Abstract
Background
As malaria transmission declines, it becomes more geographically focused and more likely due to asymptomatic and non-falciparum infections. To inform malaria elimination planning in the context of this changing epidemiology, local assessments on the risk factors for malaria infection are necessary, yet challenging due to the low number of malaria cases.
Methods
A population-based, cross-sectional study was performed using passive and active surveillance data collected in Aceh Besar District, Indonesia from 2014 to 2015. Malaria infection was defined as symptomatic polymerase chain reaction (PCR)-confirmed infection in index cases reported from health facilities, and asymptomatic or symptomatic PCR-confirmed infection identified in reactive case detection (RACD). Potential risk factors for any infection, species-specific infection, or secondary-case detection in RACD were assessed through questionnaires and evaluated for associations.
Results
Nineteen Plasmodium knowlesi, 12 Plasmodium vivax and six Plasmodium falciparum cases were identified passively, and 1495 community members screened in RACD, of which six secondary cases were detected (one P. knowlesi, three P. vivax, and two P. falciparum, with four being asymptomatic). Compared to non-infected subjects screened in RACD, cases identified through passive or active surveillance were more likely to be male (AOR 12.5, 95 % CI 3.0–52.1), adult (AOR 14.0, 95 % CI 2.2–89.6 for age 16–45 years compared to <15 years), have visited the forest in the previous month for any reason (AOR 5.6, 95 % CI 1.3–24.2), and have a workplace near or in the forest and requiring overnight stays (AOR 7.9, 95 % CI 1.6–39.7 compared to workplace not near or in the forest). Comparing subjects with infections of different species, differences were observed in sub-district of residence and other demographic and behavioural factors. Among subjects screened in RACD, cases compared to non-cases were more likely to be febrile and reside within 100 m of the index case.
Conclusion
In this setting, risk of malaria infection in index and RACD identified cases was associated with forest exposure, particularly overnights in the forest for work. In low-transmission settings, utilization of data available through routine passive and active surveillance can support efforts to target individuals at high risk.
Keywords: Risk factor, Passive surveillance, Active surveillance, Reactive case detection, Aceh Besar, Indonesia, Low-endemic setting, Malaria elimination, Plasmodium knowlesi, Plasmodium vivax, Mixed species
Background
The World Health Organization (WHO) has called for the ambitious commitment to eliminate malaria in 35 countries by 2030 [1]. All heads of states in the Asia Pacific region have committed to national malaria elimination by this date as well [2]. In the low-endemic phase that precedes the achievement of malaria elimination, and generally follows a higher transmission period, malaria programmes are faced with the challenge of a changing epidemiology of malaria. In this phase, an increasing proportion of malaria is imported and the high-risk group is often no longer young children and pregnant women, but rather tied to demographic and occupational risk factors specific to a local setting. Transmission also becomes more geographically focal, and more likely propagated through asymptomatic and non-falciparum infections [3].
In high malaria transmission settings, children under 5 years of age [4] and pregnant women [5] are the groups most vulnerable. Other risk factors in these settings include: low socio-economic status [6], low education level [7], poor quality and/or traditionally constructed housing [8], and low coverage and/or utilization of insecticide-treated bed nets (ITNs) or long-lasting insecticide-treated nets (LLINs), and/or indoor residual spraying (IRS) [9]. In contrast, risk factor assessments from low-transmission settings have shown risk factors as being an adult male, travel, outdoor exposure related to occupation, sleeping outdoors, and social activities [3, 10, 11]. However, findings from most of these studies have been extrapolated from epidemiological trends seen among cases identified through passive surveillance, and without control groups. Cross-sectional surveys are challenging to perform in low-transmission settings due to the low prevalence of infection [12] and case–control studies may not be easily implementable in operational settings. Further, there are limited data from multi-species low-transmission settings.
In order to address the challenge of malaria transmission that is more geographically focal and characterized by asymptomatic infection, the WHO recommends intensified surveillance in high-risk areas through epidemiologic investigation of symptomatic cases reported by health facilities (case investigation) as well as reactive case detection (RACD), which is the screening of household members and neighbours of index cases reported in passive surveillance. RACD aims to find any individuals with ‘secondary’, often asymptomatic infection in order to provide treatment to interrupt further transmission [13]. RACD is resource intensive and used widely [14], but what epidemiological or operational factors are associated with secondary-case detection is unclear, and likely context specific [10, 15–17].
In recent years, widespread scale-up of interventions such as ITNs, IRS, diagnostics, and effective anti-malarial drugs has led to significant declines in malaria burden in Indonesia, from over 1.3 million cases in 2006 [18] to 252,027 laboratory-confirmed cases in 2014 [19]. Among 513 districts, 213 districts (42 %) are certified as malaria free and 125 districts (24 %) have applied for certification of malaria elimination [20]. To achieve elimination in the remaining districts, intensified and targeted context-specific strategies will be needed, and an understanding of the risk factors for malaria infection is critical to inform strategic planning and implementation.
To address this challenge, a population-based, risk-factor assessment study was conducted in Aceh Besar, a district of Aceh Province that is aiming for malaria elimination and has a unique multi-species epidemiology that includes Plasmodium vivax, Plasmodium falciparum, and recently discovered Plasmodium knowlesi [21]. This cross-sectional study utilizing passive and active surveillance data was conducted to identify potential risk factors for: (1) any symptomatic or asymptomatic infection; (2) species-specific infection; and, (3) infection identified through RACD.
Methods
Study design
A cross-sectional study was performed utilizing prospectively collected data obtained through population-based passive and active malaria surveillance.
Study site
Aceh Besar is a district of Aceh Province, on Sumatra Island in western Indonesia (Fig. 1). The district covers 2903 km2 with most of its territory on Sumatra mainland plus some small islands. Being located near to the Equator, temperatures range from 25 to 29 °C and humidity is 65–85 %. From 2010 to 2014 monthly average rainfall ranged from 57.92 to 297 mm, with the rainy season spanning August to January [22, 23]. The high malaria transmission season occurs from January to July and August to December is considered the low transmission season. The annual parasite incidence (API) has been successfully reduced from 2.6 cases per 1000 population in 2006 [24], to 0.4 per 1000 in 2013 [25]. As part of an intensified malaria elimination strategy, in 2010, the District Health Office initiated case investigation and RACD, referred to as ‘contact survey’ in Indonesian. Designated malaria surveillance staff members based at health facilities visit the homes of all microscopy-confirmed malaria index cases reported from health facilities and perform an assessment to identify potential risk factors and classify the case as local or imported. Drawing on WHO guidelines and findings, the RACD policy involves microscopic diagnostic screening of all household members of an index case and of the neighbours living within a 500 m radius of the index case [26].
Fig. 1.
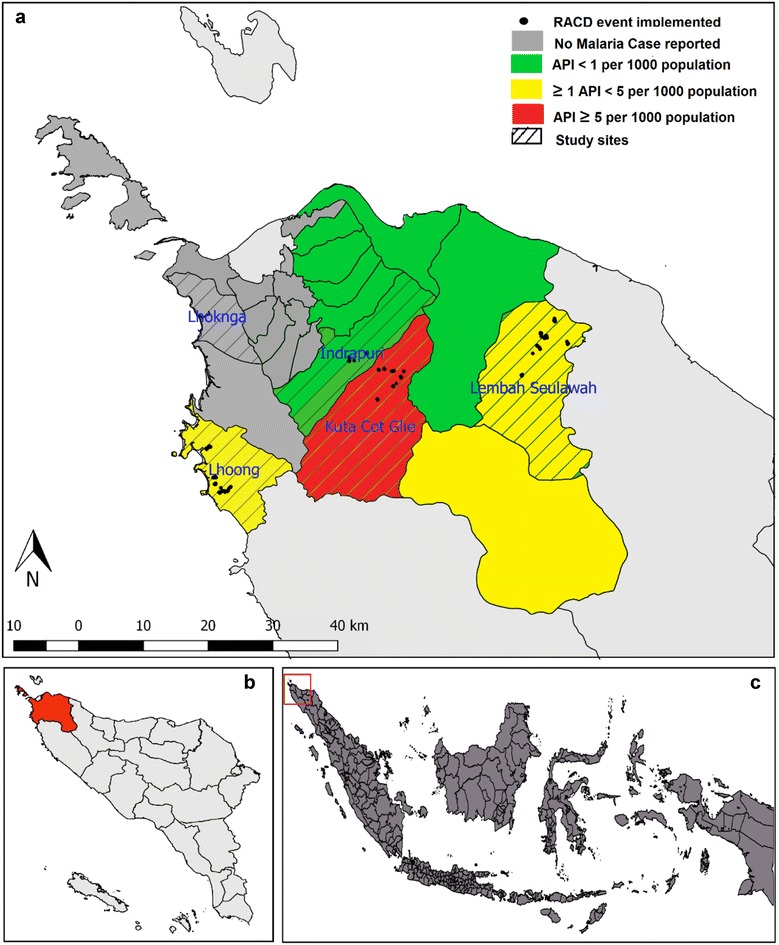
a Map of Aceh Besar District, with sub-district API rates from 2013 shown. Five study sub-districts shaded with diagonal lines. Black dots indicate locations of study RACD events. b Location of Aceh Besar in Aceh Province. c Location of Aceh Besar in Indonesia. RACD reactive case detection, API Annual parasite incidence
Study population
Study population included malaria positive cases reported from five sub-district level primary health centres (PHCs) that reported 78 % of all cases reported in Aceh Besar in 2013: Indrapuri, Lembah Seulawah, Kuta Cot Glie, Lhoong, and Lhoknga, as well as household members and neighbours residing within a 500-m radius of index cases. The study was conducted over 19 months, from June 2014 to December 2015.
Health facility and field procedures
Data collection for the study was nested within existing District Health Office passive and active surveillance procedures. Subjects presenting to PHCs with suspected malaria received a finger prick and blood was collected to prepare thick and thin smears for microscopy. Microscopy-confirmed cases were reported to district level within 1–3 days. At the time of diagnosis, informed consent was obtained for the collection of an additional 250 µL–3 mL of venous blood (depending on the age of the patient), which was partly used to generate dried blood spots (DBS), with the remaining stored as whole blood.
Within 1–3 days, the surveillance team visited the household of the index case to conduct a case investigation, which involved the administering of a structured questionnaire to assess potential risk factors. Within 1– 7 days of the index case report, RACD was conducted among subjects residing in households located within 500 m of the index cases. In RACD, blood was collected by finger prick and used to prepare thick and thin smears for microscopy as well as DBS, and household and individual level questionnaires similar to that used for the index case were administered. Questionnaires were translated into Bahasa Indonesia and administered using Nexus® tablet computers. The household level questionnaire assessed socio-economic status, housing structure type, household population, proximity of house to a potential breeding site and to the forest, and bed net ownership, bed net usage the night prior, and IRS coverage in the past year. Questions assessing socio-economic status were based on the validated Indonesian basic health survey questionnaire [27]. The individual-level questionnaire assessed age, gender, travel history (defined as spending one night outside of their village in the previous month but not including the past week due to the incubation period of malaria being at least 1 week), occupation, frequency and reasons for visits to the forest in the last month, utilization of vector control measures such as bed nets, and history of having a fever within the previous 2 weeks. All positive cases detected at PHC or through RACD activities received malaria treatment based on slide and loop-mediated isothermal amplification (LAMP) results and according to national treatment guidelines [28].
The investigation team consisted of five people: a microscopist and surveillance officer from the PHC, two community health workers from the village (a midwife plus a village malaria worker or village leader), and the study field coordinator. Up to two return visits were conducted to maximize coverage of the target area, with a goal to reach at minimum 40 subjects or at least 80 % of the residents within each of the closest five households.
Sample size
The study was part of umbrella study whereby the goal was to compare the yield of microscopy versus LAMP in RACD (anticipated positivity rates 2.5 and 5.0 %, respectively). Thus, the study was powered to compare paired proportions of LAMP versus microscopy positivity when the number screened in RACD reached 940 (α = 0.05, two-sided, β = 0.80), but with the plan to continue over at least a 1-year period to enable analyses to take into account seasonal variation.
Laboratory testing
In passive surveillance, thick and thin blood smears were collected from suspected malaria cases and examined immediately by trained microscopists at the PHCs. In RACD, PHC microscopists collected thick and thin blood smears in the field and transported them in closed slide boxes for subsequent examination at the PHC. Slides were fixed and stained with 3 % Giemsa. Parasite densities were determined by counting the number of asexual parasites per 200 or 500 white blood cells (WBC) and calculating parasites/µL assuming a WBC count of 8000 parasites/µL. A thin smear was considered negative if no parasites were seen in 100 high-powered fields. If positive, an additional 100 high-powered fields were examined to determine species [29]. Quality assurance (QA) was conducted by a district expert level-certified microscopist for all positive cases and 10 % of randomly selected negatives. Further cross-checking was carried out at provincial level for all positive cases and to resolve discrepant results between the PHC and district-level microscopists [13].
All DBS samples collected were dried overnight then stored in sealed plastic bags with desiccant. Initial extraction of DNA and LAMP testing on all samples were performed at the Aceh Provincial Health Laboratory. DNA was extracted from DBS using the Saponin/Chelex-100 method [30]. Using 15 µL of chelex-extracted DNA, Pan-LAMP testing followed by Pf-LAMP specific testing for Pan-LAMP positive samples was performed using a commerical Loopamp detection kit [31, 32] in accordance to manufacturer’s instructions (Eiken Chemical, Japan). Pan-LAMP positive cases underwent further molecular testing at the Eijkman Institute using DNA that was chelex-extracted from a second DBS. Samples first underwent nested PCR targeting the cytochrome b gene, followed by AluI enzyme digestion for species identification (not including P. knowlesi) as previously described [33–35]. After a report of indeterminate species and suspicion of P. knowlesi by a field microscopist, as well as limited data on the performance of the cytochrome b PCR method for detection of P. knowlesi, additional methods were employed. All Pan-LAMP positive samples were then tested by 18S rDNA nested PCR [36, 37] as well as P. knowlesi-specific PCR [38]. For a proportion of those testing positive by P. knowlesi-specific PCR, Qiagen-extracted DNA from whole blood (QIAamp Blood Minikit, Qiagen, CA) underwent sequencing (Eijkman Institute Sequencing Facility). All extractions were performed in rooms separate from where amplification was conducted. Using chelex-extracted DNA from a second blood spot, PCR targeting the cytochrome b gene was also performed on 10 % of randomly selected LAMP negative individuals from RACD.
DBS were stored at 4 °C within 1 week of collection, and then at −20 °C within 1 month of collection. Venous blood samples were stored at 4 °C for up to 5 days after collection, then transported along with the second blood spot in an ice box to Eijkman Institute in Jakarta using a 1-day service. Upon arrival at Eijkman, samples underwent DNA extraction or were stored at −20 °C (DBS) or −80 °C (whole blood samples). All extracted DNA was stored at −20 °C.
Data management and statistical analysis
Data were merged, cleaned and analysed using STATA version 14.0. Maps were generated using QGIS version 2.14.0.
The primary analysis was to evaluate the associations between potential risk factors and any PCR-confirmed symptomatic or asymptomatic infection. Secondary analyses were to evaluate the associations between potential risk factors and PCR-confirmed species-specific infection, as well as PCR-confirmed infection identified through RACD.
To explore relationships between potential risk factors and each of the outcome measures, the Chi squared test or Fisher’s exact test was used for categorical variables, and Wilcoxon rank-sum or Kruskal–Wallis rank test was used for continuous variables. P values less than 0.05 were considered statistically significant, and further explored in a bivariate mixed effects logistic regression model. For the multivariate mixed effects logistic regression model, variables with P values <0.25 in the unadjusted analysis were considered [39] and correlation and collinearity across all variables was considered. A purposeful selection approach was used to select the model of best fit. Variables that had P value <0.1 and changed any parameter estimates by 20 % were retained [40]. Akaike’s information criteria (AIC) and likelihood ratio test (LRT) were also taken into consideration in the model selection [41]. The bivariate and multivariate models accounted for clustering at the level of the household, and because of the small sample size for secondary outcome measures, they were only performed for the primary analysis.
Independent variables were divided into three categories: socio-demographic, prevention and behaviours, and forest exposure and environment (Tables 1, 2, 3). Occupation was originally recorded as one of 14 types. After preliminary analyses identified forest-related work as a major risk factor for infection, one constructing variable was developed by re-classifying occupation into three sub-groups: unemployed; non forest-related jobs including: student, fisherman, manufacturing/factory, office/clerical, housewife, retail/shopkeeper, and driver; and, forest-related jobs that included logger, soldier/police, farmer, rubber tapper, miner, and other forest worker). The quality of housing structure variable was constructed based on type of window, wall, floor, and roof. Good quality was defined as having a window, cement wall, cement or tile floor, and tin roof; poor quality was defined as no window, wood wall, dirt floor, and no roof or having a thatched roof. Houses not meeting these criteria were otherwise considered moderate quality. The wealth index was generated by multiple correspondence analysis (MCA) based on 11 assets ownership variables for binary and categorical data [42]. The MCA output was taken as a weight for each variables and wealth index was constructed based on the first dimension that explained 70 % by MCA output. Wealth index was then ranked into quintiles, with the wealthiest represented in the highest quintile. For the secondary case analysis, index case and RACD-level factors were also assessed including: distance to the index case household, Plasmodium species, RACD response time from date of index case presentation, and coverage of RACD among all eligible individuals in the intervention area.
Table 1.
Distribution (%) of potential risk factors among malaria cases (index and secondary cases), non-cases (screened in RACD), and by Plasmodium types
| Variable | Non-cases no. (%) (n = 1489) |
Cases no. (%) (n = 43) |
P | Cases by Plasmodium type | |||
|---|---|---|---|---|---|---|---|
| Pf no. (%) (n = 8) |
Pv no. (%) (n = 15) |
Pk no. (%) (n = 20) |
P | ||||
| Detection method | |||||||
| Passive | n/a | 37 (100) | <0.0001 | 6 (16.2) | 12 (32.4) | 19 (51.4) | 0.253 |
| RACD | 1489 (99.6) | 6 (0.4) | 2 (33.3) | 3 (50.0) | 1 (16.7) | ||
| Socio-demographic | |||||||
| Age category (years) | |||||||
| ≤15 | 481 (99.6) | 2 (0.4) | <0.0001 | 0 (0.0) | 0 (0.0) | 2 (100) | 0.033 |
| 16–30 | 362 (94.3) | 22 (5.7) | 4 (18.2) | 12 (54.6) | 6 (27.3) | ||
| 31–45 | 356 (94.9) | 19 (5.1) | 4 (21.0) | 3 (15.8) | 12 (63.2) | ||
| 46 + | 290 (100) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Gender | |||||||
| Female | 836 (99.6) | 3 (0.4) | <0.0001 | 0 (0.0) | 0 (0.0) | 3 (100) | 0.281 |
| Male | 653 (94.2) | 40 (5.8) | 8 (20.0) | 15 (37.5) | 17 (42.5) | ||
| Education of household head | |||||||
| No school | 40 (95.2) | 2 (4.8) | 0.072 | 0 (0.0) | 0 (0.0) | 2 (100) | 0.006 |
| Primary school | 481 (98.0) | 10 (2.0) | 1 (10.0) | 8 (80.0) | 1 (10.0) | ||
| Secondary school | 670 (96.1) | 27 (3.9) | 7 (25.9) | 7 (25.9) | 13 (48.2) | ||
| Tertiary school | 298 (98.7) | 4 (1.3) | 0 (0.0) | 0 (0.0) | 4 (100) | ||
| Occupation category | |||||||
| Unemployed | 281 (99.7) | 1 (0.3) | <0.0001 | 0 (0.0) | 1 (100) | 0 (0.0) | 0.112 |
| Not forest-related job | 847 (98.6) | 12 (1.4) | 1 (8.3) | 2 (16.7) | 9 (75.0) | ||
| Forest-related job | 361 (92.3) | 30 (7.7) | 7 (23.3) | 12 (40.0) | 11 (36.7) | ||
| Wealth index (quintile) | |||||||
| 1st | 295 (96.1) | 12 (3.9) | 0.517 | 3 (25.0) | 2 (16.7) | 7 (58.3) | 0.470 |
| 2nd | 306 (97.8) | 7 (2.2) | 1 (14.3) | 3 (42.9) | 3 (42.9) | ||
| 3rd | 302 (97.4) | 8 (2.6) | 3 (37.5) | 3 (37.5) | 2 (25.0) | ||
| 4th | 444 (97.8) | 10 (2.2) | 1 (10.0) | 3 (30.0) | 6 (60.0) | ||
| 5th | 142 (95.9) | 6 (4.1) | 0 (0.0) | 4 (66.7) | 2 (33.3) | ||
| Subdistrict | |||||||
| Lembah Seulawah | 525 (97.2) | 15 (2.8) | 0.978 | 2 (13.3) | 1 (6.7) | 12 (80.0) | <0.0001 |
| Kuta Cot Glie | 374 (97.4) | 10 (2.6) | 6 (60.0) | 1 (10.0) | 3 (30.0) | ||
| Lhoong | 511 (97.0) | 16 (3.0) | 0 (0.0) | 12 (75.0) | 4 (25.0) | ||
| Indrapuri | 79 (97.5) | 2 (2.5) | 0 (0.0) | 1 (50.0) | 1 (50.0) | ||
| Lhoknga | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Prevention and behaviours | |||||||
| Travel | |||||||
| No | 1340 (98.6) | 19 (1.4) | <0.0001 | 1 (5.3) | 6 (31.6) | 12 (63.2) | 0.071 |
| Yes | 149 (86.1) | 24 (13.9) | 7 (29.2) | 9 (37.5) | 8 (33.3) | ||
| ITN ownership | |||||||
| No ITN | 499 (96.2) | 20 (3.8) | 0.119 | 4 (20.0) | 6 (30.0) | 10 (50.0) | 0.911 |
| <1 ITN/2 people | 712 (98.1) | 14 (1.9) | 2 (14.3) | 5 (35.7) | 7 (50.0) | ||
| ≥1 ITN/2 people | 278 (96.9) | 9 (3.1) | 2 (22.2) | 4 (44.4) | 3 (33.3) | ||
| Slept under a bed net previous night | |||||||
| No | 658 (96.0) | 27 (4.0) | 0.016 | 7 (25.9) | 9 (33.3) | 11 (40.7) | 0.264 |
| Yes | 831 (98.1) | 16 (1.9) | 1 (6.3) | 6 (37.5) | 9 (56.3) | ||
| House sprayed in previous 1 year | |||||||
| No | 1381 (97.2) | 40 (2.8) | 0.945 | 8 (20.0) | 13 (32.5) | 19 (47.5) | 0.575 |
| Yes | 108 (97.3) | 3 (2.7) | 0 (0.0) | 2 (66.7) | 1 (33.3) | ||
| Slept outside house previous night | |||||||
| No | 1459 (97.1) | 43 (2.9) | 0.347 | 8 (18.6) | 15 (34.9) | 20 (46.5) | n/a |
| Yes | 30 (100) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Forest exposure and environment | |||||||
| Workplace near or in forest | |||||||
| No | 1027 (99.2) | 8 (0.8) | <0.0001 | 0 (0.0) | 3 (37.5) | 5 (62.5) | 0.401 |
| Yes, overnights not required | 273 (98.6) | 4 (1.4) | 0 (0.0) | 1 (25.0) | 3 (75.0) | ||
| Yes, overnights required | 189 (85.9) | 31 (14.1) | 8 (25.8) | 11 (35.5) | 12 (38.7) | ||
| Distance workplace to forest (km)a | |||||||
| In forest | 209 (87.8) | 29 (12.2) | <0.0001 | 7 (24.1) | 12 (41.4) | 10 (34.5) | 0.373 |
| <1 | 191 (98.0) | 4 (2.0) | 1 (25.0) | 0 (0.0) | 3 (75.0) | ||
| 1–5 | 59 (98.3) | 1 (1.7) | 0 (0.0) | 0 (0.0) | 1 (100) | ||
| >5–10 | 3 (75.0) | 1 (25.0) | 0 (0.0) | 0 (0.0) | 1 (100) | ||
| Visited forest in the last month for any reason | |||||||
| No | 1241 (99.0) | 12 (1.0) | <0.0001 | 1 (8.3) | 4 (33.3) | 7 (58.3) | 0.552 |
| Yes | 248 (88.9) | 31 (11.1) | 7 (22.6) | 11 (35.5) | 13 (41.9) | ||
| Main reasonb | |||||||
| Residence | 108 (94.7) | 6 (5.3) | 0.029 | 0 (0.0) | 1 (16.7) | 5 (83.3) | 0.032 |
| Work | 111 (84.1) | 21 (15.9) | 6 (28.6) | 10 (47.6) | 5 (23.8) | ||
| Other reasonc | 29 (87.9) | 4 (12.1) | 1 (25.0) | 0 (0.0) | 3 (75.0) | ||
| Median visit (days), rangeb | 30 (1–30) | 14 (1–30) | 0.002 | 14 (4–30) | 10 (1–30) | 25 (3–30) | 0.603 |
| Malaria transmission season | |||||||
| Low | 717 (97.6) | 18 (2.4) | 0.415 | 3 (16.7) | 6 (33.3) | 9 (50.0) | 0.921 |
| High | 772 (96.9) | 25 (3.1) | 5 (20.0) | 9 (36.0) | 11 (44.0) | ||
| Reported living near water body | |||||||
| No | 633 (98.0) | 13 (2.0) | 0.108 | 3 (23.1) | 2 (15.4) | 8 (61.5) | 0.204 |
| Yes | 856 (96.6) | 30 (3.4) | 5 (16.7) | 13 (43.3) | 12 (40.0) | ||
| Distance living to water bodyd (m) | |||||||
| <100 | 435 (96.0) | 18 (4.0) | 0.609 | 2 (11.1) | 8 (44.4) | 8 (44.4) | 0.563 |
| 100–499 | 168 (97.1) | 5 (2.9) | 2 (40.0) | 1 (20.0) | 2 (40.0) | ||
| ≥500 | 253 (97.3) | 7 (2.7) | 1 (14.3) | 4 (57.1) | 2 (28.6) | ||
| Reported living near or in forest | |||||||
| No | 712 (97.4) | 19 (2.6) | 0.638 | 4 (21.1) | 8 (42.1) | 7 (36.8) | 0.566 |
| Yes | 777 (97.0) | 24 (3.0) | 4 (16.7) | 7 (29.2) | 13 (54.2) | ||
| Distance living to foreste (km) | |||||||
| In forest | 147 (96.1) | 6 (3.9) | 0.651 | 0 (0.0) | 1 (16.7) | 5 (83.3) | 0.040 |
| <1 | 440 (96.9) | 14 (3.1) | 3 (21.4) | 3 (21.4) | 8 (57.1) | ||
| 1-5 | 170 (98.3) | 3 (1.7) | 0 (0.0) | 3 (100) | 0 (0.0) | ||
| >5 and <10 | 20 (95.2) | 1 (4.8) | 1 (100) | 0 (0.0) | 0 (0.0) | ||
| Housing quality, composite variable | |||||||
| Good | 831 (97.7) | 20 (2.4) | 0.162 | 3 (15.0) | 7 (35.0) | 10 (50.0) | 0.181 |
| Moderate | 335 (95.7) | 15 (4.3) | 1 (6.7) | 7 (46.7) | 7 (46.7) | ||
| Poor | 323 (97.6) | 8 (2.4) | 4 (50.0) | 1 (12.5) | 3 (37.5) | ||
an = 497 people (462 non-cases and 35 cases: eight P. falciparum, 12 P. vivax, 15 P. knowlesi)
bn = 279 people (248 non-cases and 31 cases: seven P. falciparum, 11 P. vivax, 13 P. knowlesi)
cOther reasons: farming, hunting, school, accompanying parent
dn = 886 people (856 non-cases and 30 cases: five P. falciparum, 13 P. vivax, 12 P. knowlesi)
en = 801 people (777 non-cases and 24 cases: four P. falciparum, seven P. vivax, 13 P. knowlesi)
Table 2.
Bivariate and multivariate analyses among malaria infected (n = 43) versus non-infected subjects (n = 1489)
| Variables | Bivariate | Multivariable | ||
|---|---|---|---|---|
| OR (95 % CI) | P | AOR (95 % CI) | P | |
| Socio-demographic | ||||
| Age category (years) | ≤15 as reference | |||
| 16–45 | 15.17 (3.55–64.8) | <0.0001 | 13.98 (2.17–89.58) | 0.005 |
| 46+a | – | – | – | – |
| Gender | Female as reference | |||
| Male | 20.26 (5.97–68.69) | <0.0001 | 12.54 (3.02–52.12) | 0.001 |
| Occupation category | Unemployed as reference | |||
| Not forest-related job | 4.06 (0.52–31.99) | 0.183 | – | – |
| Forest-related job | 28.87 (3.76–221.64) | 0.001 | – | – |
| Prevention and behaviours | ||||
| Travel in the previous month | No as reference | |||
| Yes | 42.78 (14.29–128.20) | <0.0001 | – | – |
| Sleep under bed net | No as reference | |||
| Yes | 0.45 (0.23–0.90) | 0.023 | 2.75 (0.83–9.05) | 0.097 |
| Forest exposure and environment | ||||
| Workplace near or in forest | No as reference | |||
| Yes, overnights not required | 2.20 (0.55–8.72) | 0.263 | 0.60 (0.11–3.21) | 0.555 |
| Yes, overnights required | 96.63 (23.00–406.21) | <0.0001 | 7.92 (1.58–39.71) | 0.012 |
| Visited forest in previous month for any reason | No as reference | |||
| Yes | 35.23 (11.54–107.58) | <0.0001 | 5.62 (1.31–24.15) | 0.020 |
aCategory dropped as no malaria infected subjects in this age category
Table 3.
Distribution and associations between epidemiological and operational factors among secondary case and non-secondary case from RACD
| Variable | Non-secondary case (n = 1489) |
Secondary case (n = 6) |
P | ||
|---|---|---|---|---|---|
| No. | (%) | No. | (%) | ||
| Socio-demographic | |||||
| Age category (years) | |||||
| ≤15 | 481 | 99.8 | 1 | 0.2 | 0.151 |
| 16–30 | 362 | 98.9 | 4 | 1.1 | |
| 31–45 | 356 | 99.7 | 1 | 0.3 | |
| 46+ | 290 | 100 | 0 | 0.0 | |
| Gender | |||||
| Female | 836 | 100 | 0 | 0.0 | 0.007 |
| Male | 653 | 99.1 | 6 | 0.9 | |
| Education of household head | |||||
| No school | 40 | 100 | 0 | 0.0 | 0.450 |
| Primary school | 481 | 99.8 | 1 | 0.2 | |
| Secondary school | 670 | 99.3 | 5 | 0.7 | |
| Tertiary school | 298 | 100 | 0 | 0.0 | |
| Occupation category | |||||
| Unemployed | 281 | 100 | 0 | 0.0 | 0.010 |
| Not forest-related job | 847 | 99.9 | 1 | 0.1 | |
| Forest-related job | 361 | 98.6 | 5 | 1.4 | |
| Wealth index ( quintile) | |||||
| 1st | 295 | 99.7 | 1 | 0.3 | 0.796 |
| 2nd | 306 | 99.7 | 1 | 0.3 | |
| 3rd | 302 | 99.3 | 2 | 0.7 | |
| 4th | 444 | 99.8 | 1 | 0.2 | |
| 5th | 142 | 99.3 | 1 | 0.7 | |
| Sub-district | |||||
| Lembah Seulawah | 525 | 99.4 | 3 | 0.6 | 0.917 |
| Kuta Cot Glie | 374 | 99.7 | 1 | 0.3 | |
| Lhoong | 511 | 99.6 | 2 | 0.4 | |
| Indrapuri | 79 | 100 | 0 | 0.0 | |
| Lhoknga | n/a | n/a | n/a | n/a | |
| Clinical history | |||||
| Reported fever in previous 2 weeks | |||||
| No | 1445 | 99.7 | 4 | 0.3 | 0.013 |
| Yes | 44 | 95.7 | 2 | 4.3 | |
| Prevention and behaviours | |||||
| Travel | |||||
| No | 1340 | 99.8 | 3 | 0.2 | 0.016 |
| Yes | 149 | 98.0 | 3 | 2.0 | |
| Bed net ownership | |||||
| No ITN | 499 | 99.2 | 4 | 0.8 | 0.289 |
| <1 ITN/2 people | 712 | 99.7 | 2 | 0.3 | |
| ≥1 ITN/2 people | 278 | 100 | 0 | 0.0 | |
| Slept under bed net previous night | |||||
| No | 658 | 99.3 | 5 | 0.7 | 0.094 |
| Yes | 831 | 99.9 | 1 | 0.1 | |
| House spraying in previous 1 year | |||||
| No | 1381 | 99.6 | 6 | 0.4 | 0.493 |
| Yes | 108 | 100 | 0 | 0.0 | |
| Slept outside house last night | |||||
| No | 1459 | 99.6 | 6 | 0.4 | 0.725 |
| Yes | 30 | 100 | 0 | 0.0 | |
| Forest exposure and environment | |||||
| Workplace near or in forest | |||||
| No | 1027 | 100 | 0 | 0.0 | <0.0001 |
| Yes, overnights not required | 273 | 100 | 0 | 0.0 | |
| Yes, overnights required | 189 | 96.9 | 6 | 3.1 | |
| Distance workplace to forest (n = 462) | |||||
| In forest | 209 | 97.2 | 6 | 2.8 | 0.085 |
| <1 km | 191 | 100 | 0 | 0.0 | |
| 1–5 km | 59 | 100 | 0 | 0.0 | |
| >5–10 km | 3 | 100 | 0 | 0.0 | |
| Visited forest in the last month | |||||
| No | 1241 | 99.9 | 1 | 0.1 | 0.001 |
| Yes | 248 | 98.0 | 5 | 2.0 | |
| Main reason (n = 253) | |||||
| Residence | 108 | 99.1 | 1 | 0.9 | 0.430 |
| Work | 111 | 96.5 | 4 | 3.5 | |
| Other reason | 29 | 100 | 0 | 0.0 | |
| Median visit (days), range (n = 253) | 30 (1–30) | – | 14 (4–30) | – | 0.596 |
| Season | |||||
| Low transmission | 734 | 99.7 | 2 | 0.3 | 0.688 |
| High transmission | 793 | 99.5 | 4 | 0.5 | |
| Reported living near water bodies | |||||
| No | 633 | 99.7 | 2 | 0.3 | 0.650 |
| Yes | 856 | 99.5 | 4 | 0.5 | |
| Reported living near or in forest | |||||
| No | 712 | 99.7 | 2 | 0.3 | 0.689 |
| Yes | 777 | 99.5 | 4 | 0.5 | |
| Housing quality | |||||
| Good | 831 | 99.6 | 3 | 0.4 | 0.858 |
| Moderate | 335 | 99.4 | 2 | 0.6 | |
| Poor | 323 | 99.7 | 1 | 0.3 | |
| RACD and index case level factors | |||||
| Distance from home of index case | |||||
| At the same house | 203 | 98.1 | 4 | 1.9 | 0.020 |
| <100 m | 926 | 99.8 | 2 | 0.2 | |
| 100–499 m | 319 | 100 | 0 | 0.0 | |
| ≥500 m | 41 | 100 | 0 | 0.0 | |
| Population coverage of RACD | |||||
| <90 % | 429 | 99.1 | 4 | 0.9 | 0.062 |
| ≥90 % | 1060 | 99.8 | 2 | 0.2 | |
| Time from report of index case to RACD | |||||
| At the same day | 45 | 100 | 0 | 0.0 | 0.804 |
| 1–7 days | 1388 | 99.6 | 6 | 0.4 | |
| >7 days | 56 | 100 | 0 | 0.0 | |
| Age category of index case (years) | |||||
| ≤15 | 18 | 100 | 0 | 0.0 | 0.715 |
| 16–30 | 770 | 99.5 | 4 | 0.5 | |
| 30–45 | 655 | 99.7 | 2 | 0.3 | |
| Gender of index case | |||||
| Female | 63 | 100 | 0 | 0.0 | 0.607 |
| Male | 1426 | 99.6 | 6 | 0.4 | |
| Occupation category of index case | |||||
| Not forest-related job | 393 | 99.5 | 2 | 0.5 | 0.658 |
| Forest-related job | 1096 | 99.6 | 4 | 0.4 | |
Results
Enrolment
Of 42 index cases reported in passive surveillance, three were excluded due to residence outside the study area. Of the 39 index cases eligible for case investigation, one was a relapse that occurred 10 weeks after the initial infection and the index case refused case investigation (Fig. 2). The remaining 38 index cases triggered 36 RACD events in 33 villages. One RACD event was conducted to cover three indexes cases that resided in the same household and were reported within 3 days of each other. In total, there were 1638 household members and neighbours (excluding index cases) who resided in the targeted screening area, of whom 1495 (91.3 %) were interviewed and provided blood for malaria testing after providing informed consent. The refusal rate for blood testing was 8.7 % (143/1638) with 81 % of refusals coming from adult men (116/143). Reasons for refusal included: afraid of pain (83), not interested (50), no reason provided (26), and child too young (19). On average, one return visit was required to reach 100 % of villagers. No eligible subjects were missed, likely because targeted households were sensitized by the village midwife, a village leader or a malaria volunteer prior the date of RACD event.
Fig. 2.
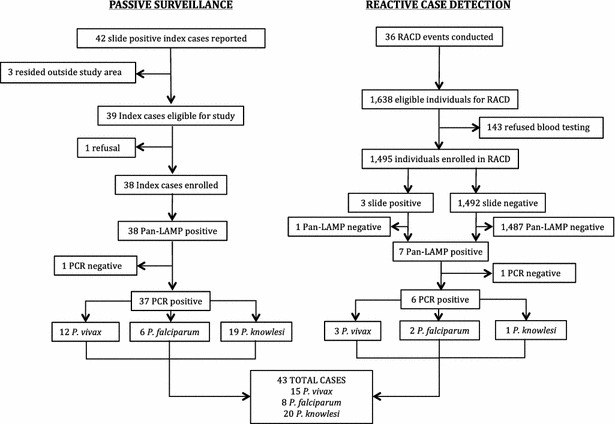
Study recruitment and laboratory testing results 38 index cases were enrolled through passive surveillance and triggered 36 RACD events. One RACD event covered three contemporaneous indexes cases from the same household. In passive surveillance, 37 cases were confirmed by PCR and by RACD, there were six PCR-confirmed cases, resulting in a total of 43 cases. Pan-LAMP Pan-loop-mediated isothermal amplification
Laboratory testing results
Of 42 slide-positive malaria cases reported through passive surveillance, 41 were ultimately confirmed microscopy positive on the second read (16 P. vivax, 20 P. falciparum, two P. knowlesi, and three Plasmodium malariae). Among 38 microscopy-confirmed index cases enrolled in the study, 37 were Pan-LAMP and PCR confirmed and species identification using molecular methods identified 12 P. vivax, six P. falciparum and 19 P. knowlesi infections. In RACD, three of 1495 tested positive by microscopy (one P. vivax and two P. falciparum). After subsequent testing by Pan-LAMP and PCR, a total of six PCR-confirmed malaria cases were identified as three P. vivax, two P. falciparum and one P. knowlesi. Pan-LAMP positive but PCR negative cases included one index case that was identified as P. vivax by microscopy but DBS was collected after treatment, and one microscopy negative case from RACD. Combining passive and active surveillance data, a total of 43 malaria cases were identified, including 15 (34.9 %) P. vivax, eight (18.6 %) P. falciparum and 20 (46.5 %) P. knowlesi (Fig. 2). Of note, P. knowlesi infections were misdiagnosed by microscopy as ten P. falciparum, seven P. vivax, one P. malariae, and two indeterminate). Non-cases for the risk factor analyses included 1489 RACD subjects who were Pan-LAMP or PCR negative. Ten percent of Pan-LAMP negative RACD samples were randomly selected for quality assurance and all were confirmed negative by PCR. Additional details of the laboratory testing results have been reported elsewhere [21].
Characteristics of the overall study population
Most study participants were female (54.7 %) (Table 1). The highest proportion of subjects (31.5 %) fell in the youngest age group (≤15 years), followed by 16–30 years (25.1 %), 31–45 years (24.5 %), and ≥46 years (18.9 %). Most of household heads had secondary school-level education (45.5 %). A quarter of study participants had forest-related jobs: farming (16.4 %), logging (3.2 %), soldier/police (0.5 %), mining (0.3 %), and other forest jobs (5.2 %). Of those reporting a workplace near or in the forest, 71.4 % were required to stay overnight. Overall, bed net usage the night prior was 55.2 % and IRS coverage in the past year was 7.3 %. More than half of study participants (57.8 %) reported living near a water body, and in most, the water body was located within 100 m. More than half of participants (52.3 %) reported living near or in the forest. Most houses (55.6 %) were good quality. More than 95 % of malaria cases occurred in three of the five sub-districts and malaria cases were reported in both the historically high (57.2 %) and low transmission seasons (42.8 %).
Characteristics of RACD events and index cases triggering RACD
Index cases were generally adult males with forest-related jobs. Of RACD events, 96.3 % were conducted within 7 days of the index case report. Among 71 % of RACD events, coverage (participation rate) was at least 90 %. The mean distance of RACD screening events conducted from the index case household was 91 m (range: 0–1897 m). Most individuals screened in RACD (75.9 %) resided within 100 m of the index cases. Forty-one subjects (2.7 %) screened resided more than 500 m from the index case but were included due to there being fewer than five households within 500 m of the index case.
Assessment of risk factors for malaria infection
Table 1 shows the distribution of potential risk factors among malaria-infected versus uninfected subjects analysed using Chi squared or Fisher’s exact test and methods for non-parametric variables to explore the associations. There were significant associations between malaria infection and age category, gender, occupation category, travel, sleeping under a bed net last night, workplace location near or in the forest (including required overnights and distance of workplace to forest for those with a workplace near or in the forest), and reported visits to the forest in the previous month for any reason.
The results of bivariate and best-fit multivariable analysis with household level adjustment for all symptomatic and asymptomatic malaria infection identified in passive or RACD are presented in Table 2. In the final multivariable model, adult age, male gender, workplace near or in the forest requiring overnight stays, and visits to the forest in previous month for any reason were significantly associated with malaria infection. Adults aged 16–45 years had 14.0 times higher odds (95 % CI 2.2–89.6, P = 0.005) of malaria infection compared to the reference group of age ≤15 years. Males had 12.5 times higher odds infection compared to females (95 % CI 3.0–52.1, P = 0.001). Individuals with a workplace location in or near the forest and requiring overnight stays had a 7.9 times higher odds of infection compared to those whose workplace was not in or near the forest (95 % CI 1.6–39.7, P = 0.012). Individuals who visited forest in previous month for any reason had a 5.6 times higher odds of infection compared to those who had not visited the forest (95 % CI 1.3–24.2, P = 0.020).
Assessment of risk factors for Plasmodium falciparum versus Plasmodium vivax versus Plasmodium knowlesi infection
There were eight P. falciparum, 15 P. vivax and 20 P. knowlesi infections. The finding of P. knowlesi was unexpected as only P. falciparum and P. vivax had been reported from Aceh Besar in the past, and in Indonesia, P. knowlesi had only previously been reported from Borneo [43, 44]. As the epidemiology of species-specific infections can vary, a secondary aim of the study was to identify risk factors for infection by specific Plasmodium types. After the finding of P. knowlesi representing almost half of the infections, the local programme was especially interested to understand specific risk factors for P. knowlesi compared to other species and with negative. The sample sizes were too small to justify logistic regression analyses, but characteristics of subjects with different species of infection were compared and the relationships between potential risk factors and P. knowlesi, P. vivax, or P. falciparum infection (compared to non-cases) were explored using Chi squared or Fisher’s exact test or non-parametric methods.
In the comparison of P. knowlesi cases to non-cases, P. vivax cases to non-cases, and P. falciparum cases to non-cases, the findings were overall similar to the primary analysis in that adult age, male gender, forest-related work, travel, overnights in the forest for work, and forest exposure for any reason were associated with each of the infections (data not shown). In the comparison of the potential risk factors between the different species of infection, P. knowlesi cases were more likely to also have forest exposure from residence and other reasons, versus work only (Table 1). Compared to P. knowlesi subjects, those with P. vivax infection or P. falciparum were more likely to report travel (at least one night outside of their village in the previous month but not including the previous week). Infections were more likely in male adults for all species, though the only three malaria cases in females and/or children were due to P. knowlesi and all had forest exposures. The three female P. knowlesi cases included two students (aged 8 and 12 years) and a 32 years old teacher. Two of the female P. knowlesi cases had forest exposures: one reported that her workplace was within 1 km of forest and another had visited her parent who worked at the forest. One child did not live or work in or near the forest, but lived with another P. knowlesi case and there was a captive monkey at the home, thought to be the source of the infection.
Plasmodium falciparum cases and P. knowlesi cases were more likely to have a household head with secondary-level education, while P. vivax cases were more like to come from households with lower education status. In terms of geography, Plasmodium types clustered by sub-district. Plasmodium falciparum cases were most likely in Kuta Cot Glie. Plasmodium vivax cases were most likely detected in Lhoong, and P. knowlesi cases were mostly in Lembah Seulawah. All Plasmodium types were identified by passive surveillance and RACD, however in passive surveillance most infections were due to P. knowlesi (51.4 %), and in RACD, half of secondary cases were asymptomatic P. vivax cases (3/6), with the other asymptomatic case being a P. falciparum case.
Assessment of factors associated with secondary case detection
In the risk factor analysis among subjects screened in RACD (Table 3), the two most notable findings were that compared to non-cases, secondary cases were more likely to have fever (4.3 vs. 0.3 % without fever, P = 0.013) and reside in the same household or within 100 m of the index case (100 vs. 0 % residing ≥100 m, P = 0.02). Among subjects residing in the same households as the index case, 1.9 % (4/207) were infected. The positivity rate dropped beyond the index case house, with 0.2 % (2/928) being infected within 100 m, and none beyond 100 m.
The relationship between secondary infection and a variety of other operational and index case-level factors were assessed. These included population coverage of the RACD event, response time, age, gender, or occupation of the index case, and there were no other significant relationships. There was also no association between high versus low malaria transmission season and finding secondary cases. As for other potential individual level risk factors, findings were similar to those in the overall primary analysis. Compared to 1489 non-cases, the six secondary cases were more likely to be male, report recent travel, be employed in forest-related work, have a workplace in or near the forest, and have visited the forest for any reason in the prior month.
Discussion
The primary risk factors for malaria infection in the low endemic, multi-species area of Aceh Besar District were adult age, male gender and forest exposures, particularly related to forest-related occupation requiring overnight stays. There were some differences in demographic and behavioural factors between the different species, and clustering of species by sub-district of residence. For secondary case detection in RACD, cases were more likely to be febrile and resided within 100 m or in the same household as the index case.
The finding of a higher risk of infection in adult males is consistent with other studies reported from low-endemic areas [3, 15, 45–47]. The variation of age distribution between high- and low-endemic areas is presumably due to the acquisition of immunity after frequent exposure [4] as well as occupational and behavioural factors [46]. In Aceh, forest-based work such as: logging, rubber tapping, mining, and cannabis farming is usually performed by men. Moreover, these jobs require workers to stay overnight in the forest, which was found to be strongly association with malaria infection and affirming the finding from other studies that adult men are at high risk for infection in low-transmission settings due to occupation and behavioural factors.
A secondary aim was to identify risk factors associated with specific Plasmodium types. One strength of this study was the use of molecular testing to classify species. The programme at district level had only been using microscopy and 20 P. knowlesi cases were misdiagnosed as P. falciparum, P. vivax, P. malariae, and indeterminate. Because many of the P. knowlesi cases had not travelled, and due to the known presence of the pig-tailed macaque and Anopheles leucosphyrus [48], a known vector of P. knowlesi, in forested areas of Aceh Besar, local transmission was established. Detailed information about this discovery of P. knowlesi in this area has recently been described [21]. It is likely at that P. knowlesi transmission has been ongoing for some time, but missed by the programme due to the known challenge of P. knowlesi diagnosis by microscopy [49]. The local programme was keen to identify specific risk factors for infection by P. knowlesi in addition to the other Plasmodium types.
Consistent with the overall finding that infection was associated with work related overnights in the forest, all of the P. falciparum cases, and most of the P. vivax and P. knowlesi cases reported occupations that required overnight stays in the forest. However, P. knowlesi cases were more likely to have forest exposure due to residence or other activities and they were less likely to have travelled, suggesting infection acquisition related to non-work exposure as well. Infections were more likely in male adults for all species, though interestingly, the only three malaria cases in females and/or children were due to P. knowlesi and all had forest exposures. Others have reported women and children to typically be at lower risk of P. knowlesi given less forest exposure [50]. Certainly, one limitation of the risk factor assessment was that exposures to macaque monkeys was not assessed because P. knowlesi infections were not anticipated. Finally, the most notable species-specific finding was that the species clustered by sub-district, suggesting further entomological and epidemiological investigation specific to the subdistricts (e.g. a macaque population near Lembah Seulawah, where most of the P. knowlesi cases occurred) is warranted.
In low-endemic areas moving toward elimination, RACD is a standard and widely practiced activity. In the study area, RACD was initiated in 2010. One challenge of RACD is that the activities are resource intensive and often yield few cases [16]. Some studies have looked at factors associated with secondary-case detection and found that secondary cases were more likely to be male [10, 16], live in the same house or close to an index case [10, 15, 51], live in a receptive area [52], have travel history to an endemic area [10], be detected within 7 days of an index case being reported [15], be associated with an index case classified as a local case [15], be under 5 years of age [53], symptomatic [17], and have a history of malaria infection [16, 17]. Although the numbers of secondary cases from this study were limited, the findings that secondary cases were more likely male, have forest-related work that required overnights near or in forest, report recent travel, report fever in the previous 2 weeks, and reside in the same house or within <100 m from the home of the index, were similar to those from other studies. While all secondary cases were found within 100 m of the index case, they were not more likely to have other risk factors that would be associated with local transmission (e.g. lack of travel, close distance to a water body). They shared the same risk factors as index cases including recent travel, forest exposures, and occupations that required overnights in the forest, suggesting that infection was less likely due to local transmission in their village. Given these findings, the low yield of RACD (0.4 %, or 6/1495), the high level of resources required to conduct it, and the possibility that secondary cases might eventually present through passive surveillance anyway, it could be argued that efforts could be better spent directly targeting forest workers rather than just targeting villagers, and the screening radius for RACD in village could be decreased to 100 m, contrary to the WHO recommendation for a 1 to 2-km screening radius in RACD due to the potential flight range of Anopheles mosquitoes [13].
This study was performed to inform local malaria elimination planning. In order to target adult males with forest exposure, the District Health Office Aceh Besar could develop collaborations with other relevant government departments (e.g., forestry, agriculture, transmission, and forest squatter resettlement) and local partners (farm owners, logging site supervisors and farming companies) to engage forest workers and their supervisors in malaria elimination activities. These partners could support education campaigns to promote health-seeking behaviours. Also, although these interventions still need to be rigorously evaluated for P. knowlesi, they could also provide insecticide-treated hammocks or tarpaulins or ITNs [54, 55] which are often not available at the workplace because distribution by the government usually takes place at the residence and these products are not otherwise available for purchase in markets. Finally, with work requiring overnight stays in a forest location outside of the village or sub-district of residence being a major risk factor for infection, migration and mobility surveillance system linked to the existing malaria surveillance system could be developed for use across sub-district, districts and provinces.
The main limitation of this study was the small sample size, which limited the ability to rigorously analyse risk factors for species-specific infection and secondary case detection, and in the primary analysis, led to wide confidence intervals in the OR estimates. Small sample sizes are a common challenge for studies in low transmission or elimination settings. In the future, better anticipation of decline in cases could prompt inclusion of neighbouring districts to improve sample size, which would also facilitate understanding of human movement across districts and its impact on malaria transmission. Another potential limitation of this study was the cross-sectional design, which can only identify associations and not prove causality. Moreover, there may be unmeasured factors confounding the association of observed independent variables with the outcome variables.
Cohort studies are an ideal study design to provide evidence of relationship between exposure and outcome or disease before the disease occurred, yet these studies are expensive, time consuming, require large sample sizes, and have risk of loss to follow-up or withdrawal of participants. Case–control studies are useful for assessing rare condition, but there is the challenge of identifying the appropriate control population and potential for recall bias. Despite their limitations, cross-sectional surveys enable analysis of data that includes point or cumulative prevalence of disease, and they are often simple, inexpensive and rapid to perform [56]. Passive and active surveillance data are easily available in most settings, and uninfected subjects screened serve as a convenient control group for cross-sectional analyses.
The study had several additional strengths. Firstly, highly sensitive and specific molecular methods were utilized to confirm malaria infection and species identification. Second, this study is one of few that looks at risk factors for P. knowlesi [50, 57], which has only recently been discovered in Indonesia outside Borneo [21]. Additionally, it is the first undertaking in Indonesia, and among few studies from any setting, that explores the factors associated with secondary case detection in RACD [10, 15–17].
Conclusion
Risk factor analyses in low-endemic areas aiming for malaria elimination are essential to inform targeting of interventions. The methodology and approach used in this study can be easily adapted to other settings with similar endemicity and passive and active surveillance programs in place. This study provided useful information on risk factors for malaria in Aceh Besar District, and will help to inform malaria elimination planning in Aceh Besar District and Indonesia at large. The high burden of P. knowlesi warrants further investigation into its epidemiology and specific risk factors in this setting, and highlights a new challenge for malaria elimination in endemic areas.
Authors’ contributions
HH, CC, FNC and MSH led the conception and study design. RG, MW and PB contributed to the study design. HH, CC, IZ, FNC, MSH, BZ, YKT and BG supported study implementation, data collection and laboratory testing. HH, IZ, BZ and CC performed data cleaning. MSH performed exploratory data analyses and HH finalized the analyses. HH and MSH wrote the manuscript. All authors read and approved the final manuscript.
Acknowledgements
The authors are grateful to Asik Surya and Elvieda Sariwati from the National Malaria Control Programme of Indonesia, as well as the chiefs and officers at the Aceh Province Health Office, Aceh Besar District Health Office, and Communicable Disease Control Malaria Programme for their support and collaboration. We are grateful to the Provincial Health Laboratory Aceh team, and staff from the five study primary health centres for support in study implementation. We thank William Hawley and Maria Endang Sumiwi from UNICEF Indonesia for support and guidance, Asen Mwandemele for support in developing the tablet-based questionnaire, Mi-suk Kang Dufour for statistical input, and Rintis Noviyanti, Iveth Gonzalez, Alanna Schwartz, Maxwell Murphy, Nicholas M. Anstey, and Jutta Marfut for laboratory inputs.
Competing interests
The authors declare that they have no competing interests. The finding and interpretations presented represent those of the authors and not any organization.
Availability of data and materials
The datasets supporting the conclusions of this article are available and can easily be made available on request, when required.
Consent for publication
Not applicable. There is no presentation of confidential or identifiable data in this manuscript.
Ethics approval and consent to participate
This study was reviewed and approved by the Committee on Health Research Ethics of Indonesia National Institute of Health Research and Development (NIHRD), the Committee on Human Research at UCSF and the School of Public Health Research Ethics Committee at the University of Queensland. Written informed consent was obtained from all subjects. For children under the age of 18, informed consent and the questionnaire were administered to a parent or guardian. Minor assent was obtained from subjects 12–15 years of age.
Funding
The primary study was funded by the Bill and Melinda Gates Foundation through a grant to the UCSF Global Health Group Malaria Elimination Initiative (A121292). MSH additionally is funded by the National Institutes of Health/National Institute of Allergy and Infectious Diseases (AI101012), Burroughs Wellcome Fund/American Society of Tropical Medicine and Hygiene (A120079), and the Horchow Family Fund Scholarship Award (5300375400). Significant in-kind funding was provided from the District Health Office Aceh Besar, Aceh Provincial Health Office, and UNICEF Aceh Field Office of malaria programme for field support and personnel. Co-funding for meetings and capacity building activities was provided from the Asia Pacific Malaria Elimination Network (APMEN) through a grant from the Department of Foreign Affairs Australian Aid Programme.
Abbreviations
- AIC
Akaike’s information criteria (AIC)
- API
annual parasite incidence
- DBS
dried blood spot
- DNA
deoxyribonucleic acid
- IRS
indoor residual spray
- ITN
insecticide-treated net
- LAMP
loop-mediated isothermal amplification
- LLIN
long-lasting, insecticidal nets
- LRT
likelihood ratio test
- PCR
polymerase chain reaction
- PHC
primary health centre
- QA
quality assurance
- RACD
reactive case detection
- WBC
white blood cells
- WHO
World Health Organization
Contributor Information
Herdiana Herdiana, Email: hherdiana@gmail.com.
Chris Cotter, Email: Chris.Cotter@ucsf.edu.
Farah N. Coutrier, Email: farah@eijkman.go.id
Iska Zarlinda, Email: iska.zarlinda2013@gmail.com.
Brittany W. Zelman, Email: Brittany.Zelman@ucsf.edu
Yusrifar Kharisma Tirta, Email: r.yusrifar@gmail.com.
Bryan Greenhouse, Email: bryan.greenhouse@ucsf.edu.
Roly D. Gosling, Email: Roly.Gosling@ucsf.edu
Peter Baker, Email: p.baker1@uq.edu.au.
Maxine Whittaker, Email: maxine.whittaker@jcu.edu.au.
Michelle S. Hsiang, Email: Michelle.Hsiang@utsouthwestern.edu
References
- 1.WHO. Global technical strategy for malaria 2016–2030. Geneva: World Health Organization; 2015. http://www.who.int/malaria/publications/atoz/9789241596084/en/. Accessed 9 Sept 2016.
- 2.APLMA. Malaria elimination roadmap. Philippines: Asia Pacific Leaders Malaria Alliance; 2015. http://www.aplma.org/upload/resource/Roadmap/APLMA_Roadmap_final_EAS_2015.pdf. Accessed 9 Sept 2016.
- 3.Cotter C, Sturrock HJW, Hsiang MS, Liu J, Phillips AA, Hwang J, et al. The changing epidemiology of malaria elimination: new strategies for new challenges. Lancet. 2013;382:900–911. doi: 10.1016/S0140-6736(13)60310-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Snow RW, Marsh K. New insights into the epidemiology of malaria relevant for disease control. Br Med Bull. 1998;54:293–309. doi: 10.1093/oxfordjournals.bmb.a011689. [DOI] [PubMed] [Google Scholar]
- 5.van Eijk AM, Hill J, Noor AM, Snow RW, ter Kuile FO. Prevalence of malaria infection in pregnant women compared with children for tracking malaria transmission in sub-Saharan Africa: a systematic review and meta-analysis. Lancet Glob Health. 2015;3:e617–e628. doi: 10.1016/S2214-109X(15)00049-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Worrall E, Basu S, Hanson K. Is malaria a disease of poverty? A review of the literature. Trop Med Int Health. 2005;10:1047–1059. doi: 10.1111/j.1365-3156.2005.01476.x. [DOI] [PubMed] [Google Scholar]
- 7.Zoungrana A, Chou Y-J, Pu C. Socioeconomic and environment determinants as predictors of severe malaria in children under 5 years of age admitted in two hospitals in Koudougou district, Burkina Faso: a cross sectional study. Acta Trop. 2014;139:109–114. doi: 10.1016/j.actatropica.2014.07.011. [DOI] [PubMed] [Google Scholar]
- 8.Liu JX, Bousema T, Zelman B, Gesase S, Hashim R, Maxwell C, et al. Is housing quality associated with malaria incidence among young children and mosquito vector numbers? Evidence from Korogwe, Tanzania. PLoS One. 2014;9:e87358. doi: 10.1371/journal.pone.0087358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hawley WA, Phillips-Howard PA, ter Kuile FO, Terlouw DJ, Vulule JM, Ombok M, et al. Community-wide effects of permethrin-treated bed nets on child mortality and morbidity in western Kenya. Am J Trop Med Hyg. 2003;68(4 Suppl):121–127. [PubMed] [Google Scholar]
- 10.Littrell M, Sow GD, Ngom A, Ba M, Mboup BM, Dieye Y, et al. Case investigation and reactive case detection for malaria elimination in northern Senegal. Malar J. 2013;12:331. doi: 10.1186/1475-2875-12-331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu Y, Hsiang MS, Zhou H, Wang W, Cao Y, Gosling RD, et al. Malaria in overseas labourers returning to China: an analysis of imported malaria in Jiangsu Province, 2001–2011. Malar J. 2014;13:29. doi: 10.1186/1475-2875-13-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hsiang MS, Hwang J, Kunene S, Drakeley C, Kandula D, Novotny J, et al. Surveillance for malaria elimination in Swaziland: a national cross-sectional study using pooled PCR and serology. PLoS One. 2012;7:e29550. doi: 10.1371/journal.pone.0029550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.WHO. Disease surveillance for malaria elimination: an operational manual. Geneva: World Health Organization; 2012. http://www.who.int/malaria/publications/atoz/9789241503334/en/. Accessed 9 Sept 2016.
- 14.Gueye CS, Sanders KC, Galappaththy GNL, Rundi C, Tobgay T, Sovannaroth S, et al. Active case detection for malaria elimination: a survey among Asia Pacific countries. Malar J. 2013;12:358. doi: 10.1186/1475-2875-12-358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sturrock HJW, Novotny JM, Kunene S, Dlamini S, Zulu Z, Cohen JM, et al. Reactive case detection for malaria elimination: real-life experience from an ongoing program in Swaziland. PLoS One. 2013;8:e63830. doi: 10.1371/journal.pone.0063830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van Eijk AM, Ramanathapuram L, Sutton PL, Kanagaraj D, Priya GSL, Ravishankaran S, et al. What is the value of reactive case detection in malaria control? A case-study in India and a systematic review. Malar J. 2016;15:67. doi: 10.1186/s12936-016-1120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hustedt J, Canavati SE, Rang C, Ashton RA, Khim N, Berne L, et al. Reactive case-detection of malaria in Pailin Province, Western Cambodia: lessons from a year-long evaluation in a pre-elimination setting. Malar J. 2016;15:132. doi: 10.1186/s12936-016-1191-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.WHO . World malaria report 2009. Geneva: World Health Organization; 2009. [Google Scholar]
- 19.WHO . World malaria report 2015. Geneva: World Health Organization; 2015. [Google Scholar]
- 20.Surya A. Indonesia gap analysis. In: Asia Pacific malaria elimination network advocacy workshop, Bangkok, Thailand; 2014.
- 21.Coutrier F, Cotter C, Tirta Y, Schwartz A, Zarlinda I, Basri H, et al. Serial molecular identification to confirm the presence of Plasmodium knowlesi in Indonesia. In: Poster session presented at: 64th annual meeting of the American society for tropical medicine and hygiene; 2015 Oct 25–29; Philadelphia.
- 22.BPS. Aceh Besar dalam angka 2015 (Aceh Besar in figure 2015). Aceh Besar: Badan Pusat Statistik (Central Bureau of Statistics); 2015.
- 23.BPS. Aceh Besar dalam angka 2012 (Aceh Besar in figure 2012). Aceh Besar: Badan Pusat Statistik (Central Bureau of Statistics); 2012.
- 24.Dinkes Aceh Besar. Profil kesehatan Kabupaten Aceh Besar tahun 2006 (District health profile of Aceh Besar 2006). Kota Jantho: Dinas Kesehatan Kabupaten Aceh Besar (District Health Office of Aceh Besar); 2006.
- 25.BPS. Aceh Besar dalam angka 2013 (Aceh Besar in figure 2013). Aceh Besar: Badan Pusat Statistik (Central Bureau of Statistics); 2013.
- 26.Dinkes Provinsi Aceh. Panduan lapangan penyelidikan epidemiologi malaria bagi petugas puskesmas dan dinas kesehatan kabupaten/kota (Field manual of epidemiology investigation of malaria for primary health center and district health office staff). Aceh: Dinas Kesehatan Provinsi Aceh (Provincial Health Office of Aceh); 2012.
- 27.Balitbangkes. Riset kesehatan dasar 2013 (Basic health research 2013). Jakarta: Badan Penelitian dan Pengembangan Kesehatan Kementerian Kesehatan RI (National Institute of Health and Research Development); 2013.
- 28.Menteri Kesehatan RI. Peraturan tatalaksana malaria (Management malaria case regulation). In: Permenkes No 5/MENKES/Per/I/2013 (Indonesia KKR editor, vol. Nomor 5 Tahun 2013): Menteri Hukum dan Hak Asasi Manusia (Minister of Law and Human Rights); 2013.
- 29.Ho W. Basic malaria microscopy. Part 1: Learner’s guide. Geneva: World Health Organization; 2010. [Google Scholar]
- 30.Plowe CV, Djimde A, Bouare M, Doumbo O, Wellems TE. Pyrimethamine and proguanil resistance-conferring mutations in Plasmodium falciparum dihydrofolate reductase: polymerase chain reaction methods for surveillance in Africa. Am J Trop Med Hyg. 1995;52:565–568. doi: 10.4269/ajtmh.1995.52.565. [DOI] [PubMed] [Google Scholar]
- 31.Aydin-Schmidt B, Xu W, Gonzalez IJ, Polley SD, Bell D, Shakely D, et al. Loop mediated isothermal amplification (LAMP) accurately detects malaria DNA from filter paper blood samples of low density parasitaemias. PLoS One. 2014;9:e103905. doi: 10.1371/journal.pone.0103905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hopkins H, Gonzalez IJ, Polley SD, Angutoko P, Ategeka J, Asiimwe C, et al. Highly sensitive detection of malaria parasitemia in a malaria-endemic setting: performance of a new loop-mediated isothermal amplification kit in a remote clinic in Uganda. J Infect Dis. 2013;208:645–652. doi: 10.1093/infdis/jit184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Steenkeste N, Rogers WO, Okell L, Jeanne I, Incardona S, Duval L, et al. Sub-microscopic malaria cases and mixed malaria infection in a remote area of high malaria endemicity in Rattanakiri province, Cambodia: implication for malaria elimination. Malar J. 2010;9:108. doi: 10.1186/1475-2875-9-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hsiang MS, Lin M, Dokomajilar C, Kemere J, Pilcher CD, Dorsey G, et al. PCR-based pooling of dried blood spots for detection of malaria parasites: optimization and application to a cohort of Ugandan children. J Clin Microbiol. 2010;48:3539–3543. doi: 10.1128/JCM.00522-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schwartz A, Baidjoe A, Rosenthal PJ, Dorsey G, Bousema T, Greenhouse B. The effect of storage and extraction methods on amplification of Plasmodium falciparum DNA from dried blood spots. Am J Trop Med Hyg. 2015;92:922–925. doi: 10.4269/ajtmh.14-0602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Snounou G, Viriyakosol S, Jarra W, Thaithong S, Brown KN. Identification of the four human malaria parasite species in field samples by the polymerase chain reaction and detection of a high prevalence of mixed infections. Mol Biochem Parasitol. 1993;58:283–292. doi: 10.1016/0166-6851(93)90050-8. [DOI] [PubMed] [Google Scholar]
- 37.Singh B, Bobogare A, Cox-Singh J, Snounou G, Abdullah MS, Rahman HA. A genus- and species-specific nested polymerase chain reaction malaria detection assay for epidemiologic studies. Am J Trop Med Hyg. 1999;60:687–692. doi: 10.4269/ajtmh.1999.60.687. [DOI] [PubMed] [Google Scholar]
- 38.Imwong M, Tanomsing N, Pukrittayakamee S, Day NPJ, White NJ, Snounou G. Spurious amplification of a Plasmodium vivax small-subunit RNA gene by use of primers currently used to detect P. knowlesi. J Clin Microbiol. 2009;47:4173–4175. doi: 10.1128/JCM.00811-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hosmer Jr DW, Lemeshow S, Sturdivant RX. Model-building strategies and methods for logistic regression. In: Applied logistic regression. New York: Wiley; 2013. p. 89–151. doi: 10.1002/9781118548387.ch4.
- 40.Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code Biol Med. 2008;3:17. doi: 10.1186/1751-0473-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stoica P, Selen Y, Li J. On information criteria and the generalized likelihood ratio test of model order selection. IEEE Signal Process Lett. 2004;11:794–797. doi: 10.1109/LSP.2004.835468. [DOI] [Google Scholar]
- 42.Howe LD, Hargreaves JR, Huttly SRA. Issues in the construction of wealth indices for the measurement of socio-economic position in low-income countries. Emerg Themes Epidemiol. 2008;5:3. doi: 10.1186/1742-7622-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Figtree M, Lee R, Bain L, Kennedy T, Mackertich S, Urban M, et al. Plasmodium knowlesi in human, Indonesian Borneo. Emerg Infect Dis. 2010;16:672–674. doi: 10.3201/eid1604.091624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sulistyaningsih E, Fitri LE, Löscher T, Berens-Riha N. Diagnostic difficulties with Plasmodium knowlesi infection in humans. Emerg Infect Dis. 2010;16:1033–1034. doi: 10.3201/eid1606.100022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lansang MAD, Belizario VY, Bustos MDG, Saul A, Aguirre A. Risk factors for infection with malaria in a low endemic community in Bataan, the Philippines. Acta Trop. 1997;63:257–265. doi: 10.1016/S0001-706X(96)00625-0. [DOI] [PubMed] [Google Scholar]
- 46.Kleinschmidt I, Sharp B. Patterns in age-specific malaria incidence in a population exposed to low levels of malaria transmission intensity. Trop Med Int Health. 2001;6:986–991. doi: 10.1046/j.1365-3156.2001.00817.x. [DOI] [PubMed] [Google Scholar]
- 47.Monteiro TH, Chaves Tdo S, Matos HJ, Sofffiatti NF, Guimarães RJ, Guimarães LH, et al. Basic sanitation, socioeconomic conditions, and degree of risk for the presence and maintenance of malaria in a low-transmission area in the Brazilian Amazon. Rev Soc Bras Med Trop. 2015;48:573–579. doi: 10.1590/0037-8682-0118-2015. [DOI] [PubMed] [Google Scholar]
- 48.Barbara KA, Sukowati S, Rusmiarto S, Susapto D, Bangs MJ, Kinzer MH. Survey of Anopheles mosquitoes (Diptera: Culicidae) in West Sumba District, Indonesia. Southeast Asian J Trop Med Public Health. 2011;42:71–82. [PubMed] [Google Scholar]
- 49.Barber BE, William T, Grigg MJ, Yeo TW, Anstey NM. Limitations of microscopy to differentiate Plasmodium species in a region co-endemic for Plasmodium falciparum, Plasmodium vivax and Plasmodium knowlesi. Malar J. 2013;12:8. doi: 10.1186/1475-2875-12-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Barber BE, William T, Dhararaj P, Anderios F, Grigg MJ, Yeo TW, et al. Epidemiology of Plasmodium knowlesi malaria in north-east Sabah, Malaysia: family clusters and wide age distribution. Malar J. 2012;11:401. doi: 10.1186/1475-2875-11-401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Stresman GH, Kamanga A, Moono P, Hamapumbu H, Mharakurwa S, Kobayashi T, et al. A method of active case detection to target reservoirs of asymptomatic malaria and gametocyte carriers in a rural area in Southern Province, Zambia. Malar J. 2010;9:265. doi: 10.1186/1475-2875-9-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rulisa S, Kateera F, Bizimana JP, Agaba S, Dukuzumuremyi J, Baas L, et al. Malaria prevalence, spatial clustering and risk factors in a low endemic area of Eastern Rwanda: a cross sectional study. PLoS One. 2013;8:e69443. doi: 10.1371/journal.pone.0069443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pinchoff J, Henostroza G, Carter BS, Roberts ST, Hatwiinda S, Hamainza B, et al. Spatial patterns of incident malaria cases and their household contacts in a single clinic catchment area of Chongwe District, Zambia. Malar J. 2015;14:305. doi: 10.1186/s12936-015-0793-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sanders KC, Rundi C, Jelip J, Rashman Y, Smith Gueye C, Gosling RD. Eliminating malaria in Malaysia: the role of partnerships between the public and commercial sectors in Sabah. Malar J. 2014;13:24. doi: 10.1186/1475-2875-13-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Guyant P, Canavati SE, Chea N, Ly P, Whittaker MA, Roca-Feltrer A, et al. Malaria and the mobile and migrant population in Cambodia: a population movement framework to inform strategies for malaria control and elimination. Malar J. 2015;14:252. doi: 10.1186/s12936-015-0773-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Webb P, Bain C. Essential epidemiology: an introduction for students and health professionals. Leiden: Cambridge University Press; 2011. [Google Scholar]
- 57.Grigg MJ, William T, Drakeley CJ, Jelip J, von Seidlein L, Barber BE, et al. Factors that are associated with the risk of acquiring Plasmodium knowlesi malaria in Sabah, Malaysia: a case-control study protocol. BMJ Open. 2014;4:e006004. doi: 10.1136/bmjopen-2014-006004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets supporting the conclusions of this article are available and can easily be made available on request, when required.


