In our recent effort, we introduced a submaximal index that utilized ventilatory efficiency relative to CO2 production (VE/CO2) to evaluate the cardiovascular effectiveness to functional electrical stimulation lower-extremity cycling (FES-LEC) in persons with spinal cord injury (SCI) (Gorgey and Lawrence, 2016). When compared to the resting state, we found that an acute bout of FES-LEC resulted in increased ventilation during exercise and a significant decrease of approximately 22% in the VE/CO2 ratio, suggesting that this ratio could be utilized to monitor the cardiovascular response during submaximal FES-LEC in the SCI population. The study demonstrated that a potential limitation to the FES-LEC application is a heavy reliance on carbohydrate storage as a main source of substrate utilization. Reliance on carbohydrate utilization, transformation to fast-twitch fibers following SCI and random muscle recruitment are likely to introduce rapid muscle fatigue during FES-LEC applications. This may limit oxygen uptake and outcomes regarding cardiovascular profile. In this perspective, we propose that skeletal muscle conditioning via surface neuromuscular electrical stimulation (NMES) may be an essential rehabilitation intervention to improve the outcomes of FES-LEC applications.
Adaptations in skeletal muscle following SCI: FES-LEC capacity is limited due to notable muscle atrophy, intramuscular fat infiltration, and architectural changes in skeletal muscle following SCI (Gorgey and Dudley, 2007). Skeletal muscle atrophy is one of the most prominent adaptations to occur post injury, with thigh muscle cross-sectional area being up to 30–50% smaller than that of able-bodied controls within several weeks post injury (Gorgey and Dudley, 2007). Extensive skeletal muscle atrophy is also correlated with the accumulation of intramuscular fat, which is associated with glucose intolerance and insulin resistance (Elder et al., 2004). Accumulation of intramuscular fat has also been shown to impede the progression of electrical current following SCI. This is likely to necessitate an increase of the amplitude of current delivered to skeletal muscle and may cause episodes of autonomic dysreflexia (Gorgey et al., 2013, 2014). Skeletal muscle fiber typing transformation occurs and leads to a shift from slow oxidative fibers to fast glycolytic fibers following SCI (Talmadge et al., 2002). One resultant characteristic of this transformation is rapid muscle fatigue, which has been observed in the current study during an acute bout of cycling, where we have found that the time until fatigue was 10 ± 8 minutes (Gorgey et al., 2014; Gorgey and Lawrence, 2016).
Limited oxygen uptake following spinal cord injury: Exercising at an intensity required to adequately stress the cardiovascular system is a major limitation of FES-LEC training. Previously, peak VO2 has been utilized as a marker for cardiopulmonary profile in persons with SCI (Hasnan et al., 2013). A previous report found that FES-LEC cycling alone was not as sufficient at improving cardiovascular profile when compared with a hybrid exercise training plan that implemented the upper extremity and lower extremity musculature following SCI (Hasnan et al., 2013). Measuring peak VO2 requires maximal effort, which is a major limitation that is often unachievable in the SCI population. It has been shown that submaximal FES-LEC elicits a VO2 between 40% and 60% of peak VO2 (Hasnan et al., 2013). We have yielded comparable results, suggesting that participants are performing at intensities close to 40% of their VO2 peak (Gorgey et al., 2014).
Substrate utilization during FES: Carbohydrate utilization was six times greater than fat utilization during an acute bout of FES-LEC in the current study (Gorgey and Lawrence, 2016). We observed a significant increase of the respiratory exchange ratio during exercise, suggesting that a reliance on glycolysis may cause preferential substrate utilization of carbohydrate over fat. With such a dramatic dependence on carbohydrate utilization during FES-LEC, it is important to emphasize the importance of prior training and conditioning since it may have the potential to decrease the respiratory exchange ratio and increase the use of fat as a substrate.
Importance of conditioning: Neuromuscular electrical stimulation (NMES) accompanied with progressive resistance training has shown to be an effective conditioning strategy for producing muscle hypertrophy and decreasing intramuscular fat in individuals with SCI (Mahoney et al., 2005; Gorgey et al., 2012). We have shown muscle hypertrophy of the knee extensors (35%) and whole thigh muscle groups (28%), increased leg lean mass, and reduced intramuscular fat and visceral adiposity over the course of 12 weeks of training (Gorgey et al., 2012). Enhancing the development of metabolically active lean muscle mass has the potential to enhance glucose homeostasis and improve lipid profile following SCI (Mahoney et. al., 2005; Gorgey et al., 2012). A decrease in intramuscular fat could also lead to an increased capillary density, which potentially suggests an increase in oxidative capacity. Figure 1 is a representative T1-weighted MRI of the mid-thigh that depicts the baseline and post intervention changes in the thigh, notably skeletal muscle hypertrophy and decreased IMF, over the course of 16 weeks of NMES resistance training (Gorgey et al., unpublished results).
Figure 1.
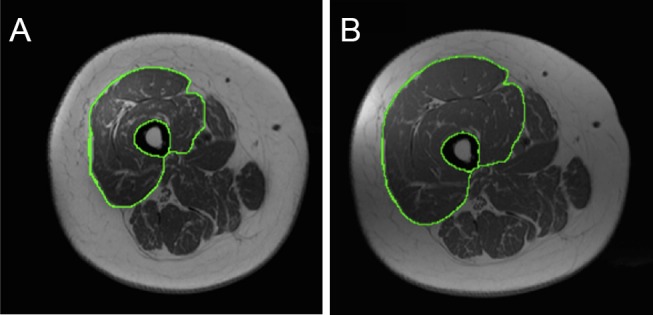
A representative T1-weighted MRI of the mid-thigh (A) pre-training and (B) post-training in an individual with complete spinal cord injury.
The knee extensor muscle group is traced out to highlight the extensive skeletal muscle hypertrophy following 16 weeks of resistance training. Bony and soft tissue landmarks were used to match pre-training and post-training images to ensure the exact anatomical location.
Achieving therapeutic benefits from FES-LEC may be hindered by an inability to produce adequate power while cycling. The amount of power necessary to achieve muscle hypertrophy and shift fast twitch muscle fibers to slow twitch muscle fibers is often unachievable, but this inefficiency may be mitigated with prior conditioning. In order for an individual to generate and increase power output on the FES-LEC, the set resistance must be overcome during active cycling. Unfortunately, due to rapid fatigue, the necessary power generation is often unfeasible without utilizing the servomotor of the FES cycle, which is activated when fatigue is detected. Conditioning via NMES resistance training maintains a realistic method for improving the skeletal musculature prior to beginning FES-LEC and could potentially increase power output and exercise capacity.
An increase in motor unit recruitment has been previously suggested to help increase oxygen uptake (Elder et al., 2006). Training the muscles of the thigh, specifically the knee extensors, could be advantageous and increase motor recruitment, muscular efficiency, and cardio-metabolic profile prior to utilizing the FES cycle. Over the course of 16 weeks, we have preliminary results showing that one participant had an increase of 25% in citrate synthase following resistance training, suggesting that prior conditioning with an emphasis on increasing muscle size may positively influence a shift back to slow oxidative fibers. Although all participants may not experience this shift, future studies should consider the clinical implications of this finding.
Conclusion: Conditioning prior to beginning FES-LEC training has potential to increase the viability of FES-LEC and provide extensive training benefits. NMES, in conjunction with progressive resistance training, is an ideal strategy for conditioning the muscles of the thigh prior to beginning FES-LEC in the SCI population. By employing NMES resistance training as a conditioning stimulus prior to training that elicits muscle hypertrophy, the FES-LEC application will be expanded to potentially improve body composition and cardio-metabolic profile of those with SCI.
We would like to thank Hunter Holmes McGuire Research Institute and Spinal Cord Injury Services and Disorders for providing the environment to conduct clinical human research trials. Ashraf S. Gorgey is currently supported by the Department of Veteran Affairs, Veteran Health Administration, Rehabilitation Research and Development Service (B7867-W) and Department of Defense-CDRMP (# SC140119).
References
- Elder C, Apple D, Bickel C, Meyer R, Dudley G. Intramuscular fat and glucose tolerance after spinal cord injury – a cross-sectional study. Spinal Cord. 2004;42:711–716. doi: 10.1038/sj.sc.3101652. [DOI] [PubMed] [Google Scholar]
- Elder CP, Mahoney ET, Black CD, Slade JM, Dudley GA. Oxygen cost of dynamic or isometric exercise relative to recruited muscle mass. Dyn Med. 2006;5:1–8. doi: 10.1186/1476-5918-5-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorgey AS, Dudley G. Skeletal muscle atrophy and increased intramuscular fat after incomplete spinal cord injury. Spinal Cord. 2007;45:304–309. doi: 10.1038/sj.sc.3101968. [DOI] [PubMed] [Google Scholar]
- Gorgey AS, Lawrence J. Acute responses of functional electrical stimulation cycling on the ventilation-to-CO2 production ratio and substrate utilization after spinal cord injury. PM R. 2016;8:225–234. doi: 10.1016/j.pmrj.2015.10.006. [DOI] [PubMed] [Google Scholar]
- Gorgey AS, Cho G, Dolbow D, Gater D. Differences in current amplitude evoking leg extension in individuals with spinal cord injury. NeuroRehabilitation. 2013;33:161–170. doi: 10.3233/NRE-130941. [DOI] [PubMed] [Google Scholar]
- Gorgey AS, Mather KJ, Cupp HR, Gater DR. Effects of resistance training on adiposity and metabolism after spinal cord injury. Med Sci Sports Exerc. 2012;44:165–174. doi: 10.1249/MSS.0b013e31822672aa. [DOI] [PubMed] [Google Scholar]
- Gorgey AS, Poarch HJ, Dolbow DD, Castillo T, Gater DR. Effect of adjusting pulse durations of functional electrical stimulation cycling on energy expenditure and fatigue after spinal cord injury. J Rehabil Res Dev. 2014;51:1455–1467. doi: 10.1682/JRRD.2014.02.0054. [DOI] [PubMed] [Google Scholar]
- Hasnan N, Ektas N, Tanhoffer AI, Tanhoffer R, Fornusek C, Middleton JW, Husain R, Davis GM. Exercise responses during functional electrical stimulation cycling in individuals with spinal cord injury. Med Sci Sports Exerc. 2013;45:1131–1138. doi: 10.1249/MSS.0b013e3182805d5a. [DOI] [PubMed] [Google Scholar]
- Mahoney ET, Bickel CS, Elder C, Black C, Slade JM, Apple D Jr, Dudley GA. Changes in skeletal muscle size and glucose tolerance with electrically stimulated resistance training in subjects with chronic spinal cord injury. Arch Phys Med Rehabil. 2005;86:1502–1504. doi: 10.1016/j.apmr.2004.12.021. [DOI] [PubMed] [Google Scholar]
- Talmadge RJ, Castro MJ, Apple DF, Jr, Dudley GA. Phenotypic adaptations in human muscle fibers 6 and 24 wk after spinal cord injury. J Appl Physiol (1985) 2002;92:147–154. doi: 10.1152/japplphysiol.000247.2001. [DOI] [PubMed] [Google Scholar]


