Abstract
The plantar calcaneonavicular ligament, also known as the spring ligament, is an important static stabilizer of the medial longitudinal foot arch. Compromise of this ligament is a primary causative factor of peritalar subluxation, and it should be repaired in addition to treatment of tibialis posterior tendon abnormalities. Open repair of the ligament requires extensive soft-tissue dissection. The development of the high distal portal for posterior tibial tendoscopy allows repair of the ligament endoscopically. This, together with endoscopically assisted reconstruction of the tibialis posterior tendon, allows complete endoscopic treatment of stage 2 posterior tibial tendon deficiency. The major structure at risk is the medial plantar nerve. This technique is technically demanding and should be reserved for experienced foot and ankle arthroscopists.
The spring (plantar calcaneonavicular) ligament is a thick ligament that extends from the undersurface of the sustentaculum tali to the inferior and medial edges of the talar facet of the navicular.1 It consists of the superomedial calcaneonavicular ligament, medioplantar oblique ligament, and inferior calcaneonavicular ligament.2, 3 The superomedial and inferior calcaneonavicular ligaments are the consistent medial and lateral components of the spring ligament. The medioplantar oblique ligament is thinner and is seen less consistently.3
Although injury to the spring ligament is commonly due to the failure of the tibialis posterior tendon in adult-acquired flatfoot deformity, isolated injury to the ligament with a normal tibialis posterior tendon has been reported.4, 5, 6 Repair of the spring ligament is indicated in case of a torn ligament with or without tibialis posterior tendon deficiency. However, an open approach to the ligament requires extensive soft-tissue dissection. We report the technique for endoscopic repair of the spring ligament and superficial deltoid ligament. This can be incorporated into posterior tibial tendoscopy7 and endoscopically assisted reconstruction of the tibialis posterior tendon.8
Technique
Step 1: Preoperative Planning
Preoperative magnetic resonance imaging is important for gauging the extent of the disease and surgical planning.
Step 2: Patient Positioning and Setup
The patient is placed in the supine position with the legs spread. A thigh tourniquet is applied to provide a bloodless surgical field. A 2.7-mm 30° arthroscope (Henke Sass Wolf, Tuttlingen, Germany) is used for this procedure.
Step 3: Portal Placement for Posterior Tibial Tendoscopy
Posterior tibial tendoscopy is performed with the proximal and distal portals along the tendon sheath. The proximal portal is located 1 cm proximal to the medial malleolar tip, and the distal portal is located close to the navicular insertion of the tendon. Five-millimeter skin incisions are made at the portal sites, followed by blunt dissection of the subcutaneous tissue with a hemostat. The posterior tibial tendon sheath is exposed and incised at the portal sites.
Step 4: Examination of Tibialis Posterior Tendon, Superficial Deltoid Ligament, and Spring Ligament
The tibialis posterior tendon is examined, and synovectomy is performed with an arthroscopic shaver (Smith & Nephew, Andover, MA) if tenosynovitis is present. The superficial deltoid ligament is identified as the medial wall of the tendon sheath. With the proximal portal as the viewing portal, any tear of the ligament can be noted because the talus will be exposed. The tibio-spring ligament is torn in the illustrated case, and the talar head is exposed. If the talonavicular joint is already exposed, as in the illustrated case, the spring ligament can be examined by retracting the tibialis posterior tendon in a plantar direction (Fig 1). If the superficial deltoid ligament is not torn, an accessory distal portal can be made at the medial wall of the tibialis posterior tendon sheath just above the septum between the tibialis posterior tendon and the flexor digitorum longus tendon.9 The arthroscope can be inserted into the plantar gutter of the talonavicular joint through the distal and accessory distal portals. The integrity of the spring ligament can then be examined.
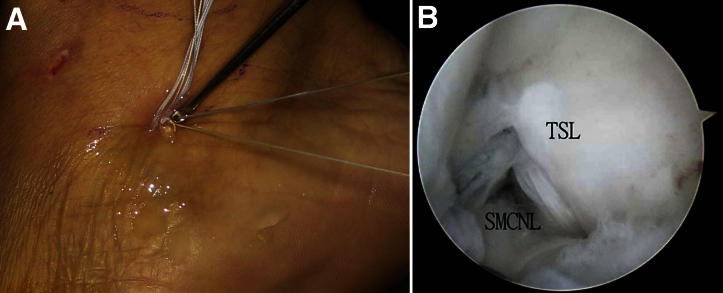
Fig 1.
Endoscopic repair of superficial deltoid ligament and spring ligament in a right foot. (A) The proximal portal is located 1 cm proximal to the medial malleolar tip, and the distal portal is located close to the navicular insertion of the tendon. (B) Posterior tibial tendoscopy is performed with the proximal portal as the viewing portal. (C) An arthroscopic view shows the torn tibio-spring ligament (TSL), and the talar head (TH) is exposed. The posterior tibial tendon (PTT) is retracted in a plantar direction. (D) An arthroscopic view shows the tear at the superomedial calcaneonavicular ligament (SMCNL).
Step 5: Repair of Torn Superficial Deltoid Ligament
After the ligamentous tears are defined, sutures are passed through the stumps of the torn ligaments by means of the CPR Viper suture passer (Arthrex, Naples, FL). The Viper suture passer preloaded with No. 2 FiberWire suture (Arthrex) is inserted through the distal portal to the proximal stump of the torn tibio-spring ligament. The head of the passer is slipped into the deep surface of the stump, and the stump is secured. The suture loop is passed through the stump and retrieved to the distal portal. The limbs of the suture are passed through the suture loop, and the suture is tightened with a good bite of the ligament stump. The procedure is repeated to pass another suture loop through the distal stump of the torn tibio-spring ligament (Fig 2).
Fig 2.
Endoscopic repair of superficial deltoid ligament and spring ligament in a right foot. (A) Passing of suture loop through the distal stump of the tibio-spring ligament by means of a CPR Viper suture passer through the distal portal. (B) An arthroscopic view shows that the head of the passer slips under the distal stump of the tibio-spring ligament (TSL). (C) The suture loop is retrieved to the distal portal, and the suture limbs pass through the loop. (D) The suture loop holds the distal stump of the tibio-spring ligament after tightening of the suture. (TH, talar head.)
Step 6: Repair of Torn Spring Ligament
The next step is suturing the stumps of the torn superomedial calcaneonavicular ligament. A high distal portal is made just plantar to the equator of the talar head and at the level of the talonavicular joint. This is located by means of a needle inserted into the talonavicular joint through the proposed portal site. A 5-mm incision is made at this portal site, and the portal tract is dilated by a hemostat. The CPR Viper suture passer preloaded with another No. 2 FiberWire is introduced through this portal to the talonavicular joint. The foot is supinated to bring the deep stump of the torn superomedial calcaneonavicular ligament to the medial side. The head of the passer is then slipped into the deep surface of the deep stump. The great toe is placed in dorsiflexion to tense up the flexor hallucis longus tendon; this will push the medial plantar nerve in a plantar direction and away from the spring ligament. A bite is obtained from the stump, and a suture loop is passed through the stump. The loop is retrieved to the high distal portal. The suture limbs are passed through the loop and are tightened to form a suture loop in the deep stump. The suture is then retrieved to the distal portal by an arthroscopic probe (Fig 3). Another suture loop is made at the superficial stump of the ligament by means of the Viper suture passer through the distal portal. The suture limbs of the stumps of the individual ligament are tied by means of a knot pusher with the foot in supination (Fig 4, Video 1).
Fig 3.
Endoscopic repair of superficial deltoid ligament and spring ligament in a right foot. (A) A bite of the deep stump of the superomedial calcaneonavicular ligament (SMCNL) is obtained by the Viper suture passer through the high distal portal. (B) The stump is held by the suture loop. (C) The suture is retrieved to the distal portal by an arthroscopic probe. (TH, talar head.)
Fig 4.
Endoscopic repair of superficial deltoid ligament and spring ligament in a right foot. (A) Repair of the ligaments by means of a knot pusher through the distal portal. (B) Arthroscopic view after repair of ligaments. (SMCNL, superomedial calcaneonavicular ligament; TSL, tibiospring ligament.)
Discussion
The mechanical integrity of the medial longitudinal arch depends on the dynamic support of muscles, the static support of ligaments and joint capsules, and the manner in which the tarsal bones interlock.10 The tibialis posterior tendon is the major dynamic stabilizer of the hindfoot, whereas the spring ligament is the most important static stabilizer.10 After rupture of the posterior tibial tendon, the spring ligament may tear, stretch, or rupture under increased stress.10 Compromise of this ligament is a primary causative factor of peritalar subluxation, and a functioning tibialis posterior tendon cannot prevent or correct a plano-valgus foot deformity.11 Therefore, the spring ligament should be repaired in addition to treatment of tibialis posterior tendon abnormalities.4
An open approach to the spring ligament requires extensive soft-tissue dissection. Endoscopic assessment of the integrity before open exploration has been proposed to avoid unnecessary soft-tissue dissection.9 The technique of endoscopic repair of the spring ligament is an advancement in the field and, together with the endoscopically assisted reconstruction of the tibialis posterior tendon,8 allows complete endoscopic treatment of stage 2 posterior tibial tendon deficiency (Table 1).
Table 1.
Pearls and Pitfalls of Endoscopic Repair of Superficial Deltoid Ligament and Spring Ligament
| Pearls |
| The superomedial calcaneonavicular ligament is most commonly involved in spring ligament tears. |
| The high distal portal facilitates passage of suture loop to the deep stump of the superomedial calcaneonavicular ligament. |
| Supination of the foot may bring the deep stump of the superomedial calcaneonavicular ligament medially to facilitate the repair. |
| Dorsiflexion of the great toe can displace the medial plantar nerve from the spring ligament. |
| Repair of the spring ligament in an outside-in manner may reduce the risk of medial plantar nerve injury. |
| Pitfalls |
| The described technique is not suitable for complex tears of the ligaments. |
| It is not suitable for a spring ligament that is torn from its bony insertion. |
| It is not suitable if the remnants of the ligaments are of poor quality for repair. Ligamentous reconstruction is more suitable in this case. |
| It is not suitable if the spring ligament is attenuated rather than torn. |
The major potential risk with this approach is injury to the medial plantar nerve (Table 2). The superomedial calcaneonavicular ligament is the most common site of rupture, whereas the medial plantar nerve is usually close to the inferior calcaneonavicular ligament (T.H.L., unpublished data, December 2013). However, the medial plantar nerve can pass underneath the superomedial calcaneonavicular ligament in around 30% of cases (T.H.L., unpublished data, December 2013). The medial plantar nerve crosses the flexor hallucis longus tendon in a plantar direction.12, 13 Passive dorsiflexion of the hallux will tense up the flexor hallucis longus tendon and push the medial plantar nerve in a plantar direction and away from the spring ligament. This may reduce the risk of nerve injury (T.H.L., unpublished data, December 2013). Furthermore, the use of the Viper suture passer allows passage of suture in an outside-in manner. This will also reduce the risk of nerve injury. To obtain a secure bite of the ligament by the Viper suture passer, the ligament should be perpendicular to the stem of the passer. An effective bite to the deep stump of the superomedial calcaneonavicular ligament is not possible through the distal portal because the stem of the passer will be parallel to the ligament. To have proper orientation of the passer to the deep stump, the passer should pass through the high distal portal. The portal is made slightly plantar to the equator of the talar head rather than above the equator to allow the deeper part of the plantar ligament to be reached by the suture passer. Moreover, supination of the foot can bring the deep part of the ligament medially for easier reaching by the suture passer.
Table 2.
Advantages and Risks of Endoscopic Repair of Superficial Deltoid Ligament and Spring Ligament
| Advantages |
| The described technique can allow repair of the spring ligament without the need for extensive soft-tissue dissection. |
| This technique, together with endoscopically assisted reconstruction of the tibialis posterior tendon, allows complete endoscopic treatment of stage 2 posterior tibial tendon deficiency. |
| Risks |
| The medial plantar nerve is the major structure at risk. |
| The flexor hallucis longus tendon can be injured. |
If the inferior calcaneonavicular ligament is involved, repair by means of the Viper suture passer through the medial portals will be difficult. Repair of the ligament can be risky to the medial plantar nerve because the nerve passes under the ligament in around 70% of cases.5 A slotted cannula (Wright Medical Technology, Arlington, TN) can be inserted underneath the ligament and an arthroscope introduced to confirm that the nerve is not sandwiched between the ligament and the cannula. Then, the arthroscope is removed, a Micro SutureLasso (Arthrex) is introduced, and suture is passed through the ligament under arthroscopic guidance through anterior subtalar arthroscopy.14, 15 The suture is retrieved to the lateral portal for subsequent tying.
This is a technically demanding procedure and should be reserved for experienced foot and ankle arthroscopists. Endoscopic repair of the spring ligament and superficial deltoid ligament is a feasible alternative to open repair.
Footnotes
The author reports that he has no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Endoscopic repair of superficial deltoid ligament and spring ligament in a right foot. Posterior tibial tendoscopy is performed through the proximal and distal portals. The tears at the superficial deltoid ligament and spring ligament are identified. Suture loops are passed through the proximal and distal stumps of the tibio-spring ligament by means of a CPR Viper suture passer through the distal portal. Suture loop is passed through the deep stump of the superomedial calcaneonavicular ligament through the high distal portal. The suture is retrieved to the distal stump by an arthroscopic probe. Suture loop is passed through the superficial stump of the ligament through the distal portal. The sutures are tied to repair the ligament.
References
- 1.Melão L., Canella C., Weber M., Negrão P., Trudell D., Resnick D. Ligaments of the transverse tarsal joint complex: MRI-anatomic correlation in cadavers. AJR Am J Roentgenol. 2009;193:662–671. doi: 10.2214/AJR.08.2084. [DOI] [PubMed] [Google Scholar]
- 2.Taniguchi A., Tanaka Y., Takakura Y., Kadono K., Maeda M., Yamamoto H. Anatomy of the spring ligament. J Bone Joint Surg Am. 2003;85:2174–2178. doi: 10.2106/00004623-200311000-00018. [DOI] [PubMed] [Google Scholar]
- 3.Mengiardi B., Zanetti M., Schottle P.B. Spring ligament complex: MR imaging-anatomic correlation and findings in asymptomatic subjects. Radiology. 2005;237:242–249. doi: 10.1148/radiol.2371041065. [DOI] [PubMed] [Google Scholar]
- 4.Orr J.D., Nunley J.A., II Isolated spring ligament failure as a cause of adult-acquired flatfoot deformity. Foot Ankle Int. 2013;34:818–823. doi: 10.1177/1071100713483099. [DOI] [PubMed] [Google Scholar]
- 5.Tryfonidis M., Jackson W., Mansour R. Acquired adult flat foot due to isolated plantar calcaneonavicular (spring) ligament insufficiency with a normal tibialis posterior tendon. Foot Ankle Surg. 2008;14:89–95. doi: 10.1016/j.fas.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 6.Borton D.C., Saxby T.S. Tear of the plantar calcaneonavicular (spring) ligament causing flatfoot: A case report. J Bone Joint Surg Br. 1997;79:641–643. doi: 10.1302/0301-620x.79b4.7396. [DOI] [PubMed] [Google Scholar]
- 7.van Dijk C.N., Kort N., Scholten P.E. Tendoscopy of the posterior tibial tendon. Arthroscopy. 1997;13:692–698. doi: 10.1016/s0749-8063(97)90002-5. [DOI] [PubMed] [Google Scholar]
- 8.Lui T.H. Endoscopic assisted posterior tibial tendon reconstruction for stage 2 posterior tibial tendon insufficiency. Knee Surg Sports Traumatol Arthrosc. 2007;15:1228–1234. doi: 10.1007/s00167-006-0282-8. [DOI] [PubMed] [Google Scholar]
- 9.Lui T.H. Posterior tibial tendoscopy: Endoscopic synovectomy and assessment of the spring (calcaneonavicular) ligament. Arthrosc Tech. 2015;4:e819–e925. doi: 10.1016/j.eats.2015.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gazdag A.R., Cracchiolo A., III Rupture of the posterior tibial tendon. Evaluation of injury of the spring ligament and clinical assessment of tendon transfer and ligament repair. J Bone Joint Surg Am. 1997;79:675–681. doi: 10.2106/00004623-199705000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Acevedo J., Vora A. Anatomical reconstruction of the spring ligament complex: “Internal brace” augmentation. Foot Ankle Spec. 2013;6:441–445. doi: 10.1177/1938640013499404. [DOI] [PubMed] [Google Scholar]
- 12.Lui T.H., Chan K.B., Chan L.K. Zone 2 flexor hallucis longus tendoscopy: A cadaveric study. Foot Ankle Int. 2009;30:447–451. doi: 10.3113/FAI-2009-0447. [DOI] [PubMed] [Google Scholar]
- 13.Lui T.H., Chan K.B., Chan L.K. Cadaveric study of zone 2 flexor hallucis longus tendon sheath. Arthroscopy. 2010;26:808–812. doi: 10.1016/j.arthro.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 14.Lui T.H. Anterior subtalar (talocalcaneonavicular) arthroscopy. Foot Ankle Int. 2008;29:94–96. doi: 10.3113/FAI.2008.0094. [DOI] [PubMed] [Google Scholar]
- 15.Lui T.H., Chan K.B., Chan L.K. Portal safety and efficacy of anterior subtalar arthroscopy: A cadaveric study. Knee Surg Sports Traumatol Arthrosc. 2010;18:233–237. doi: 10.1007/s00167-009-0917-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Endoscopic repair of superficial deltoid ligament and spring ligament in a right foot. Posterior tibial tendoscopy is performed through the proximal and distal portals. The tears at the superficial deltoid ligament and spring ligament are identified. Suture loops are passed through the proximal and distal stumps of the tibio-spring ligament by means of a CPR Viper suture passer through the distal portal. Suture loop is passed through the deep stump of the superomedial calcaneonavicular ligament through the high distal portal. The suture is retrieved to the distal stump by an arthroscopic probe. Suture loop is passed through the superficial stump of the ligament through the distal portal. The sutures are tied to repair the ligament.