The monovalent cation lithium, whose introduction in psychiatry dates back at the end of the 1940s, remains the first-line agent in the management of patients with bipolar disorder (BD). It is effective in the treatment of moderate-to-severe acute mania, prophylactic for recurrent manic and depressive episodes, and reduces the risk of suicide. It can also boost antidepressants effects in the treatment of major depressive disorder (Albert et al., 2014). More recently, a growing body of evidence seems to suggest that the benefits of lithium extend beyond mood stabilization. In vitro, lithium has been shown to provide neuroprotection against excitotoxicity induced by glutamate and N-methyl-D-aspartate (NMDA) receptor activation, calcium, thapsigargin, β-amyloid, aging, serum/growth factor deprivation, low potassium concentration, C2-ceramide, aluminum, ouabain, and specific HIV regulatory proteins. Lithium's neuroprotective effects have further been demonstrated in a series of in vivo animal models of ischemic/hemorrhagic stroke, traumatic brain/spinal cord injury (TBI/SCI), Huntington's disease (HD), Alzheimer's disease (AD), amyotrophic lateral sclerosis (ALS), fragile X syndrome (FXS), Parkinson's disease (PD), retinal degeneration, multiple sclerosis (MS), alcohol-induced degeneration, Down syndrome, spinocerebellar ataxia-1, HIV-associated neurotoxicity, and irradiation (Chiu et al., 2013). In spite of this, very little is understood about its mechanism of action. Recent research findings indicate that lithium's neuroprotective effects may stem, at least in part, from its ability to inhibit the glycogen synthase kinase-3β (GSK-3β) by directly binding to its enzyme's magnesium-sensitive site and indirectly by enhancing phosphorylation of this kinase at specific serine residues. Indeed lithium's direct inhibition of GSK-3β leads to activation of several transcription factors, including cyclic adenosine monophosphate (cAMP) response element binding protein (CREB), heat-shock factor-1 (HSF-1), and β-catenin, with subsequent induction of major neurotrophic, angiogenic, anti-inflammatory, and anti-apoptotic factors such as brain-derived neurotrophic factor (BDNF), nerve growth factor (NGF), glial cell line-derived neurotrophic factor (GDNF), vascular endothelial growth factor (VEGF), heat shock protein 70 (HSP70), and B-cell lymphoma/leukemia-2 protein (Bcl-2), respectively. Suppressed GSK-3β further reduces the activity of the pro-apoptotic proteins p53 and Bax and their negative regulatory action on Bcl-2. Noteworthy, BDNF and NGF have been reported to function as both downstream molecules resulting from the inhibition of GSK-3β and upstream signals able to inhibit this molecular pathway via specific survival signaling cascades such as the phosphatidylinositol-3-kinase (PI3K)/Akt and the MAP kinase (MEK)/ERK pathways. Lithium also indirectly inhibits GSK-3β via PI3K-dependent activation of protein kinase C (PKC), cAMP-dependent activation of protein kinase A (PKA), and the Wnt/β-catenin pathway (via Frizzled receptors). On the other hand, by decreasing inositol 1,4,5-trisphosphate (IP3) levels, lithium has been shown to induce autophagy, a sort of ‘quality control’ process believed to be particularly important in neurodegenerative disorders such as HD, AD, ALS, and PD characterized by the accumulation of misfolded disease-causing proteins. In these same neurodegenerative disorders as well as in stroke, TBI/SCI, retinal degeneration, MS, and HIV, lithium inhibits glutamate-induced excitotoxicity mediated by NMDA receptors, specifically attenuating the NR2B subunit constitutive tyrosine phosphorylation, and subsequent calcium influx, thus suppressing excitotoxicity-induced p38 and c-Jun N-terminal kinase (JNK), and subsequent transcription factor activator protein-1 (AP-1) activation to block neuronal apoptosis. Inhibition of oxidative stress, implicated in numerous central nervous system (CNS) disorders such as BD, stroke, TBI/SCI, HD, AD, and ALS may further underlie lithium beneficial effects towards these pathologies (Chiu et al., 2013, Figure 1).
Figure 1.
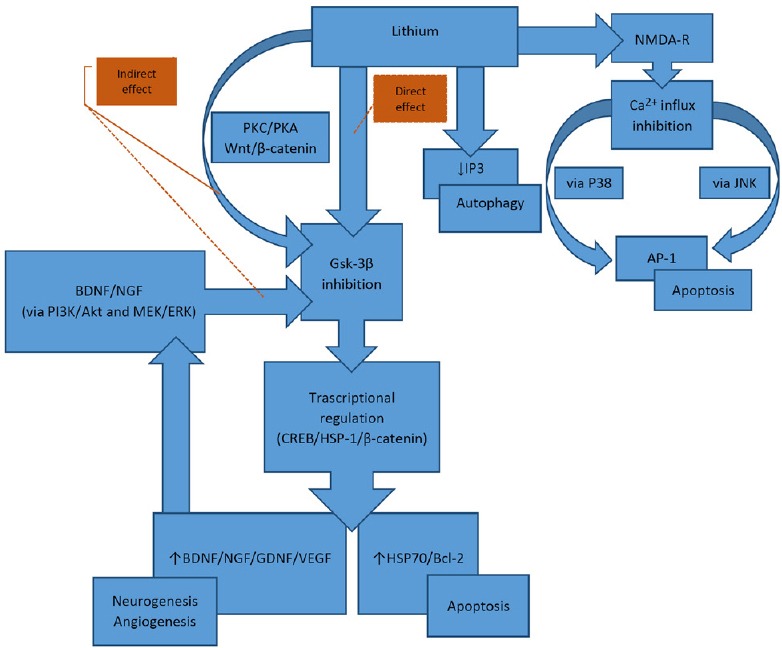
Overview of the proposed mechanisms underlining lithium neuroprotective effects.
Through the direct/indirect inhibition of glycogen synthase kinase-3β (GSK- 3β), lithium is hypothesized to disinhibit several transcription factors, including cyclic adenosine monophosphate (cAMP) response element binding protein (CREB), heat-shock factor-1 (HSF-1), and β-catenin, with subsequent induction of major neurotrophic, angiogenic, anti-inflammatory, and anti-apoptotic factors such as brain-derived neurotrophic factor (BDNF), nerve growth factor (NGF), glial cell line-derived neurotrophic factor (GDNF), vascular endothelial growth factor (VEGF), heat shock protein 70 (HSP70), and B-cell lymphoma/leukemia-2 protein (Bcl-2), respectively. Lithium also indirectly inhibits GSK-3β via PI3K-dependent activation of protein kinase C (PKC), cAMP-dependent activation of protein kinase A (PKA), and the Wnt/β-catenin path way. The ability of lithium to decrease inositol 1,4,5-trisphosphate (IP3) levels has also been shown to induce autophagy. Furthermore, lithium inhibits glutamate-induced excitotoxicity mediated by NMDA receptors and subsequent calcium influx, thus suppressing excitotoxicity-induced p38 and c-Jun N-terminal kinase (JNK), and subsequent transcription factor activator protein-1 (AP-1) activation to block neuronal apoptosis.
In contrast to preclinical studies, clinically based evidence of lithium neuroprotective effects are still limited and typically restricted to patients with BD. The most replicated finding from structural neuroimaging studies is an association between long-term lithium treatment and increased gray matter volume in brain areas implicated in emotional processing and cognitive control such as the anterior cingulate, ventral prefrontal cortex, paralimbic association cortex, superior temporal gyri, amygdala, and hippocampus, which suggests that lithium has considerable neuroprotective and/or neurotrophic effects (Chiu et al., 2013). Noteworthy, in the study by Benedetti et al. (2015), long-term lithium treatment and the less active GSK-3β rs334558*G gene promoter variant were found to be synergistically associated with increased frontal lobe gray matter volumes in patients with BD. N-acetyl-aspartate, a putative marker for neuronal viability and function, was also reported to be increased in the brain of patients with BD after lithium treatment (Hajek et al., 2012). With regard to the effects of lithium on cognition, data are at present somewhat ambiguous. Conclusions from a recent meta-analysis point overall towards various cognitive deficits in psychiatric patients, as well as in normal volunteers treated with lithium, across the areas of immediate verbal learning and memory, creativity, and psychomotor speed (Wingo et al., 2009). However, there is also evidence for better/improved executive functions and memory, mostly related to the activity of prefrontal cortex and medial temporal lobe respectively, in lithium treated BD patients (Rybakowski et al., 2009).
In our cross-sectional study (Bersani et al., 2016), results obtained seem to confirm a potential medial temporal lobe neuroprotective effects of lithium in patients with BD. Subjects enrolled were 15 euthymic BD patients undergoing long-term clinical maintenance treatment with lithium (for at least 12 months), 15 matched patients treated with other mood-stabilizing drugs and who had never received lithium, and 15 matched healthy subjects. Cognitive functions were assessed using the Cambridge Neuropsychological Test Automated Battery(CANTAB) tests of visual memory [Paired Associates Learning (PAL); Delayed Matching to Sample (DMS)], executive functions [Spatial Span (SSP); Spatial Working Memory (SWM); and Stocking of Cambridge (SOC)], attention [Rapid Visual Information Processing (RVIP) and Intra/Extradimensional set shift (IED)], decision making [Information Sampling Task (IST)] and response inhibition [Stop Signal Task (SST)]. Taken together, BD patients demonstrated robust deficits in the visual episodic memory PAL and executive functions SSP, SWM, and SOC tests. Once subdivided in treatment subgroups, only non-lithium treated BD patients demonstrated impairments in the visual episodic memory PAL test. Covarying for lifetime antipsychotic medication did not change the outcome. Noteworthy, successful performance on the PAL test is dependent on functional integrity of the medial temporal lobe. Evidence from lesion studies in rats, monkeys, and humans, as well as functional imaging studies in normal human volunteers, suggest that medial temporal lobe structures, such as the hippocampus, parahippocampal gyrus and enthorinal cortex are implicated in the main cognitive component of this test. Across a number of studies, the PAL test has also been shown to be particularly effective (sensitivity = 100%; specificity = 92%) in differentiating early AD from healthy older adults and it is now one of the most widely used test in assessing the integrity of the hippocampal memory formation (Junkkila et al., 2012). In line with our findings, suggestions have been advanced that, in patients with BD, a continued lithium treatment may exert a preventing action against the onset of dementia (Nunes et al., 2007). Always in this context, a following study by Nunes et al. (2013) has demonstrated how a microdose lithium treatment (300 μg per day) administered for a period of 15 months may be able to prevent cognitive loss in patients with AD. Indeed, lithium treatment has been shown to present disease-modifying effects in AD, mainly by the modification of its pathophysiology via inhibition of the overactive GSK-3, which definitely has been related to amyloid precursor protein processing and tau hyperphosphorylation, and by the provision of neurotrophic and neuroprotective support. It is a fact that clinical trials of lithium in AD and other neurodegenerative illnesses are now under way, unfortunately, up to date, with conflicting results. Methodological issues including small samples size, the use of diverse research designs and/or the lack of consistency in most of the neuropsychological tests administered could be at the base of such outcomes. With regard to prefrontal cortex and associated executive functions, even though a favorable effect of lithium has been suggested also for this cognitive domain, in our study, both BD treatment groups have showed moderately impaired working memory and strategy use. In the study by Rybakowski et al. (2009), better indexes of executive functions were showed in persons who benefited from long-term lithium therapy compared with lithium non-responders. In contrast, our lithium-treated BD patients did not seem to benefit of such a positive effect. Of note, subjects included in the aforementioned study were a group of patients with a mean of 15 years of lithium treatment, which certainly enables a more accurate assessment of lithium cognitive positive effect. Moreover, neither the research design nor the neuropsychological assessment is comparable between our study and that of these authors. With regard to attention and decision-making/response inhibition, an absence of a favorable effect of lithium was seen in our patients. At the same time, lithium did not seem to affect these two cognitive domains.
To the best of our knowledge, our study is the first to have demonstrated, by means of a highly sensitive test of visual memory, a potential hippocampus neuroprotective effect of lithium in patients with BD. Undoubtedly, other studies are needed to finally recognize lithium as a potential cognitive enhancer. Future studies should include, apart from highly sensitive cognitive tests, specific neurotrophic biomarkers, such as BDNF, NGF, etc. Finally, it will be of outmost importance to evaluate the minimal length of treatment and the optimum serum level in order to combine potential clinical benefit and, particularly for older patients, clinical safety.
References
- Albert U, De Cori D, Blengino G, Bogetto F, Maina G. Lithium treatment and potential long-term side effects: a systematic review of the literature. Riv Psichiatr. 2014;49:12–21. doi: 10.1708/1407.15620. [DOI] [PubMed] [Google Scholar]
- Benedetti F, Poletti S, Radaelli D, Locatelli C, Pirovano A, Lorenzi C, Vai B, Bollettini I, Falini A, Smeraldi E, Colombo C. Lithium and GSK-3β promoter gene variants influence cortical gray matter volumes in bipolar disorder. Psychopharmacology (Berl) 2015;232:1325–1336. doi: 10.1007/s00213-014-3770-4. [DOI] [PubMed] [Google Scholar]
- Bersani G, Quartini A, Zullo D, Iannitelli A. Potential neuroprotective effect of lithium in bipolar patients evaluated by neuropsychological assessment: preliminary results. Hum Psychopharmacol. 2016;31:19–28. doi: 10.1002/hup.2510. [DOI] [PubMed] [Google Scholar]
- Chiu CT, Wang Z, Hunsberger JG, Chuang DM. Therapeutic potential of mood stabilizers lithium and valproate acid: beyond bipolar disorder. Pharmacol Rev. 2013;65:105–142. doi: 10.1124/pr.111.005512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajek T, Bauer M, Pfenning A, Cullis J, Ploch J, O’Donovan C, Bohner G, Klingebiel R, Young LT, Macqueen GM, Alda M. Large positive effect of lithium on prefrontal cortex N-acetylaspartate in patients with bipolar disorder: 2-centre study. J Psychiatry Neurosci. 2012;37:185–192. doi: 10.1503/jpn.110097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Junkkila J, Oja S, Laine M, Karrasch M. Applicability of the CANTAB-PAL computerized memory test in identifying amnestic mild cognitive impairment and Alzheimer's disease. Dement Geriatr Cogn Disord. 2012;34:83–89. doi: 10.1159/000342116. [DOI] [PubMed] [Google Scholar]
- Nunes MA, Viel TA, Buck HS. Microdose lithium treatment stabilized cognitive impairment in patients with Alzheimer's disease. Curr Alzheimer Res. 2013;10:104–107. doi: 10.2174/1567205011310010014. [DOI] [PubMed] [Google Scholar]
- Nunes PV, Forlenza OV, Gattaz WF. Lithium and risk for Alzheimer's disease in elderly patients with bipolar disorder. Br J Psychiatry. 2007;190:359–360. doi: 10.1192/bjp.bp.106.029868. [DOI] [PubMed] [Google Scholar]
- Rybakowski JK, Permoda-Osip A, Borkowska A. Response to prophylactic lithium in bipolar disorder may be associated with a preservation of executive cognitive functions. Eur Neuropsychopharmacol. 2009;19:791–795. doi: 10.1016/j.euroneuro.2009.06.002. [DOI] [PubMed] [Google Scholar]
- Wingo AP, Wingo TS, Harvey PD, Baldessarini RJ. Effects of lithium on cognitive performance: a meta-analysis. J Clin Psychiatry. 2009;70:1588–1597. doi: 10.4088/JCP.08r04972. [DOI] [PubMed] [Google Scholar]


