sleep measures included: (a) daytime sleep duration—total minutes scored as sleep between daytime sleep onset and wake time, averaged across weekdays; (b) nighttime sleep duration—total minutes scored as sleep between nighttime sleep onset and wake time, averaged across weekdays; (c) total sleep duration—total minutes scored as sleep over a 24-hr period, averaged across weekdays; (d) variability in total sleep duration—SD of total sleep duration across weekdays; (e) sleep onset time—average nighttime sleep onset time across weekdays; and (f) variability in sleep onset time—SD of nighttime sleep onset time across weekdays.
Across the 16 consecutive days (15 nights) that children were asked to wear the actigraphs, daytime sleep was based on a maximum of 12 weekdays (Monday–Friday) and nighttime sleep was based on a maximum of 9 weeknights (Monday–Thursday; Friday nights were considered part of the weekend). Sunday was considered a weekend night, as sleep duration on Sunday nights has been reported to be significantly longer than sleep durations on weekdays (e.g., Basner et al., 2007), potentially compensatory to restricted sleep on Friday and Saturday nights. Children had, on average, 10 weekdays of usable data (M = 9.50, SD = 1.89); 4% had twelve, 31% had eleven, 31% had ten, 10% had nine, 8% had eight, 7% had seven, 3% had six, 2% had five, and 3% had four days of usable data. Children had, on average, seven weeknights of usable data (M = 7.37, SD = 1.67); 30% had nine, 28% had eight, 19% had seven, 9% had six, 4% had five, 7% had four, and 3% had three nights of usable data. Analyses were based on all usable actigraph data, the majority of which was contiguous days/nights (70%). Number of days/nights of usable data was not related to any outcome variables (e.g., maternal depressive symptoms, household income, variability in sleep duration and onset; p’s > .05), suggesting that variability in actigraph usage did not affect the outcome variables.
Data Analysis
In preliminary analyses, descriptive statistics and partial correlations among variables (controlling for child age) were examined. Data points that exceeded 4 SDs were set to “missing” in subsequent regression analyses. This resulted in removal of one data point for variability in sleep onset time. Listwise deletion was used to handle missing data in regression analyses.
To test the main effect of maternal depressive symptoms and its interaction with household income in the prediction of child sleep, predictors were mean-centered (to yield an accurate interpretation of lower-order regression coefficients and address the potential issue of high multicollinearity with the interaction term; Aiken & West, 1991) and submitted to a series of hierarchical regression models. Measures of variability in child weekday sleep time and duration were considered in separate models as outcome variables. Given that age was related to average total sleep duration, child age was controlled for in the initial step. Subsequently, the main effects of maternal depressive symptoms and household income were entered simultaneously in the next block, and their interactive product was entered in the final block. The purpose of this interaction term was to further explore whether the relation between maternal depressive symptoms and child sleep is moderated by household income (i.e., whether the slope of the regression line varies at different levels of income). Significant interactions indicate that slopes are different from each other. Following Aiken & West's (1991) guidelines, interactions were decomposed, with fitted regression lines plotted at high (+1 SD) and low (−1 SD) levels of income using estimates obtained from the final models. Simple slopes representing the association between maternal depressive symptoms and child sleep at high (+1 SD) and low (−1 SD) levels of income were evaluated to determine whether they were significantly different from zero.
Results
Sample characteristics and descriptive statistics are presented in Tables I–III. Ten mothers reported clinically significant depressive symptoms on the CES-D, one of which also fell in the low-income category (see below), and 26 reported poor sleep quality on the PSQI. Children’s age was correlated with average weekday total sleep duration (r = −.24, p = .025) and was thus controlled for in partial correlations (Table IV). Results revealed that mothers who reported greater depressive symptoms are more likely to have children with more inconsistent total sleep duration. Additionally, children in lower income homes were likely to have more inconsistent sleep schedules. These results and the descriptive data for child sleep are comparable with prior studies (Acebo et al., 2005; El-Sheikh et al., 2013).
Table II.
Maternal Sample Characteristics
| % | |
|---|---|
| Marital status | |
| Married | 46.7 |
| Not married, living with a partner | 17.8 |
| Never married | 21.1 |
| Divorced or separated | 14.4 |
| Maternal education | |
| Less than 12th grade | 4.0 |
| High school diploma | 8.0 |
| Some college | 26.0 |
| Associate degree | 12.0 |
| Bachelor’s degree | 18.0 |
| Graduate degree | 32.0 |
| Household income | |
| $5,000 or less | 4.4 |
| $5,001–$10,000 | 6.7 |
| $10,001–$20,000 | 17.8 |
| $20,001–$40,000 | 23.3 |
| $40,001–$70,000 | 7.8 |
| $70,001–$100,000 | 11.1 |
| $100,001–$150,000 | 14.4 |
| More than $150,000 | 6.7 |
| Do not know/missing | 7.8 |
Note. N = 90
Table I.
Child Sample Characteristics
| % | |
|---|---|
| Child ethnicity | |
| Non-Hispanic | 63.3 |
| Hispanic | 34.4 |
| Missing | 2.2 |
| Child race | |
| White | 57.8 |
| Black, African American | 8.9 |
| Asian Indian | 2.2 |
| Chinese | 1.1 |
| Vietnamese | 3.3 |
| Other Pacific Islander | 1.1 |
| Other | 4.4 |
| Multiracial | 14.3 |
| Missing | 6.7 |
Note. N = 90.
Table III.
Descriptive Statistics of Study Variables
| M | SD | Range | N | |
|---|---|---|---|---|
| Maternal depressive symptoms | 9.26 | 6.81 | 0–34 | 89 |
| Maternal sleep quality | 5.06 | 3.04 | 0–15 | 80 |
| Child sleep problemsa | 1.47 | 0.32 | 1–3 | 88 |
| Daytime sleep duration, minb | 86.96 | 21.25 | 13–136 | 88 |
| Nighttime sleep duration, minb | 569.77 | 39.47 | 444–672 | 90 |
| Total sleep duration, minb | 620.11 | 40.84 | 444–717 | 90 |
| Variability in total sleep duration, minb | 55.62 | 25.00 | 15–168 | 90 |
| Sleep onset timeb | 9:32 p.m. | 50 min | 7:09–11:23 p.m. | 90 |
| Variability in sleep onset time, minb | 38.50 | 22.69 | 9–140 | 90 |
aParent-reported data.
bActigraphy-based data.
Table IV.
Partial Correlations Among Study Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Maternal depressive symptoms | – | |||||||||
| 2. Maternal sleep quality | .34** | – | ||||||||
| 3. Household income | −.17 | −.17 | – | |||||||
| 4. Child sleep problemsa | .03 | .12 | −.22 | – | ||||||
| 5. Daytime sleep duration, minb | −.03 | −.25* | −.39*** | .13 | – | |||||
| 6. Nighttime sleep duration, minb | .16 | .26* | .25* | .01 | −.30** | – | ||||
| 7. Total sleep duration, minb | .14 | .14 | .06 | .03 | .12 | .74*** | – | |||
| 8. Variability in total sleep duration, minb | .28** | .11 | −.33** | .10 | .43*** | −.04 | .03 | – | ||
| 9. Sleep onset timeb | .02 | .04 | −.39*** | .25* | .37*** | −.45*** | −.41*** | .32** | – | |
| 10. Variability in sleep onset time, minb | .12 | .11 | −.28** | .31** | .29** | −.09 | −.14 | .55*** | .42*** | – |
Note. All correlations are controlling for child age. Pairwise deletion used to handle missing data.
aParent-reported data.
bActigraphy-based data.
*p < .05; **p < .01; ***p < .001.
Maternal Depressive Symptoms and Children’s Actigraph-Measured Sleep: Household Income as a Moderating Variable
To evaluate the role of maternal depressive symptoms in the context of household income on variability in children’s weekday sleep schedules, the following two sleep parameters were used as separate outcome variables in subsequent hierarchical regression analyses: (1) weekday variability in children’s total sleep duration and (2) weekday variability in children’s sleep onset time. Children’s age was controlled for in regression analyses.
Table V presents the results of the hierarchical regression analyses. The regression coefficients reported are those from the initial models before adding the interaction term (Model 1A) as well as the final models including the interaction effect (Model 1B). The final models predicted 21% of the overall variance in the SD of children’s weekday total sleep duration (p = .001) and 9% of the overall variance in the SD of children’s weekday sleep onset time (p = .123). Standardized residuals were plotted against adjusted predicted values for each outcome variable to ensure there were no violations of (1) normality, (2) linearity, or (3) homoscedasticity of residuals. Influential data points (multivariate outliers) were checked using Cook’s distance (Cook, 1977), with all values below the recommended maximum of 1. As a more conservative approach, data points exceeding 3 SDs above the mean for Cook’s distance were identified as potentially influential. Sensitivity analyses were conducted to assess the robustness of the models when removing these points. Results revealed that the final models were not sensitive to these data points.
Table V.
Summary of Regression Analyses Predicting Child Weekday Sleep
| Predictor | Variability in total sleep duration |
Variability in sleep onset time |
||||||
|---|---|---|---|---|---|---|---|---|
| Model 1A |
Model 1B (interaction) |
Model 1A |
Model 1B (interaction) |
|||||
| B (S.E.) | β | B (S.E.) | β | B (S.E.) | β | B (S.E.) | β | |
| (Constant) | 56.38 (2.55)*** | 55.52 (2.56)*** | 36.39 (2.10)*** | 36.10 (2.14)*** | ||||
| Child age | 0.26 (0.29) | .09 | 0.28 (0.29) | .10 | −0.30 (0.24) | −.14 | −0.29 (0.24) | −.14 |
| Maternal depressive symptoms | 0.72 (0.37) | .20 | 0.61 (0.37) | .17 | 0.23 (.31) | .08 | 0.20 (0.31) | .07 |
| Household income | −4.37 (1.38)** | −.33 | −4.50 (1.36)** | −.34 | −2.24 (1.15) | −.22 | −2.30 (1.16) | −.22 |
| Maternal depressive symptoms × income | – | – | −0.38 (0.21) | −.19 | – | – | −0.13 (0.18) | −.08 |
| R2 | 0.178** | 0.211*** | 0.080 | 0.090 | ||||
| ΔR2 | – | 0.033 | – | 0.007 | ||||
Note. B = Unstandardized coefficient; S.E. = standard error; β = standardized coefficient; R2 = model fit; ΔR2 = change in model fit; Block 1: child age; Block 2: child age, maternal depressive symptoms, household income; Block 3: child age, maternal depressive symptoms, household income, Maternal depressive symptoms × income.
*p < .05; **p < .01; ***p < .001.
In the model predicting variability in children’s weekday total sleep duration, the interaction between maternal depressive symptoms and household income was not significant (B = −0.38, S.E. = 0.21, p = .075, Cohen’s f2 = .27). In the model predicting variability in children’s weekday sleep onset time, the interaction between maternal depressive symptoms and household income was not significant (B = −0.00, S.E. = 0.00, p = .450, Cohen’s f2 = .10). These interactions were decomposed according to Aiken & West’s (1991) criteria, with fitted regression lines plotted at high (+1 SD) and low (−1 SD) levels of household income. As depicted in Figure 1, results revealed that elevated maternal depressive symptoms were related to greater variability in children’s weekday total sleep duration (B = 1.32, S.E. = 0.50, p = .010), but not with variability in children’s weekday sleep onset time (B = 0.01, S.E. = 0.01, p = .288) among lower income dyads. Among higher income dyads, maternal depressive symptoms were unrelated to variability in children’s weekday total sleep duration (B = −0.11, S.E. = 0.59, p = .855) or variability in children’s weekday sleep onset time (B = −0.00, S.E. = 0.01, p = .908).
Figure 1.
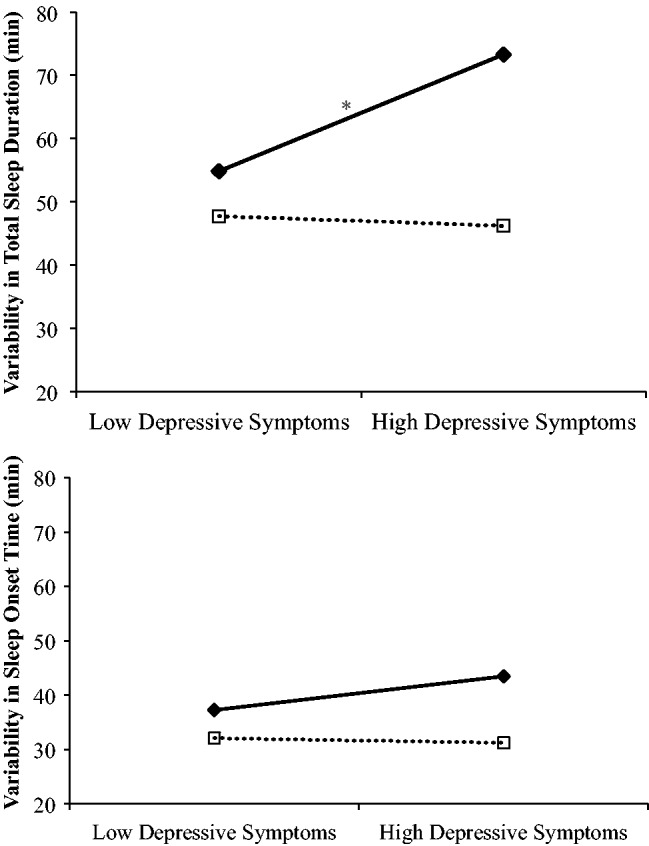
Links between maternal depressive symptoms and variability in children’s weekday sleep behaviors for low (−1 SD) and high (+1 SD) income dyads. Low-income dyads are depicted in solid lines; high-income dyads are depicted in dotted lines. Simple slopes based on regression coefficients presented in Table V. Note. *p < .05 for the simple slope.
Maternal Sleep Quality and Children’s Actigraph-Measured Sleep
To test whether maternal sleep quality played a role in the links between maternal depressive symptoms, household income, and variability in child sleep, the aforementioned models were reexamined with the inclusion of maternal PSQI scores. Maternal sleep quality was unrelated to variability in children’s weekday total sleep duration (B = −0.25, S.E. = 0.88, p = .780), and the addition of maternal sleep quality did not significantly improve the model (R2 change = 0.00, F change = 0.08, p = .780). Maternal sleep quality was also unrelated to variability in children’s weekday sleep onset time (B = 0.01, S.E. = 0.01, p = .492), and the addition of maternal sleep quality did not significantly improve the model (R2 change = 0.01, F change = 0.48, p = .492).
Discussion
Only recently has research begun to explore the role of the family context on children’s sleep, particularly in nonclinical samples (El-Sheikh et al., 2012; Kelly & El-Sheikh, 2011). The present study aimed to build on the existing literature by using comprehensive, objective sleep measures in a normative sample to explore relations between maternal depressive symptoms and preschool children’s sleep. We further examined whether these links vary across diverse socioeconomic backgrounds. Findings revealed that higher levels of maternal depressive symptoms were related to greater variability in children’s weekday total sleep duration. Furthermore, this link was stronger for dyads in lower income households. However, lower household income alone was marginally related to greater variability in children’s weekday sleep onset time. These relations were not explained by maternal sleep quality.
While maternal depressive symptoms and household income were independently linked to variability in children’s total weekday sleep duration, their interaction accounted for a marginal amount of additional variance. The interplay between these two constructs may play an imperative role in child sleep, above and beyond each alone. In other words, while there appears to be a distinctive link between maternal depressive symptoms and child sleep, and between income and child sleep, each individual link may be amplified in the presence of an additional contributing factor. These findings have notable clinical implications for children with several indices of maladaptive family functioning, a cohort that warrants further investigation to elucidate effects on child sleep patterns. However, lower income alone (independent of maternal depressive symptoms) was marginally linked to greater variability in sleep onset time. Low-income caregivers may work more than one job or irregular hours. These findings are in line with theories that focus on children’s adaptive functioning in relation to the dynamic interplay between physiological reactivity and adversity in a given context (Obradović, 2012; Obradović, Bush, Stamperdahl, Adler, & Boyce, 2010). Adversity can influence a child’s reactivity and ability to adapt to environmental risk factors. In the present study, lower income and maternal depressive symptoms are adverse factors that may interact with children’s reactivity and adaptive functioning, in this case, with respect to sleep patterns.
These results are consistent with research showing that even normal variations in parental psychosocial functioning are linked to child sleep health, highlighting the importance of using nonclinical, normative samples to examine the association between environmental factors and child sleep. Moreover, previous work using nonclinical samples was focused on elementary school-age children (Buckhalt et al., 2009; El-Sheikh et al., 2012, 2013; Kelly & El-Sheikh, 2011). The current study offers a unique and essential contribution to the existing literature by extending these findings to younger children.
Investigating sleep during the preschool years is crucial given that this period coincides with the introduction of a more rigid weekday schedule, including uniform sleep times. As previously established, upholding a consistent sleep schedule (sleep timing and duration) is especially important during the preschool years (Mindell, Meltzer, et al., 2009; National Sleep Foundation, 2014). Variable sleep duration and timing have been linked to behavior problems, as well as family stress (Bates et al., 2002; Biggs et al., 2011; El-Sheikh et al., 2010). Given that caregivers typically implement young children’s bedtimes and sleep patterns, compared with infants whose sleep schedules are largely driven by biological and dietary needs or to older children who have more independence over sleep onset, it is imperative that the contribution of the family context on preschool children’s sleep schedules is explored more thoroughly. However, many studies that have examined child sleep in the family context use only subjective measures of sleep (Bates et al., 2002; Bernier, Bélanger, et al., 2013; Biggs et al., 2011; Hale, Berger, LeBourgeois, & Brooks-Gunn, 2009; Meltzer & Mindell, 2007; Warren et al., 2006). Furthermore, this is an age that precedes the institution of formal schooling, during which nap opportunities are typically removed and new sleep patterns are being formed. This time period is also a critical transition given that early education and Head Start programs emphasize school readiness before entry into elementary school, and sleep contributes to this goal. Of the few studies that have examined child sleep in the family context using objective measures, samples have been restricted to elementary-aged children (El-Sheikh et al., 2012, 2013; Kelly & El-Sheikh, 2011). The present study used objective measurement of young children’s sleep across 16 days to capture substantial variation in sleep schedules considered to be representative of typical sleep patterns. As such, our findings provide a reliable means of exploring links between family context and variability in preschool children’s sleep.
Among an array of indices of the family context, the present work focused on the association between maternal depressive symptoms and variability in children’s weekday total sleep duration and sleep onset timing. Maternal depressive symptoms serve as a relevant index of family functioning given that the relationship a child shares with a mother experiencing depression may be characterized by unpredictability and insecurity (Warren et al., 2006). Similar to the unpredictability of a depressed caregiver, a capricious sleep schedule in itself may render a sense of uncertainty for the child. However, maternal depressive symptoms represent only one measure of family functioning. Other indices (e.g., increased maternal or child anxiety, variations in sleep environment, differences in bedtime routines) may also play a role in child sleep health, particularly with respect to inconsistent sleep onset times. Future research should incorporate additional familial-environmental variables to fully capture family functioning.
Further, this work examined such links in the context of household income given that preschool-age children from disadvantaged households tend to have more variability in bedtime and sleep duration (Acebo et al., 2005; Hale et al., 2009). Consistent sleep schedules may offer stability and dependability to family life and serve a buffering function for optimal child development, especially in the context of maternal depressive symptoms and economic disadvantage. For example, research has shown that variability in sleep parameters is related to less mature developmental age (Goodlin-Jones, Tang, Liu, & Anders, 2008). Additionally, it has been previously proposed that both child sleep quality and maternal mood can be improved by instituting a consistent nightly bedtime (Mindell, Telofski, Wiegand, & Kurtz, 2009). Thus, future studies should examine the role of consistent sleep schedules on child outcomes.
Despite the numerous strengths of this study, it is not without limitations. Given the cross-sectional nature of this data, directionality could not be explored. In line with previous work indicating that maternal depression directly impacts child sleep health (El-Sheikh et al., 2012; Warren et al., 2006), the present results suggest that the environment plays a role in child sleep schedules. However, it is possible that a bidirectional or cyclical relation exists between maternal depressive symptoms and child sleep. A mother experiencing depressive symptoms may be less likely to maintain a consistent routine sleep schedule with her child; in turn, her child’s inconsistent sleep schedule may contribute to and exacerbate her depressive symptoms, especially if her own sleep is disturbed. One possible clinical implication of these findings is to improve the consistency of children’s sleep, which may lead to a mitigation of maternal depressive symptoms. However, the clinical implications may be different for cases where maternal emotional instability is driving a chaotic environment, including sleep patterns. Future research should use a longitudinal or cross-lagged study design to discern the directionality of the link between maternal emotional well-being and child sleep.
Another caveat of the current study was the relatively modest sample size. Dyads were required to have complete data to be included in analyses; thus, a reduction in sample size resulted from children’s noncompliance wearing the actigraphs combined with mothers’ lack of response on questionnaires. Future research should use larger samples to identify effects that may be less robust with respect to indices of family functioning and child sleep. For example, the direct link between household income and variability in children’s sleep onset time in the current study approached significance, a result that may have been significant with a larger sample. However, several other aspects of this work may offset these limitations to a certain extent. Specifically, the diversity of the sample in terms of income and ethnicity, the use of a preschool-age cohort, and the use of well-established, extensive measures of sleep were strengths.
Overall, the results of this study have important implications. They demonstrate that household income moderates the relation between maternal depressive symptoms and variability in preschool children’s total sleep duration, such that this link is stronger in lower income households. These findings are consistent with previous evidence that links between children’s sleep and outcomes are exacerbated for lower SES children (Buckhalt et al., 2009; El-Sheikh et al., 2010). The use of a community sample suggests that even normative levels of maternal depressive symptomatology may play a significant role in child sleep health, which, in turn, has significant implications for children’s cognitive, socioemotional, and behavioral functioning.
Funding
This work was supported by the National Institutes of Health R01 HL111695 (to R.M.C.S.).
Conflicts of interest: None declared.
References
- Acebo C., Sadeh A., Seifer R., Tzischinsky O., Hafer A., Carskadon M. A. (2005). Sleep/wake patterns derived from activity monitoring and maternal report for healthy 1-to 5-year-old children. SLEEP, 28, 1568–1577. [DOI] [PubMed] [Google Scholar]
- Agrell B., Dehlin O. (1989). Comparison of six depression rating scales in geriatric stroke patients. Stroke, 20, 1190–1194. http://doi.org/10.1161/01.STR.20.9.1190 [DOI] [PubMed] [Google Scholar]
- Aiken L. S., West S. G. (1991). Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage. [Google Scholar]
- Basner M., Fomberstein K. M., Razavi F. M., Banks S., William J. H., Rosa R. R., Dinges D. F. (2007). American time use survey: Sleep time and its relationship to waking activities. Sleep, 30, 1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates J. E., Viken R. J., Alexander D. B., Beyers J., Stockton L. (2002). Sleep and adjustment in preschool children: Sleep diary reports by mothers relate to behavior reports by teachers. Child Development, 73, 62–75. http://doi.org/10.1111/1467-8624.00392 [DOI] [PubMed] [Google Scholar]
- Bernier A., Beauchamp M. H., Bouvette-Turcot A.-A., Carlson S. M., Carrier J. (2013). Sleep and cognition in preschool years: Specific links to executive functioning. Child Development, 84, 1542–1553. http://doi.org/10.1111/cdev.12063 [DOI] [PubMed] [Google Scholar]
- Bernier A., Bélanger M.-È., Bordeleau S., Carrier J. (2013). Mothers, fathers, and toddlers: Parental psychosocial functioning as a context for young children’s sleep. Developmental Psychology, 49, 1375–1384. http://doi.org/10.1037/a0030024 [DOI] [PubMed] [Google Scholar]
- Biggs S. N., Lushington K., van den Heuvel C. J., Martin A. J., Kennedy J. D. (2011). Inconsistent sleep schedules and daytime behavioral difficulties in school-aged children. Sleep Medicine, 12, 780–786. http://doi.org/10.1016/j.sleep.2011.03.017 [DOI] [PubMed] [Google Scholar]
- Boyd J. H., Weissman M. M., Thompson W. D., Myers J. K. (1982). Screening for depression in a community sample: Understanding the discrepancies between depression symptom and diagnostic scales. Archives of General Psychiatry, 39, 1195–1200. http://doi.org/10.1001/archpsyc.1982.04290100059010 [DOI] [PubMed] [Google Scholar]
- Buckhalt J. A., El-Sheikh M., Keller P. S., Kelly R. J. (2009). Concurrent and longitudinal relations between children’s sleep and cognitive functioning: The moderating role of parent education. Child Development, 80, 875–892. http://doi.org/10.1111/j.1467-8624.2009.01303.x [DOI] [PubMed] [Google Scholar]
- Buysse D. J., Reynolds C. F., Monk T. H., Berman S. R., Kupfer D. J. (1989). The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research, 28, 193–213. http://doi.org/10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- Carpenter J. S., Andrykowski M. A. (1998). Psychometric evaluation of the Pittsburgh sleep quality index. Journal of Psychosomatic Research, 45, 5–13. http://doi.org/10.1016/S0022-3999(97)00298-5 [DOI] [PubMed] [Google Scholar]
- Cook R. D. (1977). Detection of influential observation in linear regression. Technometrics, 19, 15–18. http://doi.org/10.2307/1268249 [Google Scholar]
- El-Sheikh M., Bagley E. J., Keiley M., Elmore-Staton L., Chen E., Buckhalt J. A. (2013). Economic adversity and children’s sleep problems: Multiple indicators and moderation of effects. Health Psychology, 32, 849–859. http://doi.org/10.1037/a0030413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sheikh M., Kelly R. J., Bagley E. J., Wetter E. K. (2012). Parental depressive symptoms and children’s sleep: The role of family conflict. Journal of Child Psychology and Psychiatry, 53, 806–814. http://doi.org/10.1111/j.1469-7610.2012.02530.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sheikh M., Kelly R. J., Buckhalt J. A., Benjamin Hinnant J. (2010). Children’s sleep and adjustment over time: The role of socioeconomic context. Child Development, 81, 870–883. http://doi.org/10.1111/j.1467-8624.2010.01439.x [DOI] [PubMed] [Google Scholar]
- Goodlin-Jones B. L., Sitnick S. L., Tang K., Liu J., Anders T. F. (2008). The Children’s Sleep Habits Questionnaire in toddlers and preschool children. Journal of Developmental & Behavioral Pediatrics, 29, 82–88. http://doi.org/10.1097/DBP.0b013e318163c39a [DOI] [PubMed] [Google Scholar]
- Goodlin-Jones B. L., Tang K., Liu J., Anders T. F. (2008). Sleep patterns in preschool-age children with autism, developmental delay, and typical development. Journal of the American Academy of Child and Adolescent Psychiatry, 47, 930–938. http://doi.org/10.1097/CHI.0b013e3181799f7c [DOI] [PubMed] [Google Scholar]
- Hale L., Berger L. M., LeBourgeois M. K., Brooks-Gunn J. (2009). Social and demographic predictors of preschoolers’ bedtime routines. Journal of Developmental and Behavioral Pediatrics, 30, 394–402. http://doi.org/10.1097/DBP.0b013e3181ba0e64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyde M., O’Driscoll D. M., Binette S., Galang C., Tan S. K., Verginis N., Davey M. J., Horne R. S. (2007). Validation of actigraphy for determining sleep and wake in children with sleep disordered breathing. Journal of Sleep Research, 16, 213–216. http://doi.org/10.1111/j.1365-2869.2007.00588.x [DOI] [PubMed] [Google Scholar]
- Kelly R. J., El-Sheikh M. (2011). Marital conflict and children’s sleep: Reciprocal relations and socioeconomic effects. Journal of Family Psychology, 25, 412–422. http://doi.org/10.1037/a0023789 [DOI] [PubMed] [Google Scholar]
- Kelly R. J., El-Sheikh M. (2014). Reciprocal relations between children’s sleep and their adjustment over time. Developmental Psychology, 50, 1137–1148. http://doi.org/10.1037/a0034501 [DOI] [PubMed] [Google Scholar]
- LeBourgeois M. K., Carskadon M. A., Akacem L. D., Simpkin C. T., Wright K. P., Achermann P., Jenni O. G. (2013). Circadian phase and its relationship to nighttime sleep in toddlers. Journal of Biological Rhythms, 28, 322–331. http://doi.org/10.1177/0748 730413506543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer L. J., Mindell J. A. (2007). Relationship between child sleep disturbances and maternal sleep, mood, and parenting stress: A pilot study. Journal of Family Psychology, 21, 67–73. http://doi.org/10.1037/0893-3200.21.1.67 [DOI] [PubMed] [Google Scholar]
- Miller W. C., Anton H. A., Townson A. F. (2008). Measurement properties of the CESD scale among individuals with spinal cord injury. Spinal Cord, 46, 287–292. http://doi.org/10.1038/sj.sc.3102127 [DOI] [PubMed] [Google Scholar]
- Mindell J. A., Meltzer L. J., Carskadon M. A., Chervin R. D. (2009). Developmental aspects of sleep hygiene: Findings from the 2004 National Sleep Foundation Sleep in America Poll. Sleep Medicine, 10, 771–779. http://doi.org/10.1016/j.sleep.2008.07.016 [DOI] [PubMed] [Google Scholar]
- Mindell J. A., Telofski L. S., Wiegand B., Kurtz E. S. (2009). A nightly bedtime routine: Impact on sleep in young children and maternal mood. Sleep, 32, 599–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Sleep Foundation. (2014). Retrieved from http://sleepfoundation.org/sleep-topics/children-and-sleep/page/0%2C2/ [Google Scholar]
- Nixon G. M., Thompson J. M., Han D. Y., Becroft D. M., Clark P. M., Robinson E., Waldie K. E., Wild C. J., Black P. N., Mitchell E. A. (2008). Short sleep duration in middle childhood: Risk factors and consequences. Sleep, 31, 71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obradović J. (2012). How can the study of physiological reactivity contribute to our understanding of adversity and resilience processes in development? Development and Psychopathology, 24, 371–387. http://doi.org/10.1017/S0954579412000053 [DOI] [PubMed] [Google Scholar]
- Obradović J., Bush N. R., Stamperdahl J., Adler N. E., Boyce W. T. (2010). Biological sensitivity to context: The interactive effects of stress reactivity and family adversity on socioemotional behavior and school readiness. Child Development, 81, 270–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens J. A., Spirito A., McGuinn M. (2000). The Children’s Sleep Habits Questionnaire (CSHQ): Psychometric properties of a survey instrument for school-aged children. SLEEP, 23, 1043–1052. [PubMed] [Google Scholar]
- Penpraze V., Reilly J. J., MacLean C. M., Montgomery C., Kelly L. A., Paton J. Y., Aitchison T., Grant S. (2006). Monitoring of physical activity in young children: How much is enough? Pediatric Exercise Science, 18, 483. [DOI] [PubMed] [Google Scholar]
- Radloff L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. http://doi.org/10.1177/014662167700100306 [Google Scholar]
- Sadeh A. (1996). Evaluating night wakings in sleep-disturbed infants: A methodological study of parental reports and actigraphy. Sleep, 19, 757–762. [DOI] [PubMed] [Google Scholar]
- Sadeh A., Lavie P., Scher A., Tirosh E., Epstein R. (1991). Actigraphic home-monitoring sleep-disturbed and control infants and young children: A new method for pediatric assessment of sleep-wake patterns. Pediatrics, 87, 494–499. [PubMed] [Google Scholar]
- Seifer R. (2011). Parental psychopathology and children’s sleep. In El-Sheikh M. (Ed.), Sleep and development: Familial and socio-cultural considerations (pp. 79–98). New York, NY: Oxford University Press. [Google Scholar]
- Tikotzky L., Sadeh A. (2001). Sleep patterns and sleep disruptions in kindergarten children. Journal of Clinical Child Psychology, 30, 581–591. http://doi.org/10.1207/S15374424JCCP3004_13 [DOI] [PubMed] [Google Scholar]
- Ward T. M., Gay C., Anders T. F., Alkon A., Lee K. A. (2008). Sleep and napping patterns in 3-to-5-year old children attending full-day childcare centers. Journal of Pediatric Psychology, 33, 666–672. [DOI] [PubMed] [Google Scholar]
- Warren S. L., Howe G., Simmens S. J., Dahl R. E. (2006). Maternal depressive symptoms and child sleep: Models of mutual influence over time. Development and Psychopathology, 18(1), 1–16. http://doi.org/10.1017/S0954579406060019 [DOI] [PubMed] [Google Scholar]


