Abstract
Rationale: Hospital chaplains provide spiritual care that helps patients facing serious illness cope with their symptoms and prognosis, yet because mechanically ventilated patients cannot speak, spiritual care of these patients has been limited.
Objectives: To determine the feasibility and measure the effects of chaplain-led picture-guided spiritual care for mechanically ventilated adults in the intensive care unit (ICU).
Methods: We conducted a quasi-experimental study at a tertiary care hospital between March 2014 and July 2015. Fifty mechanically ventilated adults in medical or surgical ICUs without delirium or dementia received spiritual care by a hospital chaplain using an illustrated communication card to assess their spiritual affiliations, emotions, and needs and were followed until hospital discharge. Feasibility was assessed as the proportion of participants able to identify spiritual affiliations, emotions, and needs using the card. Among the first 25 participants, we performed semistructured interviews with 8 ICU survivors to identify how spiritual care helped them. For the subsequent 25 participants, we measured anxiety (on 100-mm visual analog scales [VAS]) immediately before and after the first chaplain visit, and we performed semistructured interviews with 18 ICU survivors with added measurements of pain and stress (on ±100-mm VAS).
Measurements and Main Results: The mean (SD) age was 59 (±16) years, median mechanical ventilation days was 19.5 (interquartile range, 7–29 d), and 15 (30%) died in-hospital. Using the card, 50 (100%) identified a spiritual affiliation, 47 (94%) identified one or more emotions, 45 (90%) rated their spiritual pain, and 36 (72%) selected a chaplain intervention. Anxiety after the first visit decreased 31% (mean score change, −20; 95% confidence interval, −33 to −7). Among 28 ICU survivors, 26 (93%) remembered the intervention and underwent semistructured interviews, of whom 81% felt more capable of dealing with their hospitalization and 0% felt worse. The 18 ICU survivors who underwent additional VAS testing during semistructured follow-up interviews reported a 49-point reduction in stress (95% confidence interval, −72 to −24) and no significant change in physical pain that they attributed to picture-guided spiritual care.
Conclusions: Chaplain-led picture-guided spiritual care is feasible among mechanically ventilated adults and shows potential for reducing anxiety during and stress after an ICU admission.
Keywords: spiritual therapies, palliative care, mechanical ventilators, critical care, anxiety
Mechanically ventilated patients in the intensive care unit (ICU) experience substantial psychoemotional distress, because endotracheal intubation or tracheostomy prevents the majority from speaking, and most observers cannot reliably lip-read (1–6). Attempts at having mechanically ventilated patients write or point to letters to spell out words have been often unsuccessful, because handwriting is often illegible and the process is time consuming (7, 8). Nurse and chaplain interpretations of nods and gesticulations by mechanically ventilated patients are sometimes accurate, but there are also reports of misinterpretation causing significant miscommunication (2, 9, 10). When critically ill patients are unable to self-report, nurses will often use cardiorespiratory signs, ventilator compliance, and facial expressions to identify symptoms that are present. However, similar changes in vital signs or behaviors may indicate a variety of different symptoms (9, 11).
Communication cards may improve communication between mechanically ventilated patients and their providers (12, 13), but only one rigorous study exists that evaluates communication cards as part of a comprehensive communication intervention with endotracheally intubated ICU patients and their nurses (14). Since the adoption of minimized sedation as an ICU best practice (15, 16), it has been estimated that half of mechanically ventilated patients may benefit from assistive communication tools (17).
The Joint Commission and the National Quality Forum for Palliative Care guidelines include spiritual care as a component of their care standards (18, 19), and studies in non-ICU settings have shown that many patients find religion or spirituality to be the most important factor enabling them to cope with serious illness (20–22). Although previous studies in the ICU have shown that chaplain care is associated with increased family satisfaction (23, 24), the focus has traditionally been on the family members of dying patients and not the patients themselves (25). There is growing recognition of a need for a comprehensive approach to providing proactive spiritual support to ICU patients (24–28).
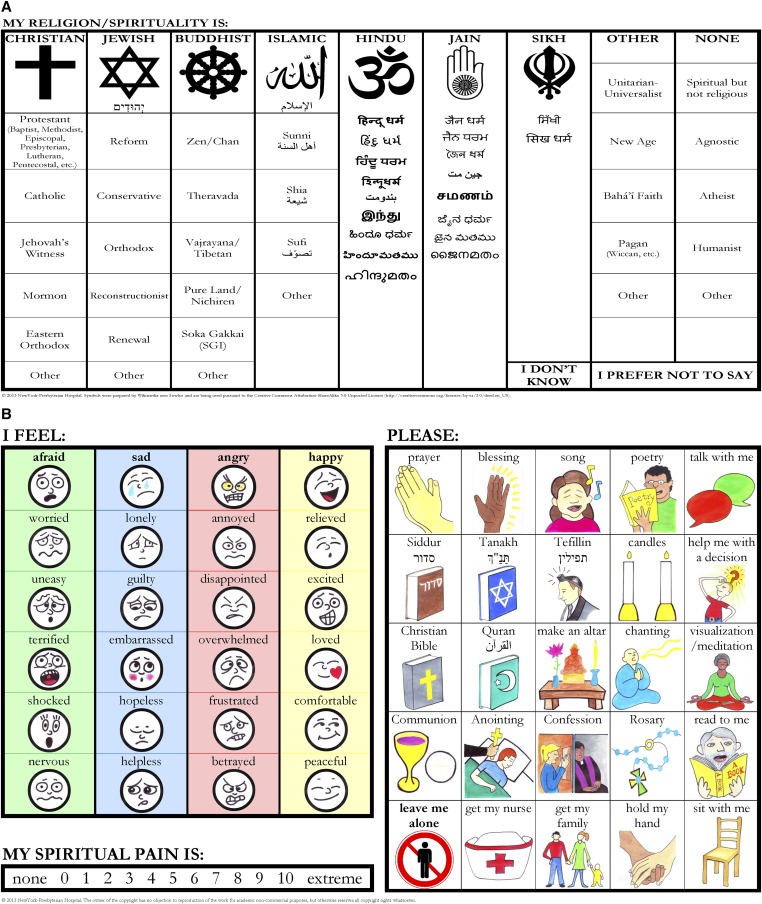
Like other healthcare providers in the ICU, our chaplain experienced difficulty with lip-reading and interpreting behavioral signs in mechanically ventilated patients he saw in consultation. Therefore, he created an illustrated spiritual care communication card to facilitate the assessment of spiritual needs and guide spiritual care in mechanically ventilated adults in a systematic way that meets established criteria of the Association of Professional Chaplains’ Standards of Practice for spiritual assessment and delivery of care in acute care settings (29). The card contains four sections that allow mechanically ventilated patients to point to pictures and words that indicate their (1) spiritual or religious affiliation, (2) emotions, (3) spiritual pain, and (4) desired chaplain interventions.
We aimed to determine the feasibility and measure the effects of chaplain-led picture-guided spiritual care in mechanically ventilated adult ICU patients. We hypothesized that awake and alert mechanically ventilated adult ICU patients without delirium or dementia would be able to identify their spiritual preferences and needs using the illustrated communication card and that, in turn, the chaplain would provide spiritual care that would alleviate their psychoemotional distress during and after the ICU admission.
Methods
Study Design and Participants
We performed a single-center prospective cohort study at an urban, tertiary care medical center. Between March 2014 and July 2015, we screened adults 18 years of age or older with 6 or more hours of mechanical ventilation who had no history of dementia, no advanced chronic neurologic disease (e.g., amyotrophic lateral sclerosis, Parkinson's disease) or stroke with receptive or expressive aphasias, were known to understand English or Spanish, and who by ICU nurse report had a Richmond Agitation Sedation Score of 0 or −1 and followed simple commands (30). Patients were considered eligible if they were alert and oriented to self, place, and time by nodding appropriately to orientation questions and were not delirious as measured by the Confusion Assessment Method ICU survey (31). We screened Monday to Friday when the medical ICU (MICU) chaplain was working and available to see adult ICU patients, and on weekends when the chaplain and at least one of the other staff involved in screening and assessments were on call. We preferentially screened MICU patients, because our MICU chaplain developed the spiritual care communication card for use. When no MICU patients were eligible, we then screened surgical ICU (SICU) patients who met the above criteria and who were not already receiving care by another chaplain.
Given our patients’ frequent inability to write, we obtained a waiver of signed consent and reviewed with eligible patients an information sheet that explained the study procedures. Only those who nodded in assent to participation were included in the study. The study was approved by the Columbia University Medical Center Institutional Review Board.
Picture-guided Spiritual Care
Our MICU chaplain (J.N.B.) developed the illustrated spiritual care communication card (Figure 1; see Figure E1 in the online supplement) and provided all of the picture-guided spiritual care to study participants, speaking either in English or Spanish. He is a member of the Association of Professional Chaplains, has a Master’s of Divinity, and completed six units of Clinical Pastoral Education accredited by the Association for Clinical Pastoral Education. He developed the illustrated spiritual care communication card with four sections that reflect the domains of a spiritual assessment that would be typically assessed by a chaplain through conversation but instead can be assessed by having the user point to pictures and words to: (1) identify spiritual or religious affiliations; (2) identify a range of feelings; (3) rate spiritual pain (32); and (4) select a desired religious, spiritual, or nonspiritual intervention that a chaplain can offer (Figure 1). He developed the range of feelings a patient could identify based first on the four classes of feelings that he was trained to assess when caring for someone: anger, happiness, sadness, and fear (33). He then intuitively added five more emotions to each class and worked with an illustrator to create cartoon faces associated with each of these emotions so that patients could describe their feelings by pointing to one or more of 24 emotions.
Figure 1.
Spiritual care communication card (English version). (A) Front side. Part 1: Spiritual/religious affiliation assessment. (B) Back side. Part 2: Feelings assessment; part 3: Spiritual pain assessment; part 4: Chaplain interventions assessment. The communication card is 11 × 17 inches and laminated. See Figure E1 in the online supplement for Spanish version.
The chaplain first reviewed the participant’s state of health by speaking with providers and reviewing the medical record. He then introduced himself to the participant and led him or her through each of the four sections of the communication card. This structured chaplain-led picture-guided spiritual care meets Standards of Practice by the Association of Professional Chaplains by evaluating relevant information pertinent to the care of a recipient’s bio-psycho-social-spiritual/religious health and by implementing a culturally sensitive plan of care to promote the well-being of the recipient (29). For participants who did not select any desired chaplain intervention, the chaplain offered well wishes specific to their hospitalization. The chaplain revisited participants during their hospitalization if they desired a chaplain intervention to be repeated (e.g., prayer) or if they had ongoing psychoemotional distress for which they desired follow-up spiritual care. During revisits, he used the communication card to guide spiritual care only if a participant remained mechanically ventilated.
Measurements
We assessed the feasibility of using the illustrated communication card to guide spiritual care by (1) measuring the proportions of participants who were able to identify or confirm their spiritual or religious affiliation, identify at least one emotion, rate their spiritual pain on a 0 to 10 integer scale, and select at least one desired chaplain intervention when using the communication card for the first time; and by (2) measuring the time needed to complete the four sections of the communication card and the time of the entire initial chaplain-led picture-guided spiritual care consultation.
We measured the effect of chaplain-led picture-guided spiritual care for mechanically ventilated ICU patients using a two-phase approach that is described in detail in the online supplement. Briefly, because we were initially unsure how participants would react to engaging in communication about their emotions and spiritual needs, we first conducted semistructured exploratory interviews with ICU survivors from the first half of study participants (n = 25) to identify the common symptoms picture-guided spiritual care treated. On the basis of our review of these interviews, we then added 100-mm visual analog scales (VASs) to measure anxiety immediately before and after the initial chaplain visit in the second half of study participants (n = 25) and ±100-mm VAS to measure changes in stress and pain attributed to chaplain-led picture-guided spiritual care among those who survived intensive care and were awaiting hospital discharge.
Demographic and clinical variables were obtained from the electronic medical record. A priori, we planned subgroup analyses comparing VAS anxiety and stress scores between participants who were younger versus older, religious versus nonreligious, cared for in the MICU versus SICU, and received picture-guided spiritual care in English versus Spanish. Post hoc, we compared VAS anxiety and stress scores between organ transplant recipients and participants without organ transplantation and between decedents and ICU survivors.
Statistical Analysis
We present categorical data using percentages and continuous data as mean (±SD) or median (interquartile range [IQR]). We compared 100-mm VAS anxiety scores immediately before and after the initial chaplain-led picture-guided spiritual care consult using the Wilcoxon signed-rank test and compared ±100-mm VAS scores measuring change in stress and pain attributed to spiritual care among ICU survivors to 0 (no change), also using Wilcoxon signed-rank test. Statistical significance was defined as a two-tailed P < 0.05. Analyses were performed with Stata 13.0 (Stata Corp., College Station, TX).
Results
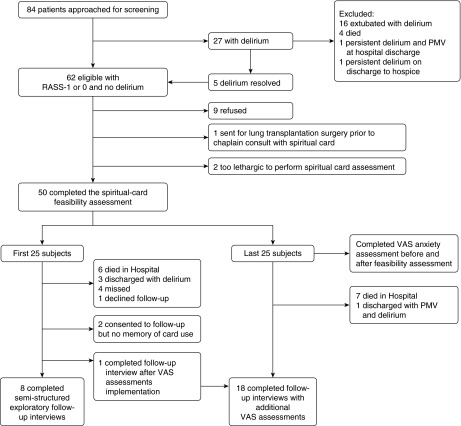
We screened 84 adult ICU patients receiving mechanical ventilation; 27 were found to have delirium and were initially excluded, but 5 had no delirium on a subsequent day of screening and remained mechanically ventilated, resulting in 62 eligible patients. Nine (15%) declined to participate, one (1.6%) enrolled but underwent lung transplantation before receiving picture-guided spiritual care, and two (3.2%) enrolled but were too lethargic to use the card. Fifty (81%) completed a feasibility assessment on the same day after enrolling and were followed until hospital discharge. Figure 2 details participant flow through the study.
Figure 2.
Study participants. PMV = prolonged mechanical ventilation; RASS = Richmond Agitation-Sedation Scale; VAS = visual analog scale.
Participants had a mean (SD) age 59 (±16) years and a wide range of Acute Physiology and Chronic Health Evaluation II scores. The most common indications for mechanical ventilation were respiratory failure or distress and pneumonia. Participants were of diverse races/ethnicities, and 10 (20%) used the Spanish version of the communication card. They had multiple comorbidities (Charlson comorbidity index median [IQR], 2.5 [1–4]). Although 14 participants (28%) were solid organ or bone marrow transplantation recipients, only 6 (12%) underwent transplantation while enrolled in the study (all lung transplants). Participants received mechanical ventilation for a median (IQR) of 19.5 (7–29) days, and 23 (46%) received a tracheostomy. Forty-two (84%) met the most recent consensus definition of chronic critical illness (34). The in-hospital mortality was 30%, 17 participants (34%) were discharged home, 17 (34%) were discharged to skilled-care facilities, and 1 (2%) was discharged to hospice (Table 1).
Table 1.
Subject characteristics
| Characteristic (n = 50) | Measure | Characteristic (n = 50) | Measure |
|---|---|---|---|
| Age (mean, SD), yr | 59, 16 | Primary ICU admission diagnosis category | |
| Male | 28 (56) | Pulmonary | 31 (62) |
| Race | Cardiac, medical | 3 (6) | |
| White | 25 (50) | Sepsis or infection | 3 (6) |
| Hispanic | 12 (24) | Gastrointestinal | 1 (2) |
| Black | 9 (18) | Neurological | 2 (4) |
| Southeast Asian | 4 (8) | Oncology | 1 (2) |
| Card language used | Shock | 3 (6) | |
| English | 40 (80) | Surgical | 5 (10) |
| Spanish | 10 (20) | Vascular | 1 (2) |
| APACHE II (mean, SD) | 22, 7.0 | Indication for mechanical ventilation | |
| Charlson Index (median, IQR) | 2.5, 1–4 | Respiratory failure or distress | 6 (12) |
| Cancer | Pneumonia | 12 (24) | |
| Solid tumor with metastatic disease | 2 (4) | Pulmonary edema | 1 (2) |
| Hematologic malignancy | 6 (12) | Hypoxemia | 8 (16) |
| Organ transplantation | 14 (28) | ARDS | 4 (8) |
| Lung transplantation during hospitalization | 6 (12) | Asthma | 2 (4) |
| Prior lung transplantation | 4 (8) | Cystic fibrosis exacerbation | 2 (4) |
| Prior renal transplantation | 3 (6) | Cardiac arrest | 1 (2) |
| Prior bone marrow transplantation | 1 (2) | Airway protection | 6 (12) |
| Type of ICU | Postoperative | 7 (14) | |
| Medical | 42 (84) | Angioedema | 1 (2) |
| Surgical | 8 (16) | Discharge disposition | |
| Total mechanical ventilation days (median, IQR) | 19.5, 7–29 | Home | 17 (34) |
| Mechanical ventilation via tracheostomy | 23 (46) | Acute Rehabilitation | 6 (12) |
| Days of mechanical ventilation before picture-guided spiritual care (median, IQR) | 7, 2–14 | Skilled Care Facility | 11 (22) |
| Total ICU length of stay (median, IQR) | 22, 13–43 | Hospice | 1 (2) |
| Total hospital length of stay (median, IQR) | 42, 26–69 | Died | 15 (30) |
Data are presented as n (%) unless otherwise noted.
Definition of abbreviations: APACHE = Acute Physiology and Chronic Health Evaluation; ARDS = acute respiratory distress syndrome; ICU = intensive care unit; IQR = interquartile range.
Using the communication card for the first time, participants’ spiritual affiliation was identified 100% of the time, 47 participants (94%) were able to identify one or more emotion, 45 participants (90%) rated their spiritual pain, and 36 (72%) selected a desired chaplain intervention. It took participants a median (IQR) of 8.5 minutes (5–13) to complete the four sections of the communication card, and it took the chaplain a median (IQR) of 18 (11–25) minutes to both use the card with participants and provide a desired spiritual care intervention (Table 2).
Table 2.
Chaplain-led picture-guided spiritual care feasibility assessment
| Communication card part 1: identify a religious or spiritual affiliation | Measure |
|---|---|
| Affiliation identified | 50 (100) |
| Communication card used to confirm affiliation* | 34 (68) |
| Communication card used to identify an affiliation different from what was listed in the medical record | 7 (14) |
| Communication card used to identify an affiliation when none was listed in the medical record | 9 (18) |
| Religion or spiritual preference | |
| Catholic | 28 (56) |
| Jewish | 5 (10) |
| Nondenominational Christian | 3 (6) |
| Baptist | 2 (4) |
| Presbyterian | 1 (2) |
| Pentecostal | 1 (2) |
| Buddhist | 1 (2) |
| Hindu | 1 (2) |
| Islamic | 1 (2) |
| Agnostic | 1 (2) |
| No spiritual or religious affiliation | 1 (2) |
| Communication card part 2: Identify emotions | |
| Identified ≥1 emotion | 47 (94) |
| No emotions identified | 3 (6) |
| Types of emotions identified† (n = 47) | |
| General emotion: fear | 18 (38) |
| General emotion: sadness | 29 (62) |
| General emotion: anger | 23 (49) |
| General emotion: happiness | 23 (49) |
| Groupings of emotions (n = 47) | |
| Happiness only | 9 (19) |
| ≥1 Negative emotion only | 24 (51) |
| Happiness + 1 negative emotion | 6 (13) |
| Happiness + 2 negative emotions | 3 (6) |
| Happiness + 3 negative emotions | 5 (11) |
| Communication card part 3: Rate spiritual pain | |
| Able to rate spiritual pain | 45 (90) |
| Spiritual pain, integer scale 0–10 (mean, SD) | 4.2, 3.7 |
| Spiritual pain score (n = 45) | |
| 0 | 14 (31) |
| 1–4 | 9 (20) |
| 5–7 | 10 (22) |
| 8–10 | 12 (27) |
| Communication card part 4: Identify chaplain intervention | |
| Identified ≥1 desired intervention | 36 (72) |
| Did not identify any intervention | 14 (28) |
| Type of intervention identified (n = 36) | |
| Religious Intervention | 27 (75) |
| Prayer | 18 (50) |
| Give blessing | 9 (25) |
| Read Christian Bible | 3 (8.3) |
| Receive communion | 9 (25) |
| Anointing | 5 (14) |
| Confession | 4 (11) |
| Pray with rosary | 8 (22) |
| Make an alter | 0 (0) |
| Siddur | 0 (0) |
| Tankah | 0 (0) |
| Tefillin | 0 (0) |
| Read Quran | 1 (2.8) |
| Chanting music | 0 (0) |
| Nonreligious intervention | 12 (33) |
| Song | 5 (14) |
| Poetry | 2 (5.6) |
| Electronic candles | 1 (2.8) |
| Talk with me | 2 (5.6) |
| Visualization | 3 (8.3) |
| Read | 4 (11) |
| Hold hand | 5 (14) |
| Sit with me | 3 (8.3) |
| Help with a decision | 1 (2.7) |
| Get other help | 5 (14) |
| Get family | 5 (14) |
| Get nurse | 2 (5.6) |
| Leave me alone | 1 (2.7) |
| Duration and No. of chaplain visits | |
| Initial card use time, min, (median, IQR) | 8.5, 5–13 |
| Total initial consult time, min, (median, IQR) | 18, 11–25 |
| No. of follow-up visits with chaplain, (median, IQR) | 2, 0–3 |
| Follow-up visit count by time, min | |
| <10 | 64 (42) |
| 11–25 | 42 (28) |
| 26–39 | 23 (15) |
| >40 | 23 (15) |
Definition of abbreviation: IQR = interquartile range. Data presented as n (%) unless otherwise noted. Participants were allowed to select more than one emotion or chaplain intervention. Therefore, percentages may add to up to greater than 100%.
The chaplain first obtained a religious affiliation from the medical record or family, and the participant nodded in acknowledgment when asked his/her preference.
Participants pointed to cartoon faces with a descriptive word above each face (see Figure 1). There were four general emotion categories, each with specific faces: (1): fear: afraid, worried, uneasy, terrified, shocked, nervous; (2) sadness: sad, lonely, guilty, embarrassed, hopeless, helpless; (3) anger: angry, annoyed, disappointed, overwhelmed, frustrated, betrayed; (4) happiness: happy, relieved, excited, loved, comfortable, peaceful. Numbers and percentages of specific emotions identified are listed in Table E1 in the online supplement.
For 34 participants (68%), identifying a spiritual affiliation consisted of the chaplain pointing to the affiliation on the card that was listed in the medical record or given by family members and observing the subject nod in acknowledgment. However, seven participants (14%) used the card to identify a spiritual affiliation that was different from what was listed in the medical record. Participants had diverse spiritual or religious affiliations, with most being either Catholic (56%) or Jewish (10%), and seven (14%) identified themselves as agnostic or having no spiritual or religious affiliation (Table 2).
Participants’ emotions varied widely (Table 2, Table E1). Forty-eight participants (51%) felt only negative emotions (fear, sadness, and anger), and nine (19%) reported only feeling happy. Fourteen (30%) reported feeling both happy and negative emotions. On a 0 to 10 integer scale, participants’ mean (SD) spiritual pain was 4.2 (±3.7) (Table 2). Among the 36 participants (72%) who selected one or more desired chaplain interventions, 75% requested religious interventions and 33% requested nonreligious interventions (Table 2). Only one subject (2.7%) indicated that he wished to be left alone after using the first three sections of the communication card. The chaplain revisited study participants during their hospitalization to provide additional spiritual care a median (IQR) of two (zero to three) times, with 70% of revisits lasting less than 25 minutes (Table 2).
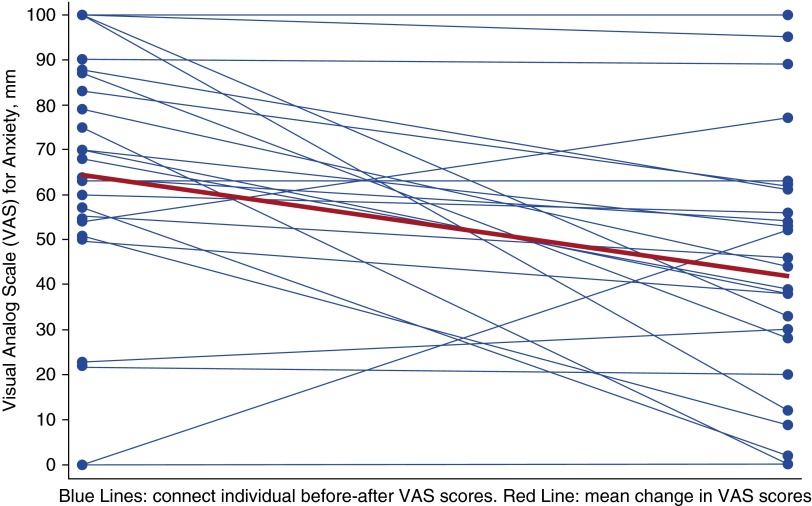
Among the second half of participants (n = 25), in whom anxiety was measured by VAS immediately before and after the initial chaplain-led picture-guided spiritual care, anxiety decreased from a mean (SD) VAS score of 64 (±29) to 44 (±28) (mean absolute reduction of 20 points, 95% confidence interval [CI], −33 to −7; P = 0.002; mean relative reduction, 31%; 95% CI, −48% to −15%; P = 0.001) (Figure 3). Among 28 ICU survivors who consented to follow-up interviews, 26 (93%) remembered receiving the chaplain’s picture-guided spiritual care in the ICU and completed the semistructured interviews. Eighty-one percent reported that they felt more capable of dealing with their hospitalization, 81% felt more at peace, 71% felt more connected with what is sacred, 96% would recommend chaplain-led picture-guided spiritual care to others, and 0% felt worse after receiving spiritual care (Table E2). Their responses to an open-ended question about why chaplain-led picture-guided spiritual care is helpful are listed in Table 3 and Table E3. Many participants report decreased anxiety and stress due to being able to communicate using the card, and several describe improved coping having recognized and acknowledged their feelings with the chaplain. On average, ICU survivors who underwent ±100-mm VAS testing at follow up (n = 18) reported mean 49-point reduction in stress (95% CI, −72 to − 24; P = 0.002) and no significant change in physical pain due to chaplain-led picture-guided spiritual care (Table E2).
Figure 3.
Anxiety was measured with 100-mm visual analog scale (VAS) immediately before and after the first time the participant received chaplain-led picture-guided spiritual care among the second half of participants (n = 25). Anxiety decreased from a mean (SD) VAS score of 64 (29) to 44 (28) (mean absolute reduction of 20 points; 95% confidence interval, −33 to −7; P = 0.002; mean relative reduction of 31%; 95% confidence interval, −48% to −15%; P = 0.001).
Table 3.
Intensive care unit survivors’ responses to an open-ended question about why chaplain-led picture-guided spiritual care is helpful
| “It was very helpful at the time to just reset everything, to gauge where you’re at and where you need to be…” |
| “I’m normally not the most spiritual or if you want to say religious person. The fact that there’s different interventions that are universally comforting—that’s really helpful because you don’t know what kind of patient you have. And I think anyone would take a blessing, even if you’re the most hardcore…” |
| “It’s a relief, a guide for expression.” |
| “It’s more than just a tool; it’s an outlet. You need that.” |
| “A [chaplain visit] is soothing to the patient and family: it’s ok to have all of these feelings, that I can feel serenity from sadness. It gives me permission to feel all this and that that is ok and part of the process of healing. Validation of it being okay to feel how you feel. It’s ok to be upset. Patients want to impress doctors and nurses and they can’t always.” |
| “It gave me more calmness, more acceptance.” |
| “Made me think for sure. With the numbers. How, for example, disappointed or excited I was…. it made me think. Pretty helpful. Especially the feelings page. Made me think about how I felt about being afraid, disappointed. Made me think about my emotions—which was helpful. A lot of times you get overwhelmed by your feelings, especially when you’re sick or in a moment of stress.” |
| “I just felt more at peace” because “I was able to communicate.” |
| “It may not change the physical pain, but it can help to reduce or decrease the pain by relaxing or calming the patient.” |
| It’s helpful “that it even prompts you to think about it all. When you’re lying there in pain and anxiety, it’s difficult to even think.” |
| “The visit from the chaplain is extremely helpful. Talking to a chaplain or a person that has the ability to help give you interior peace and to help you with your fears and frustrations means a lot to anyone and helps you to feel better.” |
Excerpts of responses; all responses from all intensive care unit survivors interviewed are listed in Table E3 in the online supplement.
Younger, nonreligious, English-speaking MICU participants reported slightly greater reductions in anxiety and stress than older, religious, Spanish-speaking SICU participants. Those who ultimately survived the ICU tended to report greater reductions in anxiety after the first chaplain visit than those who ultimately died or were discharged to hospice. The four participants (8%) who underwent lung transplant during study enrollment reported a similar reduction in stress attributed to spiritual care compared with both those who underwent organ transplantation before the study period and those without organ transplantation. Given the small subsample sizes, these results should be considered preliminary and interpreted with caution (Table E4).
Discussion
We have shown in a single-center cohort study that it is feasible to use a novel picture guide to assist chaplains with spiritual care for awake and alert mechanically ventilated adults in the ICU. Participants reported an immediate reduction in anxiety after receiving this care for the first time, and those who survived intensive care reported a reduction in stress that they attributed to picture-guided spiritual care. To our knowledge, this is the first clinical study to test a structured, integrative, and measureable approach to chaplain care aimed at treating anxiety and stress and improving coping in mechanically ventilated ICU patients. Using this unique spiritual assessment tool with ICU patients opens a novel area of chaplaincy and palliative care clinical research.
Picture-guided spiritual care may reduce anxiety during and stress after an ICU admission in several ways. Survivors of mechanical ventilation report feeling anxious and lonely because they cannot communicate vocally (1, 5, 35). Using the communication board with the chaplain addresses a mechanically ventilated patient’s fundamental need to express him or herself and to be understood. Having participants point to faces to identify their emotions on the communication card revealed that approximately 50% felt only negative emotions, 30% felt both happy and negative emotions, and 20% felt only happy. On the basis of the chaplain’s experience of providing spiritual care to study participants, the high prevalence of happiness seemed to reflect participants’ appreciation for still being alive and for family support they were receiving. Several ICU survivors reported in follow-up interviews that acknowledging their emotions with the chaplain was crucial to helping them cope with their critical illness. This finding is consistent with prior studies in non-ICU settings that have shown many patients find spiritual care to be the single most important factor enabling them to cope with a serious illness (20–22). More than half of participants rated their spiritual pain greater than or equal to 5 on a 0 to 10 integer scale, and higher spiritual pain scores have been shown to be associated with lower spiritual quality of life and adverse physical and emotional symptoms (32). The desired chaplain interventions that a patient selected, whether or not religious, focused on comforting the patient and improving his or her well-being in the context of both his or her spiritual pain and critical illness.
This study answers calls for more rigorous studies of spiritual and religious interventions (36), a need to develop a comprehensive approach to assess and meet the spiritual needs of patients (24, 26, 37, 38), and for research aimed at improving critical illness survivorship (39). A 2012 Cochrane review found inconclusive evidence that palliative care teams with a chaplain help terminally ill patients feel emotionally supported, but note that patients’ emotions and ability to cope were not well measured (36). We specifically measured participants’ emotions, showed improvement in symptoms of anxiety and stress, and elicited feedback that suggests spiritual care helps ICU survivors cope with critical illness. Prior studies have shown that chaplain-led spiritual care improves family satisfaction with end-of-life care in the ICU (23, 24), but our study is the first to proactively and systematically engage mechanically ventilated ICU patients who are not necessarily dying. With technological advances, many critically ill patients now survive what were previously fatal illnesses (40, 41), but survivors of mechanical ventilation are increasingly recognized to suffer from anxiety, depression, and post-traumatic stress disorder (42–44). Our finding that chaplain-led spiritual care potentially improves stress after the ICU and helps ICU survivors’ ability to cope raises the possibility that chaplain-led picture-guided spiritual care with follow up may be able to help prevent or alleviate these psychiatric sequelae of critical illness.
Our study has several limitations. A single chaplain provided all of the picture-guided spiritual care. Participants were primarily MICU patients sampled from an urban tertiary care center with several organ transplantation programs, but our subgroup analyses suggest little difference in the magnitude of anxiety and stress reduction in transplant and nontransplant patients who received mechanical ventilation. The feasibility of chaplain-led picture-guided spiritual care needs to be externally validated with other chaplains, in cardiac and pediatric ICU patients, and in other hospitals where case mix and patient care may differ. These validation studies should also evaluate the psychometrics of the spiritual care communication card and assess whether refinements to the card should be made. Although other ICU healthcare providers could potentially use parts of the card to screen for patients with spiritual care needs, we recommend at this time that only chaplains use the card, because they are formally trained in how to best engage communication on spiritual matters. We did not study how spiritual care affected end-of-life care among decedents, but prior studies have already shown a benefit (23, 24). Future studies of chaplain-led picture-guided spiritual care should evaluate its effect on those who die in the ICU and their families’ satisfaction with ICU care. We limited our measurements of symptoms to 100-mm VAS for anxiety after the first visit and stress and pain among ICU survivors at a single follow-up visit. Future studies should consider using more comprehensive and repeated assessments of symptoms (45, 46), spiritual quality of life (47), and coping (48–50) to determine the optimal dose of spiritual care needed to improve well-being. Although our quasi-experimental study design shows a potential for efficacy of chaplain-led picture-guided spiritual care, there is no psychometric measurement support for asking subjects to recall stress reduction. Furthermore, only a randomized controlled trial can prove efficacy, and measurements of anxiety, depression, and post-traumatic stress disorder after hospital discharge should be considered as outcomes among ICU survivors.
In conclusion, our findings demonstrate that chaplain-led picture-guided spiritual care is feasible among awake and alert mechanically ventilated adults and suggest that it may reduce anxiety during and stress after an ICU admission. Using this novel picture guide will facilitate a paradigm shift in the role of chaplains in acute care settings. Instead of primarily being consulted just before a patient’s death in the ICU, chaplains can now provide interactive spiritual support to mechanically ventilated ICU patients. This strategy represents a significant step forward in being able to integrate spiritual care with intensive care and shows promise to improve adult patients’ well-being both during and after critical illness.
Footnotes
Supported by National Institutes of Health grants UL1 TR000040, KL2 TR000081, and K23AG045560. The views expressed in this article do not communicate an official position of National Institutes of Health.
Author Contributions: M.R.B. and A.D.P. had full access to all of the data in the study and take responsibility for the integrity of the data and accuracy of the data analysis. Study concept and design: M.R.B. and J.N.B. Acquisition, analysis, or interpretation of data: M.R.B., J.N.B., S.M.B., K.R.P., and A.D.P. Drafting of the manuscript: M.R.B. Critical revision of the manuscript for important intellectual content: M.R.B., J.N.B., D.B., N.E.G., and D.J.L. Statistical analysis: M.R.B. and A.D.P. Study supervision: M.R.B. and J.N.B.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Khalaila R, Zbidat W, Anwar K, Bayya A, Linton DM, Sviri S. Communication difficulties and psychoemotional distress in patients receiving mechanical ventilation. Am J Crit Care. 2011;20:470–479. doi: 10.4037/ajcc2011989. [DOI] [PubMed] [Google Scholar]
- 2.Patak L, Gawlinski A, Fung NI, Doering L, Berg J. Patients’ reports of health care practitioner interventions that are related to communication during mechanical ventilation. Heart Lung. 2004;33:308–320. doi: 10.1016/j.hrtlng.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 3.Happ MB, Garrett K, Thomas DD, Tate J, George E, Houze M, Radtke J, Sereika S. Nurse-patient communication interactions in the intensive care unit. Am J Crit Care. 2011;20:e28–e40. doi: 10.4037/ajcc2011433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meltzer EC, Gallagher JJ, Suppes A, Fins JJ. Lip-reading and the ventilated patient. Crit Care Med. 2012;40:1529–1531. doi: 10.1097/CCM.0b013e318241e56c. [DOI] [PubMed] [Google Scholar]
- 5.Tate JA, Devito Dabbs A, Hoffman LA, Milbrandt E, Happ MB. Anxiety and agitation in mechanically ventilated patients. Qual Health Res. 2012;22:157–173. doi: 10.1177/1049732311421616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Happ MB. Caring to communicate revisited. Crit Care Med. 2012;40:1672–1673. doi: 10.1097/CCM.0b013e3182452016. [DOI] [PubMed] [Google Scholar]
- 7.Albarran AW. A review of communication with intubated patients and those with tracheostomies within an intensive care environment. Intensive Care Nurs. 1991;7:179–186. doi: 10.1016/0266-612x(91)90007-e. [DOI] [PubMed] [Google Scholar]
- 8.Lawless CA. Helping patients with endotracheal and tracheostomy tubes communicate. Am J Nurs. 1975;75:2151–2153. [PubMed] [Google Scholar]
- 9.Campbell GB, Happ MB. Symptom identification in the chronically critically ill. AACN Adv Crit Care. 2010;21:64–79. doi: 10.1097/NCI.0b013e3181c932a8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gleason JJ. The pastoral caregiver’s casebook. Valley Forge, PA: Judson Press; 2015. [Google Scholar]
- 11.Puntillo KA, Smith D, Arai S, Stotts N. Critical care nurses provide their perspectives of patients' symptoms in intensive care units. Heart Lung. 2008;37:466–475. doi: 10.1016/j.hrtlng.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 12.Patak L, Gawlinski A, Fung NI, Doering L, Berg J, Henneman EA. Communication boards in critical care: patients’ views. Appl Nurs Res. 2006;19:182–190. doi: 10.1016/j.apnr.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 13.Stovsky B, Rudy E, Dragonette P. Comparison of two types of communication methods used after cardiac surgery with patients with endotracheal tubes. Heart Lung. 1988;17:281–289. [PubMed] [Google Scholar]
- 14.Happ MB, Garrett KL, Tate JA, DiVirgilio D, Houze MP, Demirci JR, George E, Sereika SM. Effect of a multi-level intervention on nurse-patient communication in the intensive care unit: results of the SPEACS trial. Heart Lung. 2014;43:89–98. doi: 10.1016/j.hrtlng.2013.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barr J, Pandharipande PP. The pain, agitation, and delirium care bundle: synergistic benefits of implementing the 2013 Pain, Agitation, and Delirium Guidelines in an integrated and interdisciplinary fashion. Crit Care Med. 2013;41:S99–S115. doi: 10.1097/CCM.0b013e3182a16ff0. [DOI] [PubMed] [Google Scholar]
- 16.Riker RR, Fraser GL. Altering intensive care sedation paradigms to improve patient outcomes. Crit Care Clin. 2009;25:527–538, viii–ix. doi: 10.1016/j.ccc.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 17.Happ MB, Seaman JB, Nilsen ML, Sciulli A, Tate JA, Saul M, Barnato AE. The number of mechanically ventilated ICU patients meeting communication criteria. Heart Lung. 2015;44:45–49. doi: 10.1016/j.hrtlng.2014.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hodge DR. A template for spiritual assessment: a review of the JCAHO requirements and guidelines for implementation. Soc Work. 2006;51:317–326. doi: 10.1093/sw/51.4.317. [DOI] [PubMed] [Google Scholar]
- 19.Ferrell B, Connor SR, Cordes A, Dahlin CM, Fine PG, Hutton N, Leenay M, Lentz J, Person JL, Meier DE, et al. National Consensus Project for Quality Palliative Care Task Force Members. The national agenda for quality palliative care: the National Consensus Project and the National Quality Forum. J Pain Symptom Manage. 2007;33:737–744. doi: 10.1016/j.jpainsymman.2007.02.024. [DOI] [PubMed] [Google Scholar]
- 20.Koenig HG, Bearon LB, Hover M, Travis JL., III Religious perspectives of doctors, nurses, patients, and families. J Pastoral Care. 1991;45:254–267. doi: 10.1177/002234099104500306. [DOI] [PubMed] [Google Scholar]
- 21.Balboni TA, Vanderwerker LC, Block SD, Paulk ME, Lathan CS, Peteet JR, Prigerson HG. Religiousness and spiritual support among advanced cancer patients and associations with end-of-life treatment preferences and quality of life. J Clin Oncol. 2007;25:555–560. doi: 10.1200/JCO.2006.07.9046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ehman JW, Ott BB, Short TH, Ciampa RC, Hansen-Flaschen J. Do patients want physicians to inquire about their spiritual or religious beliefs if they become gravely ill? Arch Intern Med. 1999;159:1803–1806. doi: 10.1001/archinte.159.15.1803. [DOI] [PubMed] [Google Scholar]
- 23.Johnson JR, Engelberg RA, Nielsen EL, Kross EK, Smith NL, Hanada JC, Doll O’Mahoney SK, Curtis JR. The association of spiritual care providers’ activities with family members’ satisfaction with care after a death in the ICU. Crit Care Med. 2014;42:1991–2000. doi: 10.1097/CCM.0000000000000412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wall RJ, Engelberg RA, Gries CJ, Glavan B, Curtis JR. Spiritual care of families in the intensive care unit. Crit Care Med. 2007;35:1084–1090. doi: 10.1097/01.CCM.0000259382.36414.06. [DOI] [PubMed] [Google Scholar]
- 25.Choi PJ, Curlin FA, Cox CE. “The patient is dying, please call the chaplain”: the activities of chaplains in one medical center’s intensive care units. J Pain Symptom Manage. 2015;50:501–506. doi: 10.1016/j.jpainsymman.2015.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Todres ID, Catlin EA, Thiel MM. The intensivist in a spiritual care training program adapted for clinicians. Crit Care Med. 2005;33:2733–2736. doi: 10.1097/01.ccm.0000189749.24916.40. [DOI] [PubMed] [Google Scholar]
- 27.Selman L, Young T, Vermandere M, Stirling I, Leget C Research Subgroup of European Association for Palliative Care Spiritual Care Taskforce. Research priorities in spiritual care: an international survey of palliative care researchers and clinicians. J Pain Symptom Manage. 2014;48:518–531. doi: 10.1016/j.jpainsymman.2013.10.020. [DOI] [PubMed] [Google Scholar]
- 28.Sulmasy DP. Spirituality, religion, and clinical care. Chest. 2009;135:1634–1642. doi: 10.1378/chest.08-2241. [DOI] [PubMed] [Google Scholar]
- 29.The Association of Professional ChaplainsStandards of practice in acute care. 2009 [accessed 2015. Jul 22]. Available from: http://www.professionalchaplains.org/files/professional_standards/standards_of_practice/standards_practice_professional_chaplains_acute_care.pdf
- 30.Ely EW, Truman B, Shintani A, Thomason JW, Wheeler AP, Gordon S, Francis J, Speroff T, Gautam S, Margolin R, et al. Monitoring sedation status over time in ICU patients: reliability and validity of the Richmond Agitation-Sedation Scale (RASS) JAMA. 2003;289:2983–2991. doi: 10.1001/jama.289.22.2983. [DOI] [PubMed] [Google Scholar]
- 31.Ely EW, Inouye SK, Bernard GR, Gordon S, Francis J, May L, Truman B, Speroff T, Gautam S, Margolin R, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU) JAMA. 2001;286:2703–2710. doi: 10.1001/jama.286.21.2703. [DOI] [PubMed] [Google Scholar]
- 32.Delgado-Guay MO, Hui D, Parsons HA, Govan K, De la Cruz M, Thorney S, Bruera E. Spirituality, religiosity, and spiritual pain in advanced cancer patients. J Pain Symptom Manage. 2011;41:986–994. doi: 10.1016/j.jpainsymman.2010.09.017. [DOI] [PubMed] [Google Scholar]
- 33.Hill CE. Helping skills: facilitation exploration, insight, and action. Washington DC: American Psychological Association; 2009. [Google Scholar]
- 34.Kahn JM, Le T, Angus DC, Cox CE, Hough CL, White DB, Yende S, Carson SS ProVent Study Group Investigators. The epidemiology of chronic critical illness in the United States. Crit Care Med. 2015;43:282–287. doi: 10.1097/CCM.0000000000000710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rotondi AJ, Chelluri L, Sirio C, Mendelsohn A, Schulz R, Belle S, Im K, Donahoe M, Pinsky MR. Patients’ recollections of stressful experiences while receiving prolonged mechanical ventilation in an intensive care unit. Crit Care Med. 2002;30:746–752. doi: 10.1097/00003246-200204000-00004. [DOI] [PubMed] [Google Scholar]
- 36.Candy B, Jones L, Varagunam M, Speck P, Tookman A, King M. Spiritual and religious interventions for well-being of adults in the terminal phase of disease. Cochrane Database Syst Rev. 2012;5:CD007544. doi: 10.1002/14651858.CD007544.pub2. [DOI] [PubMed] [Google Scholar]
- 37.Danis M, Pollack JM. The valuable contribution of spiritual care to end-of-life care in the ICU. Crit Care Med. 2014;42:2131–2132. doi: 10.1097/CCM.0000000000000470. [DOI] [PubMed] [Google Scholar]
- 38.McBride JL, Pilkington L, Arthur G. Development of brief pictorial instruments for assessing spirituality in primary care. J Ambul Care Manage. 1998;21:53–61. doi: 10.1097/00004479-199810000-00004. [DOI] [PubMed] [Google Scholar]
- 39.Iwashyna TJ. Survivorship will be the defining challenge of critical care in the 21st century. Ann Intern Med. 2010;153:204–205. doi: 10.7326/0003-4819-153-3-201008030-00013. [DOI] [PubMed] [Google Scholar]
- 40.Spragg RG, Bernard GR, Checkley W, Curtis JR, Gajic O, Guyatt G, Hall J, Israel E, Jain M, Needham DM, et al. Beyond mortality: future clinical research in acute lung injury. Am J Respir Crit Care Med. 2010;181:1121–1127. doi: 10.1164/rccm.201001-0024WS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lerolle N, Trinquart L, Bornstain C, Tadié JM, Imbert A, Diehl JL, Fagon JY, Guérot E. Increased intensity of treatment and decreased mortality in elderly patients in an intensive care unit over a decade. Crit Care Med. 2010;38:59–64. doi: 10.1097/CCM.0b013e3181b088ec. [DOI] [PubMed] [Google Scholar]
- 42.Mikkelsen ME, Christie JD, Lanken PN, Biester RC, Thompson BT, Bellamy SL, Localio AR, Demissie E, Hopkins RO, Angus DC. The adult respiratory distress syndrome cognitive outcomes study: long-term neuropsychological function in survivors of acute lung injury. Am J Respir Crit Care Med. 2012;185:1307–1315. doi: 10.1164/rccm.201111-2025OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Davydow DS, Gifford JM, Desai SV, Needham DM, Bienvenu OJ. Posttraumatic stress disorder in general intensive care unit survivors: a systematic review. Gen Hosp Psychiatry. 2008;30:421–434. doi: 10.1016/j.genhosppsych.2008.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wunsch H, Christiansen CF, Johansen MB, Olsen M, Ali N, Angus DC, Sørensen HT. Psychiatric diagnoses and psychoactive medication use among nonsurgical critically ill patients receiving mechanical ventilation. JAMA. 2014;311:1133–1142. doi: 10.1001/jama.2014.2137. [DOI] [PubMed] [Google Scholar]
- 45.Chang VT, Hwang SS, Feuerman M. Validation of the Edmonton Symptom Assessment Scale. Cancer. 2000;88:2164–2171. doi: 10.1002/(sici)1097-0142(20000501)88:9<2164::aid-cncr24>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 46.Nelson JE, Meier DE, Oei EJ, Nierman DM, Senzel RS, Manfredi PL, Davis SM, Morrison RS. Self-reported symptom experience of critically ill cancer patients receiving intensive care. Crit Care Med. 2001;29:277–282. doi: 10.1097/00003246-200102000-00010. [DOI] [PubMed] [Google Scholar]
- 47.Peterman AH, Fitchett G, Brady MJ, Hernandez L, Cella D. Measuring spiritual well-being in people with cancer: the functional assessment of chronic illness therapy--Spiritual Well-being Scale (FACIT-Sp) Ann Behav Med. 2002;24:49–58. doi: 10.1207/S15324796ABM2401_06. [DOI] [PubMed] [Google Scholar]
- 48.Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol. 1989;56:267–283. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- 49.Carver CS. You want to measure coping but your protocol’s too long: consider the brief COPE. Int J Behav Med. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 50.Pargament KI, Koenig HG, Perez LM. The many methods of religious coping: development and initial validation of the RCOPE. J Clin Psychol. 2000;56:519–543. doi: 10.1002/(sici)1097-4679(200004)56:4<519::aid-jclp6>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]