Abstract
Restoration of anteroposterior laxity after an anterior cruciate ligament reconstruction has been predictable with traditional open and endoscopic techniques. However, anterolateral rotational stability has been difficult to achieve in a subset of patients, even with appropriate anatomic techniques. Therefore, differing techniques have attempted to address this rotational laxity by augmenting or reconstructing lateral-sided structures about the knee. In recent years, there has been a renewed interest in the anterolateral ligament as a potential contributor to residual anterolateral rotatory instability in anterior cruciate ligament–deficient patients. Numerous anatomic and biomechanical studies have been performed to further define the functional importance of the anterolateral ligament, highlighting the need for surgical techniques to address these injuries in the unstable knee. This article details our technique for an anatomic anterolateral ligament reconstruction using a semitendinosus tendon allograft.
Anterior cruciate ligament (ACL) tears requiring surgical intervention are commonly encountered in young athletes, and it is estimated that 200,000 ACL reconstructions are performed each year in the United States. Whereas technological advances have allowed for endoscopic ACL reconstruction, these injuries were historically treated with lateral extra-articular tenodesis procedures to prevent both anterolateral rotatory instability and anterior tibial translation.1 Despite the early enthusiasm for these techniques, they subsequently fell out of favor because they did not reproduce the native anatomy, and long-term outcome studies reported residual instability, overconstraint of the lateral compartment, and graft failure.2, 3, 4, 5
However, recent publications have stimulated renewed discussion regarding the anterolateral soft-tissue structures of the knee. In 2013 Claes et al.6 described the anatomic location and function of the anterolateral ligament (ALL). This work built on prior studies by numerous authors who have described an extra-articular structure in the lateral knee extending from the lateral epicondyle of the femur to the lateral tibia that may contribute to translational and rotatory stability in conjunction with the ACL.7, 8 Although previously recognized, the “rediscovery” of the synergistic relation between the anterolateral structures and ACL in controlling anterolateral rotatory stability has led to renewed interest in lateral extra-articular tenodesis procedures9 and specifically reconstruction of the ALL.
Biomechanical studies have shown that the ALL is an important stabilizer of internal rotation at knee flexion angles greater than 35°; however, it has limited function in resisting anterior translation.10 This stabilizing function may account for a small subset of patients who have continued anterolateral rotatory instability, as shown by a positive pivot-shift examination, after an appropriately performed ACL reconstruction. In this small subset of patients, ALL reconstruction can provide increased knee stability and allow for improved knee function. The purpose of this study was to describe our technique for an anatomic ALL reconstruction.
Surgical Technique
Operative Indications
Surgical indications for ALL reconstruction include a 3+ pivot shift in an ACL-deficient knee and cases of multiple revision ACL reconstructions with residual pivot shift and continued clinically significant instability after ACL reconstruction. In all cases, other causes of increased anterolateral rotation on the pivot shift, such as a deficient lateral meniscus or a concurrent posterolateral knee injury, should be ruled out.
Patient Positioning and Anesthesia
The patient is placed in a supine position with the injured leg in a leg holder (Mizuho OSI, Union City, CA), with the nonsurgical leg flexed, abducted, and held in an abduction holder (Birkova Products, Gothenburg, NE) (Video 1). A well-padded thigh tourniquet is subsequently placed on the upper thigh of the operative leg. The surgical leg is prepared and draped in the usual sterile fashion, the leg is exsanguinated, and the tourniquet is inflated.
ALL Reconstruction
After confirmation of significant anterolateral rotatory instability, an ALL reconstruction is undertaken. A lateral hockey-stick incision is made through the skin along the iliotibial band (ITB) and is extended distally between the lateral fibular head and Gerdy's tubercle (Fig 1).
Fig 1.
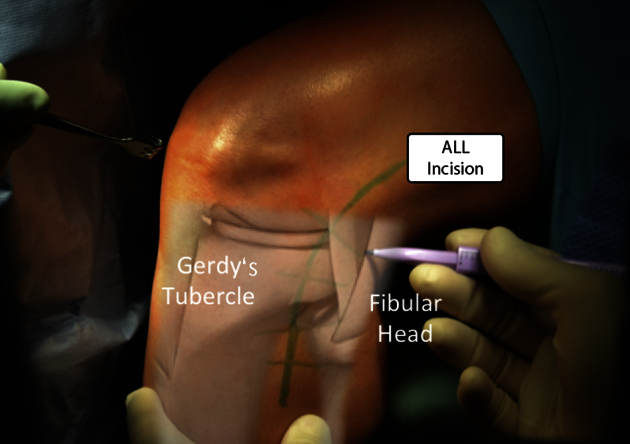
A left knee with a superimposed schematic view of the anatomic landmarks and the surgeon's incision outline. (ALL, anterolateral ligament.)
Sharp dissection is performed down to the fascia overlying the ITB. Full-thickness skin flaps with subcutaneous tissue are made anteriorly and posteriorly. The posterior skin flap should have sufficient subcutaneous tissue and vascularity to support wound healing and avoid skin necrosis postoperatively. Because this surgical procedure is often performed in revision settings, adhesions can be encountered and careful dissection should be performed.
The joint line is then identified with the aid of a spinal needle. The tibial attachment site of the ALL is identified, equidistant between the center of the Gerdy tubercle and the anterior margin of the fibular head, 9.5 mm distal to the joint line11 (Fig 2).
Fig 2.
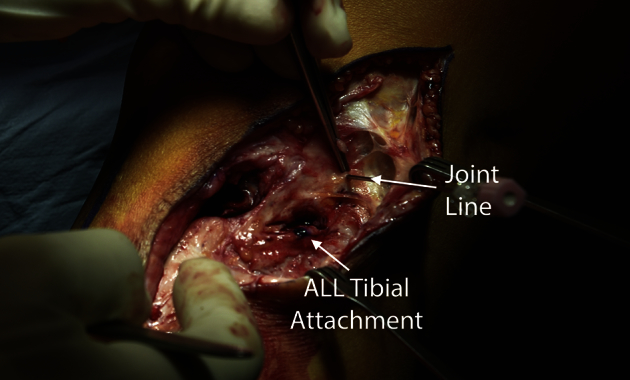
Identification of the joint line is achieved with the aid of a spinal needle in a left knee. The tibial attachment site of the anterolateral ligament (ALL) is located equidistant between the center of Gerdy's tubercle and the anterior margin of the fibular head (9.5 mm distal to the joint line11).
Subsequently, dissection of the soft tissues down to the bone is performed. With the assistance of an ACL aiming device, a guide pin is placed at the distal anatomic insertion aiming toward the superomedial tibia (Fig 3). A 6-mm-diameter reamer (Arthrex, Naples, FL) is used to create a tunnel to a depth of 30 mm.
Fig 3.

An anterior cruciate ligament aiming device is used in a left knee to position the tibial tunnel. A guide pin is placed at the anatomic attachment aiming toward the superomedial tibia.
Next, a path is created underneath the superficial layer of the ITB using gentle blunt dissection. A proximal exit point is created slightly posterior to the proximal fibular collateral ligament (FCL) attachment (identified by applying valgus force to the knee) by making a 3-cm incision through the superficial layer of the ITB. The ALL's femoral attachment is located 4.7 mm proximal and posterior to the FCL's femoral insertion as described by Kennedy et al.11 An eyelet pin is drilled into the femur, aiming anteriorly and proximally to avoid the trochlea and a potential collision with an ACL tunnel (Fig 4).
Fig 4.
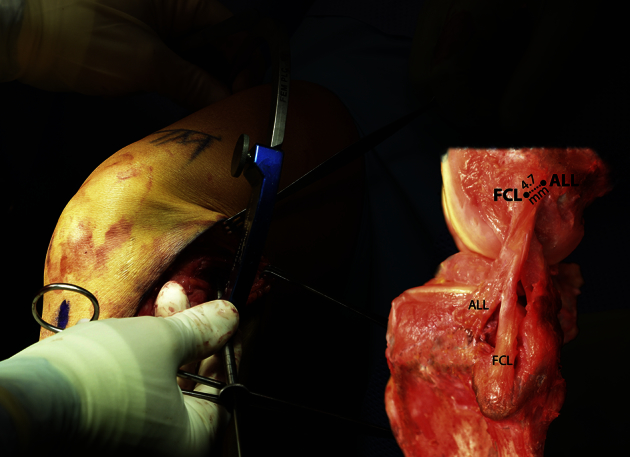
The anterolateral ligament (ALL) courses superficially to the fibular collateral ligament (FCL), and its femoral attachment is located 4.7 mm proximal and posterior to the FCL's femoral insertion as described by Kennedy et al.,11 as shown in the anatomic picture on the right (left knee). As shown on the left, an eyelet pin is drilled into the femur, aiming anteriorly and proximally on the femoral anatomic attachment in a left knee.
A closed-socket tunnel is created with a 6-mm reamer (Arthrex), again to a depth of 30 mm. The tunnel is then tapped to prevent graft injury during interference screw fixation due to the hard cortical bone in the femur at this location. The inter-tunnel distance is measured to prepare the graft length accordingly (Fig 5). In our hands, it is usually 11 cm long.
Fig 5.
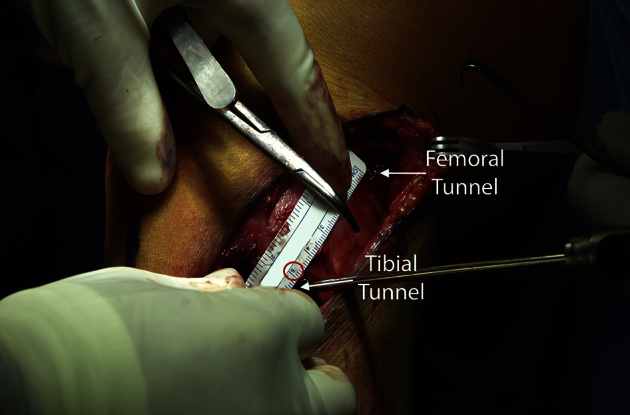
The inter-tunnel distance (femoral to tibial tunnel) is measured to prepare the graft accordingly in a left knee.
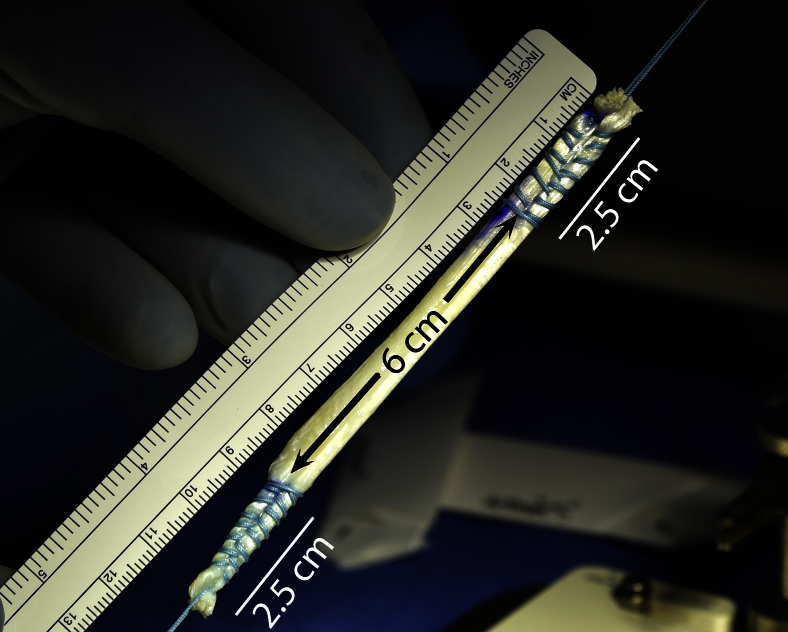
Graft Preparation
A semitendinosus tendon allograft (Allosource, Centennial, CO) is used and prepared based on the previously measured inter-tunnel (femoral and tibial) distances with the addition of 25 mm on each end for the tunnels. Both ends are whipstitched and tubularized (25 mm) with No. 2 polyethylene-polyester suture (FiberWire; Arthrex). The redundant tissue can then be excised (Fig 6). Alternatively, a semitendinosus autograft can also be used if it was not previously harvested.
Fig 6.
Prepared semitendinosus tendon allograft. Both ends are whipstitched with FiberWire suture. The size of the allograft depends on the inter-tunnel distance (femoral to tibial tunnel) previously measured.
ALL Graft Passage and Fixation
The graft is fixed distally in the tibia with a 7 × 23–mm Bio-Interference screw (Arthrex). Traction is applied to the graft to ensure sturdy fixation (Fig 7). The graft is then passed between the superficial layer of the ITB and FCL (Fig 8). Lastly, the graft is inserted into the femoral tunnel with the help of the previously placed passing suture and secured with a 7 × 23–mm Bio-Interference screw in 30° of knee flexion (Fig 9).
Fig 7.
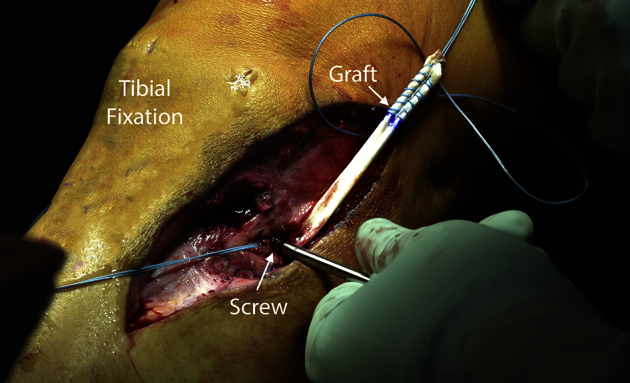
The graft is fixed in the tibial tunnel with a 7 × 23–mm Bio-Interference screw in a left knee.
Fig 8.
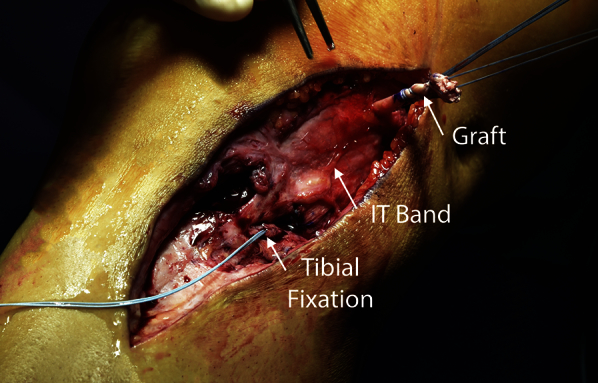
The semitendinosus allograft is being passed deep to the superficial layer of the iliotibial (IT) band in a left knee.
Fig 9.
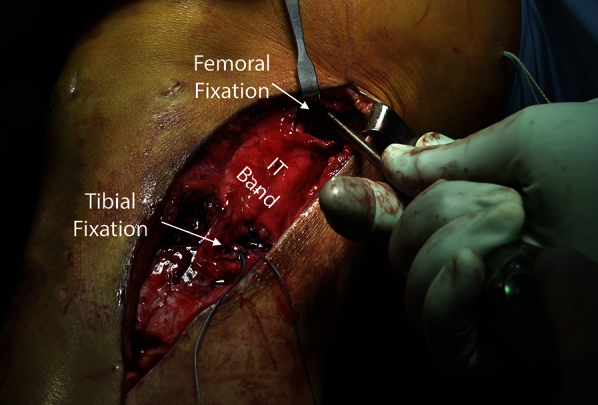
With the knee in 30° of flexion, the anterolateral ligament graft is secured with a 7 × 23–mm biointerference screw. (IT, iliotibial.)
Once fixation is complete, the knee is assessed through a complete range of motion and rotational stability is tested with the pivot-shift test for comparison to the preoperative state. Pearls and pitfall of this surgical technique are summarized in Table 1.
Table 1.
Pearls and Pitfalls
| Pearls |
| A comprehensive understanding of the anatomy is essential because ALL reconstruction is often performed in revision surgery settings and adhesions are often encountered. |
| The tibial attachment site of the ALL is at the midpoint between the center of Gerdy's tubercle and the anterior margin of the fibular head. |
| Applying a varus force to the knee will help identify the FCL, which can be used as a landmark to locate the femoral ALL attachment. |
| The ALL graft is passed deep to the superficial layer of the iliotibial band and superficial to the FCL. |
| Pitfalls |
| If the femoral tunnel pin is not aimed anterior and proximal, it can collide with an anterior cruciate ligament tunnel or damage the trochlea. |
| Higher degrees of overconstraint are observed with ALL graft fixation at higher degrees of flexion. |
| It is essential to clear the attachment sites of all soft tissues to place the tunnels at the proper location and aid with screw insertion. |
| Identification of the femoral attachment of the FCL should be performed to avoid iatrogenic injury to it when reaming the ALL reconstruction tunnel. |
ALL, anterolateral ligament; FCL, fibular collateral ligament.
Postoperative Rehabilitation
After surgery, the patient is allowed to bear weight immediately and there are no restrictions on range of motion. Crutches are used as needed for the first 4 weeks postoperatively or until the patient is comfortable walking without assistance. As soon as the patient can perform a straight leg raise without an extension lag, he or she can discontinue using a knee immobilizer and be placed into an ACL brace (CTi brace; Ossur, Reykjavik, Iceland). A supervised physical therapy program is prescribed for 3 months. Because most patients who qualify for an ALL reconstruction also undergo a concurrent ACL revision reconstruction, the postoperative ACL revision protocol will most often dictate the ongoing rehabilitation program. Physical therapy is designed to emphasize early range of motion and strengthening exercises.
Discussion
This article details our technique for an anatomic ALL reconstruction of the knee. Once thought of as simply a capsular thickening without a well-defined biomechanical role, there has been renewed interest regarding this structure in recent years, with a number of studies evaluating its incidence of injury, anatomic features, biomechanical properties, and functional role as a lateral stabilizer of the tibiofemoral joint.11 As our knowledge on treatment of the unstable knee continues to evolve, we recommend anatomic reconstruction of the ALL in cases with residual anterolateral rotatory instability on the pivot-shift test after or in conjunction with an ACL reconstruction to restore native knee kinematics and improve patient outcomes.
Segond12 first described an avulsion fracture pattern of the proximal-lateral tibia in 1879, which was reported to have a pathognomonic association with ACL tears over 100 years later.13, 14 Until recently, the anatomic structure responsible for this bony avulsion pattern was poorly understood.15, 16 Reports of the presence of a distinct structure with well-defined origin and insertion sites began to emerge in the early 21st century; it was termed the “anterolateral ligament.”6 Further studies showed the ALL to play an important role in anterior and rotational stability about the knee, especially in cases with concomitant ACL injuries.10 Residual anterolateral rotatory instability after ACL reconstruction led to a renewed interest in the functional role of the ALL and the development of surgical techniques to address this pathology.
LaPrade et al.11 performed an anatomic, radiographic, and biomechanical analysis of the structural properties of the ALL. They found the femoral origin was located 4.7 mm posterior and proximal to the FCL attachment and then coursed distally to attach at the anterolateral tibia midway between the Gerdy tubercle and the anterior margin of the fibular head.11 On anteroposterior radiographs, the ALL originated on the femur 22.3 mm proximal to the joint line and inserted on the tibia 13.1 mm distal to the lateral tibial plateau.11 On the lateral view, the femoral attachment was 8.4 mm posterior and proximal to the lateral epicondyle, whereas the tibial attachment was 19.0 mm posterior and superior to the center of the Gerdy tubercle. The biomechanical properties of the ALL showed a mean maximum load of 175 N with a stiffness of 20 N/mm. Importantly, the ALL was reproducibly identified in relation to surrounding anatomic and osseous landmarks to guide proper graft placement when performing reconstruction procedures, and the biomechanical properties suggest most traditional soft-tissue grafts are of sufficient strength.
Given this recent literature, we recommend our approach for anatomic reconstruction of the ALL of the knee for residual anterolateral rotatory instability after ACL reconstruction or in patients with ACL deficiency and a 3+ pivot shift on clinical examination. In most cases, these indications would apply to those undergoing revision ACL reconstruction. However, future long-term studies with larger samples are needed to assess the efficacy and patient-reported outcome measures after ALL reconstruction.
Footnotes
The authors report the following potential conflict of interest or source of funding: R.F.L. receives support from Arthrex; Smith & Nephew; Ossur; Health East, Norway; and an NIH R13 grant for biologics.
Supplementary Data
The patient is placed in a supine position with the injured leg in a leg holder; the nonsurgical leg is flexed at the knee and hip joints, abducted, and secured in an abduction holder. A lateral hockey-stick incision is made through the skin along the iliotibial band (ITB) and is extended distally between the lateral fibular head and the Gerdy tubercle. Sharp dissection is performed down to the fascia overlying the ITB. The joint line is then identified with the aid of a spinal needle. The tibial attachment site of the anterolateral ligament (ALL) is identified, equidistant between the center of the Gerdy tubercle and the anterior margin of the fibular head, 9.5 mm distal to the joint line. An anterior cruciate ligament aiming device is used to insert a guide pin at the distal anatomic insertion, aiming toward the superomedial tibia. A 6-mm-diameter reamer is used to create a tunnel to a depth of 30 mm. A path is created underneath the superficial layer of the ITB using gentle blunt dissection and exiting just posterior to the femoral fibular collateral ligament (FCL) attachment by making a 3-cm incision through the superficial layer of the ITB. The ALL's femoral attachment is located 4.7 mm proximal and posterior to the FCL's femoral insertion. An eyelet pin is drilled into the femur, aiming anteriorly and proximally. A closed-socket tunnel is created with a 6-mm reamer, again to a depth of 30 mm. To prepare the graft length accordingly, the inter-tunnel distance is measured and 50 mm is added to the calculation to account for 25 mm of graft that will be placed in each tunnel. A semitendinosus tendon allograft is used, and both ends (25 mm) are whipstitched and tubularized. The graft is fixed distally in the tibia with a 7 × 23–mm Bio-Interference screw. The graft is then passed between the superficial layer of the ITB and FCL. It is inserted into the femoral tunnel with the help of the previously placed passing suture and secured with a 7 × 23–mm Bio-Interference screw.
References
- 1.Chambat P., Guier C., Sonnery-Cottet B., Fayard J.M., Thaunat M. The evolution of ACL reconstruction over the last fifty years. Int Orthop. 2013;37:181–186. doi: 10.1007/s00264-012-1759-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Strum G.M., Fox J.M., Ferkel R.D. Intraarticular versus intraarticular and extraarticular reconstruction for chronic anterior cruciate ligament instability. Clin Orthop Relat Res. 1989:188–198. [PubMed] [Google Scholar]
- 3.Andrews J.R., Sanders R.A., Morin B. Surgical treatment of anterolateral rotatory instability. A follow-up study. Am J Sports Med. 1985;13:112–119. doi: 10.1177/036354658501300206. [DOI] [PubMed] [Google Scholar]
- 4.Benum P. Anterolateral rotary instability of the knee joint. Results after stabilization by extraarticular transposition of the lateral part of the patellar ligament. A preliminary report. Acta Orthop Scand. 1982;53:613–617. doi: 10.3109/17453678208992267. [DOI] [PubMed] [Google Scholar]
- 5.Amirault J.D., Cameron J.C., MacIntosh D.L., Marks P. Chronic anterior cruciate ligament deficiency. Long-term results of MacIntosh’s lateral substitution reconstruction. J Bone Joint Surg Br. 1988;70:622–624. doi: 10.1302/0301-620X.70B4.3403611. [DOI] [PubMed] [Google Scholar]
- 6.Claes S., Vereecke E., Maes M., Victor J., Verdonk P., Bellemans J. Anatomy of the anterolateral ligament of the knee. J Anat. 2013;223:321–328. doi: 10.1111/joa.12087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Terry G.C., Hughston J.C., Norwood L.A. The anatomy of the iliopatellar band and iliotibial tract. Am J Sports Med. 1986;14:39–45. doi: 10.1177/036354658601400108. [DOI] [PubMed] [Google Scholar]
- 8.Vincent J.P., Magnussen R.A., Gezmez F. The anterolateral ligament of the human knee: An anatomic and histologic study. Knee Surg Sports Traumatol Arthrosc. 2012;20:147–152. doi: 10.1007/s00167-011-1580-3. [DOI] [PubMed] [Google Scholar]
- 9.Samuelson M., Draganich L.F., Zhou X., Krumins P., Reider B. The effects of knee reconstruction on combined anterior cruciate ligament and anterolateral capsular deficiencies. Am J Sports Med. 1996;24:492–497. doi: 10.1177/036354659602400414. [DOI] [PubMed] [Google Scholar]
- 10.Parsons E.M., Gee A.O., Spiekerman C., Cavanagh P.R. The biomechanical function of the anterolateral ligament of the knee. Am J Sports Med. 2015;43:NP22. doi: 10.1177/0363546514562751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kennedy M.I., Claes S., Fuso F.A. The anterolateral ligament: An anatomic, radiographic, and biomechanical analysis. Am J Sports Med. 2015;43:1606–1615. doi: 10.1177/0363546515578253. [DOI] [PubMed] [Google Scholar]
- 12.Segond P. Aux Bureaux du Progrès Médical; Paris: 1879. Recherches cliniques et expérimentales sur les épanchements sanguins du genou par entorse. [Google Scholar]
- 13.Hess T., Rupp S., Hopf T., Gleitz M., Liebler J. Lateral tibial avulsion fractures and disruptions to the anterior cruciate ligament. A clinical study of their incidence and correlation. Clin Orthop Relat Res. 1994:193–197. [PubMed] [Google Scholar]
- 14.Goldman A.B., Pavlov H., Rubenstein D. The Segond fracture of the proximal tibia: A small avulsion that reflects major ligamentous damage. AJR Am J Roentgenol. 1988;151:1163–1167. doi: 10.2214/ajr.151.6.1163. [DOI] [PubMed] [Google Scholar]
- 15.LaPrade R.F., Gilbert T.J., Bollom T.S., Wentorf F., Chaljub G. The magnetic resonance imaging appearance of individual structures of the posterolateral knee. A prospective study of normal knees and knees with surgically verified grade III injuries. Am J Sports Med. 2000;28:191–199. doi: 10.1177/03635465000280020901. [DOI] [PubMed] [Google Scholar]
- 16.Terry G.C., LaPrade R.F. The posterolateral aspect of the knee. Anatomy and surgical approach. Am J Sports Med. 1996;24:732–739. doi: 10.1177/036354659602400606. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient is placed in a supine position with the injured leg in a leg holder; the nonsurgical leg is flexed at the knee and hip joints, abducted, and secured in an abduction holder. A lateral hockey-stick incision is made through the skin along the iliotibial band (ITB) and is extended distally between the lateral fibular head and the Gerdy tubercle. Sharp dissection is performed down to the fascia overlying the ITB. The joint line is then identified with the aid of a spinal needle. The tibial attachment site of the anterolateral ligament (ALL) is identified, equidistant between the center of the Gerdy tubercle and the anterior margin of the fibular head, 9.5 mm distal to the joint line. An anterior cruciate ligament aiming device is used to insert a guide pin at the distal anatomic insertion, aiming toward the superomedial tibia. A 6-mm-diameter reamer is used to create a tunnel to a depth of 30 mm. A path is created underneath the superficial layer of the ITB using gentle blunt dissection and exiting just posterior to the femoral fibular collateral ligament (FCL) attachment by making a 3-cm incision through the superficial layer of the ITB. The ALL's femoral attachment is located 4.7 mm proximal and posterior to the FCL's femoral insertion. An eyelet pin is drilled into the femur, aiming anteriorly and proximally. A closed-socket tunnel is created with a 6-mm reamer, again to a depth of 30 mm. To prepare the graft length accordingly, the inter-tunnel distance is measured and 50 mm is added to the calculation to account for 25 mm of graft that will be placed in each tunnel. A semitendinosus tendon allograft is used, and both ends (25 mm) are whipstitched and tubularized. The graft is fixed distally in the tibia with a 7 × 23–mm Bio-Interference screw. The graft is then passed between the superficial layer of the ITB and FCL. It is inserted into the femoral tunnel with the help of the previously placed passing suture and secured with a 7 × 23–mm Bio-Interference screw.