Abstract
Hip distractor devices or hip fracture tables (HFTs) are vital to perform a reliable hip arthroscopy (HA) for the treatment of femoroacetabular impingement, especially when labral tears, chondral-labral delaminations, ligamentum teres tears, and other intraarticular disorders are present. Adequate hip distractors were not available in the early days of HA; most of HFTs being used those days were rigid, cumbersome, and did not allow us to properly perform an arthroscopic dynamic impingement test to evaluate and assess the femoral head and its site of impingement. The mayo table technique was developed because of the lack of appropriate hip instrumentation and an HFT when the author (A.P.S.) started to perform HA. This easy technique allows the surgeon to control hip maximal range of motion and also to assess completely the cam deformity in the posterolateral, superolateral, anterior, and anteroinferior aspects. It also allows the surgeon to revise where the cam is impinging and afterward perform a complete bony resection and decompression. We strongly believe that with the mayo table technique HA can be performed simply and reliably in old rigid and cumbersome HFTs and also hip distractors that do not allow an adequate dynamic assessment of the hip with maximal range of motion.
Hip arthroscopy (HA) started several years ago for the diagnosis and treatment of femoroacetabular impingement. The use and availability of appropriate and specialized hip distractor devices for this surgical procedure was not possible at that time. Several surgeons encountered difficulties regarding hip joint distraction when accessing the central compartment (CC) or acetabular fossa. Conventional surgical tables with adapted traction pulleys and metal scales were used those days and posteriorly rigid and cumbersome hip fracture tables (HFTs) were adapted to perform a reliable HA.1
HFTs, which are still used these days, provide easy distraction of the hip and allow the surgeon to work without difficulties in the acetabulum for a rim decompression, recession, labral repair, or reconstruction, to remove cartilage floating pieces and for ligamentum teres synovectomy and debridement. HFTs have several disadvantages: they are cumbersome, rigid, static, and uncomfortable when positioning adequately the hip and leg and consequently do not allow performing hip maneuvers in maximal range of motion. Difficulty is also encountered with innovative, and latest model hip distractors, when trying to achieve a comprehensive evaluation of the hip morphology. Most importantly, they do not allow achieving properly the arthroscopic dynamic impingement test (ADIT), which allows the surgeon to observe the congruence and behavior of the hip joint. An evaluation is considered an extremely important factor nowadays because of the high demand in elite patients involving maximal or extreme hip range of motion to achieve their sport.
Surgical Technique
The author (A.P.S.) performs HA in the modified supine position, with the patient supported on a conventional old HFT (MAQUET Gmbh, Rastatt, Germany). Surgery is performed under general anesthesia. No muscle relaxants are used, although they may be added. The padded counter traction post is applied against the proximal femur deliberately lateralizing this post 2 to 4 cm away the nonoperative leg, with a well-padded perineal post; both of the feet and shins are also well padded. The foot/boot of the operative hip is out of the HFT clamp; this free leg is positioned over a simple mayo table (Productos Medicos, Monterrey, Mexico), which is protected with folded blankets or a pillow, and the contralateral hip is well secured and wrapped in its boot and clamp. The hip is prepped and draped in a standard fashion (Fig 1, Fig 2, Fig 3).
Fig 1.

Left operative hip and patient position in modified supine with the left foot over a cushioned mayo table (Productos Medicos, Monterrey, Mexico). The left foot is slightly in external rotation.
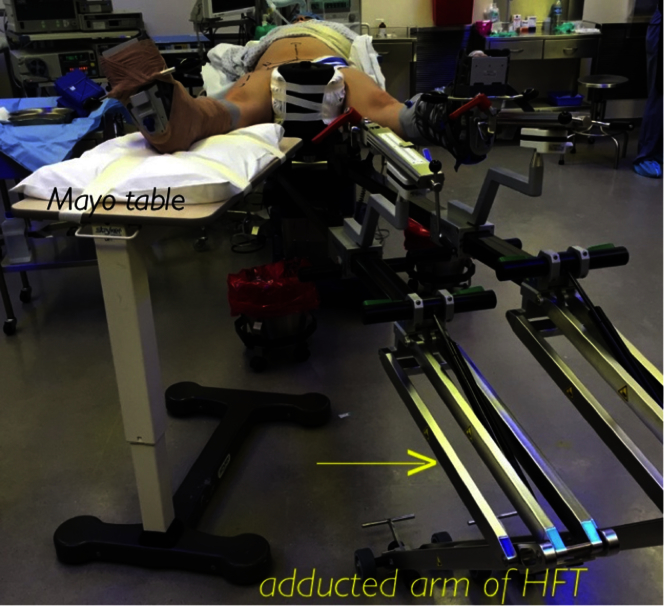
Fig 2.
Modified supine position with the right hip in abduction and over a cushioned mayo table. Observe the boot clamp out the hip fracture table (MAQUET Gmbh, Rastatt, Germany) and the adducted hip fracture table (HFT) arm toward the contralateral and nonoperative hip.
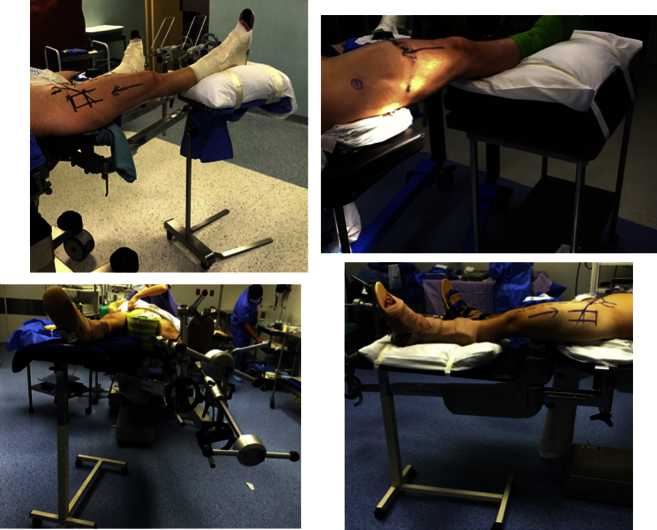
Fig 3.
Different hip fracture tables (old tables—top pictures; latest model tables—bottom pictures) and different mayo table stands. Observe that the technique is applicable in all cases without complexities.
Radiographic and anatomic landmarks are routinely used to enter the hip with no fluoroscopy. Portals are established to assess the peripheral and CC: an anterolateral portal, immediately anterior to the trochanteric tip, a peritrochanteric space portal situated 3 cm distally from the anterolateral portal, and a mid-anterior portal that is located 2 cm above the peritrochanteric space portal; the mid-anterior portal is used for anchor placement (Fig 4).2, 3, 4
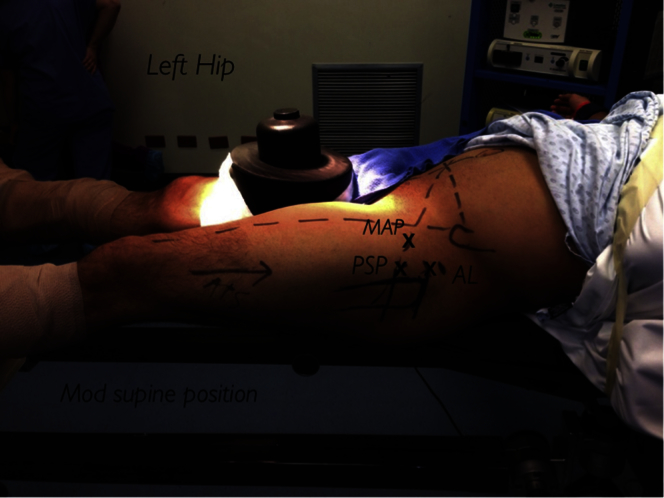
Fig 4.
Left operative hip with the modified supine position with the patient on a hip fracture table and portal placement marked with an (X): anterolateral (AL), peritrochanteric space portal (PSP), and mid-anterior portal (MAP).
When positioning the operative foot/boot over the mayo table, the arm and foot holder of the HFT is adducted toward the nonoperative leg (Fig 2). A surgical assistant will hold the hip in neutral position and he will control range of motion (flexion, extension, and rotations of the hip) depending on the surgeon's needs (Figs 5 and 6). An anterior oblique capsulotomy is achieved after radiographic and anatomic landmarks to enter to the femoral neck-head zone and posteriorly perform a femoral decompression on the cam-type deformity.4 Afterward, the ADIT is performed with the help of the surgical assistant, and it will be useful to delimitate if the cam resection is completed. After finishing on the peripheral compartment a nurse assistant or surgical technician will hold the free foot and attach it to the table clamp of the HFT and posteriorly start hip joint distraction under arthroscopic vision. A thorough evaluation, diagnosis, and treatment of the CC5, 6 is performed. Posteriorly, the hip joint is injected with viscous lubricant and a capsule closure is performed if the patients have generalized ligamentous laxity; portals are routinely injected with a local anesthetic and traction time is recorded.
Fig 5.
Intraoperative right hip (RH) examination with maximal hip range of motion (HROM) to compare postopratively with the arthroscopic dynamic impingement test when performing the cam decompression.
Fig 6.
The foot is out of the clamp of the fracture table. Observe the maximal external rotation of the hip/foot (MERH) to observe the most anterior and anteroinferior cam and the maximal internal rotation of the hip/foot (MIRH) to observe the most lateral and posterolateral cam.
A 30° arthroscopic lens is used throughout the peripheral compartment and exchanged with a 70° arthroscope when entering the CC with switching sticks or the desired technique (Table 1, Video 1).
Table 1.
Tips and Pearls for the Mayo Table Technique in Hip Arthroscopy
| 1. Use any surgical mayo table from your operating room or hospital. |
| 2. Place a well-cushioned pillow or blanket on top of the mayo table to avoid skin lacerations or iatrogenic neurologic complications to the foot and ankle. |
| 3. Drape the operative hip/leg on the cushioned mayo table in a standard fashion. |
| 4. Teach your fellow, resident, or surgical assistant how to perform hip range of motion so you can observe the femoral head-neck junction and prepare for your cam decompression or femoral osteochondroplasty. |
| 5. Arthroscopic dynamic impingement test is performed before the femoral osteochondroplasty for surgical planning and resection. |
| 6. Arthroscopic dynamic impingement test is performed again after the femoral osteochondroplasty to evaluate impinging zones left behind. |
| 7. Teach a surgical technician or a nurse how to wrap the foot or how to clamp it to the hip fracture table in a sterile fashion. |
| 8. Traction is applied under arthroscopic vision to enter the central compartment of the hip. |
It is worth mentioning that we have performed this technique in 4 different HFTs. Two of them are very old models (1975, 1984) and 2 are innovative and latest models (2012, 2014) (MAQUET Gmbh), but they do not allow performing the ADIT. We have not presented any complication, and this technique is applicable to all HFTs where the main goal is the evaluation of the hip by the ADIT with the hip and foot out of the fracture table to perform maximal and extreme hip range of motion.
Discussion
The advantage of our mayo table technique is its performance with any type of old hip fracture table or hip distractor device. The most of the hospitals devoted to hip surgery and orthopedic trauma surgery possess of an HFT. The disadvantage of our technique is that it was developed to perform HA through the peripheral compartment first, initiating without distraction through an anterior oblique capsulotomy to evaluate and decompress the cam deformity and posteriorly distract the hip joint under arthroscopic control and vision. Surgeons trained in HA with a CC starting point can find few difficulties with this technique. We strongly believe that HA can be made simple; special and expensive distractor devices are not needed to perform a reproducible hip arthroscopic surgery. The use of an HFT in these days can be part of the armament for the young, aspiring, and enthusiastic hip arthroscopic surgeons (Table 2).
Table 2.
Advantages and Disadvantages of the Mayo Table Technique in Hip Arthroscopy
| Advantages |
| 1. Friendly technique in the modified supine position and also the lateral position. |
| 2. Cost-effective technique (mayo table, pillow, standard old fracture table). |
| 3. Entire visualization of the cam deformity in the posterolateral, lateral, anterior, and anteroinferior aspects of the femoral head. |
| 4. Allows for an exhaustive evaluation of the femoral head and performance of the arthroscopic dynamic impingement test. |
| Disadvantages |
| 1. Can be unfamiliar to surgeons trained in hip arthroscopy with a central compartment starting point. |
| 2. Need for the presence of a surgical assistant in the operating room at all times, trained in how to place the foot clamp in the fracture table when starting to distract the hip joint. |
This technique allows us to perform a safe surgical procedure and also to observe exhaustively if we left behind an impinging anterior cam through an intraoperative ADIT. Maneuverability and maximal range of motion to the hip is achieved extremely well with this simple technique.
With our developed mayo table technique we want to make the young, enthusiastic, and aspiring hip surgeons aware that HA is reproducible and reliable. For this technique, no expensive instrumentation is needed. We have observed that in cases where an innovative hip distractor does not allow for an adequate maximal hip range of motion or ADIT when assessing the cam deformity, this technique is very useful.
Access to the cam deformity and femoral head is simple in the posterolateral, lateral, anterior, and anteroinferior aspects when the operative hip and/or foot is free of the boot or clamp of the HFT and controlled by the surgeon, fellow, or surgical assistant.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
This technique demonstrates how hip arthroscopy is performed in the modified supine position with the operative hip and leg placed on a mayo table support or stand with the foot or boot out of the fracture table clamp. This technique allows hip maximal range of motion posterior to the cam decompression or femoroplasty. It is reproducible in old hip fracture tables and also in hip distractor devices that do not allow for an arthroscopic dynamic impingement test.
References
- 1.Glick J.M., Sampson T.G., Gordon R.B., Behr J.T., Schmidt E. Hip arthroscopy by the lateral approach. Arthroscopy. 1987;3:4–12. doi: 10.1016/s0749-8063(87)80003-8. [DOI] [PubMed] [Google Scholar]
- 2.Byrd JWT. Hip arthroscopy the supine approach: Technique and anatomy of the intraarticular and peripheral compartments. Presented at the 3rd Annual San Francisco Hip Arthroscopy and Hip Preservation Surgery Meeting, San Francisco, CA, October 18, 2007.
- 3.Robertson W.J., Kelly B.T. The safe zone for hip arthroscopy: A cadaveric assessment of central, peripheral, and lateral compartment portal placement. Arthroscopy. 2008;24:1019–1026. doi: 10.1016/j.arthro.2008.05.008. [DOI] [PubMed] [Google Scholar]
- 4.Salas A.P. Radiographic and anatomic landmarks to approach the anterior capsule in hip arthroscopy. J Hip Preserv Surg. 2015;2:431–437. doi: 10.1093/jhps/hnv056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wettstein M., Dienst M. Arthroscopy of the peripheral compartment of the hip. Opr Tech Orthop. 2005;15:225–230. [Google Scholar]
- 6.Dienst M., Seil R., Kohn D.M. Safe access to the central compartment of the hip. Arthroscopy. 2005;21:1510–1514. doi: 10.1016/j.arthro.2005.09.014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This technique demonstrates how hip arthroscopy is performed in the modified supine position with the operative hip and leg placed on a mayo table support or stand with the foot or boot out of the fracture table clamp. This technique allows hip maximal range of motion posterior to the cam decompression or femoroplasty. It is reproducible in old hip fracture tables and also in hip distractor devices that do not allow for an arthroscopic dynamic impingement test.