Abstract
Background
Sleep patterns may change over a person’s lifetime; however, the quantity and quality of sleep always depend on individual factors such as age, sex, and psychological and environmental factors. In children, sleep is as important as development. Quantitative sleep problems related to sleep onset and qualitative sleep disorders such as frequent awakenings may lead to insufficient sleep.
Objectives
This study aimed to assess the prevalence of sleep disorders among children 4 - 6 years old attending the health centers of Shahid Beheshti University of Medical Sciences, Tehran, Iran, in 2013.
Patients and Methods
This was a cross-sectional study on 400 children selected using a multistage sampling method. Data were collected by interviews. The questionnaire included two sections: a demographic section with questions about the demographic characteristics of the children and parents and a children’s sleep habit questionnaire (CSHQ). Data were analyzed by SPSS 16 and different statistical tests were used (P < 0.05).
Results
The mean age of the children was 64.27 ± 9.3 months. The prevalence of sleep disorders was 36.25%. Sleep disorders were significantly associated with age, height, body mass index, residence of children, father’s occupation, mother’s diseases, father’s drug abuse, and parents’ marital status (P < 0.05).
Conclusions
Sleep disorders in children threaten growth and development, and are dangerous for their health. Sleep disorders should be considered in the differential diagnosis of children’s learning and behavioral problems.
Keywords: Sleep Disorders, Prevalence, Child
1. Background
Sleep disorders are very common in children, but due to their varying presentations, their incidence as behavioral, learning, and mental-behavioral problems cannot usually be diagnosed. Sleep disorders are the most common behavioral complaints in children. Sleep patterns change throughout life, although the quality and quantity of sleep always depend on individual factors such as age, sex, and psychological and environmental factors (1). In children, sleep is as important as growth and development (2). Learning good sleep habits is also important. Quantitative sleep problems such as disorders in sleep onset and qualitative sleep disorders such as frequent awakenings may lead to insufficient sleep (3). Inadequate sleep symptoms and complications in children are different from those of adults and may reveal themselves as changes in mood, activities, and excessively shortened attention span and neurological cognitive disorders such as inattention. Sleep disorders in children not only affect their health and hygiene, but can also be an important factor for causing stress, pressure, and tension in the family, and even cognitive disorders in adolescence (4). Information on sleep disorders in children is an important factor influencing their growth and development (5).
Sleep is an organized behavior that is repeated every day as a vital necessity based on biological rhythm, but its exact mechanism is not known. Chemical, vascular, and hormonal theories have been suggested in regards to sleep (2). People need different amounts of sleep depending on a variety of factors such as age, genetics, and their physical and mental states (6). At 6 weeks of age, children need about 14 - 16 hours of sleep; by one year of age, they require 12 - 24 hours; during the second year of age, the number of hours needed is reduced somewhat, reaching almost 12 hours a day; and the sleep characteristics of three-year-old children are similar to those of adults (7).
There are different views on the onset of sleep disorders in childhood according to study groups and health care providers. The prevalence of sleep disorders has been reported as 10% - 30% in primary care and up to 37% in sleep centers (8). Establishing a healthy sleep pattern in children requires parents’ information and cooperation. Therefore, at each visit for growth monitoring, the parents should be questioned regarding their child’s sleep patterns, and they must pay attention to the development of a proper sleep pattern just as they support good nutrition and oral hygiene (9). The prevalence of sleep disorders in children encompasses a wide range and has been reported from 15% to 86% (10). Goldman reported the prevalence of sleep disorders as 33% (11). In a study by Rzepecka, the prevalence of sleep disorders was reported as 42% (12). In Iran, the prevalence of sleep disorders was reported as 41.6% (13), 30.9% (14), and 50.4% (15). Ebarhim et al. found that the most common sleep problem in children was daytime sleepiness (16).
Some factors that affect sleep include socioeconomic conditions, drug side effects, psychological factors such as parental distress, environmental factors such as sleep environment, sleep patterns representing social-cultural differences that govern the communities, and children’s interactions with their parents (17). The high prevalence of sleep disorders in children indicates the considerable importance of addressing them in preschool-aged children; unfortunately, they are not addressed sufficiently in children care. The most serious complication related to sleep disorders in children is cognitive problems, which place children at risk for educational failure, family problems, and social psychological problems (18).
2. Objectives
The purpose of this study was to assess the prevalence of sleep disorders among 4- to 6-year-old children attending the health centers of Shahid Beheshti University of Medical Sciences, Tehran, Iran, in 2013.
3. Patients and Methods
This cross-sectional study was conducted on 400 children from December 2012 to May 2013. Participants included children who attended health centers for growth monitoring in Tehran, Iran. Participants were selected through multistage sampling. The area of health care centers related to Shahid Beheshti University of Medical Sciences in Tehran was divided into four geographical classes: North, South, West, and East. Two centers were chosen from each class, and 400 children from these centers were randomly selected. After explaining the study objectives, if their children met the study inclusion criteria, informed consents were obtained from the children’s mothers.
The questionnaires were filled out through interviews with each child’s mother. The sample size was calculated according to this formula: P* (1 - P) * (Z (alpha/2) + Z (beta)) ^ 2/epsilon ^ 2 = 384 (19).
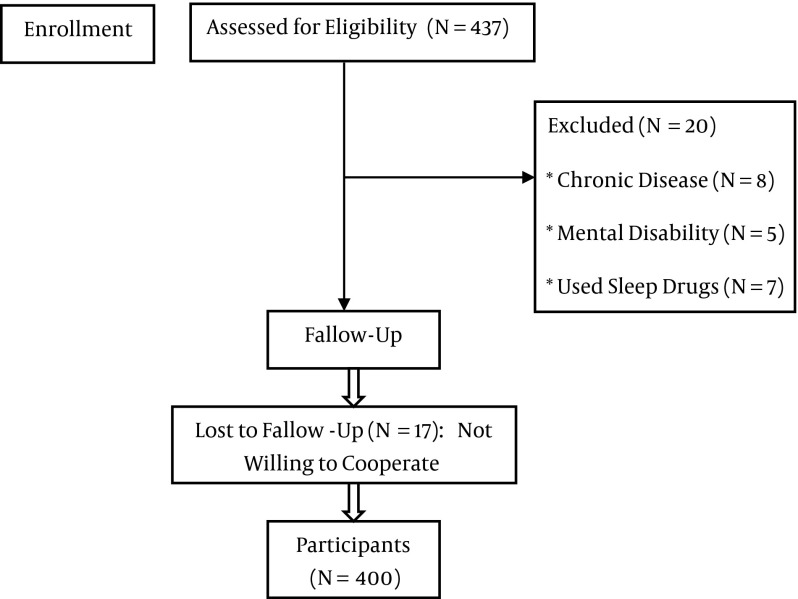
437 samples were eligible in study. Children with chronic disease (N = 8), mental disability (N = 5), or who used sleep drugs (N = 7) were excluded. In total, 400 children participated (Figure 1). This study was approved by the ethics committee of Shahid Beheshti University of Medical Sciences (No: 91-01-43-61331-1, Dated: 2012/03/18). After obtaining permission from the authorities of the Shahid Beheshti University of Medical Sciences, the authors approached the parents of qualified children. The objectives of the study were explained, written informed consent was obtained, and the parents participated in the study in a private setting. The parents were assured that all of their information would be kept confidential and that they did not need to mention their names on the questionnaires. All ethical issues-informed consent, conflicts of interest, plagiarism, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc. have been considered carefully by the authors. The respondents were anonymous and participated willingly and voluntarily in this study. The inclusion criteria were: being Iranian; not having chronic diseases or mental, physical, or mental disability; not using sleep drugs; and lack of known parental mental and physical diseases. The data collection tools were the children’s sleep habits questionnaire (CSHQ) containing 50 items, and the questionnaire for the demographics of the women and their husb parents and children ands containing 37 items. The CSHQ (standard) is designed in Likert style, with each item rated on a three-point scale: 1 = rarely (0 - 1 time per week); 2 = sometimes (2 - 4 times per week); and 3 = usually (5 - 7 times per week). A total score of greater than 41 is the cutoff for diagnosing sleep disturbances in children. A high score indicates more frequent sleep disturbances. In the present study, sleep disturbances included bedtime resistance, sleep onset delay, sleep duration, sleep anxiety, awakening during the night, parasomnias, sleep-related breathing disorders, and daytime sleepiness. In Iran, the CSHQ was used in the study by Shoghy et al.; they reported on its reliability using the test-retest method (r = 0.97) (20). Wang et al. assessed the CSHQ using the content validity method, and Cronbach’s alpha coefficient of the CSHQ was 0.80 (21). Cronbach’s alpha coefficient of the CSHQ was found in a previous study to also be 0.80 (12).
Figure 1. Flow Study of Parents Participants.
In this study, the CSHQ was validated through content validity. For internal consistency of the CSHQ, Cronbach’s alpha coefficient for the total scale was 0.82 and its reliability was measured by test-retest with a 10-day interval (r = 0.95). We faced to missing value < 10%. Missing data were replaced with the sample mean for the column.
Data were analyzed with the statistical package software for social science, version 16 (SPSS, Inc., Chicago, IL, USA). The normality of the data was evaluated by the one-sample Kolmogorov-Smirnov test (P > 0.05) and the homogeneity of variances was evaluated by the Leven test (P > 0.05). Frequency, percentage, and mean standard deviation were used to describe the characteristics of the children and the prevalence of sleep disorders. For the relationship between the quantitative variables of sleep disorders-age and body mass index-the Pearson test was used. The t test was used for the relationship between the binary variables of sleep disorders. (After checking ANOVA assumptions), the relationship among the third and fourth groups sleep disorders and father’s job, that over two groups was analyzed by ANOVA. ) .Logistic regression was also used for the strength of the relationship. For all of the statistical tests, a P value of less than 0.05 was considered significant.
4. Results
The demographic characteristics of the children are shown in Table 1. The mean age of the children was 64.27 ± 9.3 months. Children had favorable weight (98.25%), head circumference (99.75%), and developmental condition (100%). The mothers’ mean age was 31.06 ± 5.14 years and the fathers’ mean age was 36.55 ± 1.85 years. Most mothers were housewives (87.25%), many were university educated (40.5%), did not smoke (98.5%), and did not use opium (100%). Some had physical diseases (12.5%) and used drugs (7.5%). Some fathers had physical diseases (7.75%) and smoked (18.5%). The mean bedtime for children was 9:51 PM (SD = 3 hours and 58 minutes); the mean duration of sleep was 9 hours and 8 minutes (SD = 3hours and 9 minutes). The prevalence of total sleep disorders was 36.25%. Table 2 provides these results.
Table 1. Distributions of Children by Their Characteristics.
| Independent variables | No. (%) |
|---|---|
| Gender | |
| Girl | 196 (49) |
| Boy | 204 (51) |
| Sickness of child is sick | |
| Yes | 25 (6.25) |
| No | 375 (93.75) |
| Using drugs | |
| Yes | 6 (1.5) |
| No | 394 (98.5) |
| Number of children in family | |
| 1 | 164 (41) |
| 2 | 178 (44.5) |
| 3+ | 58 (14.5) |
| BirthRank of child | |
| 1 | 227 (56.75) |
| 2 | 131 (32.75) |
| 3+ | 42 (10.5) |
| Number of rooms in home | |
| 1 | 394 (98.5) |
| 2 | 6 (1.5) |
| Has separate bedroom | |
| Yes | 210 (52.5) |
| No | 190 (47.5) |
| Biological parents | |
| Yes | 395 (98.75) |
| No | 5 (1.25) |
| Income of family | |
| Low | 99 (24.75) |
| Moderate | 162 (40.5) |
| High | 139 (34.75) |
Table 2. The prevalence of specific sleep disorders.
| Sleep Disorders | Usually, No. (%) | Sometimes, No. (%) | Rarely, No. (%) |
|---|---|---|---|
| Bedtime resistance and anxiety | |||
| Going to bed at different times | 140 (34.3) | 107 (26.2) | 153 (37.3) |
| Falling asleep in another’s bed | 129 (31.6) | 47 (11.5) | 224 (54.9) |
| Needing parent in room to sleep | 122 (29.9) | 59 (14.5) | 219 (53.6) |
| Struggling at bedtime | 57 (14) | 72 (17.6) | 271 (66.4) |
| Afraid to sleep in the dark | 147 (36) | 61 (15) | 192 (47.1) |
| Afraid of sleeping alone | 150 (36.8) | 50 (12.3) | 200 (49) |
| Trouble sleeping away | 34 (8.3) | 38 (9.3) | 328 (80.3) |
| Sleep onset delay | |||
| Difficulty falling asleep in 20 minutes | 292 (71.6) | 65 (15.9) | 43 (10.6) |
| Night awakening and sleep duration | |||
| Moving to another’s bed in night | 60 (14.7) | 62 (15.2) | 278 (68.2) |
| Awakening once during night | 93 (22.8) | 161 (39.5) | 146 (35.8) |
| Awakening more than once | 109 (26.7) | 64 (15.7) | 227 (55.6) |
| Sleeping too little | 25 (6.1) | 54 (13.2) | 321 (78.6) |
| Not sleeping the same amount each night | 285 (69.6) | 48 (11.8) | 67 (16.4) |
| Sleep-related breathing disorders | |||
| Snoring loudly | 12 (2.9) | 19 (4.9) | 369 (90.4) |
| Holding breath or stopping breathing | 4 (1) | 12 (2.9) | 384 (94.1) |
| Snorting and gasping | 16 (3.9) | 16 (3.9) | 368 (90.2) |
| Parasomnias | |||
| Wetting the bed at night | 24 (5.9) | 28 (6.9) | 384 (85.3) |
| Talking during sleep | 34 (8.3) | 57 (14) | 309 (75.7) |
| Restless, moving a lot | 68 (16.7) | 56 (13.7) | 276 (67.6) |
| Sleepwalking | 15 (3.7) | 13 (3.2) | 372 (91.2) |
| Grinding teeth during sleep | 25 (6.1) | 33 (8.1) | 342 (82.1) |
| Awakening screaming, sweating | 6 (1.5) | 35 (8.6) | 359 (88) |
| Alarmed by nightmare | 14 (3.4) | 51 (12.5) | 335 (82.1) |
| Daytime sleepiness | |||
| Awakening by others in the morning | 100 (24.5) | 112 (27.5) | 188 (48) |
| Waking up in a bad mood | 51 (12.5) | 84 (20.6) | 265 (65.9) |
| Hard time getting out of bed | 31 (7.6) | 52 (12.7) | 317 (77.7) |
| Takes a long time to be alert | 21 (5.1) | 48 (11.8) | 331 (81.1) |
| Seems tired during the day | 37 (9.1) | 78 (19.1) | 285 (69.9) |
| Asleep while watching TV | 48 (11.8) | 78 (19.1) | 274 (68.5) |
| Asleep while riding in car | 122 (29.9) | 52 (12.7) | 226 (57.4) |
Sleep disorders were significantly associated with children’s age, height, and body mass index (BMI), mother’s diseases, father’s drug abuse, and the level of satisfaction of the parents’ sexual relationship (P < 0.05) (see Table 3). ANOVA showed that sleep disorders were significantly associated with the father’s job (P = 0.016). The Tukey’s test (post-test) showed that the mean scores for sleep disorders in children whose fathers worked were higher than the mean scores in children whose fathers had private jobs (P = 0.10). Sleep disorders were significantly associated with the children’s residence (P = 0.011). The Tukey’s test (post-test) showed that the mean scores for sleep disorders in children who lived in tenant housing were higher than the mean scores in children who lived in private houses (P = 0.042). Logistic regression was used for the relationship between sleep disorders and the variables (see Table 4).
Table 3. Correlations of Sleep Disorders with Variables.
| Independent Variables | No. (%) | Mean ± SD | Sleep Disorders | |
|---|---|---|---|---|
| Test | P Value | |||
| Age of child, mo | ||||
| 48 | 54 (13.5) | |||
| 49 - 60 | 87 (21.75) | 64.2 ± 9.48 | Pearson | < 0.05 |
| 61+ | 259 (64.75) | |||
| Height of child | ||||
| Favorite Good | 395 (98.75) | T Test | < 0.01 | |
| Un Favorite Bad | 5 (1.25) | |||
| BMI of child | ||||
| < 18.5 | 45 (11.25) | |||
| 18.6 - 24.9 | 277 (69.25) | 23.78 ± 4.37 | Pearson | < 0.01 |
| > 25 | 78 (19.5) | |||
| Mother is sick | ||||
| Yes | 50 (12.5) | T Test | < 0.01 | |
| No | 350 (87.5) | |||
| Father is addicted | ||||
| Yes | 13 (3.25) | T Test | <0.01 | |
| No | 387 (96.75) | |||
| Satisfactory parental sexual relationship | ||||
| Yes | 373 (93.25) | |||
| No | 27 (6.75) | T Test | < 0.01 | |
| Father’s job | ||||
| Unemployed | 11 (2.75) | 35.00 (12.42) | ||
| Worker | 170 (42.5) | 40.20 (16.16) | ANOVA | < 0.05 |
| Employee | 119 (29.75) | 37.42 (12.96) | ||
| Private | 100 (25) | 34.68 (11.19) | ||
| Residence | ||||
| Tenant | 209 (52.25) | 39.82 (14.81) | ||
| Personal accommodation | 159 (39.75) | 36.04 (13.22) | ANOVA | < 0.05 |
| Living with relatives | 32 (8) | 33.96 (12.57) | ||
Table 4. Logistic Regression of Sleep Disorders with Variables.
| Independent Variables | Odd Ratio OR | P Value | 95% | |
|---|---|---|---|---|
| Lower Limit | Upper Limit | |||
| Father’s job | 1.261 | 0.0327 | 0.633 | 1.908 |
| Mother is sick | 1.593 | 0.0405 | 0.433 | 4.763 |
| Father is addicted | 8.809 | 0.032 | 3.567 | 11.356 |
| BMI of child | 2.865 | 0.0232 | 1.768 | 4.856 |
5. Discussion
The authors found the prevalence of sleep disorders in the studied population to be 36.25%. Wang et al. reported the prevalence of sleep disorders in children to be 69.3% (21), which is higher than that of our study. This can be attributed to cultural context. Ardani et al. found the prevalence of sleep disorders in children to be 39.8% (22). Mohammadi et al. reported the prevalence of sleep disorders as 50.5% (18). Day et al. found the prevalence of sleep disorders in children to be 43.5% (23). Jan et al. reported the prevalence of sleep disorders to be 25 - 40% (24). These differences in the prevalence of sleep disorders can be attributed to differences in the study populations and the use of different tools for data gathering (13).
Sleep disorders can cause fatigue, lethargy, depression, negative moods, and dysfunction (25). Sleeping habits and the quality and quantity of sleep affect childhood health. Learning bad habits can affect adulthood health and endangers individual and public health (26). Sleep problems can cause anxiety, reduced adaptation rate, and low self-esteem in children (27). The persistence of these problems is associated with alcohol and drug abuse in adulthood (28). We found a significant association between sleep disorders and children’s age. Shoghy et al. showed a positive significant association between sleep disorders and children’s age (20). In contrast, Liu et al. found a significant association between bedtime resistance and children’s age (29), but Gharamaleki et al. did not find a significant association between sleep quality and children’s age (30).
In our study, children’s height and BMI had a significant association with sleep disorders. Arman et al. found a significant association between sleep quality and BMI (31). Bagley et al. also showed a significant association between sleep quality and BMI (32). Late-night feeding may lead to sleep disorders because increased fluid intake leads to increased urination, which can lead to more severe insomnia. BMI can be an indication of a person’s lifestyle. There is a positive relationship between a regular lifestyle and good sleep. A proper and orderly lifestyle can lead to improved sleep (33). Some childhood diseases such as diabetes whose symptoms develop at night may lead to sleep disorders in children. Inadequate sleep can compromise the immune system’s function, hormonal function, and cause other health-related consequences (34). Other studies have also acknowledged the impact of chronic illness on children’s sleep (24, 35). Furthermore, inadequate sleep is a risk factor for obesity in children. Although the mechanism is not clear, one hypothesis is that frequent insufficient sleep may change the hormones leptin and ghrelin periodically, which would result in increased hunger and desire to eat food (36). Another study claimed there was a possibility that shortening sleep duration put children at risk for diabetes (37).
The present study did not find a significant association between sleep disorders and the father’s job and level of education. However, Shoghy et al. found a significant association between sleep disorders and the father’s level of education (20), and Sadeh et al. showed that when a father’s education level increased, the children’s sleep problems decreased (38), although the reason is not clear. Scientists believe that perhaps this is a result of discipline in such families or better knowledge of educated parents about sleep problems and child-rearing (39). Furthermore, it seems that increased awareness of educated parents and intimate interactions with their children that lead to a discharge of emotions and lower psychological pressure will cause improved quality of sleep. We did not find a significant association between sleep disorders and having a separate room, but Mohammadi et al. reported a significant association between sleep disorders and having a separate room (18). In contrast, Panaghi et al. also did not find this relationship (13). Wang et al. assessed the socioeconomic status of children. They showed that 63.8% of children slept in separate rooms, 10.1% shared a room, and 26.2% shared a bed with their parents (21).
For children, socioeconomic status is associated with sleep and insomnia duration (40). Living conditions in less developed urban areas, with poor hygiene, poverty, and low income, can lead to sleep disorders (41). Unfortunately, there is no health guarantee factor for millions of children because they suffer from a lack of health promotion services. Children’s health patterns have been developed based on medical advances and social trends. The Healthy People 2020 project has been developed on this basis (11). Changes in modern society including the progress of medical awareness and technology, increased urbanization, economic changes, and other changes that will lead to lifestyle changes are factors affecting children’s health. Recent studies have a greater focus on children because they have the highest level of risk (41).
We found a significant association between sleep disorders and the mother’s sickness. Dependency on their mother develops stress in children. We found a significant association between sleep disorders and the father’s drug abuse. Another study found the same result (42). The amount of alcohol and cigarette use and other risky behaviors were greater in parents who had children with sleep disorders. This can be attributed to parents’ stress, since one way to release it is to turn to cigarettes, alcohol, and drugs, as is discussed in other research (43). Children want to receive more parental attention and love. Lack of attention or neglectfulness by their parents can lead to the development of anxiety, tension, and fear in children (23).
We observed a significant association between sleep disorders and marital satisfaction. In a study by Shoghi et al., there was a significant relationship between the number of disputes between parents and sleep disorders in children (20). Sadeh et al. showed that an increase in arguments between parents led to increased nocturnal awakenings in children (38). Researchers have reported that poor quality of sleep can be due to decreased marital satisfaction (44). Marital distress and family conflict that is caused by poor interactions between the parents can be a predisposing factor for psychological problems that ultimately show themselves as sleep disorders. Marital disputes can have harmful effects on the safety of the home environment and can lead to children’s restlessness, bad temperament, not eating, seclusion, and not participating in social games (45). Marital disputes and conflicts can cause reduced child safety in the home environment, failure or instability in parent-child communications, unsustainable practices, reduced parental monitoring, and aggression in children that requires intervention. It can even influence the addition of other environmental stress factors, such as friendship with peers with high-risk behaviors (46).
Quality of sleep is one aspect of living well and has a strong relationship with quality of life, satisfaction with life, stress hormones, and cortisol levels (47). Quality of sleep in children is an important predicting factor for the mother’s quality of sleep, which can affect her daily activities (6). Children’s sleep habits are influenced by the habits of their parents. Children’s staying awake is associated with parents’ waking hours (21). A study showed that there was a significant relationship between children’s interactions and parents’ moods. Sleep-related behaviors are not only shaped by biological and developmental factors but also by socio-cultural contexts including social values, social norms, and parents’ behaviors (48). Cultural differences may affect the place, time, and quality of children’s sleep (49). In the USA, pediatricians recommend that children sleep alone in their own bed at bedtime, which is a reflection of social factors on individual self-efficacy (50). Most often, children follow their parents’ behavioral patterns like staying awake and watching TV in bed (51). An increase in irregular sleep habits of parents and delays in their sleep will lead to an increase of bad sleep habits in their children. Therefore, correcting family behavioral patterns can lead to improved sleep disorders in children. Behaviors such as self-dominance, self-control, stability, and parents’ taking responsibility are effective for correcting children’s behaviors, and usually parents’ positive emotional responses would result in children’s peace-of-mind (52). A stressful family environment will place children and parents at risk for mental disorders. Parents with psychiatric disorders spend less time with their children, affect them less, and monitor them very little. They often use more severe punishments and less encouragement and are not flexible in their opinions (53). In short, a lot of emotional frustrations in children are associated with their sleep patterns (31).
5.1. Conclusion
Sleep is a window into the social, familial, and emotional performance of every person. Psychological and neurological problems can affect sleep quality. Sleep should be considered as an important factor affecting children’s health. Training sessions on the importance of getting enough and high quality sleep should be held in health centers and proper strategies for sleep should be provided to stressful families with low literacy. Parent training programs must prepare to improve relationships in families. Sleep disorders should be considered in the differential diagnosis of children’s learning and behavioral problems.
5.2. Limitations
One limitation of this study was that the information about sleep disorders was obtained from the children’s mothers and they may not be aware of sleep disorders in their children. Some mothers refused to talk about diseases they, their spouse, or their children had. Some would not discuss any instances of drug abuse by themselves or their spouse. One of strong points of this study was the assessment of the prevalence of sleep disorders in Iranian preschool children. The authors found there was a socioeconomic status relationship with sleep disorders. Against this strength, the cross-sectional design limited our causative assessment of sleep disorders. This study was conducted in Tehran province, so may not reflect the general population of Iran. We also did not evaluate parental medical and mental situations.
Acknowledgments
The authors thank the behavioral sciences research center of Shahid Beheshti University of Medical Sciences, Tehran, Iran, and all of the mothers who took part in this research.
Footnotes
Authors’ Contribution:Giti Ozgoli, Zohre Sheikhan, Farin Soleimani, Malihe Nasiri and Saba Amiri participated in the study design, literature review, data collection and analysis and editing the manuscript.
Funding/Support:This study was supported in part by grant 2446 from the behavioral sciences research center of Shahid Beheshti University of Medical Sciences, Tehran, Iran.
References
- 1.Wills L, Garcia J. Parasomnias: epidemiology and management. CNS Drugs. 2002;16(12):803–10. doi: 10.2165/00023210-200216120-00002. [DOI] [PubMed] [Google Scholar]
- 2.Spilsbury JC, Storfer-Isser A, Kirchner HL, Nelson L, Rosen CL, Drotar D, et al. Neighborhood disadvantage as a risk factor for pediatric obstructive sleep apnea. J Pediatr. 2006;149(3):342–7. doi: 10.1016/j.jpeds.2006.04.061. [DOI] [PubMed] [Google Scholar]
- 3.Schwebel DC, Brezausek CM, Ramey SL, Ramey CT. Interactions between child behavior patterns and parenting: implications for children's unintentional injury risk. J Pediatr Psychol. 2004;29(2):93–104. doi: 10.1093/jpepsy/jsh013. [DOI] [PubMed] [Google Scholar]
- 4.Ivanenko A, Crabtree VM, Obrien LM, Gozal D. Sleep complaints and psychiatric symptoms in children evaluated at a pediatric mental health clinic. J Clin Sleep Med. 2006;2(1):42–8. [PubMed] [Google Scholar]
- 5.Friedman NP, Corley RP, Hewitt JK, Wright KJ. Individual differences in childhood sleep problems predict later cognitive executive control. Sleep. 2009;32(3):323–33. doi: 10.1093/sleep/32.3.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meltzer LJ, Moore M. Sleep disruptions in parents of children and adolescents with chronic illnesses: prevalence, causes, and consequences. J Pediatr Psychol. 2008;33(3):279–91. doi: 10.1093/jpepsy/jsm118. [DOI] [PubMed] [Google Scholar]
- 7.Heussler HS. 9. Common causes of sleep disruption and daytime sleepiness: childhood sleep disorders II. Med J Aust. 2005;182(9):484–9. doi: 10.5694/j.1326-5377.2005.tb06793.x. [DOI] [PubMed] [Google Scholar]
- 8.Gelman VS, King NJ. Wellbeing of mothers with children exhibiting sleep disturbance. Aust J Psychol. 2001;53(1):18–22. doi: 10.1080/00049530108255117. [DOI] [Google Scholar]
- 9.Thiedke CC. Sleep disorders and sleep problems in childhood. Am Fam Physician. 2001;63(2):277–84. [PubMed] [Google Scholar]
- 10.Acebo C, Sadeh A, Seifer R, Tzischinsky O, Hafer A, Carskadon MA. Sleep/wake patterns derived from activity monitoring and maternal report for healthy 1- to 5-year-old children. Sleep. 2005;28(12):1568–77. doi: 10.1093/sleep/28.12.1568. [DOI] [PubMed] [Google Scholar]
- 11.Goldman SE, McGrew S, Johnson KP, Richdale AL, Clemons T, Malow BA. Sleep is associated with problem behaviors in children and adolescents with autism spectrum disorders. Research in Autism Spectrum Disorders. 2011;5(3):1223–9. doi: 10.1016/j.rasd.2011.01.010. [DOI] [Google Scholar]
- 12.Rzepecka H, McKenzie K, McClure I, Murphy S. Sleep, anxiety and challenging behaviour in children with intellectual disability and/or autism spectrum disorder. Res Dev Disabil. 2011;32(6):2758–66. doi: 10.1016/j.ridd.2011.05.034. [DOI] [PubMed] [Google Scholar]
- 13.Panaghi L, Kafashi A, Seraji M. Epidemiology of sleep disorders among primary school students in Tehran. Andishe & raftar J. 2004;10(1-2):50–8. [Google Scholar]
- 14.Nafeiy Z, Shakiba M, Kashavarzian F. The prevalence of sleep disorders in 1 to 2 year infants refering to health centers in yazd, 2008-2009. Toloae Behdasht J Health School Yazd. 2009;8(1):39–46. [Google Scholar]
- 15.Sadat HAS. Survey of the effect of non pharmacological intervention to improve of sleep in pediatric, that suffering of chronic illness. Nursing Research J. 2012;7(27):60–72. [Google Scholar]
- 16.Ebarhim A, Babak G, Alimohammad A, Shabnam J, Alireza A, Forough F. High Prevalence of Sleep Problems in School- and Preschool-aged Children in Tehran: a Population Based Study. Iran J Pediatr. 2013;23(1):45–52. [PMC free article] [PubMed] [Google Scholar]
- 17.Tietze AL, Blankenburg M, Hechler T, Michel E, Koh M, Schluter B, et al. Sleep disturbances in children with multiple disabilities. Sleep Med Rev. 2012;16(2):117–27. doi: 10.1016/j.smrv.2011.03.006. [DOI] [PubMed] [Google Scholar]
- 18.Mohammadi M, Ghalebaghi B, Ghaleh Bandi MF, Amintehrani E, Khodaie S, Shoaee S. Sleep patterns and sleep problems among preschool and school-aged group children in a primary care setting. Iran J Pediatr. 2007;17(3):213–21. [Google Scholar]
- 19.Munro BH. Statistical methods for health care research. 5 ed. Vol. 1. Philadelphia: Lippincott Williams and Wilkins; 2005. p. 377. [Google Scholar]
- 20.Shoghy M, Khanjari S, Farmany F, Hossaini F. Sleep pattern in school-age children, residents of the West Area in Tehran. Iran J Nursing. 2005;18(43):83–9. [Google Scholar]
- 21.Wang G, Xu G, Liu Z, Lu N, Ma R, Zhang E. Sleep patterns and sleep disturbances among Chinese school-aged children: prevalence and associated factors. Sleep Med. 2013;14(1):45–52. doi: 10.1016/j.sleep.2012.09.022. [DOI] [PubMed] [Google Scholar]
- 22.Ardani AR. Assessment the rules of demographic variables and body mass index in sleep quality among medical students. J Fundamentals Mental Health. 2012;14(2):132–9. [Google Scholar]
- 23.Day A, Haj-Bakri S, Lubchansky S, Mehta S. Sleep, anxiety and fatigue in family members of patients admitted to the intensive care unit: a questionnaire study. Crit Care. 2013;17(3):91. doi: 10.1186/cc12736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jan JE, Owens JA, Weiss MD, Johnson KP, Wasdell MB, Freeman RD, et al. Sleep hygiene for children with neurodevelopmental disabilities. Pediatrics. 2008;122(6):1343–50. doi: 10.1542/peds.2007-3308. [DOI] [PubMed] [Google Scholar]
- 25.Harmat L, Takacs J, Bodizs R. Music improves sleep quality in students. J Adv Nurs. 2008;62(3):327–35. doi: 10.1111/j.1365-2648.2008.04602.x. [DOI] [PubMed] [Google Scholar]
- 26.Gangwisch JE, Malaspina D, Boden-Albala B, Heymsfield SB. Inadequate sleep as a risk factor for obesity: analyses of the NHANES I. Sleep. 2005;28(10):1289–96. doi: 10.1093/sleep/28.10.1289. [DOI] [PubMed] [Google Scholar]
- 27.El-Sheikh M, Kelly RJ, Buckhalt JA, Benjamin Hinnant J. Children's sleep and adjustment over time: the role of socioeconomic context. Child Dev. 2010;81(3):870–83. doi: 10.1111/j.1467-8624.2010.01439.x. [DOI] [PubMed] [Google Scholar]
- 28.Wong MM, Brower KJ, Nigg JT, Zucker RA. Childhood sleep problems, response inhibition, and alcohol and drug outcomes in adolescence and young adulthood. Alcohol Clin Exp Res. 2010;34(6):1033–44. doi: 10.1111/j.1530-0277.2010.01178.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu X, Liu L, Owens JA, Kaplan DL. Sleep patterns and sleep problems among schoolchildren in the United States and China. Pediatrics. 2005;115(1 Suppl):241–9. doi: 10.1542/peds.2004-0815F. [DOI] [PubMed] [Google Scholar]
- 30.Gharamaleki AS, Hoseini SM, Zamani A, Vaezzadeh F, Djafarian K. Sleep pattern in 6-9 years old students living in tehran city. J Isfahan Med School. 2011;29(154) [Google Scholar]
- 31.Arman AR, Ay P, Fis NP, Ersu R, Topuzoglu A, Isik U, et al. Association of sleep duration with socio-economic status and behavioural problems among schoolchildren. Acta Paediatr. 2011;100(3):420–4. doi: 10.1111/j.1651-2227.2010.02023.x. [DOI] [PubMed] [Google Scholar]
- 32.Bagley SL, Weaver TL, Buchanan TW. Sex differences in physiological and affective responses to stress in remitted depression. Physiol Behav. 2011;104(2):180–6. doi: 10.1016/j.physbeh.2011.03.004. [DOI] [PubMed] [Google Scholar]
- 33.Valrie CR, Gil KM, Redding-Lallinger R, Daeschner C. Brief report: sleep in children with sickle cell disease: an analysis of daily diaries utilizing multilevel models. J Pediatr Psychol. 2007;32(7):857–61. doi: 10.1093/jpepsy/jsm016. [DOI] [PubMed] [Google Scholar]
- 34.Lee K, Cho M, Miaskowski C, Dodd M. Impaired sleep and rhythms in persons with cancer. Sleep Med Rev. 2004;8(3):199–212. doi: 10.1016/j.smrv.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 35.Hysing M, Sivertsen B, Stormark KM, Elgen I, Lundervold AJ. Sleep in children with chronic illness, and the relation to emotional and behavioral problems--a population-based study. J Pediatr Psychol. 2009;34(6):665–70. doi: 10.1093/jpepsy/jsn095. [DOI] [PubMed] [Google Scholar]
- 36.Spiegel K, Tasali E, Penev P, Van Cauter E. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141(11):846–50. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- 37.Knutson KL, Van Cauter E. Associations between sleep loss and increased risk of obesity and diabetes. Ann N Y Acad Sci. 2008;1129:287–304. doi: 10.1196/annals.1417.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sadeh A, Raviv A, Gruber R. Sleep patterns and sleep disruptions in school-age children. Developmental Psychology. 2000;36(3):291–301. doi: 10.1037/0012-1649.36.3.291. [DOI] [PubMed] [Google Scholar]
- 39.Jarrin DC, McGrath JJ, Quon EC. Objective and subjective socioeconomic gradients exist for sleep in children and adolescents. Health Psychol. 2014;33(3):301–5. doi: 10.1037/a0032924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wiater AH, Mitschke AR, Widdern SV, Fricke L, Breuer U, Lehmkuhl G. Sleep disorders and behavioural problems among 8- to 11-year-old children. Schlafstorungen und verhaltensprobleme bei 8-11 jahre alten kindern. Somnologie. 2005;9(4):210–4. doi: 10.1111/j.1439-054X.2005.00073.x. [DOI] [Google Scholar]
- 41.Dougherty D, Meikle SF, Owens P, Kelley E, Moy E. Children's health care in the first national healthcare quality report and national healthcare disparities report. Med care. 2005;43(3):58–63. doi: 10.1097/00005650-200503001-00009. [DOI] [PubMed] [Google Scholar]
- 42.Xu Z, Su H, Zou Y, Chen J, Wu J, Chang W. Sleep quality of Chinese adolescents: distribution and its associated factors. J Paediatr Child Health. 2012;48(2):138–45. doi: 10.1111/j.1440-1754.2011.02065.x. [DOI] [PubMed] [Google Scholar]
- 43.Van Cauter E, Knutson KL. Sleep and the epidemic of obesity in children and adults. Eur J Endocrinol. 2008;159 Suppl 1:S59–66. doi: 10.1530/EJE-08-0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cottrell L. Impact of childhood epilepsy on maternal sleep and socioemotional functioning. Clinical Pediatrics. 2005;44(7):613–6. doi: 10.1177/000992280504400709. [DOI] [PubMed] [Google Scholar]
- 45.El-Sheikh M, Buckhalt JA, Mize J, Acebo C. Marital conflict and disruption of children's sleep. Child Dev. 2006;77(1):31–43. doi: 10.1111/j.1467-8624.2006.00854.x. [DOI] [PubMed] [Google Scholar]
- 46.Biggs SN, Lushington K, van den Heuvel CJ, Martin AJ, Kennedy JD. Inconsistent sleep schedules and daytime behavioral difficulties in school-aged children. Sleep Med. 2011;12(8):780–6. doi: 10.1016/j.sleep.2011.03.017. [DOI] [PubMed] [Google Scholar]
- 47.Paunio T, Korhonen T, Hublin C, Partinen M, Kivimaki M, Koskenvuo M, et al. Longitudinal study on poor sleep and life dissatisfaction in a nationwide cohort of twins. Am J Epidemiol. 2009;169(2):206–13. doi: 10.1093/aje/kwn305. [DOI] [PubMed] [Google Scholar]
- 48.Meltzer LJ, Mindell JA. Impact of a child's chronic illness on maternal sleep and daytime functioning. Arch Intern Med. 2006;166(16):1749–55. doi: 10.1001/archinte.166.16.1749. [DOI] [PubMed] [Google Scholar]
- 49.Jenni OG, O'Connor BB. Children's sleep: an interplay between culture and biology. Pediatrics. 2005;115(1 Suppl):204–16. doi: 10.1542/peds.2004-0815B. [DOI] [PubMed] [Google Scholar]
- 50.Li S, Jin X, Yan C, Wu S, Jiang F, Shen X. Bed- and room-sharing in Chinese school-aged children: prevalence and association with sleep behaviors. Sleep Med. 2008;9(5):555–63. doi: 10.1016/j.sleep.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 51.Ward TM, Gay C, Anders TF, Alkon A, Lee KA. Sleep and napping patterns in 3-to-5-year old children attending full-day childcare centers. J Pediatr Psychol. 2008;33(6):666–72. doi: 10.1093/jpepsy/jsm102. [DOI] [PubMed] [Google Scholar]
- 52.Johnston C, Fine S, Weiss M, Weiss J, Weiss G, Freeman WS. Effects of stimulant medication treatment on mothers' and children's attributions for the behavior of children with attention deficit hyperactivity disorder. J Abnorm Child Psychol. 2000;28(4):371–82. doi: 10.1023/a:1005121110278. [DOI] [PubMed] [Google Scholar]
- 53.Cummings EM, Keller PS, Davies PT. Towards a family process model of maternal and paternal depressive symptoms: exploring multiple relations with child and family functioning. J Child Psychol Psychiatry. 2005;46(5):479–89. doi: 10.1111/j.1469-7610.2004.00368.x. [DOI] [PubMed] [Google Scholar]