Abstract
Post-traumatic or postsurgical flexion contractures of the knee can significantly limit function and lead to gait abnormalities. In this setting, interventions to regain full extension may include bracing, physical therapy, and open or arthroscopic surgery. Open surgical approaches to restore full motion often demand extensive recovery and promote further adhesions and loss of motion, which has led to the advent of arthroscopic techniques to address these pathologies. We present a safe, effective, and reproducible arthroscopic technique for posteromedial capsular release to address knee flexion contractures.
Posterior capsular contracture is a complication that can result from trauma or prior knee surgery. This condition often prevents the patient from fully extending the knee, which is required to perform a normal gait pattern.1
Both posterior capsular contracture and arthrofibrosis can significantly alter a patient's normal functioning and adversely affect postoperative outcomes,2 even with a dedicated rehabilitation program. Although multiligament reconstructions of the knee and meniscal transplants have been identified to have the highest incidence of postoperative deficit in knee extension,3 limitation in knee extension can also be the result of intra-articular pathologies such as adhesion bands, cyclops lesions after anterior cruciate ligament reconstructions, soft-tissue calcifications, and anteriorly placed anterior cruciate ligament tibial reconstruction tunnels or extra-articular causes such as a fibrotic posterior joint capsule.1, 4 When supervised physical therapy rehabilitation fails to improve range of motion, more extensive measures such as manipulation under anesthesia and lysis of adhesions are indicated.3
However, when the main component contributing to an extension deficit is found to be contracture of the posterior capsule, selective posteromedial capsular release can significantly improve function and range of motion. Open4 and arthroscopic2 procedures have been reported in the literature, with the goal of each to regain adequate posterior capsular tension and space to allow the knee joint to fully extend. Typically, a posteromedial release is sufficient; however, a posterolateral approach can be added if necessary to complete a transverse release of the posterior capsule.4, 5 In either setting, early recognition and treatment are accepted to comprise the most important factor to achieve good results.6 The purpose of this technical note was to describe the surgical technique for an arthroscopic posteromedial capsular release for the treatment of knee flexion contractures resulting from posterior capsular contraction.
Surgical Technique
Indications
This technique is indicated for flexion contractures of the knee principally caused by scarring in the posterior capsule, resulting in a symptomatic knee extension deficit of 10° or more compared with the uninjured contralateral knee.2 Before a posteromedial capsular release is performed, a trial of conservative measures should be attempted, including an aggressive supervised physical therapy regimen and knee bracing. If the extension deficit persists despite these conservative methods, manipulation under anesthesia or an anterior interval release and/or notchplasty and debridement can be performed. If all of the aforementioned methods fail to regain full extension, a posteromedial capsular release is indicated.
Patient Positioning
The patient is placed in the supine position on the operating table. After induction of general anesthesia, a bilateral knee examination is performed, and a goniometer is used to measure maximum flexion and extension in both the normal and operative legs (Fig 1, Video 1). Gentle and careful manipulation is performed in an attempt to regain full extension. Next, the surgeon should proceed with the planned arthroscopic intervention. The operative leg is secured to the operating table with a leg holder (Mizuho OSI, Union City, CA), and a well-padded high-thigh tourniquet is secured on the operative leg. The contralateral knee is abducted and placed into a stirrup (Birkova Products, Gothenburg, NE) to provide sufficient space to access a posteromedial arthroscopic portal.
Fig 1.
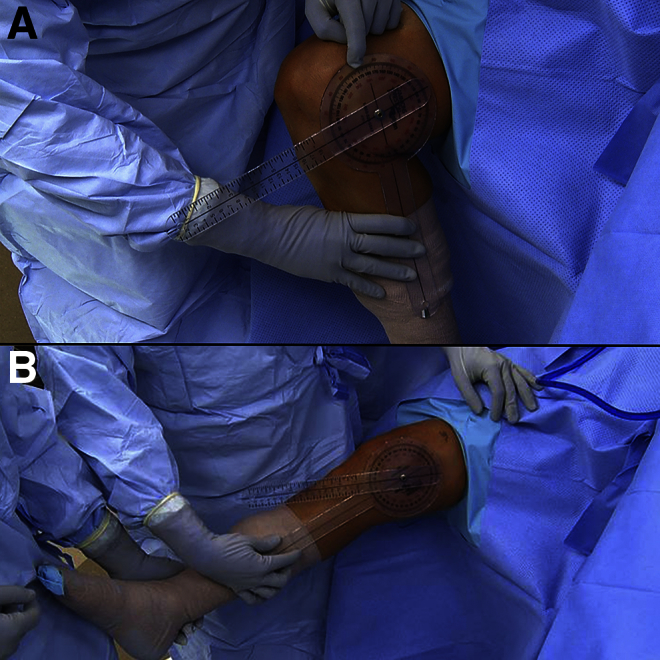
Intraoperative photographs after placing the patient in the supine position on the operating table with the operative leg secured in a leg holder. Range of motion is assessed, and the affected right knee shows maximum flexion (A) and extension (B) from 23° to 102° as measured by a goniometer.
Step 1: Diagnostic Arthroscopy and Initial Debridement
Anteromedial and anterolateral portals are created adjacent to the patellar tendon, and a diagnostic arthroscopy is performed. The suprapatellar pouch is assessed and cleared of adhesions and fibrous bands. Careful debridement of the fibrous pathology in this space allows for increases in flexion and patellar mobility. Next, the anterior interval and medial and lateral gutters are evaluated and similarly debrided if necessary (Fig 2, Fig 3, Fig 4). To ensure full release and assessment of these compartments, the arthroscope should be switched between the anteromedial and anterolateral portals.
Fig 2.
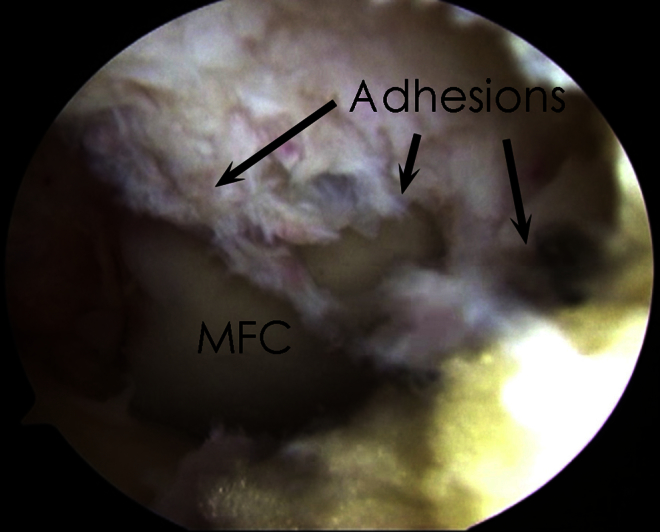
Intra-articular space of the right knee viewed through the anterolateral portal. Extensive adhesions are seen in the anterior interval and anterior to the medial femoral condyle (MFC).
Fig 3.
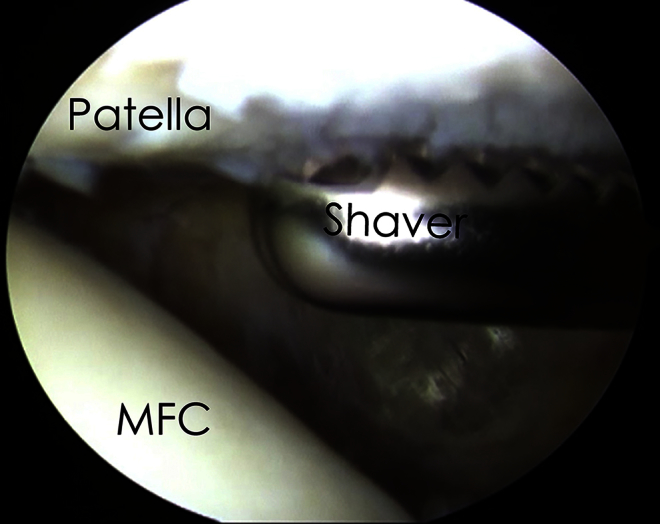
Subpatellar space of the right knee viewed through the anterolateral portal. Significant peripatellar adhesions are seen and released with the aid of an arthroscopic shaver placed through the anteromedial portal. (MFC, medial femoral condyle.)
Fig 4.
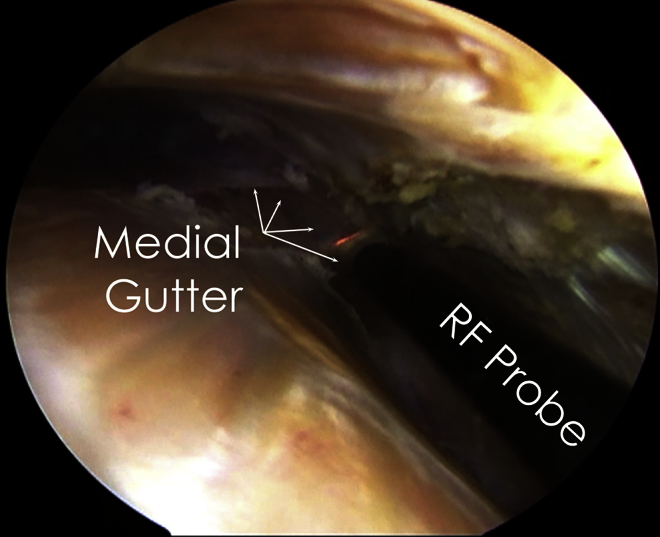
Medial gutter of the right knee viewed through the anterolateral portal. Medial gutter adhesions are noted and are released with a radiofrequency (RF) probe placed through the anteromedial portal.
Step 2: Manipulation
After evaluation and treatment of all anterior knee pathology, gentle manipulation is again performed to assess range of motion and to evaluate for any residual extension deficit. If full extension cannot be achieved, the surgeon should proceed with an arthroscopic posterior capsular release.
Step 3: Access to Posteromedial Compartment
To locate the posteromedial compartment of the knee, a 30° arthroscope (Smith & Nephew, Andover, MA) is carefully inserted between the medial femoral condyle and the posterior cruciate ligament (PCL) so that it is medial to the PCL. If adhesions prevent access to the aforementioned location, a blunt arthroscopic obturator may be used to break the adhesions so that the arthroscope may pass through this interval.
Step 4: Creation of Posteromedial Portal
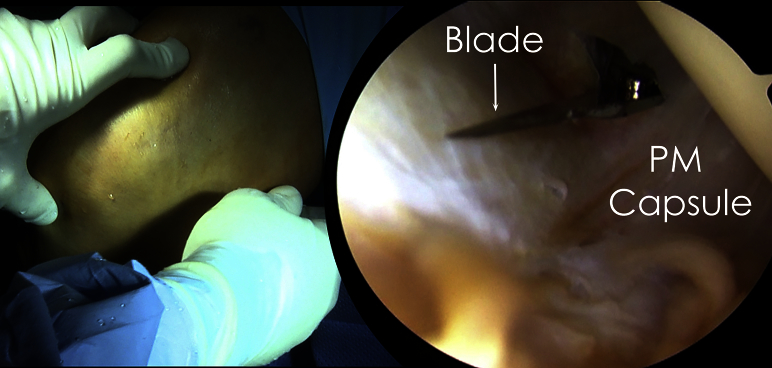
With the arthroscope in position, the entry site for instrumentation for the posteromedial capsular release can be found in the soft spot between the posterior oblique ligament, the medial head of the gastrocnemius, and the semimembranosus tendon.7 At this location, an 18-gauge spinal needle is inserted intra-articularly into the posteromedial compartment of the knee under direct arthroscopic visualization. While direct visualization is maintained, the spinal needle is removed and a small incision is created at the location projected by the needle under arthroscopic visualization (Fig 5). Through this incision, a cannula is inserted into the posteromedial joint. Of note, the sartorial branch of the long saphenous nerve runs with the long saphenous vein approximately 10 mm posterior to the ideal portal location.8
Fig 5.
Intraoperative and arthroscopic views of the right knee maintained in flexion in a knee holder. The arthroscope is placed in the anterolateral portal and carefully guided into the posterior compartment of the knee. With the arthroscope in the posterior compartment, a spinal needle is placed between the posterior oblique ligament, the medial head of the gastrocnemius, and the semimembranosus tendon. The spinal needle is then removed, and a small incision is made using a No. 11 blade in the posteromedial (PM) capsule.
Step 5: Posteromedial Capsular Release
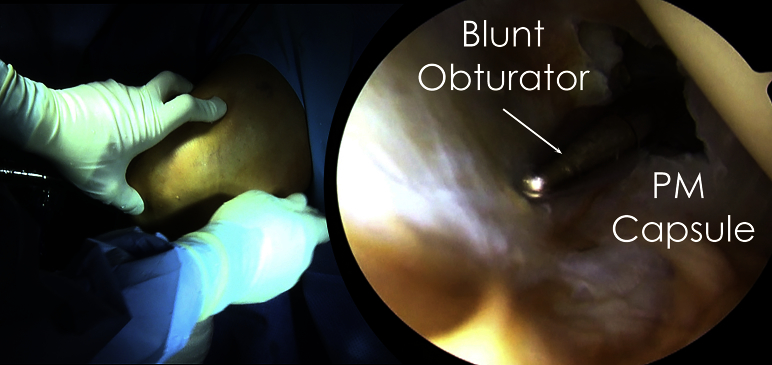
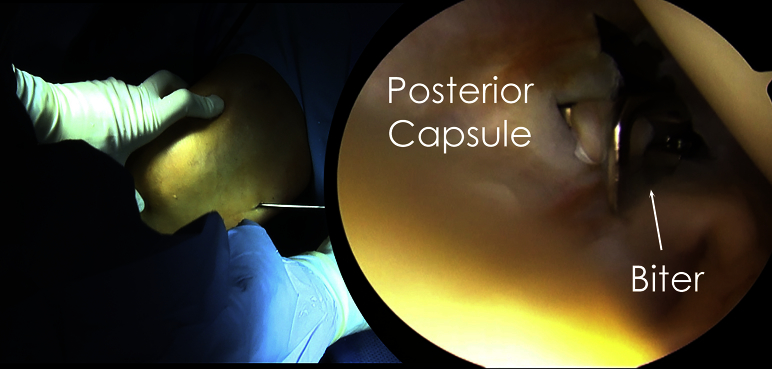
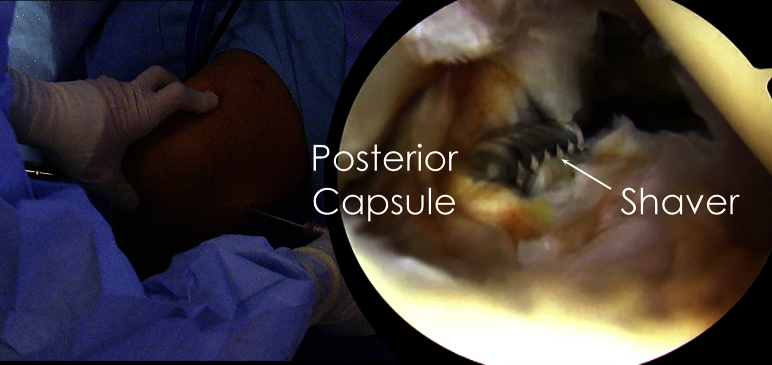
Once the portal is established, a blunt obturator or small periosteal elevator is used to gently separate the posteromedial capsule from the medial gastrocnemius muscle and tendon (Fig 6). This step is critical to avoid damaging the posterior neurovascular structures when releasing the capsule. Next, a series of shavers and biters (Smith & Nephew) are used to release the posteromedial capsule (Fig 7). Of note, when using the shaver, the surgeon should always keep the shaver blade facing anteriorly to avoid damaging the neurovascular bundle (Fig 8). The surgeon begins medially and works laterally as the capsule is released. He or she continues until the midline is reached, in line with the PCL. The arthroscope is inserted into the posteromedial portal to help identify how much of the capsule can be released. As the posteromedial capsule is released, the gastrocnemius muscle and tendon become visible. Switching to a 70° arthroscopic camera (Smith & Nephew) during the release is recommended to help view the posteromedial capsule.
Fig 6.
Intraoperative and arthroscopic views of the right knee maintained in flexion in a knee holder. After a small incision is made in the posteromedial capsule and while the posteromedial capsule is viewed directly through the anterolateral portal, a blunt obturator or small periosteal elevator is used to gently separate the posteromedial (PM) capsule from the medial gastrocnemius muscle and tendon.
Fig 7.
Intraoperative and arthroscopic views of the right knee maintained in flexion in a knee holder. While the posteromedial capsule is viewed directly through the anterolateral portal, an arthroscopic biter is used to release the posteromedial capsule in a medial-to-lateral direction until the midline is reached.
Fig 8.
Intraoperative and arthroscopic views of the right knee maintained in flexion in a knee holder. While the posteromedial capsule is viewed directly through the anterolateral portal, an arthroscopic shaver is used to clear any remaining debris or fibrous tissue. When using the shaver, the surgeon should always keep the blade facing anteriorly to avoid damaging the posterior neurovascular bundle.
Step 6: Range of Motion and Manipulation
After completion of the posteromedial capsular release, range of motion is again assessed and compared with the preoperative state as well as the contralateral knee. To ensure that full extension can be attained in the operative knee, the distal thigh is held to the table while the heel is lifted (Fig 9). If the heel can be lifted off the table, some degree of hyperextension can be achieved. If full extension is not easily achieved, manipulation is again performed. If full extension remains unattainable, a posterolateral capsular release can be considered.4, 5
Fig 9.

Intraoperative photograph with the patient in the supine position on the operating table. After completion of the posteromedial capsular release, range of motion is again assessed using a goniometer and compared with the preoperative state as well as the contralateral knee. To ensure that full extension can be attained in the operative knee, the distal thigh is held to the table while the heel is lifted.
Postoperative Rehabilitation
Postoperatively, patients are allowed to bear weight as tolerated with crutches and can wean off crutches as soon as they are able to walk with minimal pain and without a limp. For patients with an isolated extension deficit, a dynamic extension splint is prescribed for alternating periods of 4 hours while admitted to the hospital and is to be worn throughout the night. For patients treated for combined extension and flexion deficits, a dynamic extension split should be worn for 4 hours and rotated with 4 hours of continuous passive motion with the machine set to full range of motion at slow speed. On discharge, the dynamic extension splint should be used for a minimum of 2 hours twice per day and during sleep for 6 weeks, after which patients are re-evaluated to determine if continued use is necessary.
Adequate postoperative analgesia control is imperative to maintain full extension. An indwelling epidural catheter is used on a case-by-case basis depending on how well the patient is managing his or her pain, particularly if the patient cannot maintain full extension in the splint without pain. Before discharge, an indwelling catheter may be placed for pain control for up to 48 hours. After this period or on discharge without a catheter, the patient is transitioned to oral pain medication. A cold compression device is used to control pain and edema.
Supervised physical therapy is performed daily for the first 2 weeks with an emphasis on full range of motion. For the first 6 weeks, only low-impact activities should be performed, followed by a progressive increase in activity level as tolerated. If at any point knee extension decreases, the patient's activity level should be scaled back. Pearls and pitfalls of the described procedure are listed in Table 1.
Table 1.
Pearls and Pitfalls
| Pearls |
| The surgeon should create the posteromedial portal as proximally as possible to enhance visualization and freedom of movement. |
| A blunt obturator cannula or a small periosteal elevator should be used to gently separate the posteromedial structures from the medial gastrocnemius muscle and tendon. |
| The surgeon should face the shaver toward the arthroscope to avoid injuring the neurovascular bundle. |
| Use of a 70° arthroscope can improve visualization in some cases. |
| Pitfalls |
| Placing the posteromedial portal in the wrong anatomic location can make the procedure technically difficult. |
| Placing the portal too posterior can damage the sartorial branch of the long saphenous nerve. |
| Failing to release structures adhered to the posterior capsule increases the risk of vascular injury. |
| Rehabilitation is a key part of the procedure because adhesions and contractures can reoccur. |
Discussion
Extension deficits are one of the leading causes of adverse outcomes after surgical procedures on the knee, and the most common cause of post-traumatic or postsurgical extension deficits is contracture of the posterior capsule.1, 9, 10 An uneven gait and patellofemoral irritability can result from as little as a 5° to 10° loss of extension,1, 11 whereas a functional leg-length discrepancy can occur at more than 20° of extension loss.1 Although nonoperative techniques remain the first line of treatment, the arthroscopic posteromedial capsular release technique described in this report is a safe, effective, and reproducible option to address loss of knee extension if conservative treatment fails.
Arthroscopic posteromedial capsular release has yielded a very high success rate in postoperative outcome studies.2 A study performed by LaPrade et al.2 evaluated 15 patients with an average flexion contracture of 15° who underwent a posteromedial capsular release. At an average follow-up of 24 months, patients' extension deficit had significantly reduced to an average of 0.7°. The results of this study suggest that arthroscopic posteromedial capsular release is an effective surgical procedure to correct knee extension deficits when conservative treatments fail. Furthermore, there were no postoperative complications associated with the procedure, such as intraoperative fractures, postoperative infections, or deep vein thromboses.
Lobenhoffer et al.5 proposed an open posteromedial capsular release to treat posterior capsule contractures. Despite a larger incision, this technique has limited visibility, which increases the potential for iatrogenic damage.2 General advantages of arthroscopic surgery compared with open procedures on the knee include a less invasive nature, decreased operating time, quicker recovery, and decreased postoperative pain.2
A combined capsular release technique for severe flexion contracture with involved gastrocnemius contracture was proposed by Mariani.12 In addition to release of the posteromedial capsule, release of the posterolateral capsule and both gastrocnemius tendons was performed in 18 patients. Patients' extension deficits were reduced on average from 34° preoperatively to 3° at 1 year of follow-up. These results suggest that release of the posteromedial capsule, posterolateral capsule, and gastrocnemius tendons may be indicated for patients with severe flexion contractures. Furthermore, Mariani proposed the use of a posterior trans-septal portal through the posterior septum to allow simultaneous visualization and instrumentation of the entire posterior compartment for the combined release. However, this approach poses significant risk to neurovascular structures, and iatrogenic injury has been reported.13
Although a technically demanding procedure, posteromedial capsular release effectively treats extension deficits caused by contracture of the posterior capsule. When nonoperative techniques and manipulation under anesthesia do not correct flexion contractures, arthroscopic posteromedial capsular release is a viable option to treat this pathology. Advantages and limitations of this technique are summarized in Table 2. We recommend our method of arthroscopic posteromedial capsular release for posterior capsular contracture of the knee and encourage further studies by other groups to investigate and assess our surgical technique.
Table 2.
Advantages and Limitations
| Advantages |
| Possibility of extension in patients in whom conservative treatment failed |
| Good outcomes reported in literature |
| Limitations |
| Technically demanding—experienced surgeon recommended |
| Neurovascular risk |
| Higher chances of failure if not performed concurrently with rehabilitation |
Footnotes
The authors report the following potential conflict of interest or source of funding: Institution provided support by Arthrex, Ossur, Siemens, and Smith & Nephew. R.F.L. receives support from Arthrex; Smith & Nephew; Ossur; Health East, Norway; and an NIH R13 grant for biologics.
Supplementary Data
Posteromedial capsular release in a right knee. The patient is placed in the supine position on the operating table, and a goniometer is used to measure the baseline knee range of motion. Preoperatively, range of motion was 23° to 102° of knee flexion. An anterolateral portal is created, followed by an anteromedial portal, and a diagnostic arthroscopy is performed. Fibrous adhesions are released in the anterior interval with the aid of an arthroscopic biter, shaver, and radiofrequency probe. The suprapatellar pouch is assessed and cleared of adhesions and fibrous bands. In a similar manner, lysis of adhesions is performed on the medial and lateral gutters. With the arthroscope in position, the entry site for instrumentation for the posteromedial capsular release can be found in the soft spot between the posterior oblique ligament, the medial head of the gastrocnemius, and the semimembranosus tendon. At this location, a small incision is made intra-articularly into the posteromedial compartment under direct arthroscopic visualization. Once the portal is established, a blunt obturator is used to gently separate the posteromedial structures from the medial gastrocnemius muscle and tendon. This step is critical to avoid injuring the posterior neurovascular structures when releasing the capsule. A series of biters and shavers are used to release the posteromedial capsule. The release begins medially and works laterally as the capsule is released. The release continues until the midline is reached. After completion of the posteromedial capsular release, the incisions are closed and range of motion is again assessed and compared with the preoperative state.
References
- 1.Cosgarea A.J., DeHaven K.E., Lovelock J.E. The surgical treatment of arthrofibrosis of the knee. Am J Sports Med. 1994;22:184–191. doi: 10.1177/036354659402200206. [DOI] [PubMed] [Google Scholar]
- 2.LaPrade R.F., Pedtke A.C., Roethle S.T. Arthroscopic posteromedial capsular release for knee flexion contractures. Knee Surg Sports Traumatol Arthrosc. 2008;16:469–475. doi: 10.1007/s00167-008-0496-z. [DOI] [PubMed] [Google Scholar]
- 3.Werner B.C., Cancienne J.M., Miller M.D., Gwathmey F.W. Incidence of manipulation under anesthesia or lysis of adhesions after arthroscopic knee surgery. Am J Sports Med. 2015;43:1656–1661. doi: 10.1177/0363546515578660. [DOI] [PubMed] [Google Scholar]
- 4.Lindenfeld T.N., Wojtys E.M., Husain A. Surgical treatment of arthrofibrosis of the knee. Instr Course Lect. 2000;49:211–221. [PubMed] [Google Scholar]
- 5.Lobenhoffer H.P., Bosch U., Gerich T.G. Role of posterior capsulotomy for the treatment of extension deficits of the knee. Knee Surg Sports Traumatol Arthrosc. 1996;4:237–241. doi: 10.1007/BF01567970. [DOI] [PubMed] [Google Scholar]
- 6.Sanders TL, Kremers HM, Bryan AJ, Kremers WK, Stuart MJ, Krych AJ. Procedural intervention for arthrofibrosis after ACL reconstruction: Trends over two decades [published online September 26, 2015]. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-015-3799-x. [DOI] [PMC free article] [PubMed]
- 7.Ogilvie-Harris D.J., Biggs D.J., Mackay M., Weisleder L. Posterior portals for arthroscopic surgery of the knee. Arthroscopy. 1994;10:608–613. doi: 10.1016/s0749-8063(05)80056-8. [DOI] [PubMed] [Google Scholar]
- 8.Kramer D.E., Bahk M.S., Cascio B.M., Cosgarea A.J. Posterior knee arthroscopy: Anatomy, technique, application. J Bone Joint Surg Am. 2006;88:110–121. doi: 10.2106/JBJS.F.00607. [DOI] [PubMed] [Google Scholar]
- 9.Paulos L., Rosenberg T., Drawbert J., Manning J., Abbott P. Infrapatellar contracture syndrome: An unrecognized cause of knee stiffness with patella entrapment and patella infera. Am J Sports Med. 1987;15:331–341. doi: 10.1177/036354658701500407. [DOI] [PubMed] [Google Scholar]
- 10.Saito T., Takeuchi R., Yamamoto K., Yoshida T., Koshino T. Unicompartmental arthroplasty for osteoarthritis of the knee: Remaining postoperative flexion contracture affecting overall results. J Arthroplasty. 2003;18:612–618. doi: 10.1016/s0883-5403(03)00196-7. [DOI] [PubMed] [Google Scholar]
- 11.Sachs R.A., Daniel D.M., Stone M.L., Garfein R.F. Patellofemoral problems after anterior cruciate ligament reconstruction. Am J Sports Med. 1989;17:760–765. doi: 10.1177/036354658901700606. [DOI] [PubMed] [Google Scholar]
- 12.Mariani P.P. Arthroscopic release of the posterior compartments in the treatment of extension deficit of knee. Knee Surg Sports Traumatol Arthrosc. 2010;18:736–741. doi: 10.1007/s00167-009-0920-z. [DOI] [PubMed] [Google Scholar]
- 13.Hamula M., Sewick A.E., Kelly J.D. Arthroscopic trans-septal portal to treat extension deficits from arthrofibrosis. Univ Penn Orthop J. 2012;22:21–25. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Posteromedial capsular release in a right knee. The patient is placed in the supine position on the operating table, and a goniometer is used to measure the baseline knee range of motion. Preoperatively, range of motion was 23° to 102° of knee flexion. An anterolateral portal is created, followed by an anteromedial portal, and a diagnostic arthroscopy is performed. Fibrous adhesions are released in the anterior interval with the aid of an arthroscopic biter, shaver, and radiofrequency probe. The suprapatellar pouch is assessed and cleared of adhesions and fibrous bands. In a similar manner, lysis of adhesions is performed on the medial and lateral gutters. With the arthroscope in position, the entry site for instrumentation for the posteromedial capsular release can be found in the soft spot between the posterior oblique ligament, the medial head of the gastrocnemius, and the semimembranosus tendon. At this location, a small incision is made intra-articularly into the posteromedial compartment under direct arthroscopic visualization. Once the portal is established, a blunt obturator is used to gently separate the posteromedial structures from the medial gastrocnemius muscle and tendon. This step is critical to avoid injuring the posterior neurovascular structures when releasing the capsule. A series of biters and shavers are used to release the posteromedial capsule. The release begins medially and works laterally as the capsule is released. The release continues until the midline is reached. After completion of the posteromedial capsular release, the incisions are closed and range of motion is again assessed and compared with the preoperative state.