Abstract
Policy Points:
The expansive goals of the Health Information Technology for Economic and Clinical Health (HITECH) Act required the simultaneous development of a complex and interdependent infrastructure and a wide range of relationships, generating points of vulnerability.
While federal legislation can be a powerful stimulus for change, its effectiveness also depends on its ability to accommodate state and local policies and private health care markets.
Ambitious goals require support over a long time horizon, which can be challenging to maintain. The future of health information technology (health IT) support nationally is likely to depend on the ability of the technology to satisfy its users that its functionalities address the interests policymakers and other stakeholders have in using technology to promote better care, improved outcomes, and reduced costs.
Context
The Health Information Technology for Economic and Clinical Health (HITECH) Act set ambitious goals for developing electronic health information as one tool to reform health care delivery and improve health outcomes. With HITECH's grant funding now mostly exhausted but statutory authority for standards remaining, this article looks back at HITECH's experience in the first 5 years to assess its implementation, remaining challenges, and lessons learned.
Methods
This review derives from a global assessment of the HITECH Act. Earlier, we examined the logic of HITECH and identified interdependencies critical to its ultimate success. In this article, we build on that framework to review what has and has not been accomplished in building the infrastructure authorized by HITECH since it was enacted. The review incorporates quantitative and qualitative evidence of progress from the global assessment and from the evaluations funded by the Office of the National Coordinator for Health Information Technology (ONC) of individual programs authorized by the HITECH Act.
Findings
Our review of the evidence provides a mixed picture. Despite HITECH's challenging demands, its complex programs were implemented, and important changes sought by the act are now in place. Electronic health records (EHRs) now exist in some form in most professional practices and hospitals eligible for HITECH incentive payments, more information is being shared electronically, and the focus of attention has shifted from adoption of EHRs toward more fundamental issues associated with using health information technology (health IT) to improve health care delivery and outcomes.
In some areas, HITECH's achievements to date have fallen short of the hopes of its proponents as it has proven challenging to move meaningful use beyond the initial low bar set by Meaningful Use Stage 1. EHR products vary in their ability to support more advanced functionalities, such as patient engagement and population‐based care management. Many barriers to interoperability persist, limiting electronic communication across a diverse set of largely private providers and care settings.
Conclusions
Achieving the expansive goals of HITECH required the simultaneous development of a complex and interdependent infrastructure and a wide range of relationships, some better positioned to move forward than others. To date, it has proven easier to get providers to adopt EHRs, perhaps in response to financial incentives to do so, than to develop a robust infrastructure that allows the information in EHRs to be used effectively and shared not only within clinical practices but also across providers. Effective exchange of data is necessary to drive the kinds of delivery and payment reforms sought nationwide.
Keywords: health information technology, health care delivery, federal health policy, health reform
The health information technology for economic and Clinical Health (HITECH) Act, enacted as part of the American Recovery and Reinvestment Act of 2009 (ARRA), has been a major health policy initiative seeking to promote the use of electronic health information as one tool to reform the delivery of health care and improve health outcomes. Early in HITECH's implementation, we analyzed factors that would drive initial efforts to adopt electronic health records (EHRs) and expand health information exchange (HIE) to support meaningful use (MU).1 In that analysis, we examined the logic behind HITECH's requirements and programs in light of the factors driving EHR uptake (affordability, product availability, practice integration, and provider attitudes) and HIE (data harmonization, privacy and security, organizational interfaces, access to technology, provider participation, and patient support). Our analysis showed how the ambitious scope of HITECH's objectives would require rapid and simultaneous progress on multiple fronts, with critical interdependencies complicating execution. Such interdependencies were particularly challenging because key decisions important to the ultimate success of the HITECH Act would be made by private providers and diverse state and local public and private organizations, over which the federal government had only limited authority.
HITECH's funding is now mostly disbursed, but federal authority to establish standards and other requirements for health information technology (health IT) remains, and collaborative engagement with states and the private sector continues. This article, developed as part of a larger project funded by the Office of the National Coordinator for Health Information Technology (ONC) to provide a global assessment of the HITECH Act, looks back at the experience of HITECH to examine what was accomplished in terms of implementing the HITECH Act, remaining challenges, and lessons learned. As part of our evaluation, we monitored the progress of key activities and looked in more depth at selected aspects of implementation.2 This article draws on that and the other work ONC commissioned to evaluate HITECH and its specific programs, many of which have received little attention in current publications. The article provides a high‐level synthesis of what research and evaluation reveals about the implementation of HITECH and its various programs, including progress on key indicators that ONC presents on its “dashboard” and other findings that stem from research by our colleagues and ourselves.
The analysis is not without its limitations. First, the scope and time line mandated by HITECH—and the guidance and resources available for this study—meant that benchmarks to measure progress were limited in some areas. Second, while we summarize what is known about HITECH's ability to achieve its ultimate goals, we can provide only limited insight on this topic within the time frame available for study. Third, the article emphasizes findings that provide a national perspective, generally based on federal data sources and studies. While this perspective is not comprehensive, we believe it includes the major national information sources on this topic. Many of these reports and informational pieces are not well documented in the available peer literature, and thus this synthesis provides a valuable lens through which other studies of health IT can be assessed.
The Logic of HITECH
Figure 1 summarizes the core logic of the HITECH Act, including the policies and programs built into HITECH to achieve its goals, key features of the environment in which it is being implemented, and the critical interdependencies that will influence the ultimate success of the HITECH Act. As is well recognized,3 HITECH provided incentives and support for providers to adopt EHRs and allow their information to be exchanged electronically to promote the MU of health information and improve health care outcomes. Even though HITECH preceded the Patient Protection and Affordable Care Act of 2010 (ACA) it anticipated the ACA and sought to develop digitized health information regarded as important in reforming health care delivery.4, 5 As reflected in Figure 1, HITECH's programs and policies sought to address key drivers behind the adoption of EHRs (such as affordability and availability) and HIE (such as data harmonization and organizational interfaces).
Figure 1.
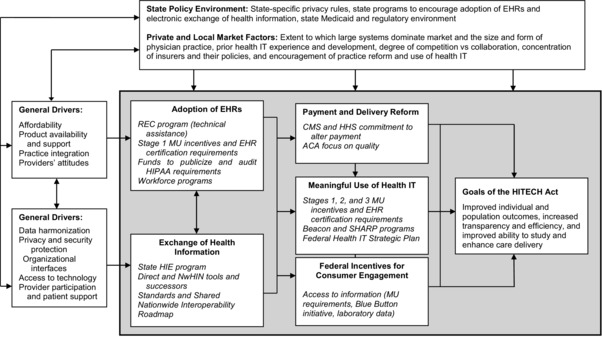
Framework for Global Assessment of HITECHa
Abbreviations: REC, Regional Extension Center; HIPAA, Health Insurance Portability and Accountability Act of 1996; CMS, Centers for Medicare and Medicaid Services; HHS, US Department of Health and Human Services; NwHIN, Nationwide Health Information Network. Italics = HITECH and related initiatives. aAuthors’ construct, building on Blumenthal3 for the core framework, Gold and colleagues1 for drivers of EHR adoption and HIE, and Ricciardi and colleagues6 for the aims of consumer engagement.
Only partially addressed by HITECH is the impact on implementation of the considerable variation in state policy environments and private and local market forces across the country that have influenced the historical experience with health IT, the form of delivery, and the practical realities of implementing change.
Meaningful Use as Central Concept
As emphasized by the National Coordinator for Health IT when HITECH was adopted,3 HITECH's central concept is to encourage MU of EHRs to enhance individual and population health outcomes and research. MU requirements were envisioned as evolving over 3 stages, becoming increasingly sophisticated over time as capacity grew.7 The intent was to move beyond meeting formal requirements that could be “checked off” toward effectively changing the way care is delivered and how patients and providers interact—what some refer to as “meaningful, meaningful use.”8 HITECH's components provide building blocks for this transition.
Critical Building Blocks
Adoption of EHRs
To encourage providers to adopt EHR systems, HITECH authorized up to $27 billion in Medicare and federal Medicaid payments over 10 years to eligible providers who adopted EHR systems that were certified as meeting federal standards and who attested to meeting MU requirements. (Eligible hospitals received payments from both Medicare and Medicaid; eligible professionals had to choose if they qualified for both.) The HITECH Act also funded a Regional Extension Center (REC) program on a short‐term basis to assist high‐priority providers in making the transition if they needed help to adopt and use EHRs. (RECs focused on providers in small practices and those serving disadvantaged or rural populations, anticipating that such support could be important to reduce disparities resulting from uneven access to market‐based support.) Short‐term workforce programs were funded to meet the anticipated increased demand for qualified professionals with skills in health IT.
Although privacy and security protections were already in place through the Health Insurance Portability and Accountability Act of 1996 (HIPAA), HITECH recognized the importance of these issues, with an emphasis on funding education and enforcement of HIPAA and identifying where additional protections might be required.
Exchange of Health Information
HITECH also sought to improve data harmonization and to enable features that would allow data to be electronically exchanged at diverse geographical levels. To complement national policy, the HITECH Act provided short‐term support for a state health information exchange (state HIE) program to work on exchange with stakeholders in states and local areas. Under HITECH, the US Department of Health and Human Services (HHS) also continued to work on national efforts to develop standards and mechanisms to promote exchange and protect the security and privacy of health information.
Supporting Meaningful Use of Health IT
Recognizing variations in health IT experience and maturity, the legislation authorized funding for a Beacon program,9 initially envisioned as supporting more advanced communities to illustrate the value of MU of health IT to improve health outcomes. The Strategic Health IT Advanced Research Project (SHARP) program was intended to spur applied research in select areas, including the security of health IT, patient‐centered cognitive support, network architecture, and the use of EHRs. The subsequent enactment of the ACA provided increased support for changes in health care delivery and payment that would complement MU requirements and enhance the value of electronic health information. Over time, recognition grew that patient engagement was also a critical aspect of change and the MU of information.6, 10
Time Frame and Resources
HITECH called for concurrent implementation on multiple fronts on a tight time line, in which government resources were front‐loaded. Implicit in the HITECH Act were assumptions that MU would transition through all 3 of its stages by 2016, with no additional Medicare financial incentive payments authorized after that year and penalties imposed starting in 2015 for those who did not begin to attest by 2014. Medicaid's initial payment requirements for eligible professionals were less demanding than Medicare's requirements on the front end; Medicaid payments were also higher than those of Medicare and are slated to continue until 2020. Grant‐supported programs involved substantially fewer resources than anticipated MU payments ($27 billion). Three‐quarters of the funds went to the REC and state HIE programs (Figure 2).
Figure 2.
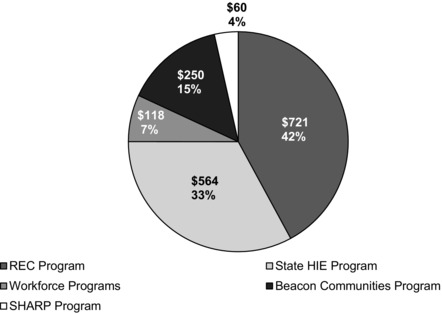
HITECH Grant Program Funding (in millions)a
aDerived from ONC grants management reports.
Funds for all grant‐supported programs have largely been spent (Figure 3). Funding was deliberately front‐loaded, consistent with the broader intent of ARRA (through which HITECH was authorized) to provide a short‐term stimulus for the economy. This front‐loading was especially true for the workforce programs, for which almost two‐thirds of the spending occurred in the first year (see Figure 3).
Figure 3.
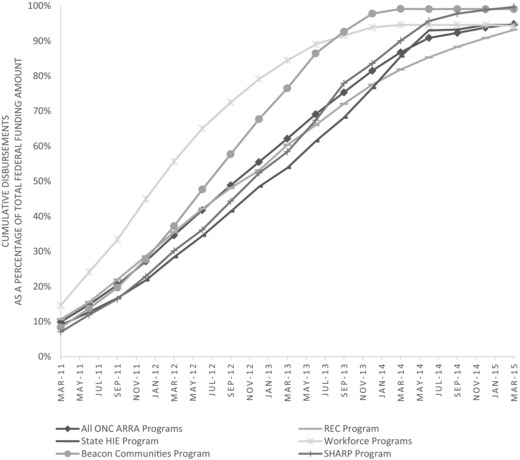
ONC Grant Program Cumulative Disbursements, 2011–2015a
aDerived from ONC grants management reports.
Implementation Experience
Moving From Meaningful Use Stage 1 to Stage 2 Slower Than Projected
As of September 2015, more than 307,000 Medicare‐eligible professionals (physicians, dentists, podiatrists, optometrists, and chiropractors) and nearly 4,500 Medicare‐eligible hospitals met at least MU Stage 1 requirements (Figure 4). This means that they have an EHR that meets certification requirements and that they have attested to use of that EHR that meets Stage 1 criteria.11 Because of the different rules under which they operate, some Medicaid‐eligible professionals (physicians, nurse practitioners, certified nurse‐midwives, dentists, and physician assistants) received initial payments upon acquisition of an EHR alone (adopt, implement, upgrade [AIU]) and have not yet gone on to meet the Stage 1 attestation requirements.12, 13
Figure 4.
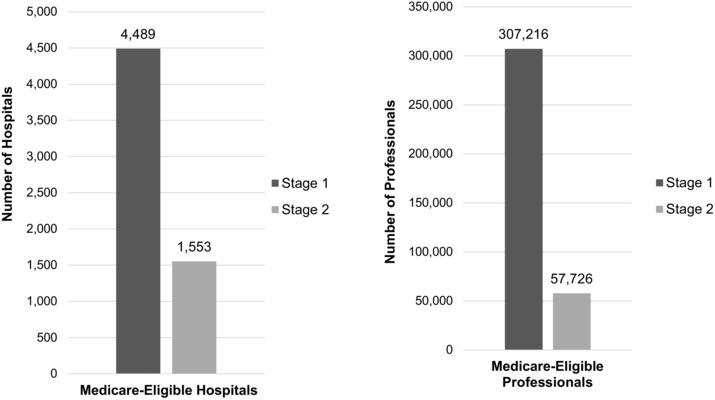
Medicare‐Eligible Hospitals and Professionals by Stage, September 2015a
aDerived from September 2015 EHR Incentive Program Summary Report.14
By December 2014, 94% of eligible hospitals had been paid for demonstrating MU Stage 1 in the Medicare incentives program.15 ONC estimates that 73% of eligible health professionals had been paid by 2014.16 Physicians that adopted EHRs following HITECH (2011‐2013) are particularly likely to cite incentive payments or financial penalties as major influences on their decisions.17
Originally, Medicare providers attesting to MU Stage 1 in 2011, at the program's start, were to begin Stage 2 attestation in 2013. Deadlines were extended, however, and Stage 2 attestations, especially among eligible professionals, did not begin to grow until 2015. As a result, Stage 3 has been delayed from its initial start date of 2015; proposed Stage 3 requirements were sent out for comment in summer 2015.18 The final rules, released for public comment in October 2015, allow providers to attest to Stage 3 for the first time on a voluntary basis in 2017.19 Stage 3 is viewed as a streamlined set of functionalities that can be met more flexibly but are also more advanced. As currently envisioned, Stage 3 requirements will apply to most eligible providers in 2018, regardless of their previous status.
The delays in moving from MU Stage 1 to later stages of adoption are important, as many advanced functionalities, such as electronic HIE and patient engagement, were addressed only in limited form in Stage 1 in the interest of jump‐starting the program. Due to these delays, fewer providers will be offered the carrot of financial payments to make the transition as the program shifts from payments to penalties, potentially influencing the provider support that is essential to the success of HITECH. Providers’ acceptance of future stages of MU may depend on how well the MU requirements reinforce their particular needs and how the dominant forms of delivery and payment evolve.
Broad‐Based EHR Adoption
EHR Adoption Nationwide
In 2014, nearly all reporting hospitals (97%) possessed certified EHR technology, with three‐quarters (75.5%) having at least a basic system that included a defined set of functions in at least 1 unit in the hospital. This change represents a substantial increase from the adoption rates of 15.6% in 2010 and 9.4% in 2008.20 Among office‐based physician practices in 2014, 83% had an EHR system, with half (51%) having a basic system with specific functionalities important to MU—more than double the share that had such a system in 2009 (21.8%) before HITECH was passed.21 One study found that while the percentage of physicians adopting any EHR system had increased by more than it would have without MU incentives, the difference was not statistically significant.22 But EHR adoption rates are higher among hospitals eligible than those ineligible for incentives.23 Researchers comparing trends in EHR adoption rates for the acute care hospitals eligible for MU incentives to those of ineligible hospitals (such as specialty and longer‐stay hospitals) attribute the much stronger gains in EHR use to HITECH and its MU incentives.24 Other researchers, estimating the increase in payments from Medicaid and Medicare that each hospital anticipated receiving from the MU payments in its first year of eligibility, found that these incentives led to an additional 10% of hospitals adopting an electronic medical record in 2011.25 This same study estimated that the 2011 level of adoption would have been reached in 2013 without the incentives.
EHR adoption is broad but to some extent still uneven, with lower rates of adoption in small rural hospitals and in small specialty and physician‐owned practices.26 Adoption rates also tend to be low for many providers excluded from MU incentives, such as those involved in long‐term care and behavioral health.27 Such gaps create challenges for care management.
The REC Program and the “Digital Divide.”
The REC program was structured to give program grantees strong incentives to encourage high‐priority providers to attest to MU since, after an initial small payment, a grantee's future funding was dependent on the grantee's demonstrated success in signing up professionals, having them adopt EHRs, and attaining sufficient quality for MU payments. ONC's program data show that the REC program met its goal of getting 100,000 providers to MU, with a focus on high‐priority providers.28 ONC's external evaluation of the REC program by the American Institutes for Research (AIR)29 found that participating with an REC was positively associated with EHR adoption and receipt of MU payments among primary care physicians whose practices were small or served a large underserved population—a finding of the Government Accountability Office as well.30 While the form of payment used with RECs could incentivize grantees to sign up those providers readier to attest to MU (so‐called low‐hanging fruit), the REC evaluation showed that providers using the REC program included both early and late adopters and also were more likely to be those without ready access to other sources of support, such as hospital systems. This finding is consistent with the REC program's targeting those providers that fall through the cracks, as HITECH intended.
Critical ingredients behind REC success are less well understood; providers participating with RECs reported they were no less likely to experience challenges than nonparticipants, and the AIR evaluation was unable to distinguish among the multiple potential factors that may have contributed to this finding. With federal REC funding ending, the sustainability of RECs depended on their ability to survive in the marketplace (or on their finding other sources of support). The AIR evaluation found that, whereas some RECs are likely to achieve sustainability with revenue from users, most will face challenges in doing so, particularly as they lose staff when their grant funds decline. From a public policy perspective, the extent of loss will depend on how effective the REC has been. If effective RECs are not sustainable in the absence of a subsidy, it could create impediments to continued progress for high‐priority providers with no alternative sources of support.
Availability of Certified EHR Products and Practice Integration
HITECH succeeded in spurring a large and active vendor market to offer EHRs, especially for office‐based practices in which such products previously were rare. Our analysis of the ambulatory vendor market in 2012 showed that eligible office‐based professionals attesting to MU from 2011 to 2012 used products from 353 different vendors, although 16 firms accounted for 75% of the market.31 A common measure of market competition (the Herfindahl‐Hirschman Index32) showed the ambulatory market to be highly competitive, particularly for practices with 50 or fewer professionals. The vendors and external analysts we interviewed concurred that Stage 1 requirements set a relatively low bar for market entry.
Stage 1 certification requirements initially were effective in generating extensive product choice, but they may have contributed to longer‐term problems as vendors did not necessarily have to create products that anticipated requirements in later stages and for the more rigorous testing to be employed in the permanent certificate program set up in Stage 2.31 The literature shows that planning and vendor selection, workflow and software design, training and user support, and optimization and modification are all critical to the successful implementation of EHRs.33 Although both vendors and RECs say they have worked with providers on these issues,29, 31 providers’ dissatisfaction with the ability of products to integrate with their workflow has contributed to their opposition to moving forward with future stages of MU.34
Workforce Implications
Concerned that workforce limitations would serve as barriers to progress in EHR adoption, especially for small and rural physician practices and critical access hospitals,35 HITECH included front‐end funding for programs to support staff training in the relevant skills required by the HITECH Act.
ONC's external evaluation of these programs (done by NORC at the University of Chicago),36 found that, while variations existed across markets, the university and community college programs generally were well received by students and resulted in a higher share of graduates employed both overall and in the health IT field, as a result of the training they received. These programs also developed curriculum and credentialing tools that may prove valuable over time. The evaluation also found, however, that the programs were not as well connected to the employer community as they might have been.
Apart from direct workforce program effects, HITECH may have stimulated the growth of labor force opportunities in the private sector; the Bureau of Labor Statistics reported that health IT jobs grew by 50,000 as a result of HITECH, with a 20% growth projected from 2008 to 2018.37
Health Information Exchange Growing but Interoperability Still Limited
Electronic Exchange by Hospitals
Between 2010 and 2014, the percentage of nonfederal acute care hospitals that exchanged health information with any outside ambulatory provider or hospital increased from 44% to 76%.38 In 2014, 69% of hospitals exchanged laboratory results, 65% radiology reports, 64% summary of care records, and 55% medication histories. In 2008, the comparable figures were 35%, 37%, 25%, and 21%. Although geographical variation exists, the majority of hospitals in most states report some exchange with outside providers. The mechanisms used for such exchange are not defined and are likely to vary across hospitals.
Despite this progress, there are still barriers to exchange that limit its breadth. While the indicator used above is the same one ONC tracks on Health IT Dashboard for HITECH Progress, it is possible for a provider to satisfy the measure and still have relatively limited external exchange of information. In 2013, we interviewed staff at 6 large and diverse hospital systems with relatively high rates of exchange.39 We found that all of these systems had worked on achieving some form of exchange; some had made this a priority years ago. Although they supported broad‐based exchange, they saw many barriers to achieving it, including limited ability to exchange information with affiliated providers, the diversity of EHRs used, and uneven EHR uptake among some important provider groups. In their own efforts, they prioritized exchange involving providers within their health system or with outside providers with whom they share patients because the business case was stronger. Most supported more broad‐based community exchange, but they saw such exchange as complementing their work rather than replacing it and perceived barriers to the evolution of such broad‐based community‐wide exchange.
Electronic Exchange by Office‐Based Physicians
Exchange is more limited among office‐based practices, although, like hospitals, they give priority to exchange within their own organizations. Whereas 39% of office‐based physicians in 2013 reported any electronic exchange with other ambulatory providers or hospitals, rates were substantially higher within physicians’ own organizations than outside of them, and physicians in larger practices were much more likely to exchange information.40 Although the proportion of physicians reporting electronic exchange with other providers increased to 42% in 2014, only 16% of physicians were sharing at least 1 of 5 kinds of information with an outside provider.41
External Exchange with Clinical Laboratories
Stage 1 limited requirements for electronic exchange of laboratory test data to a “menu” measure because it was unclear whether laboratories could support that functionality. However, an ONC survey of clinical laboratories in 2012 found that 67% had the capability to send structured test results to the ordering physician, and 80% used that functionality, although performance varied across states.42 About 58% of test results that hospitals and intermediaries processed for Medicare patients from clinical laboratories were sent electronically. The 2 main barriers reported by surveyed laboratories were the high subscription rates for exchange services (19%) and the lack of harmonization among industry‐accepted standards (17%); about 9% said their primary challenge was that EHR systems could not accept their data. Stage 2 requires incorporating laboratory results into EHRs in a structured format, though it does not require that the results be received electronically.
Federal Efforts Supporting Exchange
Perhaps recognizing the tight time frame and limited program resources of HITECH, as well as research showing mixed results from earlier efforts to develop state or locally based exchange at those levels, HHS's initial requirements for exchange in Stage 1 were limited, though they set out markers to show areas of future intention. (Stage 2 added requirements for electronic exchange of summary of care records, laboratory test exchange [for hospitals only], consumer engagement, and additional public health reporting, for example.)
HHS developed the Direct Project, a set of technical standards and services to “push” information from one health care entity to another in a trusted network.43 Direct provides a national standards‐based, encrypted method for sending electronic health information at a relatively low cost. It is a simple way for providers with no other means to exchange information on a one‐way basis. Direct was piloted in 2 states, starting in February 2011,44 and ONC issued guidelines for its broader use in more than 40 statewide HIEs a few months later.45 Vendors seeking certification for Stage 2 are required to demonstrate that their product utilizes the Direct protocol.
HHS also developed the Nationwide Health Information Network (NwHIN, now eHealth Exchange), a set of standards, policies, and procedures that provides health systems with more advanced HIE functionality, in particular the ability to send and receive electronic health information with outside providers. In 2012, the exchange was transitioned to a nonprofit public and private partner, operating as Healtheway, now called the Sequoia Project, which runs the eHealth Exchange. A total of 110 systems and related organizations now participate in the eHealth Exchange.46
State HIE Program
Early on, ONC decided that both the relatively disappointing historical experience with state and regional exchange and the limited funds available to achieve progress over a short period of time meant that it was important to focus state efforts on immediate needs and local priorities.1 States were asked to develop state‐ and locality‐appropriate plans and priorities to use program resources to (1) create or foster exchange, (2) fill gaps in exchange capacity, and (3) encourage flow across exchanges. The flexibility afforded states, as well as the differences in their starting places and strategies, makes it challenging to assess the success as it is not clear what metrics should be employed nationally in the long term.
In its evaluation for ONC, NORC found that HIE increased on a variety of metrics over the period of the program, though there was considerable variation across states based on state context and program factors. The former (context) involves state‐specific demographic and market factors and the latter (program) involves decisions states make about exchange (such as governance structure, technical and consent models, and supportive legislation). State contextual factors were more important than decisions states made about the state HIE program itself in explaining the variation in state progress on HIE in the early years.47 Between 2011 and 2013, smaller states and states with more experience with EHR adoption before HITECH progressed more than other states. Over time, market factors (such as concentration of managed care and hospital competition) also influenced exchange levels. But program factors also influenced success, often in synergy with context. Across programs, states that used opt‐out versus opt‐in methods of consent to share information and those that drew down state HIE funds faster had higher levels of exchange in later years.
From state HIE grantee reports to ONC on factors affecting grantees’ progress, NORC found that they emphasized the value of diverse stakeholders for building trust relationships with aligned goals and a shared sense of ownership. Grantees said that payment reform did play, and would continue to play, a role in HIE expansion. They also said that making progress was more resource intensive than anticipated, standards and requirements were not clear, and there were issues with developers. However, they viewed interoperability as critical to improving care through health IT. Grantees saw HITECH as a catalyst for action with a onetime infusion of funds. They remained concerned about financial sustainability of HIE efforts as the program drew to a close.
Ongoing Federal Efforts at Standardization to Support Exchange
Although HITECH provided resources for federal leadership on standards and interoperability and the state HIE program to address issues of exchange, the legislation was silent on how standardization was to be achieved and exchange promoted in a health care system that was largely private and jointly regulated at the federal and state levels.1 Recognizing that interoperability to support exchange remains a challenge, HHS and its advisory groups continue to work on identifying ways to enhance it. ONC's federal advisory committees—the Health IT Policy Committee and the Health IT Standards Committee—both have been working for some time on these issues, which increasingly are recognized as critical to HITECH's ultimate success. In its Federal Health IT Strategic Plan for 2015–2020,48 HHS outlines broad‐based health IT goals to (1) advance person‐centered and self‐management health; (2) transform health care delivery and community health; (3) foster research, scientific knowledge, and innovation; and (4) enhance the nation's health IT infrastructure. In its Shared Nationwide Interoperability Roadmap,49 ONC calls for collaboration across stakeholders to advance nationwide interoperability that blends work to achieve success in the near term with progress on reaching the longer‐term vision. ONC has proposed a time line for high‐level critical actions needed to move this effort forward between 2015 and 2024. Early feedback on that plan suggests a focus on actions that are of highest priority and that will have the most impact.50
Limitations of Vendor Products
Emerging evidence also shows that some vendors use information‐blocking techniques that enhance their market position by making it more difficult for providers using their products to share information with those using other vendors’ products.51 Flexible certification requirements helped spur innovation in the vendor market; however, if some products prove less competitive, a market shakeout could cause disruption, particularly since vendors say product migration is not easy to execute.31
Recent analysis shows that most hospitals and eligible professionals could accommodate the upgrades in MU standards effective in 2014 by either upgrading their current product or obtaining additional products or modules from their current vendor.52 Whether such products can fully support the more advanced data aggregation and patient engagement functionalities and information flows demanded by advanced payment and delivery models53 remains to be seen.
Although technical challenges exist, one can argue that the fact that no single party is responsible for interoperability in the United States is a major obstacle to making it happen. Some experts, as reflected in a JASON report,54 have called for HHS to promulgate a common architecture for interoperability, based on public application program interfaces (APIs) and standards. However, achieving consensus on those standards is difficult when our economy reserves considerable autonomy for private sector organizations and divides public authority between federal and state governments.
Meaningful Use in the Marketplace Context
The Beacon Program
HITECH's ability to use the Beacon program to generate early evidence on its value in more advanced communities was impeded because some grantees were not able to make progress as quickly as anticipated. The Beacon program involved grants to 17 diverse geographically based collaboratives nationwide to improve health care quality and outcomes while lowering overall costs of care. Grant funds were used to support building and strengthening health IT and clinical transformation efforts in communities believed to be more advanced.
NORC's independent evaluation of the Beacon program55 found that, even though they were above average, the communities selected varied substantially in their rates of EHR adoption and ability to exchange information. They also varied in their history. For example, 10 Beacon communities had a base on which to build, whereas 7 of them were developing exchange infrastructure from the ground up. NORC also found that even more advanced communities experienced challenges with interoperability involving early EHRs. These contextual barriers delayed the implementation of clinical transformation efforts, making it difficult to identify short‐term effects of health IT on clinical outcomes.55 Consistent with our framework, grantees whose efforts were aligned with existing payment and service delivery initiatives were more likely to be sustainable after grant funding ended.
Payment and Delivery Reform
As reflected in the Figure 1 framework, the implementation of HITECH has been influenced by a variety of federal and state government policies. For example, the Center for Medicare & Medicaid Innovation (the Innovation Center) of the Centers for Medicare & Medicaid Services (CMS), authorized in the ACA, has been actively engaged in supporting providers, states, and others to develop and test innovative models of health care delivery, models that often rely on having an effective IT system in place. At year‐end 2014, the Innovation Center estimated that these demonstrations would soon serve 2.5 million beneficiaries and include care furnished by more than 60,000 providers.56
Many providers now assume that future requirements will include movement toward more value‐based payment. In early 2015, HHS's secretary announced specific goals for shifting Medicare from volume‐ to value‐based payments, with a target of 50% of traditional Medicare payments in alternative models by 2018.57 The proposed Stage 3 requirements reinforce an interest in aligning MU performance metrics with those required for these value‐based payments.18 The Medicare Access and CHIP Reauthorization Act of 2015 mandates such integration within a new Merit‐Based Incentive Payment System and new parameters for alternative payment models overseen by Medicare and other payers.58
Aligning Goals With Available Functionalities
The movement toward value‐based payment and delivery reform can create additional incentives for providers to adopt and make MU of health IT. However, our interviews with diverse health system leaders and federal officials also highlighted the challenges in using digital tools to support reform.53 As these leaders saw it, delivery reform requires changes in processes of care, with each modification necessitating a specific information flow to support it. Although there are strong links between health IT and payment and delivery reform, interviewees said that health IT should be viewed as much more than an EHR to support the functionalities needed by reform initiatives—and the current EHRs and exchange infrastructure fall short. Whereas in an ideal world, there would be time to create an infrastructure before having to employ it to support delivery reform, those with whom we spoke said that current providers are being asked to do both at once. Interviewees affiliated with experienced systems said it took years to evolve their health IT to where it is now; without this experience as a base for their care delivery reforms, they would be forced to rely on workarounds that would later have to be replaced. That is where most providers are now.
A 2014 survey of accountable care organizations (ACOs) confirmed the need for better alignment; ACOs reported adopting and using health IT with various capabilities but finding significant gaps that limited their ability to use it to monitor cost and quality in a timely way.59 Recognizing these limitations, many key stakeholders now think it could be important to focus health IT on achieving high‐priority objectives, or “use cases,” that can go further in meeting the emerging needs of providers within value‐based payment models. To think through that goal, ONC's Health IT Policy Committee has formed the Advanced Health Models and Meaningful Use Workgroup and made recommendations to ONC about how to structure priorities that take into account both technical issues and strategic policy needs through a process that engages diverse stakeholders.43 Whether an increased focus on specific use cases will generate buy‐in across the provider, vendor, and consumer communities, and ultimately improve interoperability, remains to be seen.
Consumer Engagement
As reflected in Figure 1, consumer engagement is increasingly regarded as important to care transformation. Improved access to personal health information can enable consumers to consult with providers and take actions to improve their health that are consistent with their needs and values. Goals of a patient‐centered health care system include an increase in self‐management and prevention, support for seamless interaction with the health care system, and shared management of health care.60, 61 Analysts believe that in order for such goals to be achieved, there needs to be a shift in consumers’ and providers’ attitudes toward less hierarchical, more collaborative partnerships between patients and providers, enabled by health IT.6, 62
Although some progress was made in the early years of HITECH, the most substantial policies in this area were either adopted in Stage 2 or proposed for Stage 3.10 Stage 1 requirements were limited to capabilities relating to visit summaries and educational resources. In 2013, office‐based physicians made limited use of exchange to promote patient engagement; for example, whereas about two‐thirds of physicians had the ability to provide patients with electronic visit summaries or patient‐specific educational resources, only half had the capability to exchange information electronically with patients.40 Likewise, 4 in 10 physicians could enable patients to view online, download, or transmit their health information; far fewer made routine use of these capabilities.40 Requirements for download functionalities were added to Stage 1 in 2014 concurrently with their introduction in Stage 2.
HITECH also served as an impetus for amending the Clinical Laboratory Improvement Amendments of 1988 (CLIA) to increase patients' direct access to test results from laboratories. In a 2012 survey designed to provide baseline data, ONC found that about 30% of clinical laboratories allowed patients direct access to clinical tests, with 17% permitting electronic access.63 The most common mechanisms of direct access were through a physician's EHR, a laboratory web portal, and/or transmission to a personal health record. A significantly higher percentage of independent laboratories than hospital‐based laboratories allowed such access.
We recently conducted an environmental scan of the status of consumer engagement and HITECH.10 The available evidence suggests that consumers respond positively when given electronic access to personal health information. However, serious technical limitations constrain the value of the information available to them, particularly if they use multiple providers. The strength of provider support for consumer‐oriented functionalities is unclear.
Implications of Geographic Variation
A common theme emerging from both our global assessment and the individual HITECH program evaluations is that state and market variation matters and makes a very important difference in experience with HITECH. EHR adoption varied considerably across markets before HITECH, and this variation continued afterward, even as adoption rates grew.47, 64 Case studies in 8 markets, conducted over a period of time as part of the global assessment, showed that local community and state attributes influenced both initial and subsequent levels of EHR adoption, HIE, and MU achievement.64 Despite selection criteria that excluded markets with the most and least advanced EHR adoption pre‐HITECH, the 8 markets studied still were very diverse in their health IT experience and state health IT policies. The markets also varied in important local characteristics like purchaser and provider market structure, health IT infrastructure, and health reform implementation activity, all of which influenced providers’ incentives to make more advanced use of health IT. The results suggest that tremendous knowledge and skill are needed to tailor HITECH programs to specific state and community contexts, leveraging local assets and adapting to changing conditions over time.
The program evaluations documented similar kinds of state and market variation. For example, the state HIE evaluation47 found that concentration of managed care and hospital competition were important factors in changes in HIE from 2011 to 2013. That evaluation also found cross‐pollination between state HIE programs and payment reform initiatives. The Beacon evaluation found that providers in competitive markets were reluctant to share data, with hospitals viewing their data as a competitive asset.55
Characteristics of state policies and markets tend to persist over time and are not changed readily by national policy. Thus, variation across states, communities, and markets is likely to mean that provider behavior and adoption of MU will continue to evolve unevenly nationwide.
Ultimate Effect on Outcomes Still Unknown
Because HITECH's implementation proceeded more slowly than originally expected, it is too early to assess its ultimate effects on the outcomes it sought, but some early evidence is emerging.
Impact on Individual Care
Most nationwide studies of the role of health IT in improving quality of care, whether in terms of processes of care or outcomes for patients, have focused on health IT use by hospitals and have used data from before the passage of HITECH.65, 66, 67, 68 The evidence of an association between HIE and various measures of care is lacking, mixed, and mostly dated.69 An analysis that is part of the global assessment expanded on this prior evidence by examining data from 2010 to 2013, testing for correlations between the growth in health IT before and after the enactment of HITECH and hospital admissions and readmissions for Medicare beneficiaries with at least 1 of 4 chronic conditions—chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), diabetes, and ischemic heart disease (IHD).70 The analysis found that increases in hospital referral region–level health IT penetration among physicians in ambulatory care settings were correlated with decreases in ambulatory care sensitive condition (ACSC) admissions for these Medicare patients. When the authors examined each of the 4 chronic conditions separately, they found that CHF patients showed the largest magnitude decrease in ACSC admissions.
Impact on Population Health
In addition to its effects on population health through cumulative effects on individuals, HITECH sought to enhance public health by supporting the transfer of digital data on individuals from providers to public health agencies so that the latter could use those data on a population basis to identify outbreaks, assess trends in population health, and promote healthy choices for individuals.71
In Stage 1 of MU, reporting of immunization information, electronic laboratory results, and syndromic surveillance were included among the menu options eligible hospitals and professionals could use to demonstrate MU. In Stage 2, all 3 of these public health measures were moved to the core for eligible hospitals, and eligible professionals are required to report on at least the first two. The third remains a menu option, joined by new options for reporting to cancer and other specialized registries. By February 2014, 40% of eligible providers were submitting immunization data to public health registries; many fewer (6%) were submitting syndromic surveillance data.71 Among eligible hospitals, 54% submitted immunization data to public health agencies, 20% syndromic surveillance data, and 15% laboratory results. Another analysis showed that more Stage 2 hospitals reported on all applicable public health measures without exclusion than did Stage 1 hospitals.72
Although HIEs in some states helped facilitate exchange with public health agencies,47, 71 many state agencies have found it challenging to design interoperable systems that can support and accept the extensive volume of data potentially reported by providers.
Support for Research
The challenges in developing broad‐based HIE contrast with HITECH's original goal of leveraging EHRs and HIE to develop comprehensive population‐based data to support clinical and health services research, though it remains part of the long‐term vision of a nationwide learning health system that is part of the Shared Nationwide Interoperability Roadmap. However, such analysis may be feasible in more limited form sooner in locales served by public exchange models or for populations included in private exchanges that span subgroups of providers who collaborate on a voluntary basis. Some support for building population‐based clinical data is also being provided by a program funded by the ACA—the Patient‐Centered Outcomes Research Institute (PCORI)—which views such capacity as critical to the infrastructure needed to support its mission.73
Although the SHARP program funded by HITECH cannot point to large‐scale change, its evaluation74 found that the HITECH Act had led to some industry collaborations and pilot strategies. The program also served as a potentially good learning source for future public efforts to fund similar programs that seek to develop new products and operationally useful knowledge in furthering HITECH. Such knowledge includes how to address issues of market relevance and different ways to sponsor projects and set expectations.
Conclusions
Despite HITECH's complexity and tight time lines, HHS did implement key features of the HITECH Act, including MU payments and EHR certification requirements, which generally began on schedule, albeit with some state Medicaid delays. For the most part, grant programs also performed as they were charged to do. Although most of the latter's performance required a short‐term infusion of funds, it is likely that some of the capacity funded will be sustained selectively in some form.
Some trade‐offs and policy choices likely allowed successful implementation consistent with HITECH's time frame. In particular, Stage 1 requirements set a relatively low bar in the interest of retaining provider support and encouraging take‐up of EHRs, presumably under the assumption that these factors were critical to making future progress. Vendors seeking to meet Stage 1 certification requirements did not necessarily know what would be expected of them in future stages.
In the rollout of the ONC grant programs, some grants went to new, not necessarily experienced organizations; also, the need to move concurrently on several fronts complicated effective planning. For example, the REC evaluation reported that 34% of REC grants went to new organizations.29 Time lines for workforce programs were so tight that training programs and student recruitment had to take place simultaneously with the development of curriculum and certificate programs, with little time to consult with those firms and other organizations targeted to employ trainees on personnel needs and desired qualifications. Meanwhile, the Beacon program found that its ability to garner support for future investments in health IT was limited because sites were not necessarily as far along as the legislation had envisioned and could not progress rapidly enough to generate compelling evidence on the value of health IT in the planned time frame.
How to generate interoperability in a mixed public/private economy and shared federal/state governing system was an issue at the start of HITECH and arguably remains the central one today.1 In the absence of clear authority and consensus, the initial years of HITECH focused on short‐term priorities and experimentation with diverse models for engaging private providers, states, and health systems. Although mechanisms such as the Direct Project were developed to meet short‐term exchange needs, this emphasis on the immediate future delayed hard decisions about how best to approach standards within a federalized governing model that relies on the private sector to provide the dominant share of health services, decisions now addressed in the Shared Nationwide Interoperability Roadmap.49
Lessons for the Future
Although it will be many years before the final lessons from HITECH become clear, there is much to be learned from the 5 years of experience with HITECH to guide future work on health IT as well as other policy initiatives of broad scope.
First, achieving the expansive goals of HITECH required the simultaneous development of a complex and interdependent infrastructure and a wide range of relationships. HITECH programs supported the digitization and exchange of personal health information that was (1) accessible across a variety of settings, (2) integrated with workflows, and (3) interpretable by providers, patients, and other potential users with a legitimate reason to access the data.
The HITECH experience suggests that the strength of this interdependent system was challenged by the gaps in the available infrastructure to support exchange across EHRs. Although there is good evidence that, under HITECH, EHR adoption grew rapidly, along with specific kinds of one‐on‐one exchange, the lack of more robust mechanisms for capturing data in different ways and easily sharing those data across a variety of relevant providers was a critical weakness. This lack of exchange mechanisms also detracted from the ability of providers, consumers, and public health agencies to make MU of information spread across diverse settings.
Second, while federal legislation can be a powerful stimulus for change, its effectiveness in context depends on its ability to accommodate private health care markets, as well as diversity in state and local policies. HITECH greatly expanded the availability and use of health IT products, but the speed and scope of progress also was limited by contextual factors that will need to be addressed in the future if health IT is to contribute to supporting health delivery reform as proponents of HITECH hoped. In a market economy, government and industry do not necessarily have the same goals for exchange of information. For example, consolidated large hospital systems may agree with the public interest aspects of broad‐based exchange, but their business case for exchange is much stronger with providers internal to the system than with those outside of it. Similarly, some vendors appear to view open exchange as a threat to their business. Yet these large players may be both best positioned and needed to generate support for robust exchange models. Further, in a country as large and diverse as the United States, state and local government policies and conditions vary. For example, privacy laws, particularly those dealing with sensitive data, differ across states, creating state‐specific barriers to interoperability. Some states have been more willing than others to use their own funds to invest in health IT. Finally, health care markets have different characteristics, and prior experience with health IT varies across the nation so that some communities have further to go and more barriers to success than others.
Third, ambitious goals require a long time horizon. Both the realities of elections and terms of office and HITECH's connection to ARRA resulted in legislation with a short‐term focus on results, but the reality is that change on the scale HITECH envisioned takes time.
Given the current health policy agenda, the drive for delivery and payment reform will be an increasingly important lever for change. Thus, the future of health IT support nationally is likely to depend on the ability of the technology to satisfy its users that health IT functionalities address the interests policymakers and other stakeholders have in using technology to promote better care, improved outcomes, and reduced costs. While private sector collaboration is critical, the ability to meet such expectations is likely to be enhanced by ongoing public investments in those areas most essential to assuring that health IT supports broad‐based national goals in health care.
Funding/Support
This article was developed under Contract HHSP23320095642WC/HHSP23337009T from the Office of the National Coordinator for Health Information Technology (ONC) to Mathematica Policy Research. The opinions expressed in this article reflect only those of the authors and not necessarily those of the organizations for whom the authors work or the funding agency.
Conflict of Interest Disclosures: The authors completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. No disclosures were reported.
Acknowledgments: Mynti Hossain and Eric Lammers at Mathematica and Kelly Devers and Fred Blavin at the Urban Institute were key staff on the overall project, which was directed by Catherine McLaughlin. We benefited from the hard work of ONC evaluators at NORC at the University of Chicago and at the American Institutes for Research. At ONC, we benefited from the guidance of numerous project officers over the course of the work, including Dustin Charles, Meghan Gabriel, Michael Furukawa, Matthew Swain, and Yael Harris.
References
- 1. Gold MR, McLaughlin CG, Devers KJ, Berenson RA, Bovbjerg RR. Obtaining providers’ ‘buy‐in’ and establishing effective means of information exchange will be critical to HITECH's success. Health Aff. 2012;31(3):514‐526. [DOI] [PubMed] [Google Scholar]
- 2. Health IT Dashboard IV . Part D. Global evaluation of HITECH implementation. http://dashboard.healthit.gov/evaluations/library.php#HITECH-Global-Evaluations. Accessed October 27, 2015.
- 3. Blumenthal D. Launching HITECH. N Engl J Med. 2010;362(5):382‐385. [DOI] [PubMed] [Google Scholar]
- 4. Buntin M, Jain SH, Blumenthal D. Health information technology: laying the groundwork for national health reform. Health Aff (Millwood). 2010;219(6):1214‐1219. [DOI] [PubMed] [Google Scholar]
- 5. Institute of Medicine . Best care at lower cost: the path to continuously learning health care in America. http://iom.nationalacademies.org/Reports/2012/Best-Care-at-Lower-Cost-The-Path-to-Continuously-Learning-Health-Care-in-America.aspx. September 6, 2012. Accessed October 27, 2015.
- 6. Ricciardi L, Mostashari F, Murphy J, Daniel J, Siminerio E. A national action plan to support consumer engagement via e‐health. Health Aff. 2013;32(2):376‐384. [DOI] [PubMed] [Google Scholar]
- 7. Office of the National Coordinator for Health Information Technology (ONC). Federal Health Information Technology Strategic Plan, 2011‐2015 . https://www.healthit.gov/sites/default/files/utility/final-federal-health-it-strategic-plan-0911.pdf. 2014. Accessed October 27, 2015.
- 8. Mathematica Policy Research, Urban Institute and Insight Policy Research . Global Assessment of the HITECH Program Technical Expert Panel Meeting Summary Notes. Submitted to ONC on October 22, 2010. (Available from authors on request.)
- 9. Rein A; HealthIT.gov. The Beacon Community Program: three pillars of pursuit. Beacon Policy Brief 1.0. http://www.healthit.gov/sites/default/files/pdf/beacon-brief-061912.pdf. June 3, 2012. Accessed June 18, 2016. [Google Scholar]
- 10. Gold M, Hossain M, Mangum A. Consumer engagement in health IT: distinguishing rhetoric from reality. eGEMS. 2015;3(1). http://repository.edm-forum.org/cgi/viewcontent.cgi?article=1190&context=egems. Accessed December 14, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med. 2010;363:501‐504. [DOI] [PubMed] [Google Scholar]
- 12. Centers for Medicare and Medicaid Services (CMS) . Electronic health records (EHR) incentive programs. https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/index.html?redirect=/EHRIncentivePrograms/01_Overview.asp#BOOKMARK2. Updated July 14, 2016. Accessed June 18, 2016.
- 13. ONC . Data analytics update: Health IT Policy Committee meeting. http://healthit.gov/FACAS/sites/faca/files/HITPC_Data_Analytics_Update_2015-04-07_FINAL.pdf. April 7, 2015. Accessed June 18, 2016.
- 14. CMS . September 2015 EHR incentive program summary report. https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Downloads/September2015_SummaryReport.pdf. Accessed October 15, 2015.
- 15. ONC . Non‐federal acute care hospital electronic health record adoption. http://dashboard.healthit.gov/quickstats/pages/FIG-Hospital-EHR-Adoption.php. May 2016. Accessed June 18, 2016.
- 16. ONC . Office‐based health care professional participation in the CMS EHR incentive programs. http://dashboardhealthit.gov/quickstats/pages/FIG-Health-Care-Professionals-EHR-Incentive-Programs.php. December 2014. Accessed June 18, 2016.
- 17. Heisey‐Grove D, Patel V; ONC. Physician motivations for adoption of electronic health records. ONC Data Brief, No. 21. https://www.healthit.gov/sites/default/files/oncdatabrief-physician-ehr-adoption-motivators-2014.pdf. December 2014. Accessed June 18, 2016. [Google Scholar]
- 18. Medicare and Medicaid programs; electronic health record incentive program—stage 3 . Proposed rule. Federal Regist. 2015;80(60). http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Downloads/Stage3_Rule.pdf. Accessed June 18, 2016. [Google Scholar]
- 19. US Department of Health and Human Services . HHS issues rules to advance electronic health records with added simplicity and flexibility. http://www.hhs.gov/about/news/2015/10/06/hhs-issues-rules-advance-electronic-health-records-added-simplicity-and-flexibility.html. October 6, 2015. Accessed October 28, 2015.
- 20. Charles D, Gabriel M, Searcy T; ONC. Adoption of electronic health record systems among U.S. non‐federal acute care hospitals: 2008‐2014. ONC Data Brief, No. 23. https://www.healthit.gov/sites/default/files/data-brief/2014HospitalAdoptionDataBrief.pdf. April 2015. Accessed June 18, 2016. [Google Scholar]
- 21. Heisey‐Grove D, Patel V; ONC. Any, certified, and basic: quantifying physician EHR adoption through 2014. ONC Data Brief, No. 28. https://www.healthit.gov/sites/default/files/briefs/oncdatabrief28_certified_vs_basic.pdf. September 2015. Accessed June 18, 2016. [Google Scholar]
- 22. Mennemeyer ST, Menachemi N, Rahurkar S, Ford EW. Impact of the HITECH Act on physicians’ adoption of electronic health records. J Am Med Inform Assoc. 2016;23(2):375‐379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Walker D, Mora A, Demosthenidy MM, Menachemi N, Diana ML. Meaningful use of EHRs among hospitals ineligible for incentives lags behind that of other hospitals, 2009‐13. Health Aff (Millwood). 2016;35(3):495‐501. [DOI] [PubMed] [Google Scholar]
- 24. Adler‐Milstein J, Jha A. The impact of HITECH on hospital EHR adoption. Paper presented at: AcademyHealth's 2015 Annual Research Meeting; June 16, 2015; Minneapolis, MN. https://academyhealth.confex.com/academyhealth/2015arm/meetingapp.cgi/Paper/3746. Accessed June 18, 2016.
- 25. Dranove D, Garthwaite C, Li B, Ody C. Investment subsidies and the adoption of electronic medical records in hospitals. J Health Econ. 2015;44:309‐319. [DOI] [PubMed] [Google Scholar]
- 26. Adler‐Milstein J, DesRoches CM, Kralovec P, et al. Electronic health record adoption in U.S. hospitals: progress continues but challenges persist. Health Aff (Millwood). 2015;34(12):2174‐2180. [DOI] [PubMed] [Google Scholar]
- 27. Dougherty M, Williams M, Millenson M, Harvell J; US Department of Health and Human Services. EHR payment incentives for providers ineligible for payment incentives and other funding study. http://aspe.hhs.gov/daltcp/reports/2013/EHRPI.pdf. June 2013. Accessed October 28, 2015.
- 28. ONC . Regional Extension Centers (REC) priority primary care providers meaningful use milestone. http://dashboard.healthit.gov/quickstats/pages/FIG-REC-Program-Priority-Primary-Care-Provider-Meaningful-Use-Milestone.php. February 2015. Accessed October 28, 2015.
- 29. American Institutes for Research . Evaluation of the Regional Extension Center program: final report. https://www.healthit.gov/sites/default/files/Evaluation_of_the_Regional_Extension_Center_Program_Final_Report_4_4_16.pdf. April 2016. Accessed May 5, 2016.
- 30. Government Accountability Office . Electronic health records: number and characteristics of providers awarded Medicare incentive payments for 2011‐2012. http://www.gao.gov/assets/660/658534.pdf. October 2013. Accessed October 28, 2015.
- 31. Gold M, Hossain M, Charles DR, Furukawa MF. Evolving vendor market for HITECH‐certified ambulatory EHR products. Am J Manag Care. 2013;19(10 Spec No):SP353‐361. [PubMed] [Google Scholar]
- 32. US Department of Justice . Herfindahl‐Hirschman Index. https://www.justice.gov/atr/herfindahl-hirschman-index. Updated July 29, 2015. Accessed June 18, 2016.
- 33. Blavin F, Ramos C, Shah A, Devers K; US Department of Health and Human Services. Final report: lessons from the literature on electronic health record implementation. http://www.healthit.gov/sites/default/files/hit_lessons_learned_lit_review_final_08-01-2013.pdf. August 2013. Accessed October 28, 2015.
- 34. American Medical Association . AMA provides blueprint to improve the meaningful use program. http://www.ama-assn.org/ama/pub/news/news/2014/2014-10-14-ama-blueprint-improve-Meaningful-use.page. October 14, 2014. Accessed June 18, 2016.
- 35. Gabriel MH, Jones EB, Samy L, King J. Progress and challenges: implementation and use of health information technology among critical‐access hospitals. Health Aff. 2014;33(7):1262‐1270. [DOI] [PubMed] [Google Scholar]
- 36. NORC at the University of Chicago . Final report: evaluation of the Information Technology Professionals in Health Care (“Workforce”) Program—summative report. http://www.healthit.gov/sites/default/files/workforceevaluationsummativereport.pdf. March 2014. Accessed October 28, 2015.
- 37. Mathematica Policy Research . Monitoring national implementation of HITECH: status and key activity quarterly summary. https://www.healthit.gov/sites/default/files/qmr_oct-dec2011.pdf. October‐December 2011. Accessed October 28, 2015.
- 38. Swain M, Charles D, Patel V, Searcy T; ONC. Health information exchange among U.S. non‐federal acute care hospitals: 2008‐2014. ONC Data Brief, No. 24. https://www.healthit.gov/sites/default/files/data-brief/ONC_DataBrief24_HIE_Final.pdf. April 2015. Accessed June 19, 2016. [Google Scholar]
- 39. Gold M, Hossain M; Mathematica Policy Research. How early adopting hospital systems view the business case for health information exchange. Working Paper #34. http://www.mathematica-mpr.com/our-publications-and-findings/publications/how-early-adopting-hospital-systems-view-the-business-case-for-health-information-exchange. October 2014. Accessed October 28, 2015.
- 40. Furukawa MF, King J, Patel V, Hsaio C, Adler‐Milstein J, Jha AK. Despite substantial progress in EHR adoption, health information exchange and patient engagement remain low in office settings. Health Aff. 2014;33(9):1672‐1679. [DOI] [PubMed] [Google Scholar]
- 41. Heisey‐Grove D, Patel V, Searcy T; ONC. Physician electronic exchange of patient health information, 2014. ONC Data Brief, No. 31. http://dashboard.healthit.gov/evaluations/data-briefs/physician-electronic-exchange-patient-health-information.php. October 2015. Accessed October 28, 2015. [Google Scholar]
- 42. Swain M, Patel V; ONC. Health information exchange among clinical laboratories. ONC Data Brief, No. 14. https://www.healthit.gov/sites/default/files/onc-data-brief-14-testresultexchange_databrief.pdf. February 2014. Accessed October 28, 2015.
- 43. HealthIT.gov . Direct Project. http://www.healthit.gov/policy-researchers-implementers/direct-project. Updated July 15, 2014. Accessed June 19, 2016.
- 44. Mathematica Policy Research . Monitoring national implementation of HITECH: status and key activity quarterly summary. https://www.healthit.gov/sites/default/files/mni_hitech_january-march_2011.pdf. January‐March 2011. Accessed October 28, 2015.
- 45. Terry K. ONC releases guidelines for direct clinical messaging. InformationWeek. July 24, 2012. http://www.informationweek.com/regulations/onc-releases-guidelines-for-direct-clinical-messaging/d/d-id/1105476. Accessed June 19, 2016. [Google Scholar]
- 46. Sequoia Project. eHealth Exchange participants . http://healthewayinc.org/ehealth-exchange/participants/. Accessed October 28, 2015.
- 47. NORC at the University of Chicago . Final report: evaluation of the State HIE Cooperative Agreement Program. https://www.healthit.gov/sites/default/files/reports/finalsummativereportmarch_2016.pdf. March 2016. Accessed March 20, 2016.
- 48. ONC. Federal Health IT Strategic Plan, 2015‐2020 . https://www.healthit.gov/sites/default/files/9-5-federalhealthitstratplanfinal_0.pdf. n.d. Accessed October 28, 2015.
- 49. ONC . Connecting health and care for the nation: a Shared Nationwide Interoperability Roadmap. https://www.healthit.gov/sites/default/files/hie-interoperability/nationwide-interoperability-roadmap-final-version-1.0.pdf. n.d. Accessed October 28, 2015.
- 50. Health IT Policy Committee . Letter on Shared Nationwide Interoperability Roadmap. http://www.healthit.gov/sites/faca/files/hitpc_roadmap_transmittal_letter_2015.pdf. April 29, 2015. Accessed October 28, 2015.
- 51. ONC . Report to Congress: report on health information blocking. https://www.healthit.gov/sites/default/files/reports/info_blocking_040915.pdf. April 2015. Accessed October 28, 2015.
- 52. Health IT Policy Committee . Data update. http://www.healthit.gov/FACAS/sites/faca/files/HITPC_Data_Update_Presentation_Final_2015-09-09.pdf. September 9, 2015. Accessed October 28, 2015.
- 53. Gold M. Employing health information technology in the real world to transform delivery. Am J Manag Care. 2013;19(10 Spec No):SP377‐381. [PubMed] [Google Scholar]
- 54. JASON; Agency for Healthcare Research and Quality . A robust health data infrastructure. http://healthit.gov/sites/default/files/ptp13-700hhs_white.pdf. April 2014. Accessed October 28, 2015.
- 55. NORC at the University of Chicago . Final report: evaluation of the Beacon Community Cooperative Agreement Program. https://www.healthit.gov/sites/default/files/norc_beacon_evaluation_final_report_final.pdf. November 2015. Accessed January 2, 2015
- 56. CMS . The Center for Medicare and Medicaid Innovation: Report to Congress. https://innovation.cms.gov/Files/reports/RTC-12-2014.pdf. December 2014. Accessed June 22, 2016.
- 57. Burwell SM. Setting value‐based payment goals—HHS efforts to improve U.S. Health care. N Engl J Med. 2015;372(10):897–899. [DOI] [PubMed] [Google Scholar]
- 58. Medicare Access and CHIP Reauthorization Act of 2015, Pub L No . 114‐10 (2015). https://www.congress.gov/bill/114th-congress/house-bill/2. Accessed June 19, 2016.
- 59. Adler‐Milstein J, Jha A. The use of health IT to support accountable care organizations. Paper presented at: AcademyHealth's 2015 Annual Research Meeting; June 14, 2015; Minneapolis, MN. https://academyhealth.confex.com/academyhealth/2015arm/meetingapp.cgi/Paper/4308. Accessed June 18, 2016.
- 60. HealthIT.gov . Consumer Workgroup. https://www.healthit.gov/FACAS/health-it-policy-committee/hitpc-workgroups/consumer-workgroup. Updated March 10, 2015. Accessed October 29, 2015.
- 61. Charles D, Gabriel M, Henry J; ONC. Electronic capabilities for patient engagement among U.S. non‐federal acute care hospitals: 2012‐2014. ONC Data Brief, No. 29. http://dashboard.healthit.gov/evaluations/data-briefs/hospitals-patient-engagement-electronic-capabilities.php. October 2015. Accessed June 19, 2016. [Google Scholar]
- 62. Daniel J, Deering MJ, Murray M; ONC. Issue brief: using health IT to put the person at the center of their health and care by 2020. https://www.healthit.gov/sites/default/files/person_at_thecenterissuebrief.pdf. January 10, 2014. Accessed June 19, 2016.
- 63. Swain M, Patel V; ONC. Patient access to test results among clinical laboratories. ONC Data Brief, No. 13. https://www.healthit.gov/sites/default/files/onc-data-brief-13-labsurveydatabrief.pdf. February 2014. Accessed June 19, 2016. [Google Scholar]
- 64. Devers KJ, Blavin F, Cafarella‐Lallemand N, Shah A, Napoles A. State and local market barriers and spur to meaningful use of electronic health records: insights from local communities in Appendix I of The Global Assessment of HITECH—Final Report by McLaughlin C, Gold M, Lammers E, Hossain M, Barna M, Devers K and others. Submitted to the Office of the National Coordinator for Health Information Technology, October 30, 2015. In press.
- 65. Agha L. The effects of health information technology on the costs and quality of medical care. J Health Econ. 2014;34:19‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. McCullough JS, Casey M, Moscovice I, Prasad S. The effect of health information technology on quality in U.S. hospitals. Health Aff. 2010;29(4):647‐654. [DOI] [PubMed] [Google Scholar]
- 67. McCullough JS, Parente S, Town R. Health Information Technology and Patient Outcomes: The Role of Organizational and Informational Complementarities. Cambridge, MA: National Bureau of Economic Research; 2013. [Google Scholar]
- 68. Miller AR, Tucker CE. Can health care information technology save babies? J Polit Econ. 2011;119(2):289‐324. [DOI] [PubMed] [Google Scholar]
- 69. Rahurkar S, Vest JR, Menachemi N. Despite the spread of health information exchange, there is little evidence of its impact on cost, use, and quality of care. Health Aff. 2015;34(3):477‐483. [DOI] [PubMed] [Google Scholar]
- 70. Lammers E, McLaughlin C, Barna M. Physician EHR adoption and potentially preventable hospital admissions among Medicare beneficiaries: panel data evidence from 2010‐2013. Paper presented at the 2016 AcademyHealth Annual Research Meeting; June 28, 2016; Boston, MA. [DOI] [PMC free article] [PubMed]
- 71. Wu L; ONC. Issue brief: health IT for public health reporting and information systems. https://www.healthit.gov/sites/default/files/phissuebrief04-24-14.pdf. April 29, 2014. Accessed June 19, 2016.
- 72. Heisey‐Grove D, Chaput D, Daniel J; ONC. Hospital reporting on meaningful use public health measures in 2014. ONC Data Brief, No. 22. https://www.healthit.gov/sites/default/files/databrief22_hospitalreporting.pdf. March 2015. Accessed June 19, 2016. [Google Scholar]
- 73. Patient‐Centered Outcomes Research Institute . PCORI funding announcement: improving infrastructure for conducting patient‐centered outcomes research. The National Patient‐Centered Clinical Research Network (PCORnet): clinical data research networks (CDRNs)—Phase II. http://www.pcori.org/sites/default/files/PCORI-PFA-CDRN.pdf. December 22, 2014. Accessed June 19, 2016.
- 74. NORC at the University of Chicago . Final report: assessing the SHARP experience. http://www.healthit.gov/sites/default/files/sharp_final_report.pdf. July 2014. Accessed June 19, 2016.


