Abstract
Radioactive131 iodine (RAI) body burden is estimated in thyroid cancer patients by a) exposure rate meter and b) external probe counting. A calibration factor of 301 cpm/MBq (d = 16 cm) is used for the probe for estimates of whole body activity. Patients sit in a rotating stool with their center corresponding to the field of view for estimation of whole body RAI. Radioactive counts are obtained for anterio posterior (AP) and postero anterior (PA) geometries. Whole body retention factor is expressed as a ratio against assayed activity administered to the patient on day 1. With exposure rate measurement, for off-thyroxin (hypothyriod) patients, the retention factors were 0.148 ± 0.12 (n = 211) and 0.07 ± 0.08 (n = 68) at 48 h and 72 h, respectively. For recombinant TSH (rhTSH) (euthyroid) group, the retention factors were 0.089 ± 0.06 (n = 24) and 0.05 ± 0.05 (n = 19) at 48 h and 72 h, respectively. By probe counting method, the obtained retention factors were 0.081 ± 0.013 (range: 0.071–0.096) (off-thyroxine group) and 0.039 ± 0.03 (range: 0.008–0.089) for the rhTSH group at 48 h. The 72 h retentions in the off thyroxine (hypothyriod) group and the rhTSH (euthyroid) group were 0.048 ± 0.024 (range: 0.016–0.076) and 0.005, respectively. The radioactive body burdens at 48 h were in the range of 290-315 MBq (7.8–8.5 mCi) for the off-thyroxine group and 44–286 MBq (1.2–7.7 mCi) for the rhTSH group. The calculated residence times in whole body were 21.97 ± 3.8 h (range: 17.1–27.1) for off-thyroxine group and 14.28 ± 2.75 h (range: 9.97-19.46) showing high statistical significance (P < 0.001). The specific blood doses were 0.118 ± 0.025 mGy/MBq (range: 0.083–0.172) for the off-thyroxine group (females n = 23); 0.87 ± 0.028 mGy/MBq (range: 0.057–0.130) (females n = 13), 0.080 ± 0.013 mGy/MBq (range: 0.069–0.098) (males n = 5) and 0.080 ± 0.028 (range: 0.059–0.118 for rhTSH patients (males n = 4). The mean mGy/MBq for blood was higher in females—about 10% for the rhTSH group compared to 40% higher for the off thyroxine (THW) group. The dose to blood was “inversely proportional” to the body weight, both in the off-thyroxine group and the rhTSH group but the dependence was not very strong with rhTSH administration because of less residence time of the radioactive iodine. There was no correlation between administered activity and retained body burden at 48 h or 72 h.
Keywords: Blood dose in iodine131, differentiated thyroid cancer, iodine kinetics, radioactive iodine, whole body retention
Introduction
Radioactive 131 iodine (RAI) administrations continue to be in practice for the management for differentiated thyroid cancer (DTC), with adequate thyroid stimulating hormone (TSH) stimulation for subsequent ablations. The commonly followed method is to achieve this by endogenous TSH stimulation by the withdrawal of thyroxine.[1] Large doses ranging from 1.85 GBq to 7.4 GBq (50–200 mCi) are administered. Numerous studies worldwide have reported comparable results with recombinant thyroid stimulating hormone (rhTSH) intervention as a conventional thyroxine hormone withdrawal.[2] The mean radiation dose to blood, individual risk organs, and the whole body depends on the rate of clearance of radioactive iodine (131I) and therefore, has a direct correlation to the retained part of administered radioactivity.
The European Association of Nuclear Medicine (EANM) dosimetry committee indicates pretherapeutic blood and bone marrow dosimetry and issued standard operating procedures (SOPs) and advice to perform pretherapeutic or therapeutic patient-specific absorbed dose calculations.[3] Usually, an estimate of retention time is quantified with a pretherapeutic dose either using a gamma camera conjugate view imaging or by using external probe (sodium detector with crystal) and patient distance of 2 m. The Society of Nuclear Medicine (SNM), USA[4] and the American Thyroid Association[5] have stipulated the need for written instructions to the discharged patients describing methods to limit the radiation dose to the public not exceeding 1 mSV (100 mRem). Patient-specific calculations need to be performed with several assumptions to provide specific recommendations.
The retention patterns in the whole body at the time of discharge varies from patient to patient, and depends on the individual body's functional variations and extent of hydrations. The patterns of retention are relevant to calculate a) the mean blood and bone marrow dose b) the number of days these patients should follow safety guidelines at home, and c) to estimate the likely doses to the other inmates at their residences. Most of the centers measure body burden using external exposure assessment with a Geiger-Müller type or ionization type survey instruments. Generally, exact body retained activities are not quantified. In the Royal Hospital, since the year 2005 differentiated cancer thyroid treatments are being carried out in I-131 isolation wards. Radiation safety applications call for the need to understand radioactive 131I (RA 131I) clearance pattern to estimate whole body doses. If individualized retention pattern is available, it might help in estimating blood and bone marrow doses.
Materials and Methods
Study approvals
The Medical Ethics and Scientific Research Committee of the Royal Hospital, Ministry of Health, Oman in its document MESRC No. 14/2014 dated April 6, 2014 has approved the research study to obtain data on the residual body burden of radioactivity in patients. This committee has legal scope to approve human studies following the Helsinki Declaration 1975.
Methods
The available exposure rate data in the Department of Nuclear Medicine, Royal Hospital (about 250 patients) were reviewed to calculate the body burden and retention of whole body at 48 h and 72 h. Based on a method recommended in an earlier report[6] iodine-131 remnant whole body radioactive burden was estimated using a calibrated thyroid probe spectrometer. (AtomLab 950, Biodex) with 2“x2” NaI crystal.
The thyroid probe/spectrometer operation was checked with a Cs-137 check source in terms of high voltage calibration and “photo peak calibration” for spectrometer setting. Using decayed unused I-131 capsules, the calibration factor of the thyroid probe (counts/min per MBq) was estimated under “scatter conditions” using water phantom. The field of view (FOV) of the conical collimator of thyroid probe was determined, and the covering field to encompass the whole body of the patients was ensured. The estimated field of view (FOV) for a count rate variation within 8% obtained for our counting setup was 65cm, which was of the same order as indicated in previous studies. The calibration factors for the probe with neck phantom (1 cm depth) was 974 cpm/MBq. Calibration factor with water phantom was 406 cpm/MBq (11 cm source depth) and 301 cpm/MBq (16 cm source depth) respectively (refer calibration in Figure 1).
Figure 1.
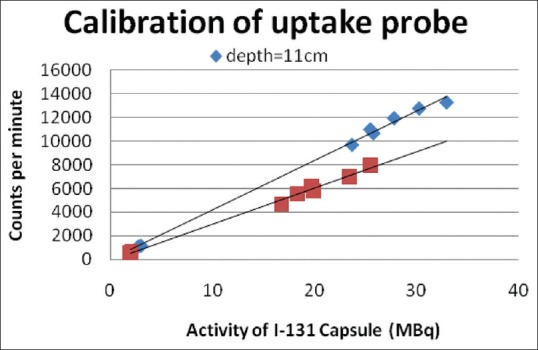
Counts/min for different I-131 activity surrounded by water at depths 11 cm, 16 cm
The patient who was about to be discharged from the ward when going for gamma camera scan was asked to sit before the thyroid probe counter at a distance of 2.2 m. Radioactive counting was carried out for 6 min (2 × 180” counts) anterior counts and 6 min (2 × 180” counts) posterior counts were recorded. Background counts for the same amount of time were determined and net counts per minute (cpm) for the patient were determined. The geometric mean of cpm was estimated and using the “probe calibration,” patients' whole body I-131 activity was calculated. The geometry of measurement is shown in Figure 2.
Figure 2.
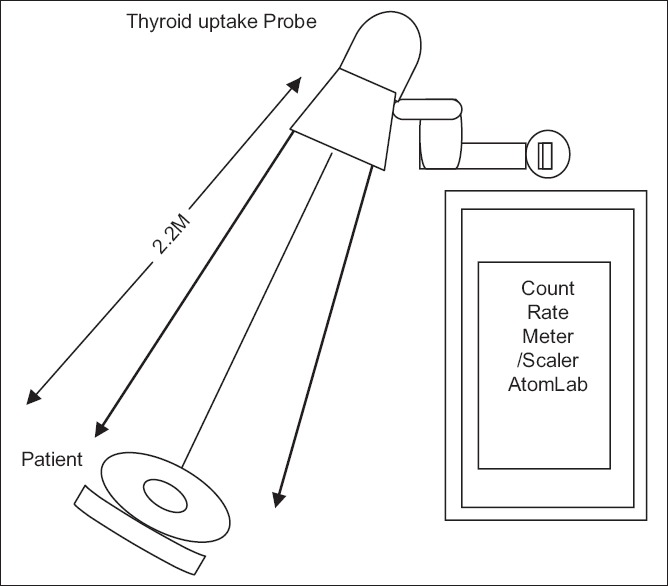
Location of the patient in a sitting position for estimation of whole body retained I-131 activity
Percentage retention was expressed with respect to the administered (assayed) activity to the patient on the first day, from equation 1. As the discharge of the patients took place on the second day (48 h) and third day (72 h), the retention fractions at 48 h and 72 h were used to calculate the “residence time” using the equation 2.
Whole body retention48h = Estimated I-131 activity in MBq48h /activity administered0h [1]
Whole body residence time in hours = 48 h/ln [100/%retn.48h] or 72 h/ln [100/%retn.72h] [2]
Empirical formulas in the literature[7] for calculation of “patient's blood volume” using height (H) in cm and weight (W) in kg are available (equations 3 and 4). Using the value of whole body residence time, the specific dose DBL and DBM per MBq administered A0 were calculated using equations 5 and 6 substituting the calculated retention time and the value of the estimated time at 48 h or 72 h.
BLVmale = {31.9 × height (H)} + {26.3 × weight (W) – 2402} [3]
BLVfemale = {56.9 × height (H)} + {14.1 × weight (W) – 6460} [4]
DBL /A0 = [{ 15.12/BLVml} + {0.0188/Wkg⅔}] × residence time in hours [5]
DBM /A0 = [{ 8.54/BLVml} + {0.0106/Wkg}] × residence time in hours [6]
Patients
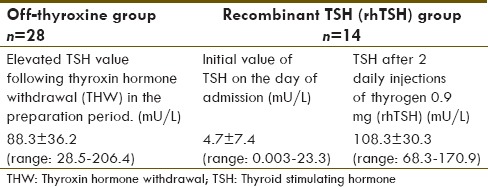
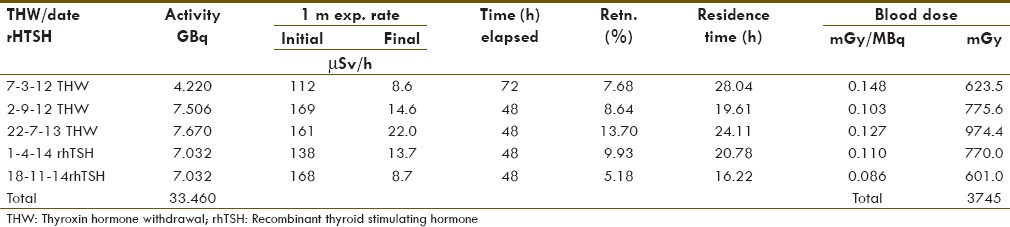
Exposure rates at 1 m measured from the total number of 244 patients using ‘beta gamma survey instrument’, were retrospectively analyzed. Tables 1 and 2 show the details of patients studied with the external counting method.
Table 1.
Details of I131activity administered, weight, height, blood volume
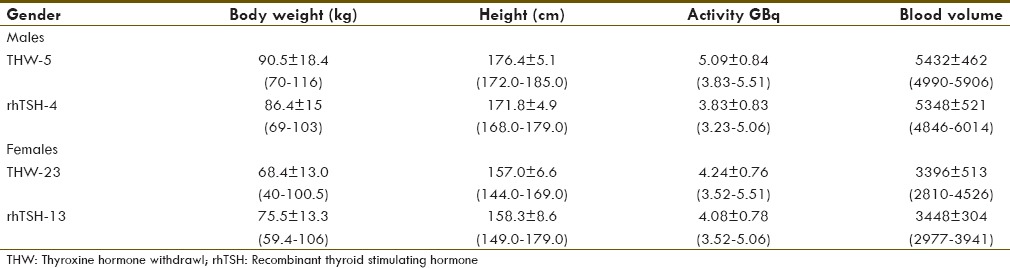
Table 2.
TSH values in the two groups (THW and rhTSH protocols) of patients
Results
Table 3 illustrates the retention factor measured with sequential external exposure rates obtained from the patients at 1 m. These retention factors were compared with earlier publications[6,8] using diagnostic and therapeutic radioactive iodine administrations. The present results were comparable to earlier reported values. Table 4 shows the estimated retention factors, residence time of I-131 in the whole body, and the whole body activity by the external counting method. The whole body residence time for the off-thyroxine group was 21.54 ± 3.62 h (in the range of 16.7-27.9 h) compared to the rhTSH group where it was 17.22 ± 6.14 h (in the range of 9.97-32.4 h). The residence time in the rhTSH group was less compared to the off-thyroxine group, with a high statistical significance (P < 0.001). Figure 3 shows the comparison of estimated residence times in these two groups of patients. The obtained residence time in the present study was comparable to the earlier reported values (8) 24.1 ± 7.8 h for the THW group and 17.3 ± 3.9 h for the rhTSH group. The 48 h retentions ranged between 0.071 and 0.096 with mean 0.081 ± 0.014 (for off-thyroxine patients) and 0.008-0.15 with mean 0.045 ± 0.04 (for recombinant TSH patients). The 72 h retentions in THW patients were almost equal to 48 h retentions in rhTSH patients. The comparison of retention factors at 48 h for rhTSH patients and at 72 h for THW patients is illustrated in Figure 4. Estimated radioactive body burden at 48 h was in the range of 290-365 MBq (7.8-9.9 mCi) for the off-thyroxine group and 44-570MBq (1.2-15.4 mCi) for the rhTSH group. The 72 h radioactive body burden in THW patients was almost equal to the 48 h remnant activity in rhTSH patients [refer Figure 5].
Table 3.
Retention factors from external exposure rates
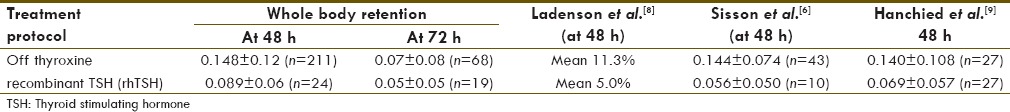
Table 4.
Estimated residence time and whole body retention by probe counting method
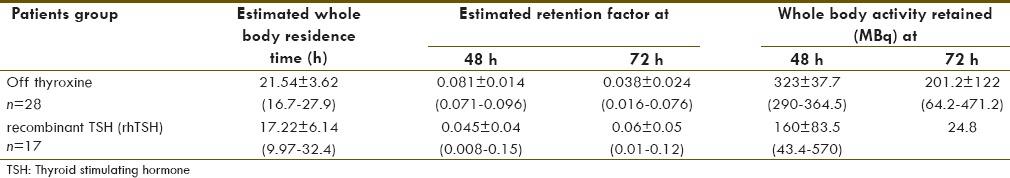
Figure 3.
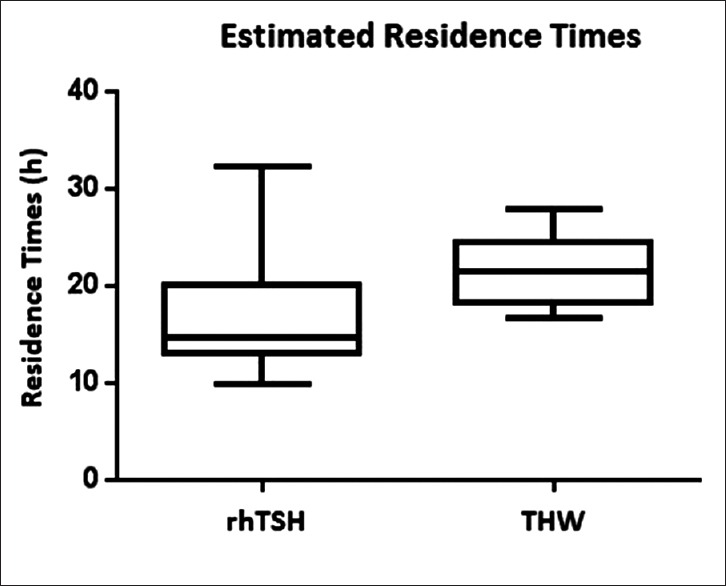
Estimated residence times in rhTSH and THW protocols
Figure 4.
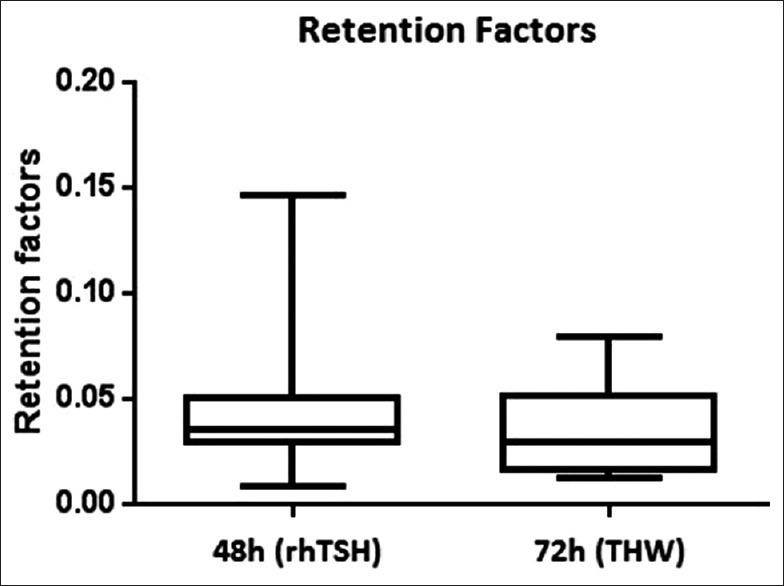
Comparison of whole body retention factors of I-131 against administered activity for two protocols of treatment
Figure 5.
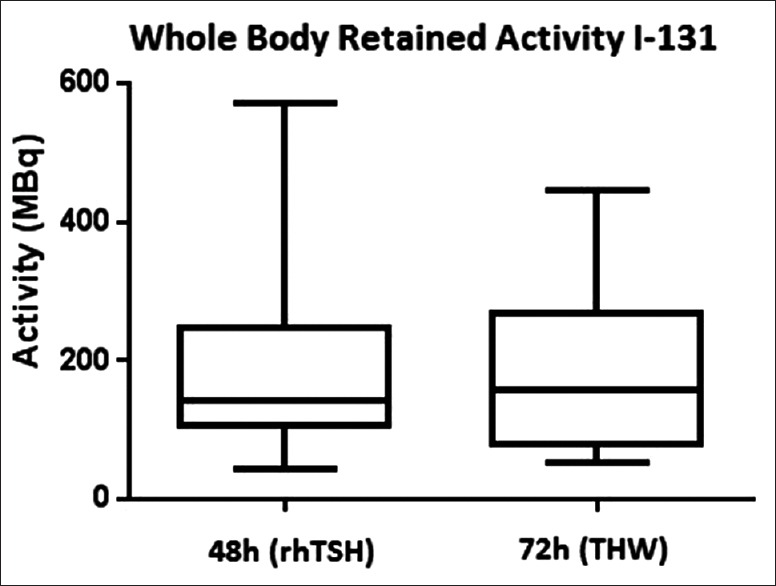
Whole body retained activity in rhTSH and THW patients expressed in MBq estimated by external probe counting
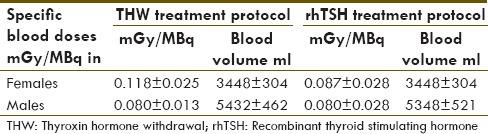
Table 5 shows the calculated specific blood and bone marrow dose in mGy/MBq, and the total dose due to the I-131 administrations. Considering males and females together, the specific dose to blood was 0.111 mGy/MBq for THW patients (n = 28) and 0.086 mGy/MBq for rhTSH patients (n = 17); (P < 0.012). Figure 6 shows the reduced specific blood dose values in rhTSH patients vis-à-vis THW patients. As the blood volume in females was less than that of male patients, the mGy/MBq value were more for female subjects compared to male subjects. For the THW group, the specific dose of blood in females was 0.118 ± 0.025 mGy/MBq (ranging from 0.083 to 0.172). For the rhTSH group, in females the specific dose to blood was 0.087 ± 0.028 mGy/MBq (ranging from 0.067 to 0.129). For the THW group, the specific dose to blood in males was 0.080 ± 0.013 (ranging from 0.069 to 0.098). For males in the rhTSH group, the specific dose to blood was 0.080 ± 0.028 (ranging from 0.048 to 0.112). It was seen that in males the mGy/MBq was almost the same with both THW and rhTSH protocols.
Table 5.
Dose to Blood and bone marrow from external counting method
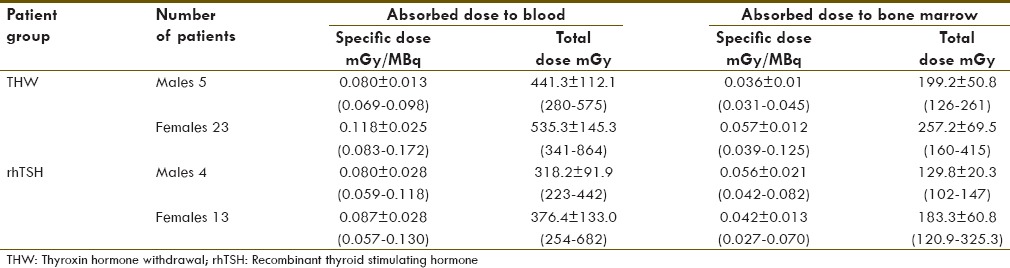
Figure 6.
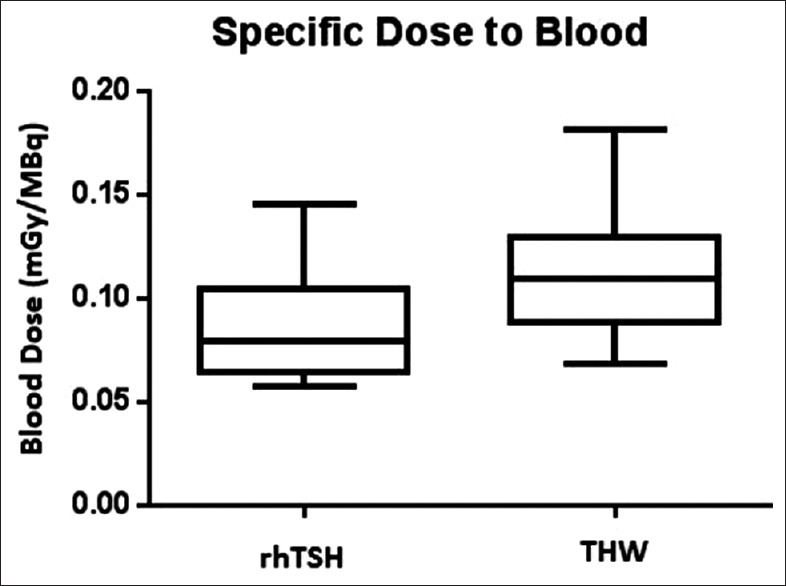
Higher value of specific blood dose seen THW group of patients compared to rhTSH patients
Grouping males and female cases together, the specific dose to bone marrow was 0.053 mGy/MBq in the THW group and 0.041 mGy/MBq in the rHTSH group, constituting about 50% of the dose to blood. For the THW group, the specific dose to bone marrow in females was 0.057 ± 0.012 mGy/MBq (range: 0.04–0.125 mGy/MBq). For females in the rhTSH group, the specific dose to bone marrow was 0.042 ± 0.013 mGy/MBq (range: 0.032 to 0.10 mGy/MBq). For the THW group, the specific dose to bone marrow in males was 0.036 ± 0.006 mGy/MBq (range: 0.031-0.045 mGy/MBq). For males in the rhTSH group, the specific dose to bone marrow was 0.037 ± 0.013 mGy/MBq (range: 0.042-0.082 mGy/MBq). Females received higher bone marrow doses compared to males, by similar magnitude as seen with absorbed dose to blood between them. Table 6 shows the present results as against a previous report;[8] it was observed that there was good agreement.
Table 6.
Specific dose to blood DBlood/A0 (by probe counting) compared with other reports
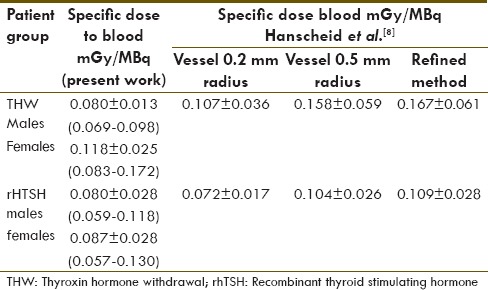
Figure 7 shows the plot of specific dose to blood and bone marrow against residence time. The dose per unit activity is directly proportional to the residence time. Specific doses to blood and red bone marrow are less in the case of recombinant TSH protocol because of reduced residence time. In Figure 8, the variations of blood dose (cGy) estimates for all the patients have been plotted and shown against body weight. It can be seen that blood dose is inversely proportional to body weight. Figure 9 shows the relation between the body burden estimated activity based on external exposure rate measured at 1 m and the activity determined by the external probe method. It can be seen that external exposure rate underestimates the body burden even by a factor of 2. In Figure 10, the residual activity estimated in the patients against administered activity at t = 0 h is shown at an elapsed time of 48 h and 72 h. It is very clear that there is no correlation of residual body burden with the activity administered. Table 7 shows the details of activity administered to a patient who had repeat administration for a metastatic spread and the calculated cumulative blood doses. For a total cumulated activity of 33.5 GBq, the cumulative blood dose was 3745 mGy over a period of 3 years.
Figure 7.
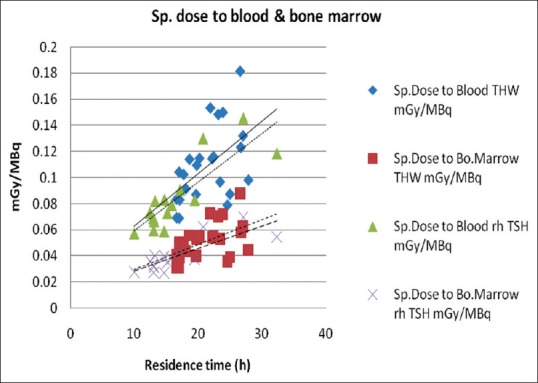
Variation of specific dose to blood and marrow related to residence time
Figure 8.
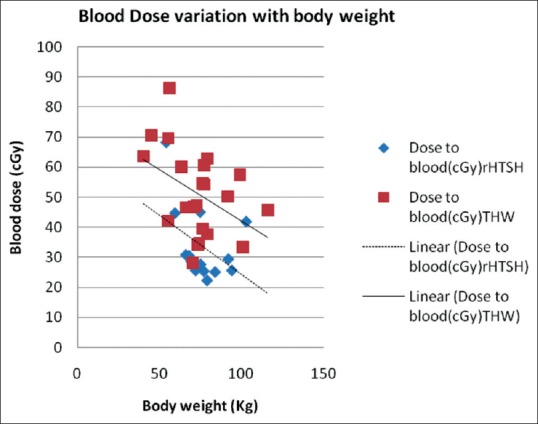
Variation of blood dose estimates against body weight
Figure 9.
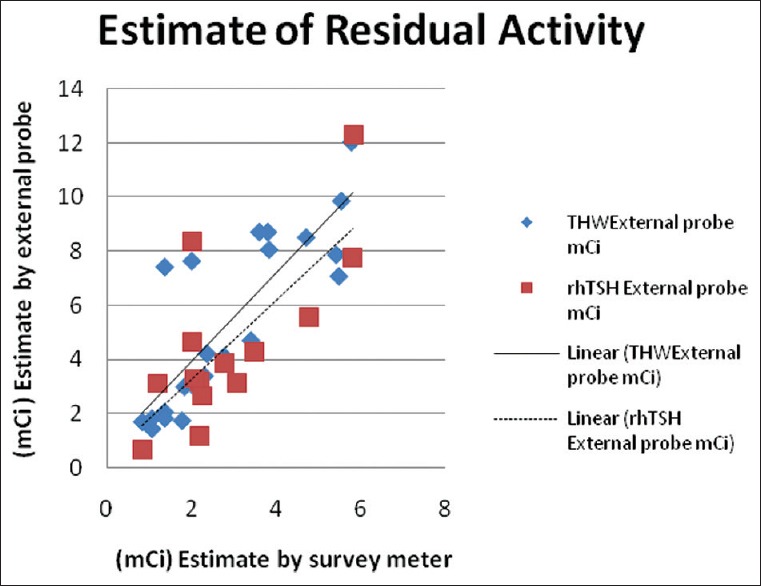
Radioactive body burden estimates by survey meter and external probe methods
Figure 10.
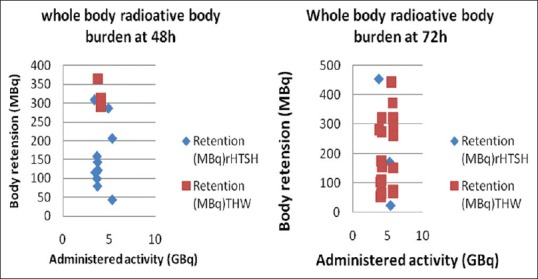
The whole body measured activity estimates at 48 h and 72 h in THW and rhTSH protocols
Table 7.
Cumulative blood dose estimates in repeat I-131 administrations
Discussion
The present work has outlined a simple method to quantify residual radioactive I-131 body burden in the patients treated for DTC. The method is based on obtaining whole body counts by a calibrated thyroid probe at 2.2 m distance. In this method, about ±10-15% accuracy is expected in estimating radioactive body burden, because of some uncertainties. An earlier work[6] outlined a similar counting for estimating residual body burden using reference whole body counts at 2 h after the administration of I-131 activity capsule without voiding urine. We have taken ratio with respect to administered measured activity. The TSH value of patients in the off-thyroxine group was 88.3 ± 36.2 mU/L (range: 28.5-206.4) (n = 28) and for the rhTSH group was 108.3 ± 30.3 mU/L (range: 68.3-170.9) (n = 14) on the day of therapy capsule administration.
The measured retention factors in Table 3 were comparable to earlier reports in the literature. Table 4 shows the retention factors obtained from the external probe method at 48 h 0.081 ± 0.014 (0.071-0.096) for the THW group and 0.045 ± 0.04 (0.008-0.15) for the rhTSH group compared to the entries in Table 3, viz., 0.148 ± 0.12 (n = 211) for the THW group and 0.089 ± 0.06 (n = 24) for the rhTSH group. This is because in Table 3 the patients who were discharged at 72 h were also included in measured exposure rates at 48 h, whereas in Table 4 the patients who stayed longer till 72 h were not counted at 48 h.
The residence times 21.54 ± 3.62 h (range: 16.7-27.9 h) (n = 28) for THW protocol and 17.22 ± 6.14 h (range 9.97-32.4 h) (n = 17) for rhTSH protocol were comparable to 24.1 ± 7.8 h (n = 27) for THW protocol and 17.3 ± 3.9 h (n = 27) for rhTSH protocol reported by Hanschied et al.[9] [Figure 7] that clearly brought out that residence time was the dominant factor deciding the whole body dose and hence, dose to blood. In Figure, eight doses to blood (in cGy) based on the administered activity demonstrated a negative slope for dose to blood against body weight. Though the body weight dependence holds good for both THW and rhTSH patients, the body weight dependence was less significant due to fast clearance in the first phase (within the first 48 h). Dose to bone marrow [Table 5] had the same pattern like irradiated blood except for less magnitude (about 70% of blood dose). Specific dose to bone marrow was around 0.036-0.057 mGy/MBq for THW patients which was in the same order reported by the I 131 manufacturer, ‘GE Healthcare’.[10] It reported that for adults, red marrow dose was 0.035 mGy/MBq, 0.054 mGy/MBq, 0.086 mGy/MBq, and 0.12 mGy/MBq for thyroid uptakes 0%, 15%, 35%, and 55%, respectively. In Table 6, our presently reported values of dose to blood were compared to the theoretical dose estimates by an earlier reference for different blood vessel radii.[9]
A guidance value of 0.17 mRem/h at 1 m distance from 1 mCi body retention was indicated in an earlier report.[5] Based on this value, if the exposure rates in the patients for whom probe estimation of body burden was carried out, the comparison of activities are shown in Figure 9. Exposure rate measurements underestimate the residual body burden even by a factor of 2 compared to external probe estimations. The attenuation offered by body tissue may not be true and therefore, the true activity in terms of exposure rate might be overestimated. In a previous report[6] the first measurement was taken at 2 h after administration without voiding urine, after the I-131 capsule got dissolved in the stomach and was available in the blood circulation. This might be representing true activity equivalent administered to the patient.
Figure 10 indicates that 48 h and 72 h of residual radioactivity in the whole body does not have any correlation with “administered dose” (GBq) of iodine-131. Therefore, discharging patients on the 2nd day and 3rd day have no relation to the activity administered. Most of the patients with rhTSH administration had a residual activity of less than 150 MBq (4 mCi) at 48 h, whereas THW patients had about 200 MBq (5.5 mCi) at 72 h.
Residence time and specific dose to blood and bone marrow
In Figure 7, the trend lines show that both THW and rhTSH protocol patients overlapped indicating that there was no separate mechanism for absorbed dose to blood because of endogenous TSH simulation or by external administration of TSH. Larger residence time in THW protocol gave rise to more absorbed dose to blood. The magnitude of less residence time in rhTSH patients was brought out in our previous study.[11] It is clearly shown in Table 4 with a high statistical significance (P < 0.001); two thyrogen injections in euthyroid patients had given fast clearance compared to THW patients. A recent publication[12] has discussed that in THW protocols, whole body I-131 activity is eliminated 35-75% in the first 24 h and about 80% is eliminated in 48 h. In this present work, it is brought out from body burden measurements, that a mean retention of whole body at 48 h is 8.1% in THW patients (eliminated portion: 91.9%) vis à vis 3.9% (eliminated portion: 96.1%) in rhTSH patients.
In Table 8, the clearance patterns have been brought out for the two protocols from the present study, and previous works.[11,13,14] If the biophysical kinetics are considered, we have two phases of clearances differing in THW and rHTSH patients. We tried to explain this based on the clearances of two types of iodines, viz., inorganic iodine and organic iodine excreted from body with both of these containing radioactive 131I. Sustained presence of TSH is responsible for a higher uptake in remnant thyroid cells (THW group), increased organification followed by fast whole body clearance in the 2nd phase. Transient presence of TSH (rHTSH) is responsible for less uptake in thyroid, slowed down organification with slowed down elimination (with prolonged clearance time in the later phase).
Table 8.
Observations in two protocols regarding 131I uptakes and clearance
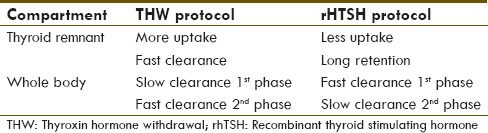
Dose to blood in males and females
Table 9 summarizes the results of mGy/MBq in both THW and rhTSH protocols in males and females. Dose to the blood was higher in females compared to males because the blood volume was less in females for an equivalent value of weight and height. Since packed cell volume (PCV) is lower in women, red cell volume (RCV) calculated in a study[15] was found to be lower in females, whereas plasma volume was the same in males and females. If there is increased organification in THW patients (due to sustained TSH value) and this organified iodine is carried by the RBCs, it will explain the increased mGy/MBq in females (because of less RCV). If we consider that organified iodine is less in case of rhTSH protocol patients (both males and females), the effect of RCV is not predominant in the both groups. This can explain as to why mGy/MBq was the same in both males and females in the rhTSH group irrespective of a large volume of blood present in males [refer to Columns 4 and 5, Table 9].
Table 9.
Summary of specific blood doses in males and females
Financial support and sponsorship
The above work forms part of research work No. MESRC #14/2014. There are no agencies which supported separate funding for the above work.
Conflicts of interest
It is declared that there are no conflicts of interests.
Acknowledgements
The authors express thanks to the Director General of Royal Hospital for giving the kind permission to publish this work and the Endocrinology Unit of the Division of Medicine for the patients' referral.
References
- 1.Das BK, Biswal BM, Krishna Bhavaraju VM. Rational management of differentiated thyroid cancer. Malays J Med Sci. 2006;13:45–51. [PMC free article] [PubMed] [Google Scholar]
- 2.Schlumberger M, Catargi B, Borget I, Deandreis D, Zerdoud S, Bridji B, et al. Tumeurs de la Thyroïde Refractaires Network for the Essai Stimulation Ablation Equivalence Trial. Strategies of radioiodine ablation in patients with low-risk thyroid cancer. N Engl J Med. 2001;366:1663–73. doi: 10.1056/NEJMoa1108586. [DOI] [PubMed] [Google Scholar]
- 3.Lassman M, Hänscheid H, Chiesa C, Hindorf C, Flux G, Luster M. EANM Dosimetry Committee. EANM Dosimetry Committee series on standard operational procedures for pre-therapeutic dosimetry I: Blood and bone marrow dosimetry in differentiated thyroid cancer therapy. Eur J Nucl Med Mol Imaging. 2008;35:1405–12. doi: 10.1007/s00259-008-0761-x. [DOI] [PubMed] [Google Scholar]
- 4.Silberstein EB, Alavi A, Balon HR, Clarke SE, Divgi C, Gelfand MJ, et al. The SNMMI practice guideline for therapy of thyroid disease with 131I 3.0. J Nucl Med. 2012;53:1633–51. doi: 10.2967/jnumed.112.105148. [DOI] [PubMed] [Google Scholar]
- 5.Sisson JC, Freitas J, McDougall IR, Dauer LT, Hurley JR, Brierley JD, et al. American Thyroid Association Taskforce on Radioiodine Safety. Radiation safety in the treatment of patients with thyroid diseases by radioiodine 131I: Practice Recommendations of the American Thyroid Association. Thyroid. 2011;21:335–46. doi: 10.1089/thy.2010.0403. [DOI] [PubMed] [Google Scholar]
- 6.Sisson JC, Shulkin BL, Lawson S. Increasing efficacy and safety of treatments of patients with well-differentiated thyroid carcinoma by measuring body retentions of 131I. J Nucl Med. 2003;44:898–903. [PubMed] [Google Scholar]
- 7.Hänscheid H, Lassmann M, Luster M, Kloos RT, Reiners C. Blood dosimetry from a single measurement of the whole body radioiodine retention in patients with differentiated thyroid carcinoma. Endocr Relat Cancer. 2009;16:1283–9. doi: 10.1677/ERC-09-0076. [DOI] [PubMed] [Google Scholar]
- 8.Ladenson PW, Braverman LE, Mazzaferri EL, Brucker-Davis F, Cooper DS, Garber JR, et al. Comparison of administration of recombinant human thyrotropin with withdrawl of thyroid hormone for radioactive iodine scanning in patients with thyroid carcinoma. N Engl J Med. 1997;337:888–96. doi: 10.1056/NEJM199709253371304. [DOI] [PubMed] [Google Scholar]
- 9.Hänscheid H, Lassmann M, Luster M, Thomas SR, Pacini F, Ceccarelli C, et al. Iodine biokinetics and dosimetry in radioiodine therapy of thyroid cancer: Procedures and results of a prospective international controlled study of ablation after rhTSH or Hormone withdrawl. J Nucl Med. 2006;47:648–54. [PubMed] [Google Scholar]
- 10.Germany: Braunschweig; 2014. Theracap 37 MBq-5.55 GBq IBS600P Package Leaflet. 12670743, GE Healthcare Buchler GmbH and Co. KG Gieselweg 1, D-38110. [Google Scholar]
- 11.Ravichandran R, Al Saadi A, Al Balushi N. Radioactive body burden measurements in (131) iodine therapy for differentiated thyroid cancer: Effect of recombinant thyroid stimulating hormone in whole body (131) iodine clearance. World J Nucl Med. 2014;13:56–61. doi: 10.4103/1450-1147.138576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hewamanna R, Loganathan N, Perera DK. Releasing thyroid cancer patients from the hospital based on dose rate measurement after 131 I activity administration. J Natn Sci Foundation Sri Lanka. 2014;42:137–41. [Google Scholar]
- 13.Ravichandran R, Binukumar J, Al Saadi A. Estimation of effective half life of clearance of radioactive Iodine (I) in patients treated for hyperthyroidism and carcinoma thyroid. Indian J Nucl Med. 2010;25:49–52. doi: 10.4103/0972-3919.72686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ravichandran R, Supe SS, Jayasree U, Devaru S. Measurement of the radioactive body burden in patients receiving Iodine-131 treatments for carcinoma of the thyroid. Eur J Nucl Med. 1997;24:464. doi: 10.1007/BF00881823. [DOI] [PubMed] [Google Scholar]
- 15.Hurley PJ. Red cell and plasma volumes in normal adults. J Nucl Med. 1975;16:46–52. [PubMed] [Google Scholar]


