Abstract
Objective Sleep problems are frequent in children and robustly predict internalizing symptoms in adolescence and adulthood. Longitudinal investigations have nonetheless used broad measures of childhood sleep problems, precluding understanding of the specific sleep problems that presage affective disturbances. Similarly, prospective examinations of mechanistic variables linking early sleep with subsequent internalizing symptoms are lacking. Method Childhood bedtime and nighttime waking problems were examined as independent predictors of adolescent internalizing symptoms within a community sample from the National Institute of Child Health and Human Development Study of Early Child Care and Youth Development (N = 1,089). The mediational role of emotional reactivity in late childhood also was examined. Results Bedtime but not nighttime waking problems significantly predicted adolescent internalizing problems. This relationship was partially explained by child emotional reactivity. Conclusions Some childhood sleep problems may more reliably predict later internalizing symptoms than others. Temperamentally based emotional reactivity may potentiate affective risk associated with childhood sleep difficulties.
Keywords: bedtime problems, emotional reactivity, internalizing, sleep, youth
Accumulated evidence shows sleep problems occurring in childhood to robustly predict emotional problems, particularly anxiety and depression, later in life (Gregory et al., 2005; Gregory, Eley, O'Connor, & Plomin, 2004; Gregory & O'Connor, 2002; Ong, Wickramaratne, Tang, & Weissman, 2006). These connections extend well into the adolescent and adult years. In children 4–19 years of age who were followed longitudinally for 14 years, early sleep problems robustly predicted later depression and anxiety (Gregory, Van der Ende, Willis, & Verhulst, 2008). Another investigation found 46% of children with persistent sleep problems between the ages of 5 and 9 years had an anxiety disorder by age 21 (compared with 33% of children without persistent sleep problems; Gregory et al., 2005). Moreover, severe sleep problems at age 5 have been shown to significantly elevate risk for depression almost 30 years later, at age 34 (Greene, Gregory, Fone, & White, 2014). These longitudinal relationships highlight the presence of a specific pathway between sleep behaviors at or around the time of school entry and the development of affective disturbances.
One noteworthy limitation within this body of research relates to the divergent ways “sleep problems” are commonly measured and defined. In some studies, a singular sleep item (e.g., Does your child have sleep difficulties?) has been used to assess the presence of childhood sleep problems (Greene et al., 2014). Other studies have used a composite measure of sleep-related items from broader measures of child behavior, most commonly the Child Behavior Checklist (CBCL; Achenbach, Howell, Quay, & Conners, 1991; Gregory & O'Connor, 2002). Sleep-related items included on the CBCL assess a limited range of both broad and specific types of nighttime behaviors and phenomena including “trouble sleeping,” “sleeping more/less than other kids,” “nightmares,” and being “overtired.” However, other common types of sleep-related problems observed in children, such as bedtime fears and nighttime awakenings, are not assessed. Still, other studies have examined the predictive value of one or several sleep problems such as sleepiness (Ong et al., 2006), inconsistency of bed/wake times (Ong et al., 2006), and/or nighttime wakings (Gregory et al., 2004). Such measurement differences are in part reflective of the inherent challenges in defining problematic sleep in children, given the consistent changes in sleep need and behaviors that distinguish early development (Dahl, 1996; Glaze, Rosen, & Owens, 2002). Still, measurement inconsistency precludes identification of precise targets for early prevention/intervention that might serve to alter the long-term trajectories of at-risk children. For example, even though child behavior problems that occur at or just before bedtime are typically lumped together with problematic awakening from an actual sleep state, divergent behavioral strategies may be used to reduce these problems. The current study therefore assessed the presence of problematic child behaviors that occur at or around bedtime as compared with during the night (i.e., awakenings from sleep) as independent predictors of adolescent internalizing symptoms.
Beyond questions related to the predictive utility of discrete types of sleep problems, precise mechanisms underlying sleep-internalizing relationships across development remain surprisingly unexplored. Experimental research in adults provides evidence that inadequate sleep may increase risk for affective disturbances via alterations in emotional reactivity (Dinges et al., 1997; Franzen, Buysse, Dahl, Thompson, & Siegle, 2009; Kahn-Greene, Killgore, Kamimori, Balkin, & Killgore, 2007; Sagaspe et al., 2006) and limited but emerging findings in youth are suggestive of similar relationships. For example, experimental sleep restriction produces decreased positive affect (Talbot, McGlinchey, Kaplan, Dahl, & Harvey, 2010), elevated emotional intensity, and decrements in emotion regulation skill among adolescents (Baum et al., 2014; Leotta, Carskadon, Acebo, Seifer, & Quinn, 1997). Although sleep deprivation studies are useful for understanding the acute effects of sleep on emotional outcomes, one night of sleep deprivation does not lead to permanent changes in emotional processing. Surprisingly few studies have examined the longer-term impact of children’s bedtime/nighttime behaviors on emotional outcomes. As the effects of disrupted sleep may be even greater in youth, for whom key brain regions are still developing (Casey, Giedd, & Thomas, 2000), altered patterns of emotional reactivity may provide a direct conduit from sleep problems to affective problems.
Increased emotional reactivity (defined as a coordinated set of responses to an emotional trigger involving experiential, behavioral, and physiological systems; Gross, 2015) is not only a core feature of most psychiatric conditions but a potent risk factor for internalizing problems (Joormann, Talbot, & Gotlib, 2007; Suveg & Zeman, 2004). Children with internalizing disorders report and demonstrate increased levels of emotional intensity and have fewer emotion regulation strategies than do healthy children (Suveg & Zeman, 2004). Likewise, healthy adolescents with increased emotional lability and less effective emotion regulation skills experience increased depressive symptoms (Silk, Steinberg, & Morris, 2003).
Regulatory skills develop gradually with age and experience, with the most significant changes occurring in early childhood (Calkins & Hill, 2007). Adolescence, and the onset of puberty more specifically, also coincides with improvements in affect modulation and the ability to discriminate among emotional cues relative to childhood (Yurgelun-Todd, 2007): skills shaped in part by advances in executive functioning and emotional processing via ongoing maturation of the prefrontal cortex, the amygdala, and connective pathways linking these areas (Casey et al., 2000; Gee et al., 2013; Schumann et al., 2004). These skills promote adaptive responses across different social and emotional situations (Salovey, Mayer, Caruso, & Yoo, 2009) and become increasingly critical as peer relationships expand and sensitivity to social evaluation heightens (Brown, 2004; Furman, 2002; O'Brien & Bierman, 1988; Steinberg & Morris, 2001). In light of these stage-specific demands and challenges, the current study was interested in the mechanistic role of emotional reactivity both in general and in late childhood (i.e., the pre-adolescent years) specifically in explaining linkages between childhood sleep and adolescent internalizing symptoms.
Current Study
Using data from the National Institute of Child Health and Human Development (NICHD) Study of Early Child Care and Youth Development (SECCYD), the current study had two primary objectives. First, we examined bedtime problems (e.g., problems getting into bed, problems falling asleep) and nighttime waking problems (e.g., awakening more than once during the night, awakened by a frightening dream) in middle childhood (i.e., during 3rd grade) as independent predictors of adolescent (i.e., at age 15) internalizing symptoms. In the absence of previous studies examining the predictive value of specific types of childhood sleep problems, we expected both types of sleep-related problems to serve as significant predictors of adolescent internalizing symptoms. Second, the role of emotional reactivity was examined as a putative mediator of these relationships. In light of the salient emotional changes that coincide with the onset of adolescence, we were specifically interested in levels of emotional reactivity during the pre-adolescent years (i.e., age 11–12) and therefore included childhood levels of emotional reactivity in our analyses. We hypothesized increased levels of emotional reactivity in preadolescence would partially explain relationships between specific sleep problems in 3rd grade and internalizing problems at age 15.
Method
Sample
Children (N = 1,364) and their families enrolled in the NICHD SECCYD were examined. The original pool of participants was selected in accordance with a continuously random sampling plan. Data were collected on facets of child social, emotional, intellectual development, language development, behavioral problems, adjustment problems, and physical health. See NICHD Early Child Care Research Network (2005) for more detailed information about the sample and the sampling plan. Participants were assessed annually (demarked by academic grade) from birth to age 15, but only data collected at birth, in middle childhood (i.e., during 3rd grade), late childhood (i.e., during 5th grade), and adolescence (i.e., at age 15) were used in the current study. Of the original sample, 48.3% were female and 80.4% identified the child participant as White. In middle childhood, the majority (58.8%) of children had parents who were married and living together. Mean household income in middle childhood was $77,000 (SD = $68,273). See Table I for a detailed breakdown of demographic information.
Table I.
Demographics
| Demographic variable | % (n) |
|---|---|
| Female | 48.3 (659) |
| Marital status | |
| Married, living together | 58.8 (802) |
| Partnered, living together | 4.1 (56) |
| Separated/divorced | 9.9 (135) |
| Other | 4.4 (60) |
| Missing | 22.8 (311) |
| Race | |
| American Indian, Eskimo, Aleutian | 0.4 (5) |
| Asian or Pacific Islander | 1.6 (22) |
| Black | 12.9 (176) |
| White | 80.4 (1,097) |
| Ethnicity | |
| Hispanic | 6.1 (83) |
| Mother’s education | |
| Less than high school diploma | 10.2 (139) |
| High school graduate or GED | 21 (287) |
| Some college or AA degree | 33.4 (455) |
| Bachelor’s degree | 20.8 (284) |
| Some graduate work/master’s degree | 11.8 (161) |
| Law degree | 11.8 (161) |
| More than masters/MD/PhD | 1.7 (23) |
| Father/partner’s education | |
| Less than high school diploma | 8.4 (105) |
| High school graduate or GED | 20.8 (284) |
| Some college or AA degree | 27.2 (340) |
| Bachelor’s degree | 19.9 (271) |
| Some graduate work/master’s degree | 10.9 (149) |
| Law degree | 1.4 (19) |
| More than masters/MD/PhD | 3.7 (51) |
| M (SD) | |
| Total family income | $77,008.04 ($68,272.663) |
Previous studies assessing sleep using the SECCYD data set have examined infant sleep and attachment (McNamara, Belsky, & Fearon, 2003), the impact of adolescent sleep disruption on social relationships (Maume, 2013), longitudinal associations between sleep and cognitive and language outcomes (Dearing, McCartney, Marshall, & Warner, 2001), the impact of sleep problems on adolescent risk taking (Thomas, Monahan, Lukowski, & Cauffman, 2015), and the relation between sleep, self-control, and delinquency (Meldrum, Barnes, & Hay, 2015). However, no study has examined the longitudinal relation between childhood sleep problems and adolescent internalizing symptoms or examined possible explanatory mechanisms of this link using the SECCYD data set.
Measures
My Child’s Sleep Habits
Collected in middle childhood, this set of questions was derived from the original Children's Sleep Habits Questionnaire (CSHQ; Owens, Spirito, & McGuinn, 2000), a parent-report measure of child sleep behaviors, habits, and difficulties with sleep. The original CSHQ (Owens et al., 2000) is a well-validated and highly used measure that assesses a range of child sleep problems using a 3-point scale for each item (3 = usually, 2 = sometimes, 1 = rarely, and don’t know). Based on the CSHQ, the modified questionnaire used in the current study used a reversed coding scale (1 = usually, 2 = sometimes, 3 = rarely, and don’t know) relative to the original coding. Several items from the modified scales were reverse coded (i.e., three items from the bedtime problems scale and four items from the nighttime waking problems scale; see Table II). One question requesting an impairment rating regarding nighttime wakings (i.e., “How much of a problem are sleep wakings for you?”) was scored on a similar 3-point scale (3 = A big problem, 2 = A bit of a problem, 1 = Not a problem). Parents were provided with guidelines for each rating category (i.e., usually = if something occurs five or more times in a week; sometimes = if it occurs two to four times in a week; rarely = if something occurs never or one time during a week). Only items from the modified bedtime problems and nighttime waking problems subscales (see Table II) were used in the current study, although parents completed a total of 27 items across the bedtime problems, nighttime waking problems, sleep problems, morning waking problems, and daytime sleepiness problems subscales. Item scores were averaged for both the bedtime problems and nighttime waking problems scales. Although there was no parasomnia scale on this questionnaire, it should be noted that two parasomnias were assessed in our nighttime waking problems scale (i.e., nightmares and night terrors). Internal reliability for the bedtime problems scale (six items) was α = .67, and α = .81 for the nighttime waking problem scale (five items). These estimates are consistent with previous child sleep research and are somewhat expected, as Cronbach alpha values are relatively sensitive to the number of items used (e.g., <10 items; DeVellis, 2003).
Table II.
Sleep Questionnaire Items by Problem Type and Response Rates
| Sleep problems | Usually = 1% (N) | Sometimes = 2% (N) | Rarely = 3% (N) | Don’t know/no response% (n) |
|---|---|---|---|---|
| Bedtime problems | ||||
| My child goes to bed at the same time every night | 72.3 (784) | 18.2 (198) | 4 (43) | 5.6 (60) |
| Child falls asleep within 20 minutes of bedtime | 67.7 (735) | 18.9 (205) | 7.6 (82) | 5.9 (63) |
| My child falls asleep in own bed | 79.1 (858) | 8.9 (97) | 6.5 (70) | 5.5 (60) |
| Child needs me/parent in room to fall asleepa | 6.1 (66) | 9.3 (101) | 78.6 (853) | 6 (65) |
| My child is afraid of sleeping alonea | 5.9 (64) | 13.1 (142) | 74.3 (806) | 6.7 (73) |
| Getting my child to bed at night is a problema | 4.1 (44) | 24.3 (264) | 65.9 (715) | 5.7 (62) |
| Nighttime waking problems | ||||
| Child awakens at night screaming/sweating/inconsolablea | 0.4 (4) | 1.4 (15) | 91.7 (955) | 6.5 (71) |
| My child awakens alarmed by a frightening dreama | 0.5 (5) | 10 (108) | 82.7 (897) | 6.9 (75) |
| My child awakes once during the nighta | 4 (43) | 17.6 (191) | 769.3 (752) | 9.1 (99) |
| My child awakes more than once during the nighta | 0.8 (9) | 3.1 (34) | 86.4 (937) | 9.7 (105) |
| How much of a problem are sleep wakings for youb | 87.6 (950) | 5.4 (59) | 1.5 (16) | 5.5 (60) |
Note. Prevalence rates are presented based on the 1,085 participants who completed the bedtime problems and nighttime waking problems scales.
aReverse-coded items.
bItem scored on altered scale: 1 = Not a problem, 2 = A bit of a problem, 3 = A big problem.
Parent Report of Children’s Reactions
Mother report of child emotional reactivity was collected via a 10-item questionnaire administered both in middle childhood and in late childhood. This measure was developed for the SECCYD based on items adapted from Larsen and Diener's (1987) Affective Intensity Scale (El-Sheikh & Buckhalt, 2005) to assess maternal perceptions of child emotional expression in response to events. The original Affective Intensity Scale is a reliable and valid measure of emotional reactivity (Larsen & Diener, 1987). Example items from the adapted scale used in the current study include “my child responds very emotionally to stories, movies, and events,” and “when my child feels an emotion, either positive or negative, my child feels it strongly.” Mothers rated the general frequency (no time frame was specified) of different observed emotional responses in their children using a 5-point scale for each item (1 = never, 2 = occasionally, 3 = about half the time, 4 = usually, 5 = always). Items from this scale were summed to produce the total Emotional Reactivity score in middle childhood and in late childhood. The summed total from late childhood was used in all mediation analyses and the summed total from middle childhood was used as a covariate in the final mediation model. Reliability of the scale was acceptable for both middle childhood (α = .76) and late childhood (α = .77).
Youth Self-Report
Collected in adolescence, the Youth Self-Report (YSR) is a widely used self-reported measure of social competence and problem behavior for youth between 11 and 18 years of age (Achenbach, 1991b). Each child rated every behavior on a 3-point scale. Broad-band scales of internalizing and externalizing problems, and narrow band scales of social problems, aggression, attention problems, and depression (among others) were derived from a computerized scoring program. The YSR is highly reliable and internally consistent (Achenbach, 1991b). Raw scores from the broad-band internalizing problems scale were used in regression analyses in the current study. Broad-band internalizing problems t-scores were used for calculating prevalence estimates of clinically significant internalizing problems.
Child Behavior Checklist
Collected in middle childhood, the CBCL is a widely used measure of social competence and problem behavior in children between 4 and 18 years of age (Achenbach, 1991a). Each mother rated approximately 100 different behaviors on a 3-point scale. The CBCL is a highly reliable and internally consistent measure (Achenbach, 1991a). In the current study, broad-band internalizing raw scores were used to control for baseline levels of internalizing problems. Broad-band internalizing t-scores were used to calculate prevalence estimates of clinically significant internalizing symptoms in middle childhood.
Analytic Plan
Linearity for all variables was found to be acceptable based on results of scatter plots and bivariate correlations. Multicollinearity diagnostics were acceptable. Data were significantly non-normally distributed; however, transformations were not completed as normality is regarded as the least essential of assumptions required for linear regression and research has demonstrated that severe normality violations only impact statistical inferences in small samples (Hayes, 1996, 2013).
Missing Data
Completely Missing/Dropout. Although retention was good throughout the project, of the original sample (N = 1,364), 275 (20.16%) participants had missing data across sleep, emotional reactivity, and internalizing measures or had dropped out of the study before middle childhood. These participants did not differ on sex, race, or parental marital status from participants who remained in the study (N = 1,089).
Missing Individual Measures. Of the remaining 1,089 participants, 4 (0.4%) were missing parent report of bedtime problems, 4 (0.4%) were missing parent report of nighttime waking problems, 67 (6.2%) were missing mother report of emotional reactivity, and 67 (6.2%) were missing mother report of internalizing problems in 3rd grade. In late childhood (5th grade), 68 (6.2%) participants were missing mother report of emotional reactivity. At age 15, a total of 174 (16%) participants were missing self-report of internalizing symptoms. Little’s Missing Completely at Random test rejected the hypothesis of completely at random missing data (χ2(126) = 349.874, p < .001); meaning there was a statistical relation between missing and observed variables. We then assessed whether data were missing at random (MAR; i.e., missingness was conditional on another variable) by comparing participants with and without missing data. Significantly more White than minority children were missing emotional reactivity in middle childhood (χ2 = 4.374, p = .036) and mother-reported internalizing problems in middle childhood (χ2 = 4.374, p = .036). Also, significantly more males than females were missing parent report of internalizing problems in middle childhood (χ2 = 5.826, p = .016) and parent report of emotional reactivity in middle childhood (χ2 = 4.640, p = .031). No meaningful trends in missing data were found, and data were therefore assumed to be MAR and Expectation Maximization imputation was completed (Peugh & Enders, 2004). This form of data imputation involves an expectation step, in which missing values are imputed using a regression imputation, and a maximization step in which the covariance matrix and mean vector are estimated. This process continues iteratively until the differences between covariance matrices from the ongoing maximization steps differ by only a trivial amount.
Planned Analyses
All analyses were conducted using SPSS version 23. Before imputation, the prevalence of bedtime problems and nighttime waking problems was examined for participants with complete data on these scales. Prevalence rates for both bedtime and nighttime waking problems scales were calculated by first dummy coding all items marked “sometimes” and “always” (i.e., score of 2 or 3) as a sleep problem and all items marked as “rarely” (i.e., score of 1) as no sleep problem. Dummy coded items for each participant were then summed to calculate the total number of bedtime problems and nighttime waking problems, respectively.
Demographic variables were dummy coded for all correlation, regression, and mediation analyses (i.e., White vs. all other racial statuses, married and living together vs. all other groups at birth, and females vs. males). Aim 1 was examined using a hierarchical linear regression framework. Two separate hierarchical linear regression models were examined for bedtime problems and nighttime waking problems in middle childhood. Covariates (total family income, marital status, sex, and internalizing problems in middle childhood) were entered into Step 1 in both models. Bedtime problems was entered into Step 2 in the first model, and nighttime waking problems was entered into Step 2 in the second model. Adolescent internalizing problems was entered as the dependent variable across both models.
Aim 2 was analyzed using the PROCESS Macro in SPSS. PROCESS is a conditional process modeling program developed by Preacher and Hayes that uses an ordinary least squares-based path analytical framework to test for both direct and indirect effects (Hayes, 2013). This procedure was used to examine each regression pathway in mediation models and to test the indirect effect of the predictor on the criterion variable through the mediator. Emotional reactivity in late childhood was examined as a mediator of the link between middle childhood sleep problems and adolescent internalizing problems using four mediation models. Two models were planned with specific sleep problems entered as the predictor in either model. In both models, internalizing problems in adolescence was entered as the criterion variable, identified covariates (i.e., total family income, marital status, sex, and internalizing problems in middle childhood) were accounted for, and emotional reactivity in late childhood was entered as the mediator. Two additional mediation models were also planned, with emotional reactivity in middle childhood entered as an additional covariate to account for any changes in emotional reactivity across development. All relative indirect effects were subjected to follow-up bootstrap analyses with 10,000 samples and a 95-percentile confidence interval estimate (as recommended by Hayes & Matthes, 2009; Preacher & Hayes, 2008). Across all models, covariates were entered for the mediator and outcome variables.
Results
Prevalence of Sleep Problems
Of participants with complete bedtime problems data (N = 1,085), 57.6% (n = 625) experienced one or more bedtime problems and 35% (n = 382) experienced two or more bedtime problems at least two to four nights per week (i.e., “sometimes”). Specifically, 22.2% (n = 241) of parents reported their child does not go to bed at the same time each night, 26.5% (n = 287) of parents reported their child does not fall asleep within 20 min of going to bed, 15.4% (n = 167) of parents reported their child does not fall asleep in his/her own bed, 15.4% (n = 167) of parents reported their child needs a parent in the room to fall asleep, 19% (n = 206) of parents reported their child is afraid of sleeping alone, and 28.4% (n = 308) of parents reported that getting their child to bed at night is a problem.
Of individuals with complete nighttime waking problems data (N = 1,085), 27% (n = 296) had one or more nighttime waking problems and 9% (n = 98) experienced two or more nighttime waking problems at least two to four nights per week (i.e., “sometimes”). Specifically, 1.8% (n = 19) of parents reported that their child awakens with night terrors, 10.4% (n = 113) of parents reported that their child experiences nightmares, 21.6% (n = 234) of parents reported their child awakens once during the night, 4% (n = 43) of parents reported their child wakes up more than once a night, and 6.9% (n = 75) of parents reported that nighttime waking problems in their child is a problem for them. A detailed breakdown of individual sleep item prevalence ratings is presented in Table II.
Prevalence of Internalizing Problems and Emotional Reactivity
Before imputation the prevalence of internalizing problems on the CBCL and YSR were examined in middle childhood and in adolescence, respectively. Of the participants (N = 1,022) with complete CBCL scores, 3.1% (n = 31) of mothers reported a t-score of ≥ 69 on the internalizing problems scale, indicating clinically significant internalizing symptoms. Additionally, 6.8% (n = 68) of mothers reported t-scores in the borderline range. Of the adolescents with complete YSR data (N = 915) at age 15 years, 2.5% (n = 23) of youth reported a t-score of ≥69 on the internalizing problems scale, indicating clinically significant internalizing symptoms. Additionally, 4.7% (n = 42) of youth reported t-scores in the borderline range. Emotional reactivity scores (summed total score ranging from 10 to 50) were relatively similar across middle (M = 33.91, SD = 5.59) and late childhood (M = 33.50, SD = 5.66).
Bivariate Correlations
Bivariate Pearson correlation coefficients (presented in Table III) using the final imputed sample (N = 1,089) were examined and identified total family income, marital status, and sex as covariates to be included in all remaining regression and mediation analyses.
Table III.
Bivariate Correlations
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Sex (female) | 1 | |||||||||
| 2. Race (White) | −.004 | 1 | ||||||||
| 3. Marital status | −.021 | .308** | 1 | |||||||
| 4. Income | .003 | .168** | .304** | 1 | ||||||
| 5. Bedtime problems (X1) | −.038 | −.118** | −.176** | −.094** | 1 | |||||
| 6. Nighttime waking problem (X2) | −.047 | −.087** | −.127** | −.005 | .508** | 1 | ||||
| 7. Emotional reactivity in LC (M) | .056 | .015 | −.008 | −.084** | .108** | .078** | 1 | |||
| 8. Emotional reactivity in MC | .006 | .032 | −.008 | −.079* | .094** | .050 | .674** | 1 | ||
| 9. Internalizing in MC | .039 | −.015 | −.099** | −.128** | .168** | .101** | .221** | .257** | 1 | |
| 10. Internalizing in Adol (Y) | .182** | −.015 | −.087** | −.100** | .097** | .043 | .112** | .216** | .198** | 1 |
Note. Sex—dummy coded, female; Marital status—dummy coded, married, and living together; Race—dummy coded, White vs. all else.
MC = middle childhood; LC = late childhood; Adol = adolescence.
*p < .05; **p < .01.
Regression Analyses
Overall hierarchical linear regression models examining both bedtime and nighttime waking problems were significant (bedtime problems: adjR2 = .078, df = 5, 1,079, F = 19.215, p < .001, N = 1,089; nighttime waking problems: adjR2 = .074, df = 5, 1,079, F = 18.389, p < .001, N = 1,089). However, only the inclusion of bedtime problems increased model significance (Fchange = 4.458, p = .035). Thus, the planned mediation models using nighttime waking problems as a predictor were not conducted. Parameter estimates (see Table IV) revealed that bedtime problems was a significant predictor of internalizing problems in adolescence (t = 2.111, p = .035), as was being female (t = 6.085, p < .001), total family income (t = −2.007, p = .045), and internalizing problems in middle childhood (t = 5.665, p < .001).
Table IV.
Hierarchical Linear Regressions of Bedtime Problems and Nighttime Waking Problems on Adolescent Internalizing Problems
| Model—independent variable | Step | Variable | R2 change | F change | p | β | p |
|---|---|---|---|---|---|---|---|
| Bedtime problems | 1 | Covariates | .077 | 22.579 | <.001** | ||
| Sex (female) | .183 | <.001** | |||||
| Income | −.056 | .071 | |||||
| Married | −.025 | .413 | |||||
| Internalizing in MC | .168 | <.001** | |||||
| 2 | Bedtime problems | .005 | 5.389 | .020* | .070 | .020* | |
| Nighttime waking problems | 1 | Covariates | .077 | 22.579 | <.001** | ||
| Sex (female) | .183 | <.001** | |||||
| Income | −.058 | .060 | |||||
| Married | −.031 | .311 | |||||
| Internalizing in MC | .175 | <.001** | |||||
| 2 | Nighttime waking problems | .001 | 1.557 | .212 | .037 | .212 |
Note. β corresponds to standardized β in a model with all variables included.
MC = middle childhood.
Mediation Analyses
When examining emotional reactivity in late childhood (5th grade) as a putative mediator of the link between middle childhood bedtime problems and adolescent internalizing problems (see Figure 1), the total direct mediation model was significant (adjR2 = .078, df = 5, 1079, F = 19.215, p < .001, N = 1,089; path c), as was the full model with emotional reactivity included as a mediator (R2 = .086, df = 6, 1078, F = 16.858, N = 1,089, p < .0001). The direct effect (c’ path) of bedtime problems on internalizing problems in adolescence after accounting for covariates (i.e., total family income, marital status, and sex, and internalizing problems in middle childhood) and 5th grade emotional reactivity remained significant per Maximum Likelihood (ML) confidence intervals (CI), t = 2.147, p = .03, 95% CI (0.105, 2.326). There was also a significant indirect effect of bedtime problems on internalizing problems through emotional reactivity, demonstrated by the bootstrapped 95% CI of the indirect effect, b = 0.096, SE = 0.063, 95% CI (0.010, 0.265). See Table V.
Figure 1.
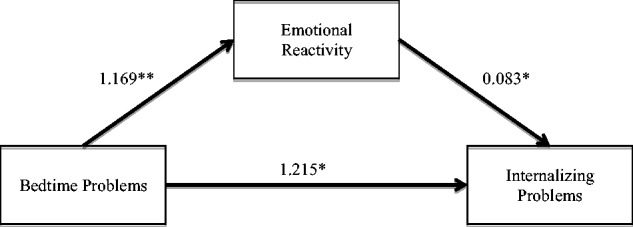
Mediation model of the significant indirect effect of bedtime problems on internalizing problems through emotional reactivity. Test of the indirect effect: b = .097, SE = 0.063, Confidence Interval (lower) = 0.010, Confidence Interval (upper) = 0.265*; **p < .01; *p < .05.
Table V.
Meditation Model Results
| Simple mediation | b | SE | t | p | CI (lower) | CI (Upper) |
|---|---|---|---|---|---|---|
| Bedtime problems →ER (a) | 1.169 | 0.453 | 2.579 | .010** | 0.280 | 2.059 |
| ER→ YSR (b) | 0.083 | 0.0379 | 2.178 | .030* | 0.008 | 0.148 |
| Bedtime problems –>YSR (c) | 1.312 | 0.565 | 2.321 | .020* | 0.203 | 2.420 |
| Bedtime problems –>YSR (c') | 1.215 | 0.566 | 2.148 | .032* | 0.105 | 2.326 |
| X1-->M-->Y (a1*b1) | 0.097 | 0.063 | 0.010 | 0.265* |
Note. ER = emotional reactivity in late childhood [mediator], YSR = internalizing in adolescence.
Covariates included total family income, marital status, sex, and internalizing problems in middle childhood.
*p < 0.05; **p < 0.01.
In the second mediation model, which included emotional reactivity in middle childhood (3rd grade) as an additional covariate, the total direct model was significant (adjR2 = .078, df = 5, 1079, F = 19.215, p < .001, N = 1,089; path c), as was the full model with emotional reactivity in late childhood included as a mediator (R2 = .085, df = 6, 1078, F = 16.7160, p < .0001, N = 1,089). The direct effect (c’ path) of bedtime problems on internalizing problems in adolescence after accounting for covariates and emotional reactivity in late childhood remained significant per ML confidence intervals, t = 2.3247, p = .0203, 95% CI (0.203, 2.395). However, there was no significant indirect effect of bedtime problems on internalizing problems through emotional reactivity, per the bootstrapped 95% CI of the indirect effect, b = 0.0539, SE = 0.0466, 95% CI (−0.027, 0.1951). See Table VI.
Table VI.
Meditation Model Results With Emotional Reactivity in Middle Childhood as a Covariate
| Simple mediation | b | SE | t | p | CI (lower) | CI (Upper) |
|---|---|---|---|---|---|---|
| Bedtime problems →ER (a) | 0.596 | 0.3343 | 1.784 | .075 | −0.060 | 1.253 |
| ER→ YSR (b) | 0.090 | 0.0508 | 1.780 | .075 | −0.009 | 0.190 |
| Bedtime Problems -->YSR (c) | 1.312 | 0.565 | 2.321 | .020* | 0.203 | 2.420 |
| Bedtime Problems -->YSR (c') | 1.299 | 0.5588 | 2.325 | .0203* | 0.203 | 2.395 |
| X1–>M–>Y (a1 × b1) | 0.054 | 0.047 | −0.003 | 0.195 |
Note. ER = emotional reactivity in late childhood [mediator], YSR = internalizing in adolescence.
Covariates included total family income, marital status, sex, internalizing problems in middle childhood, and emotional reactivity in middle childhood.
*p < 0.05.
Discussion
Recognition that sleep problems in childhood independently and reliably predict anxiety and depression later in life calls for research aimed at explicating these robust relationships. With this goal in mind, the current study sought to address some critical gaps in the research literature. First, rather than using a broad-based measure of childhood sleep problems, we examined difficulties occurring at or around bedtime and awakenings during the actual sleep period as separate predictors of later internalizing symptoms. Just over 57% of youth in middle childhood (i.e., 8–9 years of age) experienced at least one bedtime problem, while 27% experienced at least one nighttime waking problem (i.e., occurring at least two to four times per week). Overall, our findings are consistent with rates of sleep problems reported in community-based studies of school-aged children (Kahn et al., 1989; Mindell, 1993; Sadeh, Raviv, & Gruber, 2000).
Analyses showed bedtime problems but not nighttime waking problems in 3rd grade to significantly predict internalizing problems in adolescence. This result must be considered within the developmental period sleep problems were assessed. Specifically, our measure of bedtime problems examined a range of child behaviors occurring at or around lights out that typify behavioral insomnia in school-aged children, such as bedtime resistance or refusal. Younger children may be more likely to awaken during the night and seek parental comfort—problems that typically resolve with age. By comparison, problems with sleep initiation may persist over time and strengthen a developmental shift toward an evening circiadian preference in adolescence (Jenni, Achermann, & Carskadon, 2005), in turn increasing internalizing risk (Giannotti, Cortesi, Sebastiani, & Ottaviano, 2002; Selvi et al., 2010). As such, the current set of results may not generalize to younger children.
It is also possible that some bedtime problems serve to forecast later internalizing issues more than others. As an example, bedtime/nighttime fears serve as a specific marker for later anxiety (Kushnir, Gothelf, & Sadeh, 2014), and approximately 20% of children with nighttime fears suffer from anxiety disorders (Muris, Merckelbach, Mayer, & Prins, 2000). Although commonly described by parents as “sleep problems,” the extent to which nighttime fears correspond with actual sleep alterations is not known. Persistently elevated levels of arousal at bedtime, poor child coping strategies, parental sleep loss, and/or responses to children’s fearful nighttime behavior may equally serve to elevate affective risk. Still, the finding that 3rd grade bedtime problems rather than nighttime waking problems predict later internalizing symptoms has potentially meaningful implications for early intervention efforts. With additional research clarifying the specific types of sleep problems that elevate risk, development of more targeted interventions may be possible.
In comparison with bedtime problems, the relatively low frequency of nighttime waking problems reported by parents was somewhat surprising. A lower base rate together with nonsignificant prediction of adolescent internalizing problems may be explained by the specific items that comprised this scale. For example, parasomnias such as night terrors are normative in young children and diminish with age (DSM-5, 2013). Moreover, parental awareness of night awakenings may only occur when they are frequent and/or severe enough to require parental involvement (i.e., child calls for or seeks out the parent on awakening from sleep). Thus, in addition to incorporating child reports, research exploring relationships between more specific types of nighttime awakenings and subsequent internalizing symptoms in youth is needed.
We chose to examine emotional reactivity at/around the age of 11 years based on developmental research suggesting the onset of puberty to mark a key developmental window for understanding the emergence of internalizing symptoms (Dahl, 2004; Spear, 2000; Steinberg et al., 2006). Analyses showed emotional reactivity in late childhood to partially mediate (i.e., explain) the relationship between middle childhood bedtime problems and internalizing problems at age 15. This finding is consistent with a body of experimental research showing inadequate sleep to produce heightened levels of emotional arousal (Cousins et al., 2011; Franzen et al., 2009) as well as cross-sectional studies finding increased levels of emotional reactivity among youth with internalizing problems and disorders (Suveg & Zeman, 2004; Weems, Zakem, Costa, Cannon, & Watts, 2005). However, this mediational effect was not observed after including levels of emotional reactivity in middle childhood in the model. This result likely reflects the fact that individual differences in emotional reactivity are observable aspects of temperament that emerge during infancy and remain relatively stable across development (Fox, 1989; Gunnar, Porter, Wolf, Rigatuso, & Larson, 1995). Studies comparing emotional reactivity to emotion regulation skills in youth also find consistent levels of reactivity, whereas regulatory skills continue to develop with age (McRae et al., 2012; Silvers et al., 2012). Although our reactivity measure was comprised not just of items reflecting negative emotions but of reactivity/arousal in general (e.g., “When happy, my child is contented and calm rather than exhilarated and excited”), we did not specifically assess dimensions of temperament in the current study. Ostensibly, difficulty settling down for sleep, problems falling asleep, and intense emotional displays during the day represent behaviors occurring along a broader dimension of emotional arousal.
Limitations
Several limitations need to be considered. Although bedtime and nighttime waking problems scales were derived from a validated sleep measure (Owens et al., 2000), the reliability of this alternative version of the original CSHQ has not been established. Additionally, the persistence of bedtime and nighttime waking problems was not assessed in the current study, and previous research has highlighted the chronicity of sleep problems to be particularly important in predicting later internalizing symptoms (Gregory et al., 2005). Although evidence for a bidirectional relationship exists between sleep and internalizing problems (Cousins et al., 2011; Fuligni & Hardway, 2006), inconsistent measurement of sleep across time points (i.e., adolescents reported on their morningness/eveningness preferences at age 15 rather than sleep behaviors) prevented meaningful examination of bidirectional effects. Still, internalizing symptoms in middle childhood may contribute to the maintenance of specific sleep problems across development.
We examined emotional reactivity in the current study but note this is only one aspect of Gross’s five-part process model of emotional generation (Gross, 1998) and other related and salient processes (e.g., emotion regulation) were not assessed. We also relied on parent report of emotional reactivity rather than self-reports or objective measures. Physiologic measures would ultimately provide stronger evidence for the role of emotional reactivity; although self- and parent-reported measures of emotion correlate with objective measures (El-Sheikh & Buckhalt, 2005; Vasilev, Crowell, Beauchaine, Mead, & Gatzke-Kopp, 2009). Further, we focused on internalizing symptoms in adolescence, but sleep problems have been shown to forecast externalizing problems as well (Gregory et al., 2008). Lastly, as both sleep and emotional reactivity measures were collected via maternal report, shared-source variance may have impacted our results.
Implications and Conclusions
Results from the current study make several important contributions to our understanding of childhood sleep problems and their relation to later psychological problems. Although a majority of studies reveal sleep problems, broadly, to predict later internalizing problems (Gregory et al., 2004, 2005; Gregory & O'Connor, 2002; Ong et al., 2006), our results suggest this relationship may be more specific to problematic behaviors occurring at or around bedtime. If replicated, this finding could hold important implications for childhood assessment approaches and prevention/early intervention strategies. For example, brief interventions that target the sleep onset period specifically may produce more efficient and robust reduction of internalizing risk. Particularly as the U.S. healthcare system becomes more integrated, such interventions hold potential for wider dissemination and, ultimately, reducing the societal costs of psychological care.
Our results also suggest that levels of emotional reactivity partially explicate longitudinal links between sleep and internalizing symptom domains. Incorporation of objective measures of reactivity and assessment of other aspects of the emotion generation process (e.g., emotion regulation) is necessary nonetheless for clarifying mechanistic relationships and advancing understanding. Finally, the ways in which early sleep patterns and simultaneous changes in emotion-based skills intersect to heighten affective vulnerability during the post-pubertal years is an area of increasing attention but as of yet has limited understanding. Longitudinal, multi-method designs are best suited to addressing these developmental questions.
Acknowledgments
The authors are grateful for the families for their participation in this research. The authors express their thanks to Jennifer Tackett, PhD, Haniko Yoshida, PhD, and members of the Sleep and Anxiety Center of Houston for their support and feedback throughout this project.
Funding
The larger study on which this report is based, the National Institute of Child Health and Human Development (NICHD) Study of Early Child Care and Youth Development, was directed by a Steering Committee and supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institutes of Health, through a set of cooperative agreements (grant numbers 5U10HD027040, 5U10HD025460, 5U10HD025447, 5U10HD025420, 5U10HD025456, 5U01HD033343, 5U10HD025445, 5U10HD025451, 5U10HD025430, 5U10HD025449, 5U10HD027040, and 5U10HD025455). The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the Interuniversity Consortium for Political and Social Research, the NICHD, or the National Institutes of Health.
Conflicts of interest: None declared.
References
- Achenbach T. M. (1991a). Manual for the child behavior checklist/4-18 and 1991 profile. Burlington, VT: Department of Psychiatry, University of Vermont. [Google Scholar]
- Achenbach T. M. (1991b). Manual for the youth self-report and 1991 profile. Burlington, VT: Department of Psychiatry, University of Vermont. [Google Scholar]
- Achenbach T. M., Howell C. T., Quay H. C., Conners C. K. (1991). National survey of problems and competencies among four- to sixteen-year-olds: Parents' reports for normative and clinical samples. Monographs of the Society for Research in Child Development , 56, 1–131. [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistic Manual of Mental Disorders (DSM-5). Washington, DC: American Psychiatric Association. [Google Scholar]
- Baum K. T., Desai A., Field J., Miller L. E., Rausch J., Beebe D. W. (2014). Sleep restriction worsens mood and emotion regulation in adolescents. Journal of Child Psychology and Psychiatry , 55, 180–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown B. B. (2004). Adolescents' relationships with peers. In R. M. Lerner & L. Steinberg (Eds.), Handbook of adolescent psychology (Vol. 2, pp. 363–394). Hoboken, NJ: John Wiley & Sons, Inc. [Google Scholar]
- Calkins S. D., Hill A. (2007). Caregiver influences on emerging emotion regulation. In Gross J. J. (Ed.), Handbook of emotion regulation. New York, NY: The Guilford Press. [Google Scholar]
- Casey B. J., Giedd J. N., Thomas K. M. (2000). Structural and functional brain development and its relation to cognitive development. Biological Psychology , 54, 241–257. [DOI] [PubMed] [Google Scholar]
- Cousins J. C., Whalen D. J., Dahl R. E., Forbes E. E., Olino T. M., Ryan N. D., Silk J. S. (2011). The bidirectional association between daytime affect and nighttime sleep in youth with anxiety and depression. Journal of Pediatric Psychology , 36, 969–979. doi:10.1093/jpepsy/jsr036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahl R. E. (1996). The impact of inadequate sleep on children's daytime cognitive function. Seminars in Pediatric Neurology , 3(1), 44–50. doi:10.1016/S1071-9091(96)80028-3 [DOI] [PubMed] [Google Scholar]
- Dahl R. E. (2004). Adolescent brain development: A period of vulnerabilities and opportunities. Keynote address. Annals of the New York Academy of Sciences , 1021(1), 1–22. [DOI] [PubMed] [Google Scholar]
- Dearing E., McCartney K., Marshall N. L., Warner R. M. (2001). Parental reports of children’s sleep and wakefulness: Longitudinal associations with cognitive and language outcomes. Infant Behavior and Development , 24, 151–170. [Google Scholar]
- DeVellis R. F. (2003). Factor analysis, scale development theory and application. Applied Social Research Method Series , 26, 10–137. [Google Scholar]
- Dinges D. F., Pack F., Williams K., Gillen K. A., Powell J. W., Ott G. E., Aptowicz C., Pack A. I. (1997). Cumulative sleepiness, mood disturbance and psychomotor vigilance performance decrements during aweek of sleep restricted to 4-5 hours per night. Sleep: Journal of Sleep Research and Sleep Medicine , 20, 267–277. [PubMed] [Google Scholar]
- El-Sheikh M., Buckhalt J. A. (2005). Vagal regulation and emotional intensity predict children's sleep problems. Developmental Psychobiology , 46, 307–317. doi:10.1002/dev.20066 [DOI] [PubMed] [Google Scholar]
- Fox N. A. (1989). Psychophysiological correlates of emotional reactivity during the first year of life. Developmental Psychology , 25, 364. [Google Scholar]
- Franzen P. L., Buysse D. J., Dahl R. E., Thompson W., Siegle G. J. (2009). Sleep deprivation alters pupillary reactivity to emotional stimuli in healthy young adults. Biological Psychology , 80, 300–305. doi:10.1016/j.biopsycho.2008.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuligni A. J., Hardway C. (2006). Daily variation in adolescents’ sleep, activities, and psychological well-being. Journal for Research on Adolesence , 16, 353–378. [Google Scholar]
- Furman W. (2002). The emerging field of adolescent romantic relationships. Current Directions in Psychological Science , 11, 177–180. [Google Scholar]
- Gee D. G., Humphreys K. L., Flannery J., Goff B., Telzer E. H., Shapiro M., Hare T. A., Bookheimer S. Y., Tottenham N. (2013). A developmental shift from positive to negative connectivity in human amygdala–prefrontal circuitry. The Journal of Neuroscience , 33, 4584–4593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giannotti F., Cortesi F., Sebastiani T., Ottaviano S. (2002). Circadian preference, sleep and daytime behaviour in adolescence. Journal of Sleep Research , 11, 191–199. [DOI] [PubMed] [Google Scholar]
- Glaze D. G., Rosen C. L., Owens J. A. (2002). Toward a practical definition of pediatric insomnia. Current Therapeutic Research , 63, B4–B17. [Google Scholar]
- Greene G., Gregory A. M., Fone D., White J. (2014). Childhood sleeping difficulties and depression in adulthood: The 1970 British Cohort Study. Journal of Sleep Research , 24, 19–23. [DOI] [PubMed] [Google Scholar]
- Gregory A. M., Caspi A., Eley T. C., Moffitt T. E., O'Connor T. G., Poulton R. (2005). Prospective longitudinal associations between persistent sleep problems in childhood and anxiety and depression disorders in adulthood. Journal of Abnormal Child Psychology , 33, 157–163. [DOI] [PubMed] [Google Scholar]
- Gregory A. M., Eley T. C., O'Connor T. G., Plomin R. (2004). Etiologies of associations between childhood sleep and behavioral problems in a large twin sample. Journal of the American Academy of Child and Adolescent Psychiatry , 43, 744–751. doi:10.1097/01.chi/0000122798.47863.a5 [DOI] [PubMed] [Google Scholar]
- Gregory A. M., O'Connor T. G. (2002). Sleep problems in childhood: A longitudinal study of developmental change and association with behavioral problems. Journal of the American Academy of Child and Adolescent Psychiatry , 41, 964–971. doi:10.1097/00004583-200208000-00015 [DOI] [PubMed] [Google Scholar]
- Gregory A. M., Van der Ende J., Willis T. A., Verhulst F. C. (2008). Parent-reported sleep problems during development and self-reported anxiety/depression, attention problems, and aggressive behavior later in life. Archives of Pediatric Adolescent Medicine , 162, 330–335. doi:10.1001/archpedi.162.4.330 [DOI] [PubMed] [Google Scholar]
- Gross J. J. (1998). The Emerging Field of Emotion Regulation: An Integrative Review. Review of General Psychology , 2(3), 271–299. [Google Scholar]
- Gross J. J. (2015). Emotion regulation: Conceptual and empirical foundations. In J. J. Gross (Ed.), Handbook of emotion regulation (2nd ed.). New York, NY: The Guilford Press. [Google Scholar]
- Gunnar M. R., Porter F. L., Wolf C. M., Rigatuso J., Larson M. C. (1995). Neonatal stress reactivity: Predictions to later emotional temperament. Child Development , 66(1), 1–13. [DOI] [PubMed] [Google Scholar]
- Hayes A. F. (1996). Permutation test is not distribution-free: Testing HQ: p = 0. Psychological Methods , 1, 184–198. [Google Scholar]
- Hayes A. F. (2013). Introduction to mediation, moderation, and conditional process analysis. New York, NY: Guilford. [Google Scholar]
- Hayes A. F., Matthes J. (2009). Computational procedures for probing interactions in OLS and logistic regression: SPSS and SAS implementations. Behavioral Research Methods , 41, 924–936. doi:10.3758/brm.41.3.924 [DOI] [PubMed] [Google Scholar]
- Jenni O. G., Achermann P., Carskadon M. A. (2005). Homeostatic sleep regulation in adolescents. Sleep , 28, 1446. [DOI] [PubMed] [Google Scholar]
- Joormann J., Talbot L., Gotlib I. H. (2007). Biased processing of emotional information in girls at risk for depression. Journal of Abnormal Psychology , 116, 135–143. doi:10.1037/0021-843x.116.1.135 [DOI] [PubMed] [Google Scholar]
- Kahn A., Van de Merckt C., Rebuffat E., Mozin M. J., Sottiaux M., Blum D., Hennart P. (1989). Sleep problems in healthy preadolescents. Pediatrics , 84(3), 542–546. [PubMed] [Google Scholar]
- Kahn-Greene E. T., Killgore D. B., Kamimori G. H., Balkin T. J., Killgore W. D. (2007). The effects of sleep deprivation on symptoms of psychopathology in healthy adults. Sleep Medicine , 8, 215–221. doi:10.1016/j.sleep.2006.08.007 [DOI] [PubMed] [Google Scholar]
- Kushnir J., Gothelf D., Sadeh A. (2014). Nighttime fears of preschool children: A potential disposition maker for anxiety? Comprehensive Psychiatry , 55, 336–341. [DOI] [PubMed] [Google Scholar]
- Larsen R. J., Diener E. (1987). Affect intensity as an individual difference characteristic: A review Journal of Research in Personality , 21(1), 1–39. [Google Scholar]
- Leotta C., Carskadon M., Acebo C., Seifer R., Quinn B. (1997). Effects of acute sleep restriction on affective response in adolescents: Preliminary results. Sleep research , 26, 201. [Google Scholar]
- Maume D. J. (2013). Social ties and adolescent sleep disruption. Journal of Health and Social Behavior , 54, 498–515. [DOI] [PubMed] [Google Scholar]
- McNamara P., Belsky J., Fearon P. (2003). Infant sleep disorders and attachment: Sleep problems in infants with insecure-resistant versus insecure-avoidant attachments to mother. Sleep and Hypnosis , 5, 17–26. [Google Scholar]
- McRae K., Gross J. J., Weber J., Robertson E. R., Sokol-Hessner P., Ray R. D., Gabrieli J. D., Ochsner K. N. (2012). The development of emotion regulation: An fMRI study of cognitive reappraisal in children, adolescents and young adults. Social Cognitive and Affective Neuroscience , 7, 11–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meldrum R. C., Barnes J., Hay C. (2015). Sleep deprivation, low self-control, and delinquency: A test of the strength model of self-control. Journal of Youth and Adolescence , 44, 465–477. [DOI] [PubMed] [Google Scholar]
- Mindell J. A. (1993). Sleep disorders in children. Health Psychol , 12(2), 151–162. [DOI] [PubMed] [Google Scholar]
- Muris P., Merckelbach H., Mayer B., Prins E. (2000). How serious are common childhood fears? Behavior Research and Therapy , 38(3), 217–228. [DOI] [PubMed] [Google Scholar]
- NICHD Early Child Care Research Network (2005). Child care and child development: Results from the NICHD study of early child care and youth development. New York, NY: Guilford Press.
- O'Brien S. F., Bierman K. L. (1988). Conceptions and perceived influence of peer groups: Interviews with preadolescents and adolescents. Child Development, 59, 1360–1365. [DOI] [PubMed] [Google Scholar]
- Ong S. H., Wickramaratne P., Tang M., Weissman M. M. (2006). Early childhood sleep and eating problems as predictors of adolescent and adult mood and anxiety disorders. Journal of Affective Disorders , 96(1–2), 1–8. doi:10.1016/j.jad.2006.05.025 [DOI] [PubMed] [Google Scholar]
- Owens J. A., Spirito A., McGuinn M. (2000). The Children's Sleep Habits Questionnaire (CSHQ): Psychometric properties of a survey instrument for school-aged children. Sleep, 23, 1043–1052. [PubMed] [Google Scholar]
- Peugh J. L., Enders C. K. (2004). Missing data in educational research: A review of reporting practices and suggestions for improvement. Review of Educational Research , 74, 525–556. [Google Scholar]
- Preacher K. J., Hayes A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavioral Research Methods , 40, 879–891. [DOI] [PubMed] [Google Scholar]
- Sadeh A., Raviv A., Gruber R. (2000). Sleep patterns and sleep disruptions in school-age children. Developmental Psychology , 36, 291–301. [DOI] [PubMed] [Google Scholar]
- Sagaspe P., Sanchez-Ortuno M., Charles A., Taillard J., Valtat C., Bioulac B., Philip P. (2006). Effects of sleep deprivation on Color-Word, Emotional, and Specific Stroop interference and on self-reported anxiety. Brain and Cognition , 60, 76–87. [DOI] [PubMed] [Google Scholar]
- Salovey P., Mayer J. D., Caruso D., Yoo S. (2009). The positive psychology of emotional intelligence. In C. R. Snyder & S. J. Lopez (Eds.), Handbook of positive psychology (2nd ed., pp. 237–248). New York, NY: Oxford University Press. [Google Scholar]
- Schumann C. M., Hamstra J., Goodlin-Jones B. L., Lotspeich L. J., Kwon H., Buonocore M. H., Lammers C. R., Reiss A. L., Amaral D. G. (2004). The amygdala is enlarged in children but not adolescents with autism; the hippocampus is enlarged at all ages. The Journal of Neuroscience , 24, 6392–6401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selvi Y., Aydin A., Boysan M., Atli A., Agargun M. Y., Besiroglu L. (2010). Associations between chronotype, sleep quality, suicidality, and depressive symptoms in patients with major depression and healthy controls. Chronobiology International , 27, 1813–1828. doi:10.3109/07420528.2010.516380 [DOI] [PubMed] [Google Scholar]
- Silk J. S., Steinberg L., Morris A. S. (2003). Adolescents' emotion regulation in daily life: Links to depressive symptoms and problem behavior. Child Development , 74, 1869–1880. [DOI] [PubMed] [Google Scholar]
- Silvers J. A., McRae K., Gabrieli J. D., Gross J. J., Remy K. A., Ochsner K. N. (2012). Age-related differences in emotional reactivity, regulation, and rejection sensitivity in adolescence. Emotion , 12, 1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spear L. P. (2000). The adolescent brain and age-related behavioral manifestations. Neuroscience and Biobehavioral Reviews , 24, 417–463. [DOI] [PubMed] [Google Scholar]
- Steinberg L., Dahl R. E., Keating D., Kupfer D. J., Masten A. S., Pine D. S. (2006). The study of developmental psychopathology in adolescence: Integrating affective neuroscience with the study of context. In Cicchetti D., Cohen D. J. (Eds.), Developmental neuroscience (2nd ed.). Hoboken, NJ: John Wiley & Sons Inc. [Google Scholar]
- Steinberg L., Morris A. S. (2001). Adolescent development. Journal of Cognitive Education and Psychology , 2, 55–87. [Google Scholar]
- Suveg C., Zeman J. (2004). Emotion regulation in children with anxiety disorders. Journal of Clinical Child and Adolescent Psychology , 33, 750–759. doi:10.1207/s15374424jccp3304_10 [DOI] [PubMed] [Google Scholar]
- Talbot L. S., McGlinchey E. L., Kaplan K. A., Dahl R. E., Harvey A. G. (2010). Sleep deprivation in adolescents and adults: Changes in affect. Emotion , 10, 831–841. doi:10.1037/a0020138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas A. G., Monahan K. C., Lukowski A. F., Cauffman E. (2015). Sleep problems across development: A pathway to adolescent risk taking through working memory. Journal of Youth and Adolescence , 44, 447–464. [DOI] [PubMed] [Google Scholar]
- Vasilev C. A., Crowell S. E., Beauchaine T. P., Mead H. K., Gatzke-Kopp L. M. (2009). Correspondence between physiological and self-report measures of emotion dysregulation: A longitudinal investigation of youth with and without psychopathology. Journal of Child Psychology and Psychiatry , 50, 1357–1364. [DOI] [PubMed] [Google Scholar]
- Weems C. F., Zakem A. H., Costa N. M., Cannon M. F., Watts S. E. (2005). Physiological response and childhood anxiety: Association with symptoms of anxiety disorders and cognitive bias. Journal of Clinical Child and Adolescent Psychology , 34, 712–723. [DOI] [PubMed] [Google Scholar]
- Yurgelun-Todd D. (2007). Emotional and cognitive changes during adolescence. Current Opinion in Neurobiology , 17, 251–257. [DOI] [PubMed] [Google Scholar]


