Abstract
Study Design: Prospective cohort study.
Objectives: Comparison of the classification performance between the worksheet revisions of 2011 and 2013 of the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI).
Settings: Ongoing ISNCSCI instructional courses of the European Multicenter Study on Human Spinal Cord Injury (EMSCI). For quality control all participants were requested to classify five ISNCSCI cases directly before (pre-test) and after (post-test) the workshop.
Participants: One hundred twenty-five clinicians working in 22 SCI centers attended the instructional course between November 2011 and March 2015. Seventy-two clinicians completed the post-test with the 2011 revision of the worksheet and 53 with the 2013 revision.
Interventions: Not applicable.
Outcome Measures: The clinicians’ classification performance assessed by the percentage of correctly determined motor levels (ML) and sensory levels, neurological levels of injury (NLI), ASIA Impairment Scales and zones of partial preservations.
Results: While no group differences were found in the pre-tests, the overall performance (rev2011: 92.2% ± 6.7%, rev2013: 94.3% ± 7.7%; P = 0.010), the percentage of correct MLs (83.2% ± 14.5% vs. 88.1% ± 15.3%; P = 0.046) and NLIs (86.1% ± 16.7% vs. 90.9% ± 18.6%; P = 0.043) improved significantly in the post-tests. Detailed ML analysis revealed the largest benefit of the 2013 revision (50.0% vs. 67.0%) in a case with a high cervical injury (NLI C2).
Conclusion: The results from the EMSCI ISNCSCI post-tests show a significantly better classification performance using the revised 2013 worksheet presumably due to the body-side based grouping of myotomes and dermatomes and their correct horizontal alignment. Even with these proven advantages of the new layout, the correct determination of MLs in the segments C2–C4 remains difficult.
Keywords: International standards for neurological classification of spinal cord injury, ISNCSCI, Worksheet, Classification performance, Motor levels
Introduction
The International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI)1 published by the American Spinal Injury Association (ASIA) is a well-established2,3 international communication tool for researchers and clinicians to quantify the neurological impairment resulting from a spinal cord injury (SCI). It is occasionally refined4–7 by ASIA's International Standards Committee for improvement of its quality and consistency. In February of 2013, a modified worksheet was made available,4 with a new graphical layout of the boxes for the motor and sensory scores including light touch appreciation and pin prick discrimination. In contrast to the examination modality (motor and sensory) based grouping in the prior revision (2011) of the worksheet (Fig. 1A), the examination modalities were now grouped according to the body side (Fig. 1B). Body sides on the worksheet were configured from the patient's perspective analog to many other diagnosis processes in medicine. In addition, the myotomes and dermatomes were graphically aligned in the respective row by assigned levels.
Figure 1. ISNCSCI worksheet layouts.
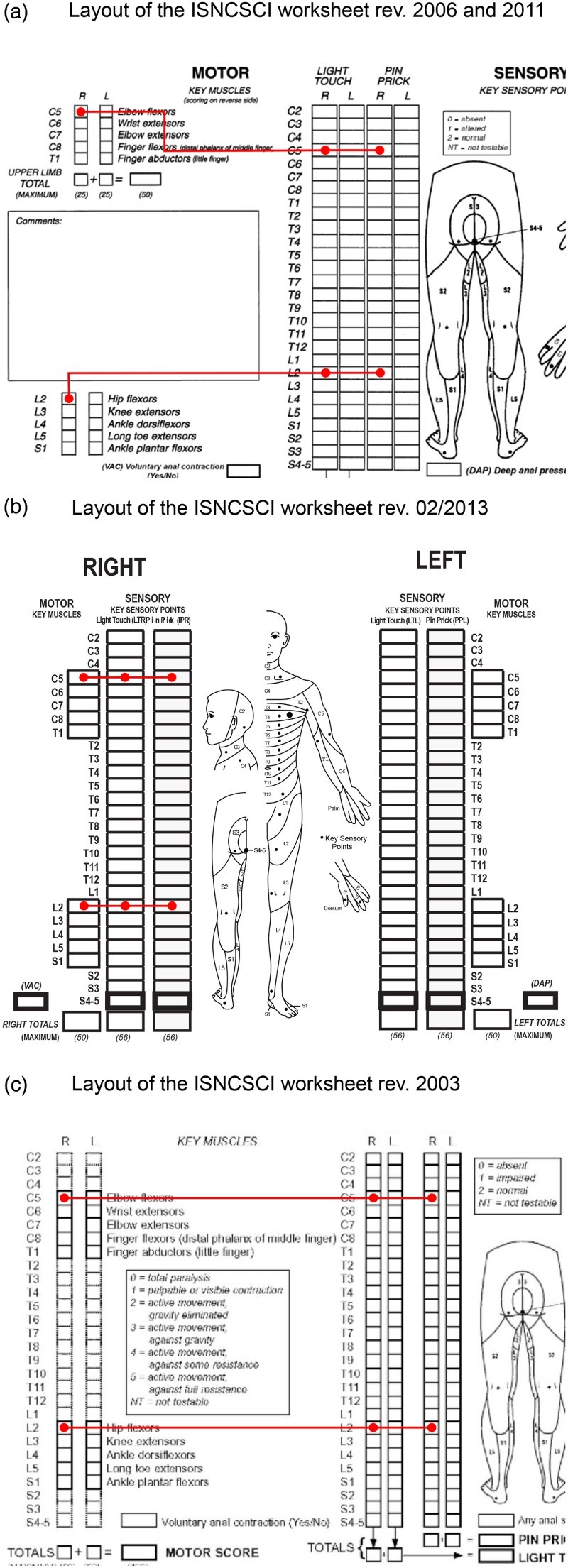
Layouts and alignments of the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) worksheet layouts 2006/2011 (A), revision 2013 (B) and revision 2003 (C). Distances between myotomes and dermatomes and their horizontal alignment are visualized by the angled red lines for the spinal segments C5 and L2
Determination of motor levels (ML) and classification of the ASIA Impairment Scale (AIS) are the most difficult classification tasks in ISNCSCI.8–10 A major factor in the difficulty in ML determination is explained by the fact that motor testing is only performed in 10 key myotomes of the arms and legs. Since there are 28 dermatomes tested, for all other segments (cervical C2–C4, thoracic T2-L1 and sacral S2–S5) the ML defers to the sensory level (SL) if testable motor function rostral to this level is graded as intact as well.11 In order to apply this rule correctly, the first step in ML determination is to look at the sensory scores of the segments C2–C4. This concept seems to be difficult to communicate.9 Among others, the large spatial distance (indicated by circled start and end markers of the red lines in Fig. 1) between myotomes and dermatomes on the 2011 worksheet (and prior) and the horizontal misalignment (as indicated by the angled red lines with the circled start and end markers in Fig. 1A) of myotomes and dermatomes of the same spinal segment were assumed as main reasons for the high misclassification rate of ML in segments without myotomes to test. This issue was addressed by the 2013 revision of the worksheet. We hypothesized that the new graphical layout of the 2013 ISNCSCI worksheet would increase the classification performance, especially the correct determination of MLs and NLI. The aim of this study was to verify this hypothesis by comparing the results of posts-tests of the ongoing ISNCSCI instructional courses of the European Multicenter Study on Human Spinal Cord Injury (EMSCI - http://emsci.org),12 which were based until April 2013 on the 2011 worksheet and from November 2013 utilizing the 2013 revised ISNCSCI worksheets. The presented study was conducted as a part of the ongoing quality management system (ISO 9001:2008) initiative of EMSCI network since 2010.
Materials and methods
To compare both revisions of the worksheet from 2011 and 2013, the post-test classification performances of participants of the ongoing ISNCSCI instructional courses for the EMSCI network were used. ISNCSCI instructional courses are conducted two to three times per year, either in German or in English. The EMSCI study is approved (S-188/2003) by the ethics commission of the medical faculty of the Heidelberg University. The pre- and post-test setup is part of the ongoing quality management system. Experienced ISNCSCI examiners and classification professionals are teaching up to 12 attendees per course. The scope of the course is to teach the theory and practice of ISNCSCI. It is divided into two parts: a seminar for gaining theoretical and practical experience in performing the clinical examination (∼9 hours), and a seminar to impart the knowledge of the ISNCSCI classification rules (∼4 hours). The first part comprises presentation modules on the sensory examination, the manual muscle test and the anorectal examination, followed by hands-on training sessions in able-bodied subjects and in-house patients with SCI in small groups. The second part begins with a presentation on the theory of ISNCSCI classification rules, followed by discussions on the classification of previously examined patients. Finally, Kirshblum's collection of difficult cases13 are discussed and solved interactively.
The presentation of the theory of the ISNCSCI classification rules contains three to four slides showing the evolution of the ISNCSCI worksheet from the 2001 revision to the revision that was most recently published at the time of course conduction. The worksheets of each revision have been introduced regarding their layout, and the changes to its predecessors and the rationale for the modifications. By the time of the introduction of the 2013 worksheet a slide was added to the presentation showing the new front and back side. Similar to the introduction of the older worksheets the rationale for the new layout is briefly discussed during the presentation.
To evaluate the efficacy of the instructional course, all participants are asked to classify five ISNCSCI cases before (pre-test) and the same cases after the instructional course (post-test). Specifically, MLs and SLs, the neurological level of injury (NLI), the AIS and the zones of partial preservation (ZPP) have to be determined in a selection of real cases. These were carefully selected from the EMSCI database to reflect different kinds of classification challenges. Additional details on the instructional course setup and the ISNCSCI cases for pre- and post-testing are published elsewhere.9 The cases were printed on the ISNCSCI worksheet available at the time the instructional courses were conducted. Courses held after May 2013 utilized the 2013 revised form. Primary outcomes measures included the differences in overall classification performance assessed by the percentage of correctly determined afore-mentioned ISNCSCI variables between the group using the revision 2011 (group: rev2011) worksheet and the group using the revision of 2013 (group: rev2013).
Two-sided Mann–Whitney U tests (ordinal variables) and Fisher's exact tests (categorical variables) were used to compare both groups. The significance level was set to α = 0.05. All descriptive and confirmatory statistics were performed with Statistica 9.1 (StatSoft Inc., Tulsa, OK, USA).
Results
Overall 125 clinicians working in 22 SCI centers were trained in 11 workshops during the study period from November 2011 to March 2015. Of these, 72 participants (6 workshops) completed the pre- and post-tests with the 2011 revision worksheet (group rev2011) and 53 participants (5 workshops) were trained using the 2013 layout (group rev2013). Table 1 summarizes the characteristics and the results of both groups. No significant differences were found in group characteristics. Most of the attendees were physicians (rev2011: 54.72%, rev2013: 58.33%) and physical therapists (37.44% versus 30.56%) and had less than one year experience in SCI medicine (39.44% versus 48.08%). No significant differences between the groups were found in the pre-tests. The pre- and post-test comparison over both groups revealed highly significant improvements from 57.55% ± 28.83% to 93.10% ± 7.17% (P < 0.001). The greatest differences (Supplemental Table 1) between pre- and post-test were found in the ML (from 31.2% to 85.3%), NLI (from 49.9% to 88.2%) and AIS (from 48.5% to 86.1%).
Supplemental Table 1.
Overall Pre-test and post-test results of the ISNCSCI instructional course attendees not grouped by the worksheet revisions 2011 and 2013.
| Pre-Test classification performance | Post-Test classification performance | Difference between Post-Test and Pre-Test | |
|---|---|---|---|
| ASIA Impairment Scale | 48.48 % | 86.08% | 37.60% |
| Completeness | 81.28% | 98.40% | 17.12% |
| Neurological level of injury | 49.92% | 88.16% | 38.24% |
| Sensory levels | 65.68% | 97.92% | 32.24% |
| Motor levels | 31.20% | 85.25% | 54.05% |
| Sensory ZPPs | 62,96% | 95,44% | 32.48% |
| Motor ZPPs | 63,04% | 94.64% | 31.60% |
| Overall | 57.55% | 93,10% | 35.55% |
Abbreviations: N/A, not applicable; ASIA, American Spinal Injury Association; SCI, Spinal Cord Injury; ZPP, Zone of partial preservation; ISNCSCI, International Standards for Neurological Classification of Spinal Cord Injury
Table 1.
Basic group characteristics, pre-test and post-test results of the ISNCSCI instructional course attendees grouped by the worksheet revisions 2011 and 2013
| 2011 Worksheet | 2013 Revised worksheet | P-Value | |
|---|---|---|---|
| Characteristics | |||
| Participants | 72 | 53 | N/A |
| Workshops | 6 | 5 | N/A |
| Language | 34.72% English | 35.85% English | 0.896a |
| 65.28% German | 64.15% German | ||
| Profession | 54.72% physician | 58.33% physician | 0.829a |
| 37.74% physical therapist | 30.56% physical therapist | ||
| 03.77% other | 05.56% other | ||
| 03.77% occupational therapist | 04.17% occupational therapist | ||
| 01.39% nurse | |||
| Experience in SCI medicine | 39.44% < 1 year | 48.08% < 1 year | 0.605a |
| 26.76% 1–5 years | 26.92% 1–5 years | ||
| 11.27% 6–10 years | 11.54% 6–10 years | ||
| 22.54% >10 years | 13.46% >10 years | ||
| Pre Test Results (percentage correct answers; mean ± standard deviation) | |||
| ASIA Impairment Scale | 49.44% ± 29.64% | 47.20% ± 31.66% | 0.798b |
| Completeness | 82.50% ± 31.83% | 79.62% ± 32.70% | 0.522b |
| Neurological level of injury | 50.00% ± 33.74% | 49.81% ± 33.19% | 0.958b |
| Sensory levels | 63.19% ± 35.69% | 69.06% ± 39.39% | 0.602b |
| Motor levels | 31.39% ± 28.89% | 30.94% ± 28.51% | 0.871b |
| Sensory ZPPs | 60.97% ± 34.89% | 65.66% ± 34.05% | 0.495b |
| Motor ZPPs | 60.97% ± 33,07% | 65.85% ± 35.49% | 0.345b |
| Overall | 56.50% ± 22.89% | 58.98% ± 22.89% | 0.500b |
| Post Test Results (percentage correct answers mean ± standard deviation) | |||
| ASIA Impairment Scale | 86.11% ± 14.49% | 86.03% ± 15.48% | 0.935b |
| Completeness | 98.33% ± 05.57% | 98.49% ± 07.70% | 0.689b |
| Neurological level of injury | 86.11% ± 16.66% | 90.94% ± 18.63% | 0.043b |
| Sensory levels | 97.92% ± 06.04% | 97.92% ± 09.89% | 0.586b |
| Motor levels | 83.19% ± 14.53% | 88.11% ± 15.32% | 0.046b |
| Sensory ZPPs | 94.44% ± 10,33% | 96.79% ± 08.03% | 0.290b |
| Motor ZPPs | 93.33% ± 11.13% | 96.42% ± 08.57% | 0.223b |
| Overall | 92.22% ± 06.65% | 94.30% ± 07.73% | 0.010b |
Abbreviations: N/A, not applicable; ASIA, American Spinal Injury Association; SCI, Spinal Cord Injury; ZPP, Zone of partial preservation; ISNCSCI, International Standards for Neurological Classification of Spinal Cord Injury
a Fisher's exact test
b Mann–Whitney U test
In post-tests (Supplemental Figure 1) significant group differences were found in the overall performance (rev2011: 92.22% ± 6.65%, rev2013: 94.30% ± 7.73%; P = 0.010), and the percentage of correctly determined MLs (83.19% ± 14.53% versus 88.11% ± 15.32%; P = 0.046) and NLIs (86.11% ± 16.66% versus 90.94% ± 18.63%; P = 0.043). Motor and sensory ZPP performance was better (although not significantly) in the group that utilized the 2013 worksheet (Supplemental Fig. 1).
Detailed motor level analysis
A more detailed analysis of the ML determinations is shown in Figure 2. Significant differences between worksheet revisions were found for the ISNCSCI post-test cases 1 and 5 (Fig. 2A). Case 1 (Fig. 2B) represents a high cervical lesion with an NLI of C2 because of the impairment of pin prick sensation in the C3 dermatome. Accordingly, the motor level defers to the sensory level and has to be classified as C2, although myotomes C5 and C6 are graded as intact. Group rev2011 determined 50% of the ML correctly, whereas group rev2013, using the 2013 revised worksheet, had a significantly (P = 0.010) higher percentage of correct answers of 67%. Independent from the revision the most frequently misclassified ML was C6 (rev2011: 50.00%, rev2013: 31.13%, Fig. 2B). Case 5 (Fig. 2D and E) represents a very incomplete asymmetrical lumbosacral lesion with a ML of S1 on the right side and L3 on the left side. Group rev2013 determined the MLs significantly better (86.11% versus 94.34%, P = 0.038). The S1 ML on the right side was most frequently misclassified as intact (Figure 2D) in the group using the 2011 worksheet.
Figure 2. Detailed motor level (ML) analysis.

Detailed motor level analysis of all five post-testing cases (A). ML distributions are presented unilaterally for the cases 1 (B) and 2 (C) and bilaterally for the case 5 (D, E). The correct MLs are highlighted in green and additionally marked with arrows. Abbreviations: ISNCSCI, International Standards for Neurological Classification of Spinal Cord Injury.* Left side ISNCSCI scoring in the depicted segments is symmetrical besides left light touch in C5, which is graded as 1.** Left side ISNCSCI scoring in the depicted segments is symmetrical besides left pin prick in C7, which is graded as 0
In Case 2 (Fig. 2C) both motor levels are located in the transition zone C4-C5. The term transition zone was first introduced by Waring et al. 2010 7 and refers to the cut-off levels C5 and L2. In cases where these cut-off levels are graded 3 or better, all participants of the instructional course were taught to use a virtual motor score for C4 (L1) derived from LT and PP to consistently determine the correct ML. We found a trend (rev2011: 86.11%, rev2013: 93.40%, P = 0.098) towards better applicability of this concept on the 2013 worksheet.
Detailed neurological level of injury analysis
A detailed error analysis for the NLI determination is shown in Figure 3. Although not significant, case 2 (P = 0.065) also showed a trend towards better classification performances with the new revision of the worksheet (Fig. 3A). The NLI is defined as the most rostral level of the four single levels: left/right SL and left/right ML. In case 2 the decisive levels for the NLI are the MLs (Fig. 3B). Both MLs are determined as C5 because C5 is graded ≥3 while the rostral adjacent level is considered normal because of the intact sensory scores at C4 and above. This intact graded virtual motor score of C4 is derived from the likewise intact graded sensory scores of C4.7 Based on the previous 2011 worksheet, the NLI was most frequently misclassified one segment too rostral (13.89%) and one segment too caudal (18.06%), respectively. These misclassification rates were lower in the group working with the revised 2013 worksheet (7.55% and 3.77%). For case 5 (Fig. 3C), the NLI is determined by the left ML of L3. This was most often (15.28%) misclassified as L4 with the old worksheet. This specific error is significantly (P = 0.033) reduced (1.89%) in the group using the new worksheet.
Figure 3. Detailed neurological level of injury (NLI) analysis.

Detailed neurological level of injury analysis of all five post-testing cases (A). NLI distributions are presented for the case 2 (B) and case 5 (C). The correct NLIs are highlighted in green and additionally marked with arrows. Abbreviations: ISNCSCI, International Standards for Neurological Classification of Spinal Cord Injury
Discussion
The new graphical layout of the 2013 ISNCSCI worksheet revision was investigated in terms of changes in classification performance of freshly instructed clinicians. We found an improved overall classification performance in a group using the new worksheet compared to a group using the older 2011 version. This improvement is explained by significant improvements of both the ML and the NLI classification performances by approximately 5% each and non-significant improvements in sensory (∼2%) and motor ZPPs (∼3%).
Previously reported classification performances10,14,15 are summarized in Table 2. All listed studies have a comparable pre-test and post-test setup but were conducted using the older version of the worksheet. Most consistently, the performance seems to have improved from moderate 68.5% to good 88.11%. AIS classification performances above 90% still seem to be hard to achieve. Liu et al. postulated15 that NLI classification performance does not need be evaluated, because the NLI can be deduced from SLs and MLs. However, we found approximately 9% misclassified NLIs, revealing that the NLI is actually the third most error-prone ISNCSCI variable after ML and AIS. Clinicians seem to determine the NLI by applying the long definition of the NLI, namely “The NLI refers to the most caudal segment of the spinal cord with normal sensory and antigravity motor function on both sides of the body, provided that there is normal (intact) sensory and motor function rostrally”, rather than applying the aforementioned simpler shortcut rule, that the NLI can be deduced as the most rostral level of the four single levels: left/right SL and left/right ML. We found difficulties in NLI determination in the transition zone C4/C5 (Fig. 3B) and in very incomplete lesions (Fig. 3C). Comparing our previously reported work 9 utilizing the same five post-tests when presented on the 2003 version of the worksheet (Fig. 1C), allowing for comparison of the classification performance achieved with revision 2003 (three most right columns in Table 2) with the revised worksheets of 2011 and 2013, a stable progression towards better performances can be seen for the ML performance as well as the overall classification performance.
Table 2.
Comparison of previously reported ISNCSCI classification performances with the results of the present work (two right most columns)
| Post-test classification performances | Cohen et al.14 1998 | Chafetz et al.10 2008 | Liu et al.15 2013 | Schuld et al.9 2013 | This work revision 2011 |
This work revision 2013 |
|---|---|---|---|---|---|---|
| ASIA Impairment Scale | 81.50% | 79% | 91.30% | 88.1% | 86.11% | 86.03% |
| Completeness | 98.50% | 100% | — | 96.2% | 98.33% | 98.49% |
| Neurological level of injury | — | 94% | — | — | 86.11% | 90.94% |
| Sensory levels | 84.50% | 97% | 88.04% | 96.8% | 97.92% | 97.92% |
| Motor levels | 68.75% | 81% | 82.61% | 81.9% | 83.19% | 88.11% |
| Sensory ZPPs | 78.50% | — | — | 96.8% | 94.44% | 96.79% |
| Motor ZPPs | 78.25% | — | — | 93.3% | 93.33% | 96.42% |
| Overall | 81.67% | 89.90% | 86.52% | 91.5% | 92.22% | 94.30% |
| Number of attendees | 106 | 28 | 46 | 106 | 72 | 53 |
| Number of ISNCSCI cases | 2 | 10 | 1 | 5 | 5 | 5 |
| ISNCSCI worksheet revision | < 2001 | 2006 | 2006 | 2003 | 2011 | 2013 |
ASIA = American Spinal Injury Association; ZPP = Zone of partial preservation; ISNCSCI = International Standards for Neurological Classification of Spinal Cord Injury
The most likely reason for the better post-test performance in the revision 2013 group is the body side based arrangement of the boxes for myotomes and dermatomes. This measure substantially increased the comprehensibility of the worksheet so that it can now be evaluated in a more focused and less oversight-prone manner. This is underlined by the high cervical lesion (Fig. 2A), in which both motor levels are deferred to the sensory levels. For this case a much better classification rate is found in the group using the 2013 revision of the worksheet. The difference between the revision 2011 group (50.00%) and the revision 2013 group (66.98%) is the most obvious outcome of our analysis. This newer layout seems to help apply the ‘motor follows sensory rule’, but more so in the thoracic region (90.56%) as compared to the high cervical region (66.98%).
It seems that the decision whether the ML follows sensory rule has to applied can be drawn more concisely on the new worksheet, because attention can be more focused due to the close arrangement of segmentally corresponding myotomes and dermatomes.
The results cannot be attributed exclusively to the new worksheet layout. Also the continuous efforts of the International Standards Committee contribute to the improvements. The committee created or updated many educational resources like the International Standards Training e-Learning Program (InStep),11 updates4 and clarifications5,6 during the study period.
However, the rather low overall ML classification performance (88.11%), which even drops to low 66.98% in the high cervical case (Fig. 2B), might indicate that the current ML rule may need adjustments regarding the “motor follows sensory” aspect. Insights towards a possible adjustment can be drawn from the incorrect answers of the aforementioned case having a motor level deferred form the sensory level of C2 but with intact graded myotomes C5 and C6 (Fig. 2B). Many of the attendees (rev2011: 50%, rev2013: 31.13%) determined a C6 motor level even after being extensively trained to apply the ‘motor follows sensory rule’ for C2–C4. Thus, C6 seems to be the more intuitive choice. The reason is most probably that the first actually tested myotomes C5 and C6 on the arms are graded as intact. This confirms our earlier finding,9 that it seems to be counterintuitive to first check the sensory scores of C2–C4 for determination of a ML, if the first testable myotome C5 is graded as intact.
To verify this hypothesis an additional post-test case was introduced 2012 to the instructional course participants. This case is a copy of the discussed case 2 (Fig. 2B), but with myotomes C5 and C6 being graded as 3 (variant 2) instead of 5 (variant 1). It is anticipated that the ‘motor follows sensory’ rule is more often correctly applied in this modified case variant 2. In a companion publication16 we have shown that variant 2 (89.13%) is significantly (P < 0.0001) better classified than variant 1 (65.76%). This confirms the hypothesis that the current ’motor follows sensory’ is counterintuitive in cases where the most rostral testable myotomes C5/C6 are graded as intact. Therefore, a modification of the motor level rule seems advisable. A possible modification could be that the motor level only defers to the sensory level, if the cut-off myotome C5 (L2) is not graded as intact.
While ISNCSCI calculators provide a valuable tool for consistent ISNCSCI classification17–20 and minimize classification errors,18 it is essential that clinicians maintain their classification skills to identify to most crucial segments for classification8 and to identify the need to examine non key-muscles which is exclusively needed for sensory incomplete lesions. For example, to distinguish between sensory incomplete lesions (AIS B) and motor incomplete lesions (AIS C/D) the ASIA Impairment Scale has to be determined during or right after the examination. Relying exclusively on computer classifications might degrade this very important classification skill8 needed for a high quality ISNCSCI examination.
Limitations of the study
The ISNCSCI cases used in this study for the pre- and post-tests had already been published9 during the study period. As a consequence, 72% of the attendees could have had the theoretical chance of memorizing the correct classification of the cases by reading the respective publication before the workshop. To address this issue, we performed additional significance tests on the pre-test results of the attendees participating in the ISNCSCI workshop before and after the date of publication. No significant differences could be found between these two groups.
The selected ISNCSCI cases for the pre- and post-tests were intentionally difficult containing consistently tricky scoring constellations and/or borderline decisions. We wanted to avoid ceiling effects and to keep the classification challenging in post-tests even for experts in SCI medicine and rehabilitation. Thus, the cases do not reflect a typical SCI cohort found in clinical trials. It is anticipated that the classification errors in a typical SCI will be substantially lower than the found results.
Conclusion
The 2013 revised ISNCSCI worksheet that has the levels lined up, is likely to be the reason for a reduction of misclassifications of MLs and NLIs. We strongly recommend maintaining the new graphical aspects of the layout for future revisions of the worksheet. However, the correct determination of motor levels in the segments C2 to C4 remains difficult. For ISNCSCI trainings in general, we recommend to extensively discuss at least one case of a high cervical lesion to emphasize on the fact that the ML determination starts with evaluation of the sensory segments C2 to C4. Additionally, the understanding of the concept and the rationale of “motor follows sensory” should be taught intensively. Anecdotally, attendees tend to understand the necessity for application of this concept better, if they are made aware of its consequences. The statistical properties of the variable ML would decrease without the “motor follows sensory” rule, because the range of possible myotomes would decrease from a continuous definition C2–S4/5 to C4–T1 and L2–S1 with a gap between T2 and L1. For the distribution of MLs in large populations this would result in a clustering of MLs at the segments C2 (high cervical lesions) and T1 (all paraplegic lesions).
Disclaimer statements
Contributors None.
Funding None.
Conflicts of interest None.
Ethics approval The EMSCI study is approved (S-188/2003) by the ethics commission of the medical faculty of the Heidelberg University. The pre- and post-test setup is part of the ongoing quality management system.
Supplementary material
Supplementary material for this article is available here: doi:10.1080/10790268.2016.1180831.
ORCID
Christian Schuld http://orcid.org/0000-0003-1921-2938
References
- 1.Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. . International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med 2011;34(6):535–46. doi: 10.1179/204577211X13207446293695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Steeves JD, Lammertse D, Curt A, Fawcett JW, Tuszynski MH, Ditunno JF, et al. . Guidelines for the conduct of clinical trials for spinal cord injury (SCI) as developed by the ICCP panel: clinical trial outcome measures. Spinal Cord 2007;45(3):206–21. doi: 10.1038/sj.sc.3102008 [DOI] [PubMed] [Google Scholar]
- 3.Furlan JC, Fehlings MG, Tator CH, Davis AM. Motor and sensory assessment of patients in clinical trials for pharmacological therapy of acute spinal cord injury: psychometric properties of the ASIA Standards. J Neurotrauma 2008;25(11):1273–301. doi: 10.1089/neu.2008.0617 [DOI] [PubMed] [Google Scholar]
- 4.Kirshblum S, Waring W 3rd. Updates for the International Standards for Neurological Classification of Spinal Cord Injury. Phys Med Rehabil Clin N Am 2014;25(3):505–17, vii. doi: 10.1016/j.pmr.2014.04.001 [DOI] [PubMed] [Google Scholar]
- 5.Kirshblum SC, Biering-Sørensen F, Betz R, Burns S, Donovan W, Graves DE, et al. . International Standards for Neurological Classification of Spinal Cord Injury: cases with classification challenges. J Spinal Cord Med 2014;37(2):120–7. doi: 10.1179/2045772314Y.0000000196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kirshblum SC, Waring W, Biering-Sørensen F, Burns SP, Johansen M, Schmidt-Read M, et al. . Reference for the 2011 revision of the International Standards for Neurological Classification of Spinal Cord Injury. J Spinal Cord Med 2011;34(6):547–54. doi: 10.1179/107902611X13186000420242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Waring WP, Biering-Sørensen F, Burns S, Donovan W, Graves D, Jha A, et al. . 2009 review and revisions of the international standards for the neurological classification of spinal cord injury. J Spinal Cord Med 2010;33(4):346–52. doi: 10.1080/10790268.2010.11689712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schuld C, Franz S, van Hedel HJ, Moosburger J, Maier D, Abel R, et al. . International standards for neurological classification of spinal cord injury: classification skills of clinicians versus computational algorithms. Spinal Cord 2015;53(4):324–31. doi: 10.1038/sc.2014.221 [DOI] [PubMed] [Google Scholar]
- 9.Schuld C, Wiese J, Franz S, Putz C, Stierle I, Smoor I, et al. . Effect of formal training in scaling, scoring and classification of the International Standards for Neurological Classification of Spinal Cord Injury. Spinal Cord 2013;51(4):282–8. doi: 10.1038/sc.2012.149 [DOI] [PubMed] [Google Scholar]
- 10.Chafetz RS, Vogel LC, Betz RR, Gaughan JP, Mulcahey MJ. International standards for neurological classification of spinal cord injury: training effect on accurate classification. J Spinal Cord Med 2008;31(5):538–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Spinal Injury Association International Standards Training E Program (InSteP) http://www.asia-spinalinjury.org/elearning/elearning.php [cited April 15, 2015].
- 12.Curt A, Schwab ME, Dietz V. Providing the clinical basis for new interventional therapies: refined diagnosis and assessment of recovery after spinal cord injury. Spinal Cord 2004;42(1):1–6. doi: 10.1038/sj.sc.3101558 [DOI] [PubMed] [Google Scholar]
- 13.Kirshblum SC. Difficult cases in classification of SCI. Presented at the American Paraplegia Society Meeting; Las Vegas, NV, USA, 2006.
- 14.Cohen ME, Ditunno JF, Donovan WH, Maynard FM. A test of the 1992 International Standards for Neurological and Functional Classification of Spinal Cord Injury. Spinal Cord 1998;36(8):554–60. doi: 10.1038/sj.sc.3100602 [DOI] [PubMed] [Google Scholar]
- 15.Liu N, Zhou MW, Krassioukov AV, Biering-Sørensen F. Training effectiveness when teaching the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) to medical students. Spinal Cord 2013;51(10):768–71. doi: 10.1038/sc.2013.75 [DOI] [PubMed] [Google Scholar]
- 16.Franz S, Kirshblum SC, Weidner N, Rupp R, Schuld C. Motor levels in high cervical spinal cord injuries: implications for the international standards for neurological classification of spinal cord injury. J Spinal Cord Med 2016. 25 Feb; Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Linassi G, Shan RLP, Marino RJ. A web-based computer program to determine the ASIA impairment classification. Spinal Cord 2010;48(2):100–4. doi: 10.1038/sc.2009.98 [DOI] [PubMed] [Google Scholar]
- 18.Schuld C, Wiese J, Hug A, Putz C, van Hedel HJA, Spiess MR, et al. . Computer implementation of the international standards for neurological classification of spinal cord injury for consistent and efficient derivation of its subscores including handling of data from not testable segments. J Neurotrauma 2012;29(3):453–61. doi: 10.1089/neu.2011.2085 [DOI] [PubMed] [Google Scholar]
- 19.Waring W, Echeverria E, Kirshblum S, Reeves R. ISNCSCI Calculator (International Standards for the Neurological Classification of Spinal Cord Injury). Presented at International Spinal Cord Society (ISCOS) Meeting 2013; London, UK.
- 20.Chafetz RS, Prak S, Mulcahey MJ. Computerized classification of neurologic injury based on the international standards for classification of spinal cord injury. J Spinal Cord Med 2009;32(5):532–7. [DOI] [PMC free article] [PubMed] [Google Scholar]


