Abstract
We review our clinical studies of psychiatric comorbidity in short-term and long-term abstinent and in treatment naïve alcoholics (STAA, LTAA and TNA). TNA ypically have less severe alcoholism than treated abstinent samples and evidence less severe psychiatric disturbance. Lifetime psychiatric diagnoses are the norm for STAA and LTAA but not for TNA. Individuals with alcohol and drug use disorders show greater antisocial personality disturbance, but do not show differences in the mood or anxiety domains or in borderline personality disorder (BPD) symptoms. The studies show that alcoholics can achieve and maintain abstinence in the face of ongoing mood, anxiety, or BPD problems. By contrast, for ASPD, LTAA essentially stop current antisocial behaviors in all seven domains of antisocial behaviors. We believe that ongoing antisocial behavior is not consistent with maintaining abstinence, and that LTAA modify their antisocial behavior despite continued elevated social deviance proneness and antisocial dispositionality. Abstinent individuals without lifetime psychiatric disorders and TNA show more (subdiagnostic threshold) psychiatric symptoms and abnormal psychological measures than nonalcoholic controls in the mood, anxiety, BPD, and antisocial domains. In summary, our studies show that although LTAA have achieved multi-year abstinence, they still report significant psychological distress compared to NAC. We believe this distress may negatively affect their quality of life. This suggests the importance of developing effective care models to address comorbid mental health problems in LTAA. We also show that antisocial personality disorder symptoms decline to the levels seen in normal controls, and that excluding individuals from research with a psychiatric diagnosis does not control for subdiagnostic psychiatric differences between alcoholics and controls.
Keywords: alcoholism, psychiatric comorbidity
Introduction
Over the past 25 years the high prevalence of comorbid psychiatric disorders in individuals with an alcohol use disorder (AUD) or drug use disorder (DUD) (substance use disorders (SUDs) refers to both AUDs and DUDs) has been well documented in a number of large sample epidemiological studies (Regier et al. 1990; Kessler et al. 1997; Grant et al. 2004a; Grant et al. 2004b). In the Epidemiologic Catchment Area Study, about half of persons with an AUD (and ¾ of those with a DUD) had a co-occurring psychiatric disorder (a ‘dual-diagnosis’) (Regier et al. 1990). The National Comorbidity Study also found over ¾ of alcoholic men and women met lifetime criteria for a psychiatric diagnosis (Kessler et al. 1997). The greater psychiatric comorbidity in DUDs than AUDs (Currie et al. 2005; Grant et al. 2004a; Regier et al. 1990; Grant et al. 2009; Grant 2006; Hasin et al. 2007) increased psychiatric comorbidity rates for AUD individuals with comorbid DUDs. Psychiatric comorbidity is also greater in samples drawn from substance abuse treatment settings than in untreated community samples (Helzer and Pryzbeck 1988; Regier et al. 1990; Tomasson and Vaglum 1995). A large cross-national investigation of comorbidity reported strong associations of anxiety, mood, and antisocial personality disorders with SUDs, even in the context of large differences in the prevalence of these disorders across study sites (Merikangas et al. 1998). The more severe the substance use (on the continuums of use, problems, or dependence), the stronger the association with comorbid psychiatric disorders and, conversely, the greater the number of comorbid psychiatric disorders, the more severe the substance use pattern. It has also been shown that psychiatric comorbidity is greater in SUDs that have received treatment compared to untreated samples (Helzer and Pryzbeck 1988; Regier et al. 1990; Tomasson and Vaglum 1995).
The literature on the effects of psychiatric disorders on SUD treatment outcome has yielded less uniform results. Some studies reported a negative association between psychiatric comorbidity and treatment outcome (Burns et al. 2005; Greenfield et al. 1998; Hasin and Grant 2002; Hesselbrock et al. 1985; Loosen et al. 1990; Rounsaville et al. 1987; Schuckit 1983). By contrast, Chi and colleagues (Chi et al. 2006) showed that SUD individuals with comorbid psychiatric disorders (104 Subjects of 747) had one-year SUD treatment outcomes comparable to individuals with no comorbid psychiatric disorders. Bischof et al. (Bischof et al. 2005) contacted 4,075 individuals (response rate: 70.2%) in Northern Germany, of whom 3.8% met DSM-IV lifetime criteria for alcohol dependence and 1.3% were alcohol dependent in the last year. The percentage who remitted from alcohol dependence without formal help was almost identical for individuals with vs. without comorbid psychiatric disorders. Utilization of formal help was also unrelated to psychiatric comorbidity.
Review of Clinical Studies in our Laboratories
Studies in the San Francisco Bay Area
Psychiatric Comorbidity in Long-Term Abstinent Alcoholics
In 2000, we began clinical studies in Northern California of the neurobiology and clinical characteristics of long-term (greater than 6 month) abstinent alcoholics and treatment naïve actively drinking alcoholics. An important part of these studies involved the assessment of comorbid psychiatric problems. Table 1 presents the various measures (by domain) gathered in all the studies presented in this manuscript. Psychiatric diagnoses were assessed using the computerized Diagnostic Interview Schedule (c-DIS, (Robins LN 1998)) which was administered to all participants by a research associate. We found it helpful to have the research associate ask the individual the c-DIS questions to avoid the participants' frustration with the c-DIS decision tree. In addition, this allowed the research associate to compare participants' answers to the c-DIS with their phone screen and other volunteered information. The c-DIS generates a list of endorsed lifetime symptoms, and examines the symptoms to determine whether individuals met criteria for a lifetime diagnosis. The c-DIS assessed symptoms in the anxiety disorder domain of: Agoraphobia, Compulsive Disorder, Obsessive Disorder, Panic Disorder, Post-Traumatic Stress Disorder, and Social Phobia. In the mood disorder domain of: Dysthymia, Mania, and Major Depressive Disorder. In the externalizing disorder domain of: Antisocial Personality Disorder, and Conduct Disorder (without ASPD). If criteria for a lifetime diagnosis were met, the c-DIS followed up with questions about whether criteria were met for a current diagnosis (one that existed in the prior 12 months). The number of symptoms of anxiety, mood, and externalizing disorders were quantified as the sum total of the positive responses to all direct symptom questions for each diagnosis screened by the cDIS. Unfortunately, the cDIS does not gather information on whether symptoms are current, unless criteria for a lifetime diagnosis are met. The symptom count for a disorder did not include the positive responses to indirect symptom questions (e.g., for depression: “Was there any time in the last 12 months when you wanted to talk to a doctor or other health professional about feeling sad, depressed, or empty most of the time?”). Affirmative responses to indirect symptom questions are counted by the cDIS as criteria toward a positive diagnosis of a disorder, but in our study were considered secondary consequences of the direct symptoms, and therefore not counted toward a disorder’s symptom count. In addition, we gathered psychological measures of mood, anxiety, and externalizing problems. The psychological scales used to assess the anxiety construct were the Reiss-Epstein Anxiety Sensitivity Index (ASI) (Reiss et al. 1986), and the State and Trait Scales of the State-Trait Anxiety Inventory for Adults (STAI-S and STAI-T) (Reiss et al. 1986). Mood was assessed using the Depression and Hypomania Scales of the Minnesota Multiphasic Personality Inventory-2 (MMPI-D and MMPI-H) (Hathaway and McKinley 1989). The externalizing construct was assessed using the Socialization Scale of the California Psychological Inventory (CPI-SS) (Gough 1969) and the Psychopathic Deviance Scale of the MMPI-2 (MMPI-PD) (Hathaway and McKinley 1989).
Table 1.
Measures by Domain
| Mood Disorders Dys, Man, Hyp, MDD, Bipolar |
Anxiety Disorders Ag, OCD, PD, SP, PTSD |
ASPD | Borderline Disorder |
|
|---|---|---|---|---|
| California Study | ||||
| Lifetime Diagnosis | c-DIS: | c-DIS | c-DIS ASPD, CD | |
| Current (last year) Diagnosis | c-DIS | c-DIS | c-DIS ASPD c-DIS ASPD |
|
| Lifetime Symptoms | c-DIS | c-DIS | ||
| Psychological Measures | MMPI-DE, MMPI-Hy | ASI, STAI-S, STAI-T | MMPI-Pd, CPI Socialization Scale |
|
| Hawaii Study | ||||
| Lifetime Diagnosis | c-DIS: | c-DIS | c-DIS ASPD, AABO | |
| Current (last year) Diagnosis | c-DIS | c-DIS | c-DIS ASPD, AABO | |
| Lifetime Symptoms | c-DIS | c-DIS | c-DIS - per each of 7 diagnostic Sx domains |
SCID-II - per each of 9 diagnostic Sx domains |
| Current Symptoms | c-DIS with follow up questions for all endorsed Sxs |
c-DIS with follow up questions for all endorsed Sxs |
c-DIS with follow up questions for all endorsed Sx |
SCID-II follow up questions for all endorsed Sx |
| Psychological Measures | MMPI-D, MMPI-Hy | ASI, Spielberger STAI-S, STAI-T |
MMPI-Pd, CPI Socialization Scale |
In 2007 (Fein et al. 2007), we published our first paper examining lifetime and current psychiatric comorbidity in 35–55 year old long-term abstinent alcoholics (LTAA) compared to age and sex-comparable nonalcoholic controls (NAC). LTAA had an increased prevalence of lifetime psychiatric diagnoses compared to NAC in all three (mood, anxiety and externalizing) psychiatric domains assessed. LTAA also had an increased prevalence of current mood and anxiety diagnoses compared to NAC. Although 25% of LTAA had lifetime diagnoses of externalizing psychopathology, none had a current externalizing disorder diagnosis. Finally, there was no association of duration of abstinence with lifetime or current psychiatric diagnoses, consistent with psychiatric diagnoses having little or no effect on relapse once individuals achieved at least six months abstinence (minimal abstinence duration required for study entry).
These data support the idea that lifetime psychiatric comorbidity does not militate against achieving long-term abstinence. In fact, psychiatric comorbidity was the norm, with over 85% of the LTAA sample having a lifetime psychiatric diagnosis, comparable to the rates in the epidemiologic studies cited above. Our study demonstrates that long-term abstinence can be attained in a sample of alcohol-dependent individuals (without comorbid drug use disorders), most of whom have a lifetime psychiatric diagnosis. Our data show that individuals with comorbid current mood or anxiety disorders (fully 26% of the LTAA sample) can maintain abstinence in the context of their current mood or anxiety disorder. This is in agreement with other studies supporting the finding that sobriety can be achieved and maintained in the face of a current diagnosis (Chi et al. 2006; Bischof et al. 2005). Mann and colleagues (Mann et al. 2004) found one-year relapse rate comparable or lower in individuals with vs. without a comorbid diagnosis. Comparable results were also found by Davidson and Blackburn (Davidson and Blackburn 1998) and Charney et al. (Charney et al. 1998). Regarding our findings of increased lifetime, but not current ASPD diagnoses, we found that LTAA compared to NAC had very much higher MMPI psychopathic deviance scale scores and lower Socialization scores on the California Psychological Inventory (Fein 2006a); i.e., they showed a much higher propensity toward social deviance than NAC, even though they did not meet criteria for a current diagnosis of ASPD. This suggested that further studies investigating the processes that result in the decrease of overt disinhibitory behavior in LTAA (in the face of their continuing psychological tendency toward social deviance) are critical to understanding how individuals are successful in achieving long-term abstinence.
Psychiatric Comorbidity in Older Abstinent Alcoholics
In 2008 (Fein et al. 2008), we examined psychiatric comorbidity in 89 older (60–85 year old) LTAA (LTAA-O) averaging 14.8 years abstinence compared to 53 age and sex comparable older normal controls (NAC-O). Middle-aged long-term abstinent alcoholics (LTAA-M) compared with middle-aged normal controls (NAC-M) (both from our earlier study cited above) versus LTAA-O compared with NAC-O were similar in the following ways: 1) both comparisons showed more lifetime psychiatric diagnoses in LTAA than NAC, 2) both comparisons showed higher lifetime symptom counts in the anxiety, mood, and externalizing domains in LTAA than NAC, 3) both LTAA groups showed evidence of psychological abnormality in all three domains, and 4) both middle-aged and older comparisons showed larger differences between LTAA and NAC in the externalizing versus the mood and anxiety domains.
Overall, the LTAA-O were less different from NAC-O than were LTAA-M from NAC-M in psychiatric diagnosis rates, symptom counts and psychological measures. The interpretation of this smaller difference between abstinent alcoholics and controls in the LTAA-O versus LTAA-M studies is not obvious. There is the possibility that psychiatric disorder makes maintaining abstinence difficult as one ages, so that the rate of relapse in psychiatrically impaired alcoholics increases with age, resulting in a smaller percentage of comorbid individuals being present in LTAA-O vs. LTAA-M. That interpretation would be consistent with our findings.
There are other factors that may have contributed to the lower prevalence and severity of psychiatric disorder in LTAA-O compared with LTAA-M. First, selective survivorship may be a factor. Although selection bias is almost unavoidable in clinical studies of samples of any age, it may be more of an issue in older samples. Heavy alcohol consumption has been shown to negatively affect life expectancy both directly and indirectly (Ojesjo et al. 1998; Jarque-Lopez et al. 2001; Regier et al. 1990; Goldacre et al. 2004; Sher 2005; Wojtyniak et al. 2005; Rehm et al. 2006). It is also possible that the alcoholics who survived into their sixties, seventies, and eighties and volunteer for demanding research studies are also physically healthier than those who do not. This would reduce psychiatric comorbidity in the LTAA-O sample, since psychiatric and physical health are related, especially in older populations (Haug et al. 2004; Braam et al. 2005; Kisely and Simon 2006; Summaries for patients. The effects of limited sleep and alcohol on driving performance in people with untreated sleep apnea 2009; Ng et al. 2006; Copsey Spring et al. 2007). If this type of selection bias is present in the current study, our results underestimate psychiatric comorbidity in LTAA-O, strengthening our finding of psychiatric disorder in LTAA-O compared with NAC-O.
Sub-Diagnostic Psychiatric Comorbidity in Alcoholics
In 2007, we also revisited our study of LTAA-M vs. NAC-M where we had acquired data on the symptom counts that went into making the psychiatric diagnoses and also on measures of the psychological abnormalities underlying the psychiatric disturbances. We revisited that data set, examining psychiatric symptom counts and psychological measures both in individuals who did and in individuals who did not meet criteria for comorbid psychiatric disorders. We examined the question of whether there are differences between LTAA-M and NAC-M in subthreshold psychiatric illness, and on whether removing individuals with comorbid psychiatric diagnoses (i.e., removing those with supra-diagnostic threshold symptom counts and keeping only those with subthreshold symptom) removes (i.e., controls for) differences in psychiatric morbidity between LTAA and NAC. We found that the bulk of the difference in psychiatric symptoms between LTAA and NAC is sub-diagnostic. Excluding individuals with a psychiatric diagnosis did not control for the differences in psychiatric symptoms and psychological measures between LTAA and NAC groups in any of the psychiatric illness domains. Finally, differences in the presence and severity of psychiatric illness between LTAA and NAC as indicated by lifetime symptom counts and current psychological measures were more than twice as large for antisocial personality disorder (ASPD) domain as it was for mood or anxiety domains.
Psychiatric Comorbidity in Treatment-naive Active Alcoholics
Most alcoholism research is performed on convenience samples of alcoholics in treatment, or shortly after treatment. Improper generalization from select samples to an entire population is called ‘Berkson’s fallacy’; an example would be generalization from the 25% of alcoholics who have received treatment (B. Dawson et al. 2005; D. A. Dawson et al. 2005) to the 75% of alcoholics who have not. (See (Fein and Landman 2005) for a history of Berkson's fallacy and examples in biomedical and psychiatric research.) In addition to alcoholism severity, findings on any measures of the antecedents or consequences of alcohol dependence that may be associated with levels of alcohol use (e.g., preexisting comorbid psychopathologic characteristics or exacerbation with continued alcohol abuse of comorbid psychopathologic characteristics) also may not extend from treated samples of alcoholics to untreated alcoholics in the general population. Given that psychiatric problems are so often a major concomitant of alcohol dependence, and that untreated alcoholics are so rarely examined in alcoholism research, we examined psychiatric diagnoses and both psychiatric symptoms and psychological measures of comorbid psychiatric problems in 86 (49 men and 37 women) treatment naïve actively drinking alcoholics (TNA) 20–50 years of age, averaging 31 years of age, compared to age and sex comparable non alcoholic controls (NAC).
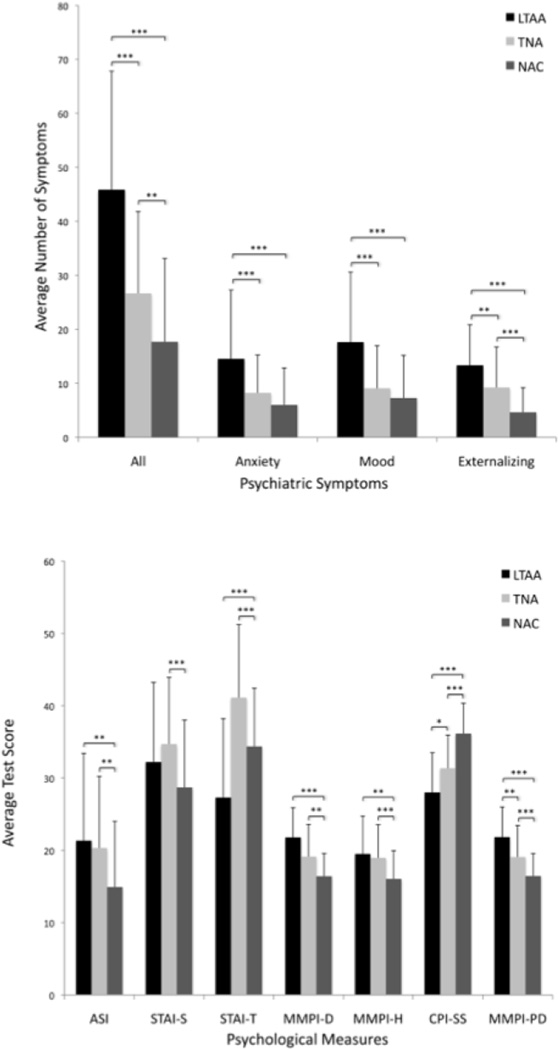
TNA compared to NAC did not differ in the lifetime or current prevalence of psychiatric disorders (p’s > 0.12). Compared to middle-aged LTAA, TNA had fewer lifetime psychiatric, mood, and anxiety, but not externalizing diagnoses. They had a trend toward fewer current psychiatric diagnoses, and exhibited fewer current anxiety diagnoses. The core finding was that TNA do not evidence more psychiatric diagnoses than NAC, but did show substantial psychological differences from NAC in the anxiety, mood, and externalizing domains. TNA showed evidence of more anxiety and mood disturbance (both depressive and hypomanic) and of deviance proneness on all psychological measures compared to NAC. The results for symptom counts were intermediate between the lack of findings on diagnosis rates and the strong findings on psychological tests. Compared to NAC, TNA had 50% more psychiatric symptoms, with more anxiety symptoms being present primarily in TNA men, with a trend for mood symptoms to also be greater, primarily in TNA men. There was also 82% more externalizing symptoms in TNA vs NAC, with no group by sex interaction. Symptom counts were dramatically lower in TNA compared to middle-aged LTAA for total psychiatric symptoms (42% lower), mood (50% lower), anxiety (43% lower), and externalizing symptoms (30% lower). In sum, with regard to psychiatric disorder in the anxiety, mood, and externalizing domains, we see psychological differences between TNA and NAC, smaller differences in psychiatric symptom counts, and no differences in actual psychiatric diagnosis rates. The observed psychological abnormality is attenuated with regard to manifestation in behavior (symptoms), seldom resulting in behavior that meets criteria for a psychiatric diagnosis. Figure 1 presents the symptom count and psychological measure data for the middle-aged LTAA sample, the TNA sample, and the combined control sample for the two studies (values for controls did not differ across the two studies), illustrating the various findings presented above.
Fig. 1.
Bar charts showing the psychiatric symptom counts (top) and psychological measures (bottom) for NAC (non-alcoholic controls), TNA (treatment naïve alcoholics), and LTAA (long-term abstinent alcoholics). Group differences are shown by: *p ≤ 0.05, **p ≤ 0.01, ***p ≤ 0.005 (Di Sclafani et al. 2008)
Studies in Honolulu, Hawaii
In 2005, we moved the laboratory to Honolulu, Hawaii, and embarked on our next set of clinical studies. We expanded our assessment of comorbidity by modifying the c-DIS to assess currency for all endorsed symptoms, and to include an assessment of Borderline Personality Disorder using the SCID-II (Gibbon et al. 1997) (modified to include an assessment of currency of all symptoms). We also added the Eysenck Impulsivity Scale (Eysenck and Eysenck 1975) to our assessment of psychological measures associated with antisocial behavior. For studies of abstinent alcoholics, we expanded our assessments to study both short-term (6–15 week) and long-term (changed to require 18 months minimum abstinence) abstinent alcoholics (STAA and LTAA). For all studies, we modified the age range to be slightly larger than that of the middle-aged abstinent alcoholic study (35–60 years of age), and included individuals with and without a lifetime comorbid drug use disorder.
Borderline Personality Symptoms in Short-Term and Long-Term Abstinent Alcoholics
Borderline personality disorder (BPD), a serious mental illness characterized by pervasive instability and impulsivity in interpersonal relationships, self-image, and behavior (First and Tasman 2004) is prevalent in men and women at nearly equal ratios (5.6% in men, 6.2% in women (Grant et al. 2008). Although earlier views held that BPD was on the “borderline” of psychosis (Barnow et al. 2010) the more current view is that when psychotic features are present, they may be due to the high comorbidity of BPD and Axis I psychotic disorders (Grootens et al. 2008; Zanarini et al. 1990; Zanarini et al. 1998b; Zanarini et al. 2004; Zanarini et al. 1998a). The comorbidity of BPD and SUDs (including AUDs) is very high (Barnow et al. 2010; Trull et al. 2000; Johnson et al. 2003). In a meta-analysis of 26 studies, Trull et al. (Trull et al. 2000) found that 27.4% of SUD and 14.3% of AUD patients met BPD diagnostic criteria. In Wave 2 of the NESARC, Grant et al. (Grant et al. 2008) found a lifetime BPD diagnosis is associated with a lifetime prevalence rate of 50.7% for SUDs (including AUDs). It has been suggested that much of the comorbidity can be attributed to the similar personality traits that characterize both disorders, and may also be associated with shared risk factors (e.g., past trauma (Brown and Anderson 1991; Sabo 1997) and serotonergic depletion; (Trull et al. 2000). These findings suggest a negative synergy between BPD and SUDs, affecting an individual’s ability to achieve remission of either disorder in the presence of the other.
We examined BPD symptoms in 262 individuals, 35 – 60 years of age (Fein and Nip 2012). Five subject groups (each composed of both men and women) were studied: LTAA with lifetime dependence on alcohol only (LTAA ALC) and with lifetime dependence on alcohol + drugs (LTAA ALC+DRG); comparably defined STAA groups (STAA ALC and STAA ALC+DRG); and non-substance-abusing controls (NAC). BPD symptoms were obtained using the SCID-II. For each endorsed symptom, we asked whether the symptom was current.
Tables 1 presents lifetime and current endorsed BPD symptoms for each of the BPD diagnostic criteria, scaled by the number of questions in the SCID-II for each of the criteria (so that criteria have equivalent scales). Alcoholics (STAA and LTAA) had more lifetime symptoms than NAC for all BPD criteria, with effect sizes varying from an odds ratio of 1.6 for anger symptoms to 3.1 for unstable identity. For current symptoms, alcoholics had more symptoms than NAC for all criteria, except anger-related symptoms, with slightly smaller effect sizes than for lifetime symptoms. For both lifetime and current symptoms, there were no effects of a comorbid drug use disorder. LTAA exhibited less lifetime transient, stress-related paranoid ideation and/or dissociative symptoms than STAA and more current feelings of emptiness, for all other criteria STAA and LTAA did not differ. There was also a significant group-by-sex interaction for both lifetime and current symptoms of intense, inappropriate, and/or difficult-to-control anger, and for lifetime frantic efforts to avoid real or imagined abandonment. For both criteria, there were higher symptom counts for STAA women vs. men, with no such effect in LTAA.
Since all of our subjects achieved at least six weeks abstinence prior to study entrance, our results do not speak to the effects of BPD symptoms on treatment seeking or initial success in stopping drinking. The group-by-sex effects are consistent with women in early abstinence who exhibit the BPD-related symptoms of intense, inappropriate, or difficult-to control anger and frantic efforts to avoid real or imagined abandonment being at increased risk for relapse. Longitudinal study of this possible greater risk for relapse is warranted. We do show that BPD symptoms do not prevent the maintenance of abstinence in those who have established at least six weeks abstinence. We find only minor differences in current BPD symptom counts between STAA and LTAA, consistent with alcoholics current BPD symptoms not interfering with the progressing from short-term to long-term abstinence (with exceptions noted above regarding specific symptom categories in women).
Antisocial Diagnoses and Symptoms in Short-Term and Long-Term Abstinent Alcoholics
In our earlier study (Fein et al. 2007), we found that LTAA showed an elevated propensity toward social deviance (higher MMPI Psychopathic Deviance scores and lower CPI Socialization Scores than controls), in the absence of a current ASPD diagnosis. Decreasing disinhibitory behavior in the face of a continuing psychological tendency toward social deviance may be critical in achieving long-term abstinence. To meet diagnostic criteria for ASPD, a childhood and adult components are required (Conduct Disorder with onset before age of 15 years is necessary). Cottler et al. (DeMallie et al. 1995) found that a full ASPD diagnosis ignored 33% of men and 42% of women with an Adult Antisocial Behavior Only (AABO) subtype in a study of 405 drug users. Similarly, Brooner et al. found 24% of opioid injectors had AABO (Brooner et al. 1992). In this study, we focused on ASPD (and AABO) diagnoses and symptoms in the long-term and short-term abstinent and non-substance abusing samples, examining both diagnoses and symptom counts for each of the 7 ASPD criteria.
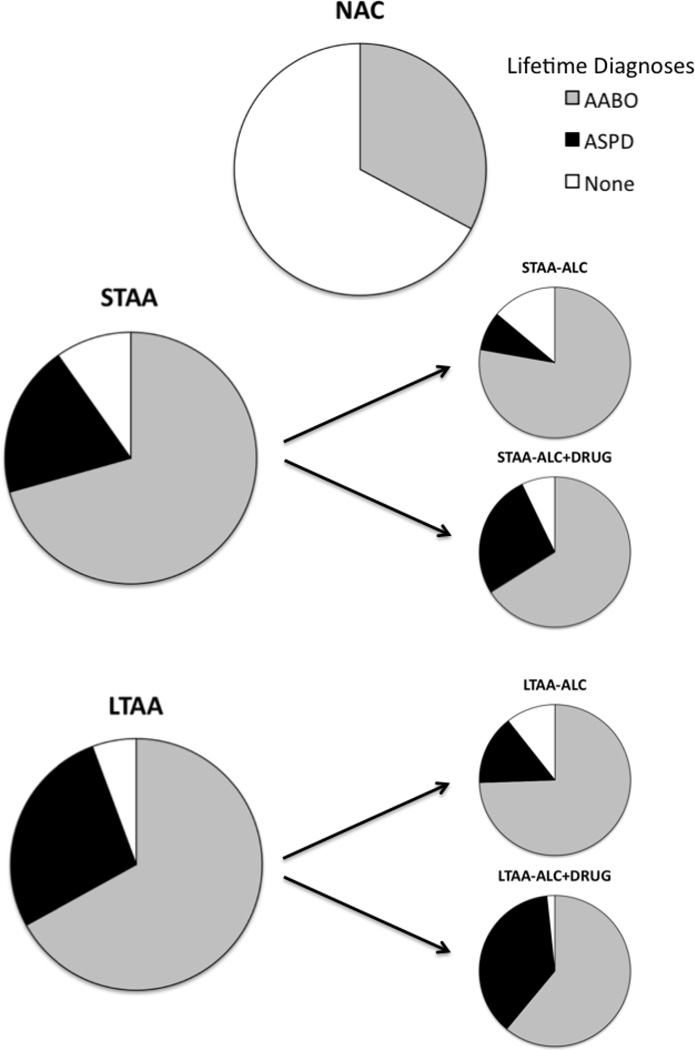
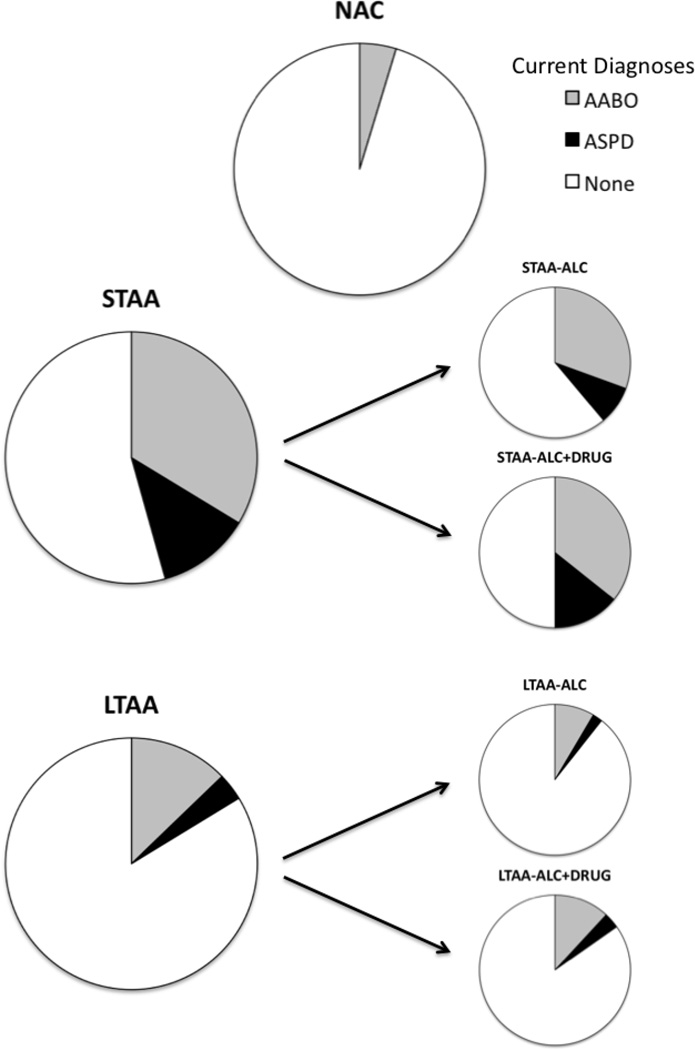
Figure 2 and 3 presents lifetime and current ASPD and AABO diagnoses for all groups. The odds of a control not having a lifetime antisocial diagnosis were 25 times that an abstinent alcoholic. Current antisocial diagnoses had much lower prevalence than lifetime diagnoses. No controls had a current ASPD diagnosis and just under 5% had a current AABO diagnosis, while for abstinent alcoholics, just over 7% had a current ASPD diagnosis and just over 21% had a current AABO diagnosis. The odds of a current ASPD or AABO diagnosis were 8 times greater in abstinent alcoholics vs. controls. While the odds of a lifetime antisocial diagnosis were no different in STAA versus LTAA (p = 0.27, chi-square test), the odds of a current antisocial diagnosis in LTAA were less than one fifth that in STAA.
Fig. 2.
Proportion of lifetime diagnoses of AABO and ASPD for NAC, STAA, and LTAA. STAA and LTAA are then further broken down into pure alcohol users (STAA-ALC and STAA-ALC+DRUG) and polysubstance users (STAA-ALC+DRUG and LTAA-ALC+DRUG) (Fein and Fein 2013)
Fig. 3.
Proportion of current diagnoses of AABO and ASPD for NAC, STAA, and LTAA. STAA and LTAA are then further broken down into pure alcohol users (STAA-ALC and STAA-ALC+DRUG) and polysubstance users (STAA-ALC+DRUG and LTAA-ALC+DRUG) (Fein and Fein 2013)
Table 2 presents lifetime and current antisocial symptom counts. Lifetime symptoms were over 4 times as great for abstinent alcoholics vs. controls, with no difference between STAA and LTAA, nor between sexes, but with about 60% higher lifetime symptom counts for ALC+DRG versus ALC. LTAA and STAA show more lifetime antisocial symptoms for all of the seven ASPD symptom domains, with group accounting for over 15% of the symptom count variance for five of the seven domains, and accounting for over 38% of the variance for total antisocial symptoms. The results are different for current antisocial symptoms. The number of current antisocial symptoms was 5 times as large for STAA vs. controls, with current symptoms in LTAA being 60% lower than in STAA, and just twice that of controls, and with symptom counts being about 50% higher in ALC+DRG versus ALC. When LTAA ALC are compared with controls, there are no significant differences. Analyses of current symptom counts after including age as a covariate to control for LTAA being older than STAA, showed an age effect, but a much larger effect of group, showing that LTAA’s lower current symptom count relative to STAA was not a consequence of the age difference between the groups. Table 4 also breaks down ASPD symptoms (both lifetime and current) for each of the 7 ASPD criteria. The number of lifetime symptoms for all 7 criteria was greater in STAA/LTAA versus controls, with effect sizes varying from 2.9% for lack of remorse to 27.0% for irresponsibility with work or finances. There was no difference for lifetime symptoms for any criteria between STAA and LTAA; and ALC+DRG had more lifetime symptoms than ALC for all criteria except lack of remorse, with effect sizes varying between 4.8% for lack of remorse to 74.3% for reckless disregard for the safety of self and others. STAA had higher current symptom counts than LTAA for all criteria except lack of remorse. Current symptom counts in STAA were significantly higher than those of controls for all criteria, (effect sizes varied from 4.0 to 21.6%), while for LTAA, current symptom counts were higher than those of controls only for financial irresponsibility, effect size = 8.8%, and lack of remorse, effect size = 2.8%, with all other effect sizes being less than 1.3%. For LTAA ALC, current symptom counts were higher than those of controls only for financial irresponsibility (es = 6.2%). For LTAA ALC+DRG, current symptom counts were higher than those of controls for financial irresponsibility (es = 14.8%), lack of remorse (es = 4.1%), and failure to conform to social norms with respect to lawful behavior (es = 3.4%).
Table 2.
Borderline Personality Disorder Symptoms by Diagnostic Criteria
| STAA | LTAA | NAC | Effect Size (Wilcoxon Mann-Whitney Odds Ratios) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ALC (n=36) |
ALC+DRG (n=56) |
ALC (n=47) |
ALC+DRG (n=59) |
(n=64) | STAA & LTAA vs. NAC |
STAA vs. LTAA |
ALC+D RG vs. ALC |
Women vs. Men |
||||||
| Men (n=25) |
Women (n=11) |
Men (n=34) |
Women (n=22) |
Men (n=27) |
Women (n=20) |
Men (n=29) |
Women (n=30) |
Men (n=30) |
Women (n=34) |
|||||
|
Lifetime Symptoms |
||||||||||||||
| Frantic avoidance of abandonment |
.60±.50 | .73±.47 | .56±.50 | .86±.35 | .74±.45 | .60±.50 | .79±.41 | .73±.45 | .23±.43 | .32±.48 | 2.4*** | 0.9 | 1.1 | 1.1 |
| Intense, unstable interpersonal relationships |
.52±.51 | .46±.53 | .41±.50 | .64±.49 | .52±.51 | .50±.51 | .55±.51 | .57±.50 | .20±.41 | .29±.46 | 1.7*** | 0.9 | 1.1 | 1.1 |
| Markedly unstable identity or self-image |
.45±.28 | .23±.33 | .33±.35 | .44±.39 | .39±.34 | .51±.39 | .36±.30 | .43±.40 | .08±.21 | .12±.25 | 3.1*** | 0.9 | 0.9 | 1 |
| Detrimental impulsivity in at least two areas |
.64±.49 | .55±.52 | .65±.49 | .82±.40 | .67±.48 | .65±.49 | .62±.49 | .83±.38 | .37±.49 | .32±.48 | 2.0*** | 1 | 1.2 | 1.1 |
| Suicidal or self-harming behavior |
.28±.41 | .32±.41 | .12±.22 | .59±.45 | .19±.34 | .33±.41 | .16±.24 | .53±.39 | .10±.28 | .10±.27 | 1.8*** | 1 | 1.2 | 1.7*** |
| Marked mood reactivity & emotional instability |
.24±.44 | .27±.47 | .32±.48 | .46±.51 | .41±.50 | .55±.51 | .35±.48 | .50±.51 | .07±.25 | .27±.45 | 1.6*** | 0.8 | 1.1 | 1.3* |
| Feelings of emptiness |
.64±.49 | .46±.47 | .47±.51 | .46±.51 | .48±.51 | .40±.50 | .46±.50 | .40±.50 | .07±.25 | .12±.33 | 2.2*** | 1 | 1.1 | 1.1 |
| Intense, inappropriate, or uncontrollable anger |
.09±.26 | .33±.3 | .19±.32 | .52±.41 | .31±.40 | .27±.38 | .38±.41 | .36±.42 | .89±.19 | .15±.29 | 1.6*** | 0.8 | 1.4* | 1.3* |
| Transient paranoia or dissociative symptoms |
.32±.48 | .09±.30 | .24±.43 | .36±.49 | .33±.48 | .65±.49 | .35±.48 | .37±.49 | .07±.25 | .59±.24 | 1.8*** | 0.7* | 0.9 | 1.1 |
|
Current Symptoms (past 12 months) |
||||||||||||||
| Frantic avoidance of abandonment |
.20±.41 | .27±.47 | .17±.38 | .64±.49 | .22±.42 | .40±.50 | .35±.48 | .40±.50 | .03±.18 | .03±.17 | 1.8*** | 0.9 | 1.2 | 1.3** |
| Intense, unstable interpersonal relationships |
.24±.44 | .27±.47 | .24±.43 | .64±.49 | .37±.49 | .35±.49 | .35±.48 | .43±.50 | .10±.31 | .18±.39 | 1.6*** | 0.9 | 1.2 | 1.3* |
| Markedly unstable identity or self-image |
.34±.30 | .18±.32 | .25±.30 | .42±.37 | .27±.33 | .33±.37 | .22±.27 | .28±.32 | .06±.20 | .08±.20 | 3.1*** | 0.9 | 0.9 | 1 |
| Detrimental impulsivity in at least two areas |
.52±.48 | .27±.47 | .50±.51 | .68±.48 | .59±.50 | .40±.50 | .41±.50 | .60±.50 | .17±.38 | .18±.39 | 2.0*** | 1 | 1.1 | 1 |
| Suicidal or self-harming behavior |
.10±.25 | .00±.00 | .03±.12 | .41±.45 | .06±.19 | .27±.42 | .07±.23 | .13±.32 | .03±.18 | .00±.00 | 1.3*** | 1.2 | 1.1 | 1.1 |
| Marked mood |
.20±. | .27±.4 | .24±. | .41±.5 | .22±. | .45±.5 | .28±. | .40±.5 | .07±.25 | .21±.41 | 1.4* | 0.9 | 1.1 | 1.3** |
| reactivity & emotional instability |
41 | 7 | 43 | 0 | 42 | 1 | 46 | 0 | ** | |||||
| Feelings of emptiness |
.64±.49 | .27±.48 | .41±.50 | .41±.50 | .30±.47 | .20±.41 | .26±.44 | .30±.47 | .03±.18 | .09±.29 | 1.8*** | 1.5** | 1 | 0.8 |
| Intense, inappropriate, or uncontrollable anger |
.04±.15 | .21±.31 | .09±.24 | .38±.40 | .17±.30 | .07±.23 | .23±.32 | .17±.29 | .08±.19 | .10±.24 | 1.3 | 1 | 1.3* | 1.2 |
| Transient paranoia or dissociative symptoms |
.32±.48 | .09±.30 | .19±.33 | .32±.48 | .20±.41 | .24±.44 | .21±.41 | .30±.47 | .07±.25 | .03±.17 | 1.5*** | 0.9 | 0.9 | 1.1 |
Effect is significant:
p ≤0.05,
p ≤0.01,
p ≤0.001
This data is taken from (Fein and Nip, 2012).
Table 4.
Internalizing Symptom Counts
| Lifetime Mood Diagnosis |
STAA | LTAA | NAC | Effect Size (Partial η2) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ALC | ALC+DRG | ALC | ALC+DRG | |||||||||||
| N=24 | N=28 | N=25 | N=32 | N=18 | ||||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | (STAA & LTAA) vs NAC |
STA A vs LTAA |
ALC vs ALC+DRG |
Wome n vs Men |
|
| Lifetime Symptom Count |
26.38 | 8.70 | 28.79 | 13.12 | 27.68 | 14.42 | 24.84 | 11.05 | 23.17 | 11.02 | 1.2 | 0.4 | 0.0 | 0.5 |
| Current Symptom Count |
4.53 | 2.65 | 4.89 | 3.90 | 5.92 | 4.42 | 3.75 | 1.88 | 5.00 | 2.16 | 0.0 | 0.0 | 1.2 | 0.1 |
|
Lifetime Anxiety Diagnosis |
STAA | LTAA | NAC | Effect Size (Partial η2) | ||||||||||
| ALC | ALC+DRG | ALC | ALC+DRG | |||||||||||
| N=10 | N=16 | N=15 | N=22 | N=7 | ||||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD |
(STAA& LTAA) vs NAC |
STA A vs LTAA |
ALC vs ALC+DRG |
Wome n vs Men |
|
| Lifetime Symptom Count |
24.10 | 9.13 | 30.75 | 13.62 | 27.60 | 13.51 | 25.91 | 14.08 | 24.71 | 17.91 | 0.3 | 0.4 | 0.4 | 0.0 |
| Current Symptom Count |
11.83 | 8.40 | 17.63 | 13.53 | 16.67 | 11.93 | 19.63 | 11.10 | 5.00 | 5.66 | 6.9 | 2.1 | 3.8 | 0.5 |
|
Sub Diagnosti c Mood Disorder |
STAA | LTAA | NAC | Effect Size (Partial η2) | ||||||||||
| ALC | ALC+DRG | ALC | ALC+DRG | |||||||||||
| N=15 | N=34 | N=23 | N=30 | N=64 | ||||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD |
(STAA & LTAA) vs.NAC |
STA A vs LTAA |
ALC vs ALC+DRG |
Wome n vs Men |
|
| Lifetime Symptom Count |
3.27 | 3.60 | 2.65 | 4.25 | 6.83 | 12.41 | 4.13 | 6.00 | 1.34 | 2.90 | 4.8** | 2.8 | 1.9 | 0.3 |
| Current Symptom Count |
1.95 | 2.70 | 1.16 | 2.42 | 1.33 | 2.75 | 0.78 | 1.25 | 0.13 | 0.42 | 3.4** | 0.8 | 1.7 | 0.0 |
|
Sub Diagnosti c Anxiety Disorder |
STAA | LTAA | NAC | Effect Size (Partial η2) | ||||||||||
| ALC | ALC+DRG | ALC | ALC+DRG | |||||||||||
| N=29 | N=46 | N=33 | N=40 | N=75 | ||||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD |
(STAA & LTAA) vs.NAC |
STA A vs LTAA |
ALC vs ALC+DRG |
Wome n vs Men |
|
| Lifetime Symptom Count |
9.90 | 10.14 | 8.74 | 9.24 | 7.82 | 9.41 | 8.03 | 6.84 | 3.60 | 5.87 | 8.1*** | 0.5 | 0.0 | 1.4 |
| Current Symptom Count |
6.67 | 7.97 | 6.61 | 8.53 | 5.33 | 8.52 | 3.17 | 5.02 | 1.41 | 3.81 | 5.1*** | 2.7* | 0.4 | 0.5 |
This study replicates and extends the results from our California studies. Only 10% of abstinent alcoholics did not have a lifetime antisocial diagnosis, providing additional evidence for the strong association between antisocial personality problems and AUDs / SUDs. Our data illustrate the importance of AABO when examining antisocial problems in DUDs, with lifetime AABO having much higher lifetime and current prevalence than ASPD in all groups and carry a majority of the increased prevalence of antisocial diagnoses in the abstinent alcoholics.
Our results support the idea from our earlier paper that disinhibitory and socially deviant behavior reflected in an antisocial diagnosis must decrease to maintain long-term abstinence. We now show that current ASPD symptom counts in LTAA are much closer to controls than in STAA. Antisocial symptoms in LTAA ALC were comparable with those in controls, with such symptoms about 50% higher in ALC+DRG, giving evidence of greater antisocial pathology in ALC+DRG versus ALC. However, even in LTAA ALC +DRG, current symptom counts were much lower than in STAA ALC+DRG and closer to those of controls than to STAA ALC+DRG. One might argue that antisocial behavior may be a result of alcohol and drug use wherein stopping the use results in a reduction in the antisocial behavior. This might intuitively make sense for the symptom domain of work / financial irresponsibility, but it is unclear how stopping drinking could account for the reduction in the other symptom domains (social norms conformity, deceitfulness, impulsivity, irritability / aggressiveness, disregard for safety, and lack of remorse).
Social deviance proneness, or antisocial dispositionality, was comparably abnormal in both STAA and LTAA, and current measures were very close to lifetime levels. The close to normal level of current antisocial behaviors in long-term abstinence therefore takes place in the context of elevated social deviance proneness and antisocial dispositionality. This suggests a top-down model whereby one invokes executive control to inhibit deviance-prone tendencies. A crucial question is whether this increased inhibitory control is specific to reducing substance use or manifests in a general increase in inhibitory control of behavior. We recently (Camchong et al. 2013) examined fMRI resting-state synchrony (RSS) in LTAA ALC. We found a compensatory mechanism in long-term abstinence, evident during rest, in which decision-making networks showed reduced synchrony with appetitive drive regions and increased synchrony with inhibitory control regions (in comparison to controls), with the greater synchrony with inhibitory control regions being associated with generalized better cognitive flexibility. These findings suggest a general adaptive mechanism in long-term abstinence that may facilitate the behavioral control required to maintain abstinence. The data are consistent either with recovery of function in executive control and a reduction in appetitive drive or with individuals with greater executive control and lesser appetitive drive being better able to sustain recovery, alternatives that are testable in longitudinal studies.
Mood and Anxiety Disorders in Short-Term and Long-Term Abstinent Alcoholics
In Honolulu, we replicated and expanded on our 2007 study with respect to mood and anxiety disturbance in abstinent alcoholics by not only including LTAA and NAC samples about twice the size of the earlier study, but also including short-term abstinent alcoholics (STAA, 6–15 week abstinent) to assess whether comorbid mood and/or anxiety diagnoses impact achieving very long-term abstinence (i.e., differ between STAA and LTAA). Moreover, both alcoholic groups included subsamples with comorbid illicit drug dependence.
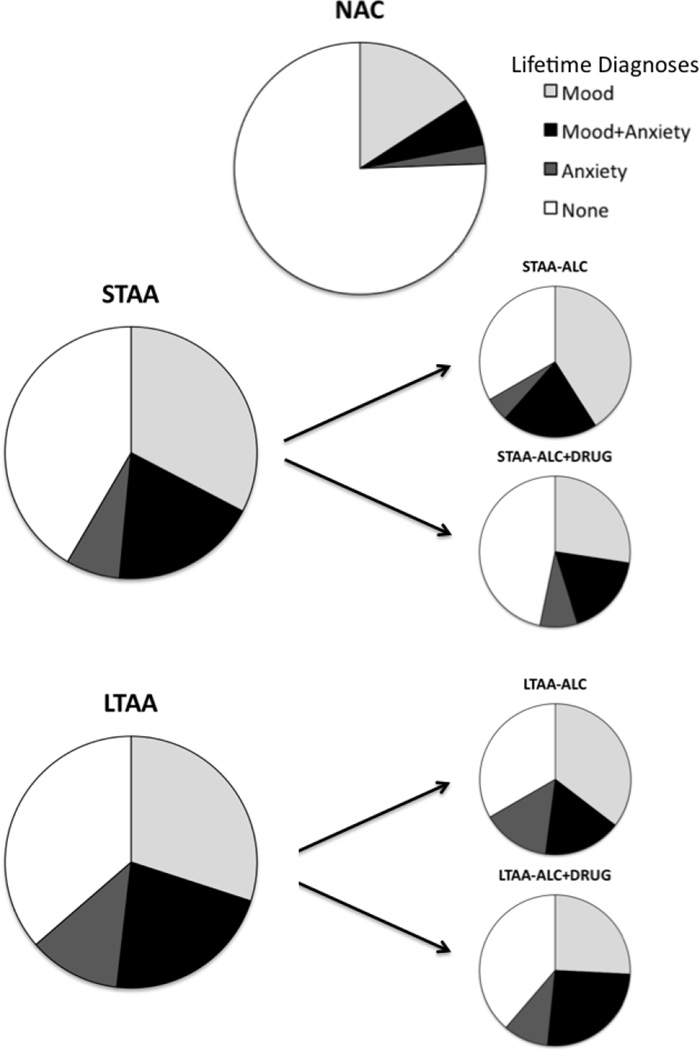
Figure 4 presents the proportions of lifetime internalizing diagnoses for NAC, STAA and LTAA groups. Both STAA and LTAA have higher diagnosis rates for Mood, Anxiety and comorbid Mood and Anxiety disorders than NAC, but do not differ from each other. Compared to a 22 percent prevalence in controls, more than half of STAA and LTAA had a lifetime mood disorder diagnosis, with no difference between STAA and LTAA, and no group by sex interactions. In each group, about ¾ of subjects with a lifetime mood diagnosis had a Major Depressive Disorder (MDD) diagnosis, with comparisons among groups for MDD mirroring comparisons for mood disorders. For mania and bipolar disorder, prevalence was much lower (below 13%), resulting in lower power (although odds ratios were similar to those for MDD, only one of which – mania comparing LTAA and NSAC - was statistically significant). There were no differences between those dependent on alcohol only or on alcohol and drugs on any of the above comparisons. Figure 4 also shows lifetime anxiety disorder diagnoses. Women had twice the prevalence of men. Compared to a 8.5% prevalence in controls 25.7% of STAA and 33.6% of LTAA had a lifetime anxiety disorder, with no difference in rates between LTAA and STAA (p = .211). The comparisons among groups in anxiety diagnoses did not differ between men and women. In each group, over 80% of subjects with a lifetime anxiety diagnosis had a Post-Traumatic Stress Disorder (PTSD) diagnosis, with PTSD results mirroring those for anxiety disorders. For agoraphobia and panic disorder, prevalence was much lower, resulting in lower power for group comparisons (only one of which – agoraphobia comparing LTAA and NAC – was statistically significant, with odds ratios similar to those for PTSD). Within the combined LTAA and STAA groups, the presence of comorbid drug dependence did not affect the rates of anxiety diagnoses.
Fig. 4.
Proportion of lifetime mood and anxiety diagnoses NAC, STAA, and LTAA. STAA and LTAA are then further broken down into pure alcohol users (STAA-ALC and STAA-ALC+DRUG) and polysubstance users (STAA-ALC+DRUG and LTAA-ALC+DRUG) (Fein 2013)
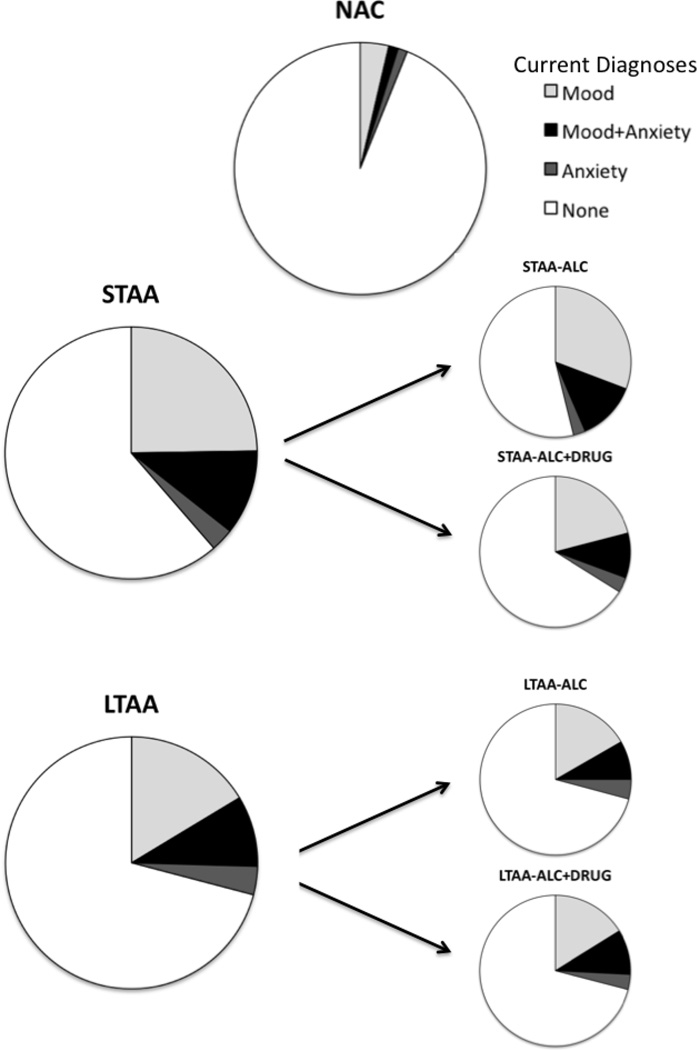
Figure 5 presents the proportions of current internalizing disorder diagnoses for NAC, STAA and LTAA groups. Both STAA and LTAA have more current Mood, Anxiety and comorbid Mood and Anxiety diagnoses than NAC. STAA and LTAA have similar proportions of Anxiety and comorbid Mood and Anxiety diagnoses, while LTAA has a lower proportion than STAA for mood disorders.
Fig. 5.
Proportion of current mood and anxiety diagnoses NAC, STAA, and LTAA. STAA and LTAA are then further broken down into pure alcohol users (STAA-ALC and STAA-ALC+DRUG) and polysubstance users (STAA-ALC+DRUG and LTAA-ALC+DRUG) (Fein 2013)
Women showed a trend toward more current mood disorders (28.4%) than men (18.9%) (p =.055). Compared to a 4.9% rate of current mood diagnoses in controls, more than 1/3 of STAA and 1/4 of LTAA had a current mood disorder. In each group, about 2/3 of those with a current mood disorder had a Major Depressive Disorder (MDD) diagnosis. For current MDD, the prevalence was higher in STAA (26.7%) compared to LTAA (14.5%) (p = .028). Within the combined LTAA and STAA groups, current mood diagnoses did not differ consequent to a comorbid drug disorder. Women had a higher prevalence of current anxiety disorders than men (14.9% vs. 6.3%, p < .015). Compared to a 2.4% prevalence in controls, 13.9% of STAA and 12.7% of LTAA had a current anxiety diagnosis, with no difference between LTAA and STAA, and with group comparisons unaffected by sex or comorbid drug dependence. Over 80% of individuals with a current anxiety diagnosis had PTSD, with comparisons for PTSD mirroring the comparisons for anxiety diagnoses.
Table 3 shows lifetime and current mood disorder symptom counts for individuals with a lifetime mood diagnosis and anxiety disorder symptom counts for individuals with a lifetime anxiety diagnosis. No comparison showed any differences by group or sex nor as a function of comorbid drug dependence. Although there were more individuals with diagnosable mood or anxiety disorders in the alcoholic groups, there was no evidence that abstinent alcoholics with a lifetime mood or anxiety diagnosis had more mood or anxiety symptoms than controls with a similar diagnosis. Table 3 also shows mood and anxiety symptom counts (both lifetime and current) for individuals without a lifetime mood or anxiety diagnosis (i.e., with fewer symptoms than needed to reach lifetime diagnostic thresholds). In these data, alcoholics (STAA and LTAA) had more lifetime and current mood symptoms than NAC, but did not differ from each other, nor were there effects of sex nor of comorbid lifetime drug dependence. A similar pattern was present for anxiety symptoms except that the effect sizes comparing alcoholics to controls were about 50% larger for anxiety symptoms than the effects for mood symptoms.
Table 3.
ASPD Symptom Count per ASPD Diagnosis Criteria and Psychological Measures
| STAA | LTAA | NSAC | Effect Size (Partial eta²) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ALC (n=36) |
ALC + DRG (n=56) |
ALC (n=47) |
ALC + DRG (n=59) |
(n=64) | STAA & LTAA vs NAC |
Men vs Women |
STAA vs LTAA |
ALC+ DRG vs. ALC |
LTAA ALC vs NAC |
|||
| Lifetime Symptomx: | 52.2*** | |||||||||||
| Social Norms Conformity |
72±.94 | 1.8±1.1 | 1.0±1.2 | 2.1±1.3 | .08±.32 | 22.7*** | 0.1 | 1.2 | 1.7*** | 26.3*** | ||
| Deceitfulness | .22±.42 | .30±.46 | .28±.45 | .47±.50 | .00±.00 | 10.5*** | 0.2 | 1.4 | 2.2* | 18.1*** | 32.0*** | |
| Impulsivity | 1.4±1.0 | 1.6±1.6 | .98±1.0 | 1.6±1.1 | .31±.61 | 18.7*** | 0.1 | 0.8 | 3.9* | 16.5*** | 35.4*** | |
| Irritability / Aggressiveness |
.47±.65 | 1.3±1.0 | .83±.89 | 1.5±1.2 | .13±.42 | 17.0*** | 0.2 | 1.5 | 12.1*** | 22.0*** | 37.3*** | |
| Disregard for Safety | 1.3±.79 | 1.6±.75 | 1.2±.81 | 1.6±.89 | .52±.64 | 21.6*** | 1.6* | 0.1 | 3.9** | 19.9*** | 33.8*** | |
| Work / Financial Irresponsibility |
2.5±1.6 | 3.2±1.6 | 2.1±1.5 | 3.1±1.5 | .63±1.0 | 27.0*** | 1.4 | 0.7 | 6.6*** | 25.8*** | 47.5*** | |
| Lack of Remorse | .92±1.2 | 1.1±1.1 | 1.1±1.1 | 1.3±1.1 | .69±.85 | 2.9** | 0.4 | 0.4 | 0.8 | 3.9* | 7.5** | |
| Total Lifetime Sx | 10.6±5.1 | 15.6±6.1 | 10.8±5.5 | 16.6±5.8 | 3.1±3.7 | 38.7*** | 0.5 | 0.3 | 18.1*** | 41.4*** | 66.4*** | |
| Current Symptoms | ||||||||||||
| Social Norms Conformity |
.19±.47 | .57±.87 | .04±.20 | .12±.38 | .02±.13 | 3.3** | 0.1 | 6.8*** | 4.0** | 0.7 | 3.4* | |
| Deceitfulness | .14±.35 | .07±.26 | .00±.00 | .03±.18 | .00±.00 | 1.4 | 0.0 | 3.6** | 0.1 | n/a | 1.8 | |
| Impulsivity | .83±.88 | .61±.89 | .15±.36 | .15±.45 | .13±.38 | 2.8** | 1.1 | 15.0*** | 0.7 | 0.1 | 0.1 | |
| Irritability / Aggressiveness |
.14±.42 | .39±.76 | .06±.32 | .19±.51 | .05±.28 | 2.0* | 0.0 | 1.6 | 2.9* | 0.1 | 2.9 | |
| Disregard for Safety | .25±.44 | .57±.85 | .06±.25 | .19±.54 | .11±.36 | 1.7* | 0.0 | 5.5*** | 3.4** | 0.5 | 0.7 | |
| Work / Financial Irresponsibility |
.94±1.3 | 1.4±1.3 | .45±.78 | .69±.86 | .13±.49 | 9.0*** | 0.2 | 7.0*** | 2.5* | 6.2** | 14.8*** | |
| Lack of Remorse | .39±.80 | .54±.79 | .40±.83 | .42±.68 | .17±.55 | 2.4* | 0.5 | 0.1 | 0.3 | 2.8 | 4.1* | |
| Total Current Sx | 3.5±3.0 | 5.2±5.0 | 1.6±2.3 | 2.1±2.2 | 0.9±1.9 | 7.3*** | 0.5 | 12.2*** | 2.6* | 2.9 | 7.7** | |
| Psychological Measures | ||||||||||||
| CPI Socialization Scale |
18.1±.3.9 | 17.5±.3.8 | 17.5±.3.8 | 16.6±.4.1 | 22.1±.3.2 | 23.0*** | 0.1 | 0.7 | 1.0 | 29.7*** | 36.5*** | |
| Eysenck Impulsivity Scale |
8.3±.4.2 | 8.3±.4.2 | 8.4±.4.4 | 8.8±.5.0 | 4.4±.3.4 | 18.6*** | 0.2 | 0.9 | 1.9 | 21.1*** | 21.7*** | |
| MMPI Psychopathic Deviance Scale |
26.5±.5.9 | 26.9±.5.2 | 23.2±.5.8 | 25.1±.5.6 | 16.8±.4.8 | 31.3*** | 0.6 | 4.8** | 1.0 | 26.9*** | 39.0*** | |
This study shows that a lifetime mood or anxiety diagnosis does not militate against achieving and maintaining abstinence from alcohol or from both alcohol and drugs. This was true across sex, across mood diagnoses (MDD, Bipolar 1, and Manic Disorder) and anxiety diagnoses (PTSD, Agoraphobia, and Panic Disorder) and was unaffected by lifetime dependence on other drugs of abuse. The almost identical prevalence of lifetime mood and anxiety diagnoses in STAA and LTAA strongly supports the contention that such diagnoses do not affect the likelihood of progression from 6–15 weeks abstinence to multi-year abstinence. Although the prevalence of current diagnoses was lower than lifetime diagnoses for all groups (current diagnoses are a subset of lifetime diagnoses), the differences between abstinent alcoholics and controls were larger. This would be consistent with greater recovery from lifetime mood and anxiety diagnoses in the middle-aged control samples than in the alcoholic samples. We also found higher current MDD prevalence in STAA vs. LTAA, consistent with some recovery as abstinence progresses or with STAA with a current MDD diagnosis being less likely to achieve long term abstinence. In this regard, a six year study of abstinent alcoholics found those who relapsed had significantly more lifetime major depressive diagnoses than those who remained abstinent (Landheim et al. 2006). It has also been suggested that having both comorbid anxiety and depressive symptoms leads to relapse (Boschloo 2012). However, as shown in Figures 4 and 5, the prevalence of dual comorbidity of mood and anxiety diagnoses is comparable for STAA and LTAA, suggesting that the effect of having both diagnoses is not much different from the effect of either diagnosis separately.
These results are silent with regard to whether comorbid mood and anxiety disorders have an effect on achieving and maintaining abstinence during the first six weeks of abstinence. Comorbidities may be higher in individuals initiating abstinence than in our STAA and some individuals with comorbidities may be more likely to relapse prior to 6–15 week abstinence. If such an effect exists, it would pertain to a relatively small proportion of individuals initiating abstinence. The examination of mood and anxiety symptom counts in individuals without a mood or anxiety disorder diagnosis shows that excluding individuals with a diagnosis does not eliminate mood and anxiety disorder differences between alcoholics and controls. Finally, these results support the contention that the bulk of the mood and anxiety disorder diagnoses observed in our abstinent substance abusing samples have a life independent of the comorbid substance use disorder. The strongest evidence for this is displayed in Figure 5, which shows that over a quarter of multi-year abstinent substance dependent individuals have a current mood or anxiety disorder. Were such disorders secondary to the substance use, one would have expected that the majority of disorders would have resolved over multiple years of abstinence.
The neuropsychology of psychiatric disorders vs. alcoholism
Depression
A recent review (Snyder 2013) and meta-analysis of 113 studies of depression shows that MDD is reliably associated with impaired performance on neuropsychological measures of executive function, with motor slowing not able to account for the executive function findings. Additionally, evidence suggests that executive function deficits are greater in patients with more severe current depression symptoms and those taking psychotropic medications, with no evidence for a synergistic effect of age. Results suggest that MDD is associated with broad impairment in multiple aspects of executive function.
Anxiety Disorders (Anx) (Zlomuzica et al. 2014)
Central to cognitive theories of Anx is the proposition that the negative beliefs and covert cognitive avoidance behavior in Anx result from patient’s misinterpretation of internal and external stimuli as being highly dangerous. Moreover, avoidance behavior is maintained because anxiety patients tend to selectively retrieve (personally relevant) information from the past that confirms their negative interpretation of current or anticipated situations. One major factor possibly contributing to the maintenance of negative beliefs, maladaptive emotional responses, and avoidance behavior is the dysfunctional retrieval of past experiences from autobiographical and episodic memory. A growing body of neuropsychological investigations has shown that individuals with clinically significant anxiety also exhibit impaired episodic memory for neutral, emotionally irrelevant information, suggesting that healthy storage and retrieval of episodic memory in Anx depends on the emotional valence of the processed information.
Depression and Anxiety (including anxious depression) (Ionescu et al. 2014)
The approach-withdrawal model attempts to correlate the clinical deficits of emotion and motivation seen in anxiety and depression. This model hypothesizes two separate systems for emotion and motivation (Davidson 1992). The approach system (left frontal lobe) controls behavioral motivation towards reward and is hypothesized to be hypoactive in depression, while the withdrawal system (right frontal lobe) controls behavioral inhibition and is hypothesized to be hyperactive in anxiety. This frontal asymmetry may become more apparent in subjects suffering from both depression and anxiety. Alternatively, a tripartite model uses three dimensions as a framework for classifying symptoms of anxiety and depression: negative affectivity, positive affectivity, and physiological hyperarousal (Clark and Watson 1991). Depression is marked by the absence of positive affectivity (i.e., anhedonia), whereas physiological hyperarousal is relatively specific to anxiety. What unifies the two diagnostic states is the high level of negative affectivity.
Borderline Personality Disorder (Schmahl et al. 2014)
Research suggests three core domains of psychopathology in Borderline Personality Disorder: affective dysregulation, interpersonal disturbances, and behavioral dysregulation. Recent work has established deficits in cognitive empathy and emotional empathy in Borderline Personality Disorder. Thus, individuals with Borderline Personality Disorder have deficits in accurately attributing mental states to others (cognitive empathy) and having an appropriate emotional response to another person’s emotional state (emotional empathy) (Preissler et al. 2010; Roepke et al. 2012). These deficits relate to a theory of mind deficit possibly related to insecure and disorganized early attachment (Mosquera et al. 2014).
Antisocial Personality Disorder (Oscar-Berman et al. 2009)
Antisocial Personality Disorder and Alcoholism are of comorbid conditions. Alcoholics as well as nonalcoholics with ASPD (or AABO) exhibit behaviors associated with prefrontal and orbital-frontal brain dysfunction such as increased impulsivity, myopia for the future (Bechara and Damasio 2002), emotional dysregulation, a blunted negative valence attached to negative feedback about behavioral consequences (Fein and Chang 2008) and emotional dysregulation. Oscar-Berman and colleagues (Oscar-Berman et al. 2009) have shown that alcoholism and ASPD have more than additive effects on frontal cortex function.
Summary
At their core, SUDs involve compulsively taking mind-altering substances. Individuals with mood or anxiety disorders (and BPD) are often in an uncomfortable and unpleasant state of mind, and it may not be surprising that they would take substances to change their mental state. This would be true above and beyond any comorbid genetic predisposition to SUDs and psychiatric disorders. The studies presented above show an association of substance use disorders and psychiatric disorders that scales with alcohol disorder severity such that TNA, who have less severe alcoholism than treated abstinent samples also evidence less severe psychiatric disturbance. Individuals with alcohol and drug use disorders show greater antisocial personality disturbance than those without comorbid drug use disorders but do not show differences in mood or anxiety domains or in BPD symptoms. The studies also show that alcoholics can achieve and maintain abstinence in the face of an ongoing mood, anxiety, or BPD disorder. Abstinent individuals without diagnosable lifetime psychiatric disorders still have more psychiatric symptoms and abnormal psychological measures than nonalcoholic in the mood, anxiety, BPD, and antisocial domains. This suggests that individuals with an AUD have problems in living beyond drinking, and that these problems affect their quality of life. The association of SUDs with comorbid antisocial disorders is different. In this case, it appears as though ongoing antisocial behavior is not consistent with maintaining abstinence and must essentially be halted. Individuals must stop current antisocial behaviors in the context of elevated social deviance proneness and antisocial dispositionality.
The results presented above show that lifetime psychiatric comorbidity is the norm for treated alcoholics (present in over ¾ of them). The preponderance of the work reviewed above on abstinent alcoholics examined individuals in mutual help recovery networks such as AA and NA. We were completely unsuccessful in our attempts to recruit LTAA who were not current members of mutual help recovery groups. We are not sure of the reasons for this, but we expect that it had something to do with members of such groups having already self-identified as abstinent alcoholics and addicts. Given this selection bias, we cannot assume that our comorbidity results generalize to abstinent alcoholics who are not current members of such groups. Within the samples studied, we are not sure the degree to which recovery groups are important in helping abstinent alcoholics maintain abstinence in the face of ongoing psychiatric and psychological distress (e.g., see (Bergman et al. 2014)). The work above focused on individuals in and post treatment for alcoholism and other SUDs and shows little change in psychiatric and psychological distress from STAA to LTAA groups. Even though such individuals remain abstinent, their psychological distress may negatively affect their quality of life and suggests the importance of developing effective care models to address comorbid mental health problems.
Research involving human participants.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the studies summarized in this review.
Acknowledgments
Funding: This work was supported by the National Institutes for Health Grants 3R01AA016944-02S1, 5R01AA013659, 5R01AA016944, and 5R01AA11311.
Footnotes
Conflict of Interest: George Fein is President and CEO of Neurobehavioral Research, Inc. There is no conflict of interest in the writing of this review.
References
- Barnow S, Arens EA, Sieswerda S, Dinu-Biringer R, Spitzer C, Lang S. Borderline personality disorder and psychosis: a review. Curr Psychiatry Rep. 2010;12(3):186–195. doi: 10.1007/s11920-010-0107-9. [DOI] [PubMed] [Google Scholar]
- Bechara A, Damasio H. Decision-making and addiction (part I): impaired activation of somatic states in substance dependent individuals when pondering decisions with negative future consequences. Neuropsychologia. 2002;40(10):1675–1689. doi: 10.1016/s0028-3932(02)00015-5. [DOI] [PubMed] [Google Scholar]
- Bergman BG, Greene MC, Hoeppner BB, Slaymaker V, Kelly JF. Psychiatric Comorbidity and 12-Step Participation: A Longitudinal Investigation of Treated Young Adults. Alcoholism: Clinical and Experimental Research. 2014;38(2):501–510. doi: 10.1111/acer.12249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bischof G, Rumpf HJ, Meyer C, Hapke U, John U. Influence of psychiatric comorbidity in alcohol-dependent subjects in a representative population survey on treatment utilization and natural recovery. [Research Support, Non-U.S. Gov't] Addiction. 2005;100(3):405–413. doi: 10.1111/j.1360-0443.2005.01008.x. [DOI] [PubMed] [Google Scholar]
- Braam AW, Prince MJ, Beekman AT, Delespaul P, Dewey ME, Geerlings SW, Kivela SL, Lawlor BA, Magnusson H, Meller I, Peres K, Reischies FM, Roelands M, Schoevers RA, Saz P, Skoog I, Turrina C, Versporten A, Copelan JR. Physical health and depressive symptoms in older Europeans. Results from EURODEP. Br J Psychiatry. 2005;187:35–42. doi: 10.1192/bjp.187.1.35. [DOI] [PubMed] [Google Scholar]
- Brooner RK, Schmidt CW, Felch LJ, Bigelow GE. Antisocial behavior of intravenous drug abusers: implications for diagnosis of antisocial personality disorder. 1992;149(4):482–487. doi: 10.1176/ajp.149.4.482. [DOI] [PubMed] [Google Scholar]
- Brown GR, Anderson B. Psychiatric morbidity in adult inpatients with childhood histories of sexual and physical abuse. 1991;148(1):55–61. doi: 10.1176/ajp.148.1.55. [DOI] [PubMed] [Google Scholar]
- Burns L, Teesson M, O'Neill K. The impact of comorbid anxiety and depression on alcohol treatment outcomes. Addiction. 2005;100(6):787–796. doi: 10.1111/j.1360-0443.2005.001069.x. [DOI] [PubMed] [Google Scholar]
- Camchong J, Stenger A, Fein G. Resting-State Synchrony During Early Alcohol Abstinence Can Predict Subsequent Relapse. Cereb Cortex. 2013;23(9):2086–2099. doi: 10.1093/cercor/bhs190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charney DA, Paraherakis AM, Negrete JC, Gill KJ. The impact of depression on the outcome of addictions treatment. J Subst Abuse Treat. 1998;15(2):123–130. doi: 10.1016/s0740-5472(97)00183-9. [DOI] [PubMed] [Google Scholar]
- Chi FW, Satre DD, Weisner C. Chemical dependency patients with cooccurring psychiatric diagnoses: service patterns and 1-year outcomes. [Research Support, N.I.H., Extramural] Alcoholism Clinical and Experimental Research. 2006;30(5):851–859. doi: 10.1111/j.1530-0277.2006.00100.x. [DOI] [PubMed] [Google Scholar]
- Clark LA, Watson D. Tripartite model of anxiety and depression: psychometric evidence and taxonomic implications. J Abnorm Psychol. 1991;100(3):316–336. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- Copsey Spring TR, Yanni LM, Levenson JL. A shot in the dark: failing to recognize the link between physical and mental illness. J Gen Intern Med. 2007;22(5):677–680. doi: 10.1007/s11606-006-0089-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie SR, Patten SB, Williams JV, Wang J, Beck CA, El-Guebaly N, Maxwell C. Comorbidity of major depression with substance use disorders. Can J Psychiatry. 2005;50(10):660–666. doi: 10.1177/070674370505001013. [DOI] [PubMed] [Google Scholar]
- Davidson KM, Blackburn IM. Co-morbid depression and drinking outcome in those with alcohol dependence. Alcoholism Clinical and Experimental Research. 1998;33(5):482–487. doi: 10.1093/alcalc/33.5.482. [DOI] [PubMed] [Google Scholar]
- Davidson RJ. Anterior cerebral asymmetry and the nature of emotion. Brain Cogn. 1992;20(1):125–151. doi: 10.1016/0278-2626(92)90065-t. [DOI] [PubMed] [Google Scholar]
- Dawson B, Cow S, Modra S, Bishop D, Stewart G. Effects of immediate post-game recovery procedures on muscle soreness, power and flexiblity levels over the next 48 hours. J Sci Med Sport. 2005;8(2):210–221. doi: 10.1016/s1440-2440(05)80012-x. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS. Psychopathology associated with drinking and alcohol use disorders in the college and general adult populations. Drug Alcohol Depend. 2005;77(2):139–150. doi: 10.1016/j.drugalcdep.2004.07.012. [DOI] [PubMed] [Google Scholar]
- DeMallie DA, Cottler LB, Compton WM., 3rd Alcohol abuse and dependence: consistency in reporting of symptoms over ten years. Alcoholism Clinical and Experimental Research. 1995;90(5):615–625. doi: 10.1046/j.1360-0443.1995.9056153.x. [DOI] [PubMed] [Google Scholar]
- Di Sclafani V, Finn P, Fein G. Treatment-naive active alcoholics have greater psychiatric comorbidity than normal controls but less than treated abstinent alcoholics. Drug Alcohol Depend. 2008;98(1–2):115–122. doi: 10.1016/j.drugalcdep.2008.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenck HJ, Eysenck SBG. Manual for the Eysenck Personality Questionnaire. (Educational and Industrial Testing Service) San Diego, CA: 1975. [Google Scholar]
- Fein G. Structural Brain MRIs in a Treatment-Naïve Active Drinking Alcohol Dependent Sample. Paper presented at the ISBRA meeting in Sydney, Australia. 2006a [Google Scholar]
- Fein G. Lifetime and Current Mood and Anxiety Disorders in Short-Term and Long-Term Abstinent Alcoholics. Alcoholism: Clinical & Experimental Research. 2013;37(11):1930–1938. doi: 10.1111/acer.12170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fein G, Chang M. Smaller feedback ERN amplitudes during the BART are associated with a greater family history density of alcohol problems in treatment-naive alcoholics. Drug Alcohol Depend. 2008;92(1–3):141–148. doi: 10.1016/j.drugalcdep.2007.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fein G, Di Sclafani V, Finn P, Scheiner DL. Sub-diagnostic psychiatric comorbidity in alcoholics. Drug Alcohol Depend. 2007;87(2–3):139–145. doi: 10.1016/j.drugalcdep.2006.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fein G, Di Sclafani V, Flinn P, Shumway R. Psychiatric Comorbidity in Older Long-Term Abstinent Alcoholics. Alcoholism Clinical and Experimental Research. 2008;33(12):1564–1571. doi: 10.1016/j.addbeh.2008.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fein G, Fein D. Antisocial Symptoms Decrease to Normal Levels in Long-Term Abstinence. Alcoholism: Clinical and Experimental Research. 2013;37(S1):E271–E280. doi: 10.1111/j.1530-0277.2012.01904.x. [DOI] [PubMed] [Google Scholar]
- Fein G, Landman BA. Treated and Treatment-Naïve Alcoholics Come From Different Populations. Alcohol. 2005;36(2):19–26. [PMC free article] [PubMed] [Google Scholar]
- Fein G, Nip V. Borderline Personality Symptoms in Short-Term and Long-Term Abstinent Alcohol Dependence. Alcoholism: Clinical and Experimental Research. 2012;36(7):1188–1195. doi: 10.1111/j.1530-0277.2011.01730.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First M, Tasman A. DSM-IV-TR Mental Disorders (Alcoholism Clinical and Experimental Research) Chichester: John Wiley and Sons; 2004. [Google Scholar]
- Gibbon M, Spitzer RL, First MB. User's guide for the structured clinical interview for DSM-IV axis II personality disorders: SCID-II: American Psychiatric Pub. 1997 [Google Scholar]
- Goldacre MJ, Duncan M, Griffith M, Cook-Mozaffari P. Alcohol as a certified cause of death in a 'middle England' population 1979–1999: database study. J Public Health (Oxf) 2004;26(4):343–346. doi: 10.1093/pubmed/fdh183. [DOI] [PubMed] [Google Scholar]
- Gough HG. Alcoholism Clinical and Experimental Research. Palo Alto: Consulting Psychologists Press; 1969. Manual for the California Psychological Inventory. [Google Scholar]
- Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, Smith SM, Dawson DA, Pulay AJ, Pickering RP, Ruan WJ. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69(4):533–545. doi: 10.4088/jcp.v69n0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Dawson DA. Introduction to the national epidemiologic survey on alcohol and related conditions. Alcohol Research & Health. 2006;29(2):74–78. [Google Scholar]
- Grant BF, Goldstein RB, Chou SP, Huang B, Stinson FS, Dawson DA, Saha TD, Smith SM, Pulay AJ, Pickering RP, Ruan WJ, Compton WM. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. [Research Support, N.I.H., Extramural Research Support, N.I.H., Intramural] Mol Psychiatry. 2009;14(11):1051–1066. doi: 10.1038/mp.2008.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Alcoholism Clinical and Experimental Research. 2004a;61(8):807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Pickering RP. Co-occurrence of 12-month alcohol and drug use disorders and personality disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Alcoholism Clinical and Experimental Research. 2004b;61(4):361–368. doi: 10.1001/archpsyc.61.4.361. [DOI] [PubMed] [Google Scholar]
- Greenfield SF, Weiss RD, Muenz LR, Vagge LM, Kelly JF, Bello LR, Michael J. The effect of depression on return to drinking: a prospective study. Alcoholism Clinical and Experimental Research. 1998;55(3):259–265. doi: 10.1001/archpsyc.55.3.259. [DOI] [PubMed] [Google Scholar]
- Grootens KP, van Luijtelaar G, Buitelaar JK, van der Laan A, Hummelen JW, Verkes RJ. Inhibition errors in borderline personality disorder with psychotic-like symptoms. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32(1):267–273. doi: 10.1016/j.pnpbp.2007.08.020. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Grant BF. Major depression in 6050 former drinkers: association with past alcohol dependence. Alcoholism Clinical and Experimental Research. 2002;59(9):794–800. doi: 10.1001/archpsyc.59.9.794. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Alcoholism Clinical and Experimental Research. 2007;64(7):830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Hathaway S, McKinley J. MMPI-2: Minnesota Multiphasic Personality Inventory (Alcoholism Clinical and Experimental Research) Minneapolis: The University of Minnesota Press; 1989. [Google Scholar]
- Haug TT, Mykletun A, Dahl AA. The association between anxiety, depression, and somatic symptoms in a large population: the HUNT-II study. Psychosom Med. 2004;66(6):845–851. doi: 10.1097/01.psy.0000145823.85658.0c. [DOI] [PubMed] [Google Scholar]
- Helzer JE, Pryzbeck TR. The co-occurrence of alcoholism with other psychiatric disorders in the general population and its impact on treatment. J Stud Alcohol. 1988;49(3):219–224. doi: 10.15288/jsa.1988.49.219. [DOI] [PubMed] [Google Scholar]
- Hesselbrock VM, Hesselbrock MN, Stabenau JR. Alcoholism in men patients subtyped by family history and antisocial personality. J Stud Alcohol. 1985;46(1):59–64. doi: 10.15288/jsa.1985.46.59. [DOI] [PubMed] [Google Scholar]
- Ionescu DF, Niciu MJ, Richards EM, Zarate CA., Jr Pharmacologic treatment of dimensional anxious depression: a review. Prim Care Companion CNS Disord. 2014;16(3) doi: 10.4088/PCC.13r01621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarque-Lopez A, Gonzalez-Reimers E, Rodriguez-Moreno F, Santolaria-Fernandez F, Lopez-Lirola A, Ros-Vilamajo R, Espinosa-Villarreal JG, Martinez-Riera A. Prevalence and mortality of heavy drinkers in a general medical hospital unit. Alcoholism Clinical and Experimental Research. 2001;36(4):335–338. doi: 10.1093/alcalc/36.4.335. [DOI] [PubMed] [Google Scholar]
- Johnson DM, Shea MT, Yen S, Battle CL, Zlotnick C, Sanislow CA, Grilo CM, Skodol AE, Bender DS, McGlashan TH, Gunderson JG, Zanarini MC. Gender differences in borderline personality disorder: findings from the Collaborative Longitudinal Personality Disorders Study. Compr Psychiatry. 2003;44(4):284–292. doi: 10.1016/S0010-440X(03)00090-7. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC. Lifetime cooccurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Alcoholism Clinical and Experimental Research. 1997;54(4):313–321. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- Kisely S, Simon G. An international study comparing the effect of medically explained and unexplained somatic symptoms on psychosocial outcome. J Psychosom Res. 2006;60(2):125–130. doi: 10.1016/j.jpsychores.2005.06.064. [DOI] [PubMed] [Google Scholar]
- Loosen PT, Dew BW, Prange AJ. Long-term predictors of outcome in abstinent alcoholic men. Alcoholism Clinical and Experimental Research. 1990;147(12):1662–1666. doi: 10.1176/ajp.147.12.1662. [DOI] [PubMed] [Google Scholar]
- Mann K, Hintz T, Jung M. Does psychiatric comorbidity in alcohol-dependent patients affect treatment outcome? Eur Arch Psychiatry Clin Neurosci. 2004;254(3):172–181. doi: 10.1007/s00406-004-0465-6. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Mehta RL, Molnar BE, Walters EE, Swendsen JD, Aguilar-Gaziola S, Bijl R, Borges G, Caraveo-Anduaga JJ, DeWit DJ, Kolody B, Vega WA, Wittchen HU, Kessler RC. Comorbidity of substance use disorders with mood and anxiety disorders: results of the International Consortium in Psychiatric Epidemiology. Alcoholism Clinical and Experimental Research. 1998;23(6):893–907. doi: 10.1016/s0306-4603(98)00076-8. [DOI] [PubMed] [Google Scholar]
- Mosquera D, Gonzalez A, Leeds AM. Early experience, structural dissociation, and emotional dysregulation in borderline personality disorder: the role of insecure and disorganized attachment. Borderline Personal Disord Emot Dysregul. 2014;1:15. doi: 10.1186/2051-6673-1-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng TP, Feng L, Chiam PC, Kua EH. Psychiatric morbidity and acute hospitalization in elderly people. Int Psychogeriatr. 2006;18(4):701–711. doi: 10.1017/S1041610206003346. [DOI] [PubMed] [Google Scholar]
- Ojesjo L, Hagnell O, Otterbeck L. Mortality in alcoholism among men in the Lundby Community Cohort, Sweden: a forty-year follow-up. J Stud Alcohol. 1998;59(2):140–145. doi: 10.15288/jsa.1998.59.140. [DOI] [PubMed] [Google Scholar]
- Oscar-Berman M, Valmas MM, Sawyer KS, Kirkley SM, Gansler DA, Merritt D, Couture A. Frontal brain dysfunction in alcoholism with and without antisocial personality disorder. Neuropsychiatr Dis Treat. 2009;5:309–326. doi: 10.2147/ndt.s4882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preissler S, Dziobek I, Ritter K, Heekeren HR, Roepke S. Social Cognition in Borderline Personality Disorder: Evidence for Disturbed Recognition of the Emotions, Thoughts, and Intentions of others. Front Behav Neurosci. 2010;4:182. doi: 10.3389/fnbeh.2010.00182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264(19):2511–2518. [PubMed] [Google Scholar]
- Rehm J, Patra J, Popova S. Alcohol-attributable mortality and potential years of life lost in Canada 2001: implications for prevention and policy. Alcoholism Clinical and Experimental Research. 2006;101(3):373–384. doi: 10.1111/j.1360-0443.2005.01338.x. [DOI] [PubMed] [Google Scholar]
- Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behaviour Research and Therapy. 1986;24(1):1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Robins LNCL, Bruckholz K, Compton W. The diagnostic interview schedule for DSM-IV. St. Louis MO: Washington University of Medicine; 1998. [Google Scholar]
- Roepke S, Vater A, Preissler S, Heekeren HR, Dziobek I. Social cognition in borderline personality disorder. Front Neurosci. 2012;6:195. doi: 10.3389/fnins.2012.00195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rounsaville BJ, Dolinsky ZS, Babor TF, Meyer RE. Psychopathology as a predictor of treatment outcome in alcoholics. Alcoholism Clinical and Experimental Research. 1987;44(6):505–513. doi: 10.1001/archpsyc.1987.01800180015002. [DOI] [PubMed] [Google Scholar]
- Sabo AN. Etiological significance of associations between childhood trauma and borderline personality disorder: conceptual and clinical implications. J Pers Disord. 1997;11(1):50–70. doi: 10.1521/pedi.1997.11.1.50. [DOI] [PubMed] [Google Scholar]
- Schmahl C, Herpertz SC, Bertsch K, Ende G, Flor H, Kirsch P, Lis S, Meyer-Lindenberg A, Rietschel M, Schneider M, Spanagel R, Treede RD, Bohus M. Mechanisms of disturbed emotion processing and social interaction in borderline personality disorder: state of knowledge and research agenda of the German Clinical Research Unit. Borderline Personal Disord Emot Dysregul. 2014;1:12. doi: 10.1186/2051-6673-1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuckit M. Alcoholic patients with secondary depression. Alcoholism Clinical and Experimental Research. 1983;140(6):711–714. doi: 10.1176/ajp.140.6.711. [DOI] [PubMed] [Google Scholar]
- Sher L. Alcohol use and suicide rates. Med Hypotheses. 2005;65(6):1010–1012. doi: 10.1016/j.mehy.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Snyder HR. Major depressive disorder is associated with broad impairments on neuropsychological measures of executive function: a meta-analysis and review. Psychol Bull. 2013;139(1):81–132. doi: 10.1037/a0028727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Summaries for patients. The effects of limited sleep and alcohol on driving performance in people with untreated sleep apnea. [Patient Education Handout]. Annals of Internal Medicine. 2009;151(7):I-32. doi: 10.7326/0003-4819-151-7-200910060-00002. [DOI] [PubMed] [Google Scholar]
- Tomasson K, Vaglum P. A nationwide representative sample of treatment-seeking alcoholics: a study of psychiatric comorbidity. Alcoholism Clinical and Experimental Research. 1995;92(5):378–385. doi: 10.1111/j.1600-0447.1995.tb09600.x. [DOI] [PubMed] [Google Scholar]
- Trull TJ, Sher KJ, Minks-Brown C, Durbin J, Burr R. Borderline personality disorder and substance use disorders: a review and integration. Clin Psychol Rev. 2000;20(2):235–253. doi: 10.1016/s0272-7358(99)00028-8. [DOI] [PubMed] [Google Scholar]
- Wojtyniak B, Moskalewicz J, Stokwiszewski J, Rabczenko D. Gender-specific mortality associated with alcohol consumption in Poland in transition. Alcoholism Clinical and Experimental Research. 2005;100(12):1779–1789. doi: 10.1111/j.1360-0443.2005.01247.x. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Dubo ED, Sickel AE, Trikha A, Levin A, Reynolds V. Axis I comorbidity of borderline personality disorder. Alcoholism Clinical and Experimental Research. 1998a;155(12):1733–1739. doi: 10.1176/ajp.155.12.1733. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Dubo ED, Sickel AE, Trikha A, Levin A, Reynolds V. Axis II comorbidity of borderline personality disorder. Compr Psychiatry. 1998b;39(5):296–302. doi: 10.1016/s0010-440x(98)90038-4. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Hennen J, Reich DB, Silk KR. Axis I comorbidity in patients with borderline personality disorder: 6-year follow-up and prediction of time to remission. Alcoholism Clinical and Experimental Research. 2004;161(11):2108–2114. doi: 10.1176/appi.ajp.161.11.2108. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Gunderson JG, Frankenburg FR. Cognitive features of borderline personality disorder. Alcoholism Clinical and Experimental Research. 1990;147(1):57–63. doi: 10.1176/ajp.147.1.57. [DOI] [PubMed] [Google Scholar]
- Zlomuzica A, Dere D, Machulska A, Adolph D, Dere E, Margraf J. Episodic memories in anxiety disorders: clinical implications. Front Behav Neurosci. 2014;8:131. doi: 10.3389/fnbeh.2014.00131. [DOI] [PMC free article] [PubMed] [Google Scholar]