Abstract
Various surgical procedures for carpal tunnel syndrome exist, such as open release, ultrasound-guided percutaneous release, and endoscopic release. Postoperative pain, scarring, and slow recovery to normal function are reported complications of open release. Damage to vessels and the median nerve and its branches underlying the transverse carpal ligament is a reported complication of ultrasound-guided percutaneous release. Damage to the superficial palmar arch and incomplete release are reported complications of endoscopic release. By performing endoscopic carpal tunnel release with ultrasound assistance, we could visualize neurovascular structures directly with the endoscope and also indirectly with ultrasound to minimize complications. We could also evaluate the morphologic changes of the median nerve dynamically before and after the release. We discuss the technique for this procedure and outline pearls and pitfalls for success.
Various surgical procedures for carpal tunnel syndrome exist, such as open release, ultrasound-guided percutaneous release,1, 2, 3 and endoscopic release.4, 5 Postoperative pain, scarring, and slow recovery to normal function are complications of open release.6, 7 Ultrasound-guided percutaneous release requires only a small skin incision; however, damage to the structures underlying the transverse carpal ligament, such as vessels and the median nerve, as well as its branches (i.e., third common digital nerve) (Fig 1), cannot be avoided because of poor visualization of small and thin anatomic structures with ultrasound.8 Endoscopic release enables the surgeon to directly visualize and prevent damage to the neurovascular structures underlying the transverse carpal ligament; however, incomplete release of the ligament and damage to the superficial palmar arch distal to the ligament during distal portal placement (Fig 2) are complications reported in previous literature.9, 10, 11, 12 To minimize these risks, we have been performing endoscopic carpal tunnel release with ultrasound assistance when creating the proximal and distal portals and in confirming a complete release (Video 1). This technique enables us to not only visualize the neurovascular structures at risk and prevent complications but also evaluate the morphologic changes of the median nerve dynamically before and after the release. Tips for ultrasound use during endoscopic carpal tunnel release are presented in Table 1. The purpose of this report was to discuss our technique of ultrasound-assisted endoscopic carpal tunnel release.
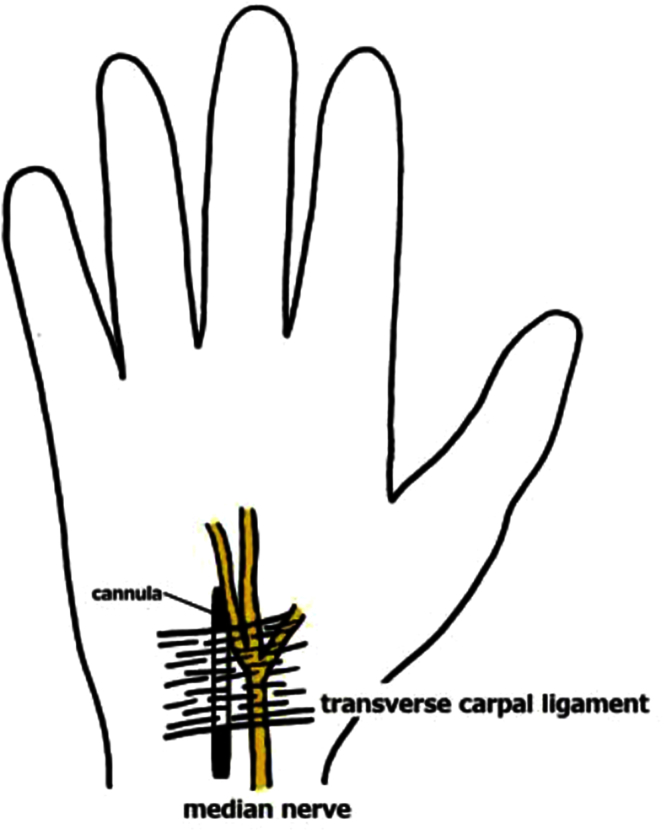
Fig 1.
The transverse carpal ligament is in proximity to the median nerve. Endoscopy of the carpal tunnel enables visualization of the median nerve and its branches and prevents inadvertent damage to the nerve during cannula placement and release of the transverse carpal ligament.
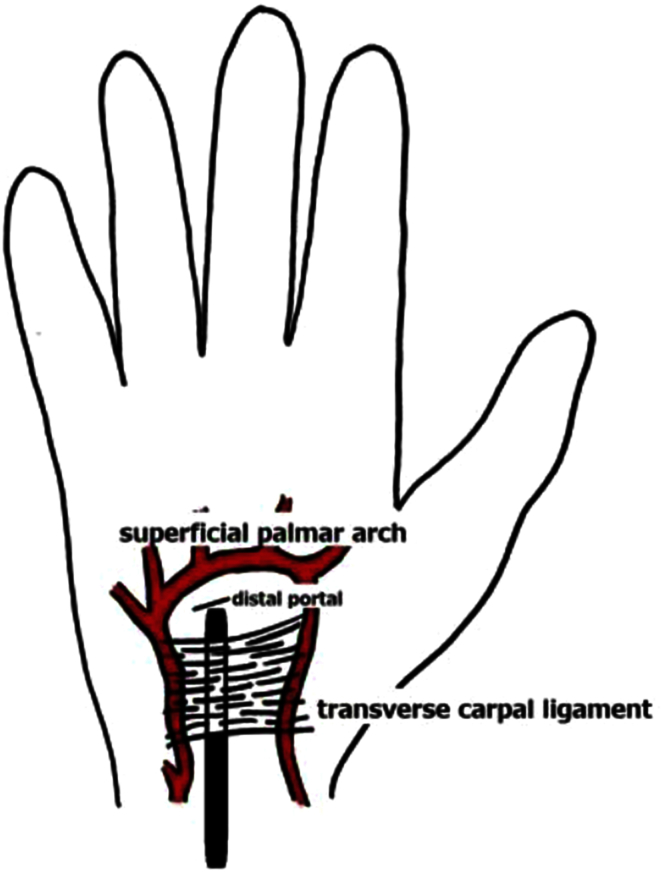
Fig 2.
The superficial palmar arch lies distal to the transverse carpal ligament and in proximity to the distal portal in endoscopic carpal tunnel release. Ultrasound assists in locating the superficial palmar arch and prevents inadvertent damage to the arch during distal portal placement.
Table 1.
Tips for Ultrasound Use During Endoscopic Carpal Tunnel Release
| Tips | Reasons |
|---|---|
| Localize median nerve compression site | Minimize release for less invasiveness |
| Localize superficial palmar arch | Prevent damage to arch in distal portal placement |
| Visualize median nerve and palmar arch in 2 planes | Obtain accurate three-dimensional orientation |
| Adjust focus to depth of median nerve | Obtain high sensitivity in visualizing nerve branches |
| Use power Doppler | Obtain high sensitivity in visualizing vessels |
Surgical Technique
We used the ECTRA 2 Carpal Ligament System (Smith & Nephew Endoscopy, Tokyo, Japan) and the M-Turbo ultrasound machine with a 13-6 MHz transducer (SonoSite, Tokyo, Japan) for our ultrasound-assisted endoscopic carpal tunnel release technique.
Positioning of Proximal Portal
The proximal portal is made as a 1-cm skin incision on the ulnar side of the palmaris longus tendon at the level of the proximal wrist flexor crease. If the palmaris longus tendon is not palpable, the skin incision is made at a point approximately 1.5 cm radial from the pisiform bone running 1.0 cm in length radially at the level of the proximal wrist flexor crease. We use ultrasound to confirm that this incision is not directly above but lies just ulnar to the median nerve (Figs 3 and 4) and that it is proximal enough to allow easy access to the undersurface of the transverse carpal ligament without compressing the flexor tendons deep to the ligament.
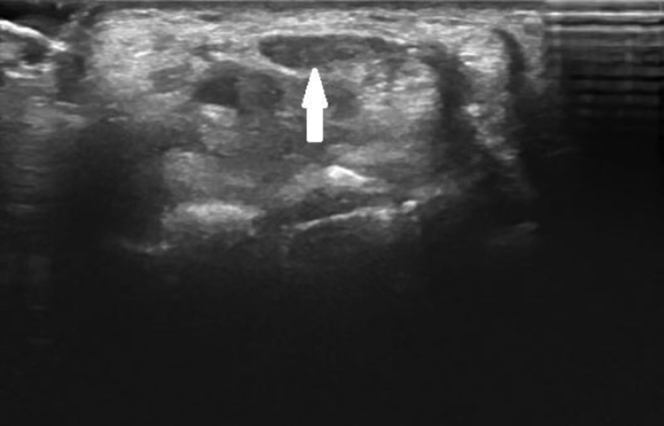
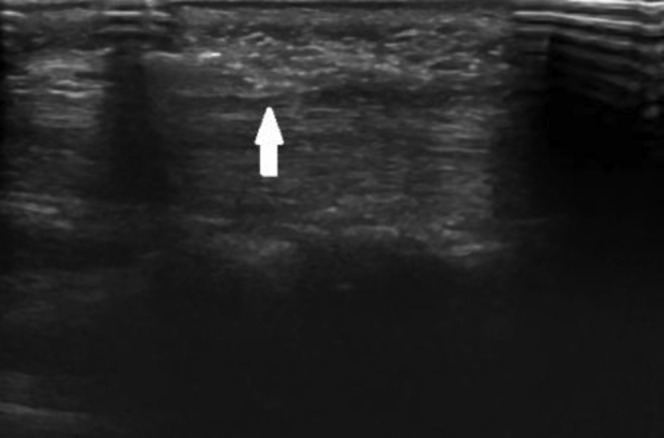
Fig 3.
Short-axis ultrasound image of median nerve (arrow). The median nerve is superficial to the flexor tendons inside the carpal tunnel and has an oval low echoic appearance.
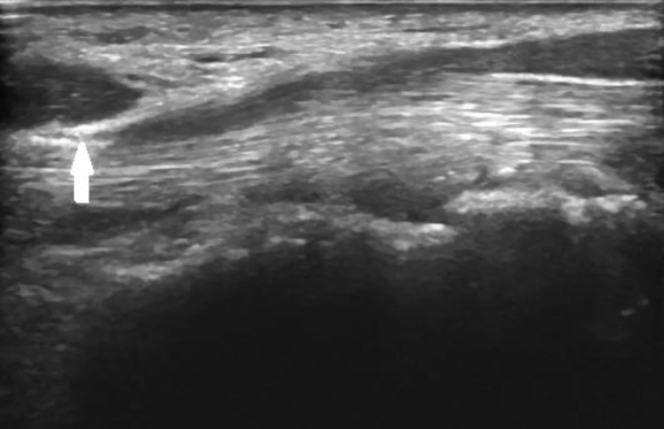
Fig 4.
Long-axis ultrasound image of median nerve. There is an abrupt change in nerve size, indicating the compression point at the proximal carpal tunnel. The left side of the image is proximal; the arrow indicates the compressed nerve.
Positioning of Distal Portal
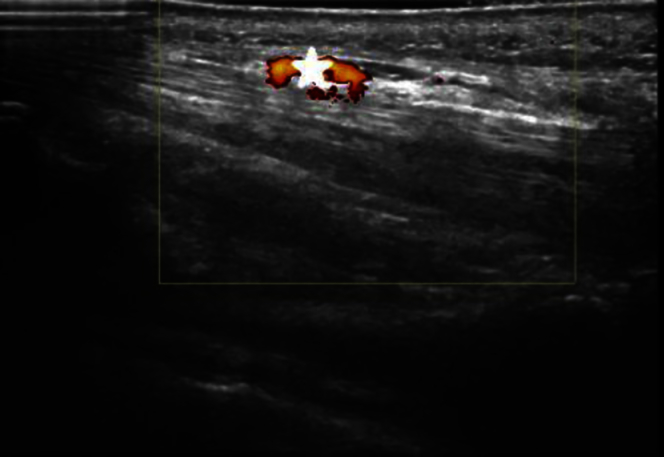
With the patient's thumb in full abduction, a line is drawn across the palm from the distal border of the thumb and a second line is drawn from the web between the second and third fingers to meet the first line, forming a right angle. A line bisecting this right angle running 1.0 cm proximally has been the recommended location of the distal portal13; however, often this portal is in proximity to the palmar arch. Thus we use power Doppler ultrasound to locate the arch (Fig 5) and make the distal portal as proximal as possible to minimize the risk of damage to the superficial palmar arch and, at the same time, confirm that it is distal enough to release the compressed median nerve completely.
Fig 5.
Power Doppler evaluation of superficial palmar arch (star). Visualization of vessels prevents inadvertent damage to these structures during distal portal placement. The left side of the image is proximal.
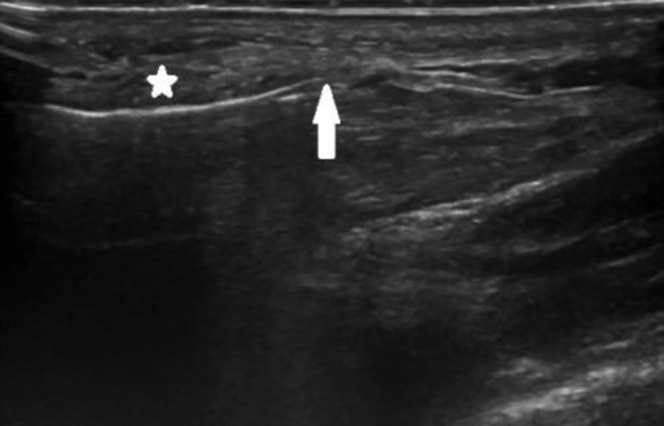
Creation of Portals and Placement of Cannula
The procedure is begun with the creation of the proximal portal. Subcutaneous tissue is bluntly dissected, and an incision is made through the volar forearm fascia to pass a curved dissector (Smith & Nephew Endoscopy) into the carpal tunnel underneath the transverse carpal ligament. The tenosynovium is dissected off the transverse carpal ligament with the curved dissector, resulting in a washboard feeling when probing the undersurface of the ligament. The surgeon uses the tip of the curved dissector to palpate the distal border of the transverse carpal ligament while visualizing the superficial palmar arch with power Doppler ultrasound (Fig 6), and after removal of the curved dissector, a slotted cannula (Smith & Nephew Endoscopy) is advanced underneath the ligament with the wrist and hand in hyperextension. The distal portal is placed at this point after confirmation that the total length of the ligament compressing the median nerve will be released and that the superficial palmar arch will not be damaged.
Fig 6.
Ultrasound image of distal border of transverse carpal ligament (star) palpated with curved dissector to confirm that placement of the distal portal will not result in damage to the superficial palmar arch. The palmar arch lies further distally (not shown). The left side of the image is proximal; the arrow indicates the tip of the dissector.
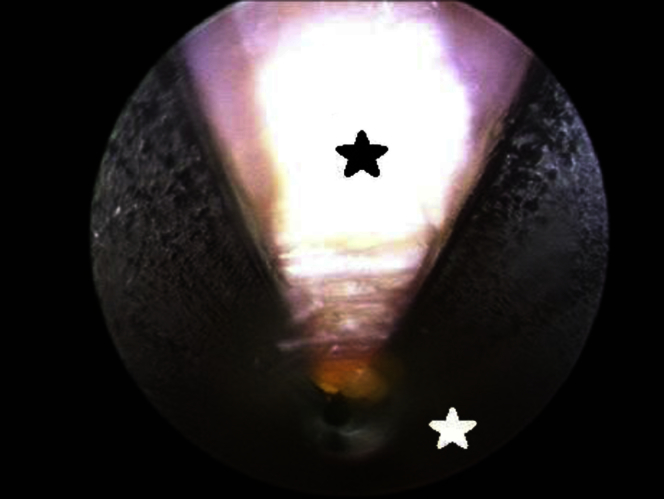
Endoscopic View of Transverse Carpal Ligament
The Carpal Tunnel VideoEndoscope (Smith & Nephew Endoscopy) is inserted into the slotted cannula at the proximal portal, and the transverse carpal ligament is identified (Fig 7). At this point, we checked for any intervening structures such as the median nerve or branch of the nerve, tendon sheath, or vessels, and if visible, the cannula can be rotated or removed or the intervening structures can be bluntly pushed away with a swab stick or probe through the slot. The transverse carpal ligament needs to be clearly seen with no other tissue visible between the ligament and the cannula.
Fig 7.
Endoscopic image of transverse carpal ligament (black star), viewed from proximal portal. The transverse carpal ligament needs to be clearly visualized with no intervening structures between the ligament and the cannula for a safe release. The white star indicates the slotted cannula.
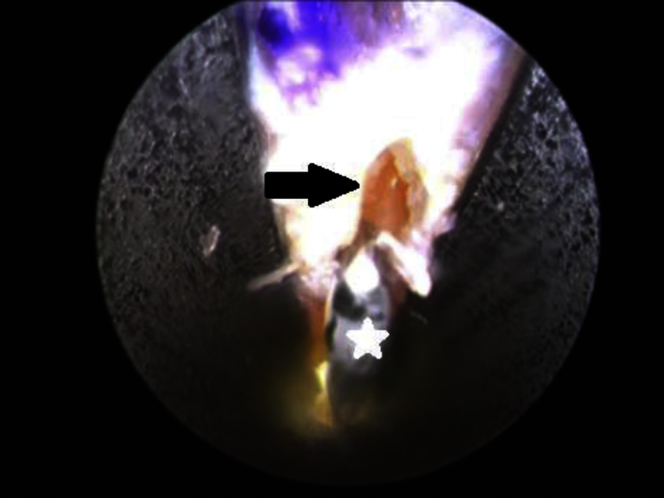
Release of Transverse Carpal Ligament and Ultrasound Confirmation
Different knives (probe knife, triangle knife, and retrograde knife; Smith & Nephew Endoscopy) are then used to release the total length of the transverse carpal ligament (Fig 8), and the release is probed to ensure complete release of the ligament (Fig 9). After irrigation of the portals, the wounds are sutured and a simple dressing is applied to finish the case. Finally, ultrasound is used to confirm successful release of the nerve (Fig 10).
Fig 8.
Endoscopic image of carpal ligament release with hook knife (star), viewed from proximal portal. The probe knife, triangle knife, and retrograde knife are used to release the total length of the transverse carpal ligament. To prevent excision beyond the distal border of the carpal ligament, this side is released by pushing the knife distally to proximally. The arrow indicates the partially released transverse carpal ligament.
Fig 9.
Endoscopic image after complete release with fat protruding into cannula, viewed from distal portal. The probe can be used to ensure complete release of the ligament without any additional fibers remaining. The black star indicates protruding fat, and the white star indicates the slotted cannula.
Fig 10.
Long-axis ultrasound image of released median nerve. After suturing of the wounds, ultrasound is used to confirm successful release of the nerve with no abrupt change in nerve size at the proximal carpal tunnel. The left side of the image is proximal; the arrow indicates the released nerve site.
Postoperative Care
Active range of motion is allowed as tolerated, and we instruct patients to avoid overuse of the hand for 2 weeks. Sutures are removed 1 week after surgery.
Discussion
Various studies have used intraoperative ultrasonography for assistance in open and percutaneous carpal tunnel release.1, 2, 14, 15, 16, 17, 18 They have reported that ultrasound is useful in visualizing the potential risks of injury to the flexor tendon and neurovascular bundles, in evaluating the completeness of the release and in identifying causes of failure such as incomplete release, and in observing the recovery process of the median nerve after the release. However, we have not found an article describing the actual techniques for use of ultrasound along with an endoscopic procedure to minimize complications and confirm complete release. Advantages and disadvantages of ultrasound-assisted endoscopic carpal tunnel release are shown in Table 2. The most important disadvantage is that there is a steep learning curve and successful treatment with this technique is operator dependent.19 However, we believe that this is the most useful technique for minimizing complications related to carpal tunnel release because of the ability to visualize anatomic structures at risk directly endoscopically and, at the same time, indirectly with ultrasound.
Table 2.
Advantages and Disadvantages of Ultrasound-Assisted Endoscopic Carpal Tunnel Release
| Advantages |
| Uses small skin incision and is minimally invasive |
| Allows multiplanar and real-time imaging |
| Minimizes neurovascular damage |
| Enables confirmation of successful release |
| Disadvantages |
| Requires high-frequency ultrasound device |
| Has steep learning curve |
| Is operator dependent |
| Has increased operative time |
Footnotes
The authors report the following potential conflict of interest or source of funding: H.O. receives support from Arthrex. S.H. receives support from Konica Minolta.
Supplementary Data
Key principles and technical pearls of ultrasound-assisted endoscopic carpal tunnel release. The proximal portal is made using ultrasound to confirm that the incision is not directly above but lies just ulnar to the median nerve and that it is proximal enough to allow easy access to the undersurface of the transverse carpal ligament without compressing the flexor tendons deep to the ligament. The distal portal is made using ultrasound to confirm that it is distal enough to release the compressed median nerve completely and to minimize the risk of damage to the superficial palmar arch. Under an endoscopic view, the transverse carpal ligament is identified, and after confirmation that there are no intervening structures, the release is performed using arthroscopic knives. After irrigation and suturing of the portals, ultrasound is used to confirm successful release of the nerve.
References
- 1.Rowe N.M., Michaels J.V., Soltanian H., Dobryansky M., Peimer C.A., Gurtner G.C. Sonographically guided percutaneous carpal tunnel release: An anatomic and cadaveric study. Ann Plast Surg. 2005;55:52–56. doi: 10.1097/01.sap.0000168281.77528.02. [DOI] [PubMed] [Google Scholar]
- 2.Nakamichi K., Tachibana S., Yamamoto S., Ida M. Percutaneous carpal tunnel release compared with mini-open release using ultrasonographic guidance for both techniques. J Hand Surg Am. 2010;35:437–445. doi: 10.1016/j.jhsa.2009.12.016. [DOI] [PubMed] [Google Scholar]
- 3.Chern T.C., Kuo L.C., Shao C.J., Wu T.T., Wu K.C., Jou I.M. Ultrasonographically guided percutaneous carpal tunnel release: Early clinical experiences and outcomes. Arthroscopy. 2015;31:2400–2410. doi: 10.1016/j.arthro.2015.06.023. [DOI] [PubMed] [Google Scholar]
- 4.Chow J.C. Endoscopic release of the carpal ligament: A new technique for carpal tunnel syndrome. Arthroscopy. 1989;5:19–24. doi: 10.1016/0749-8063(89)90085-6. [DOI] [PubMed] [Google Scholar]
- 5.Agee J.M., McCarroll H.R., Jr., Tortosa R.D., Berry D.A., Szabo R.M., Peimer C.A. Endoscopic release of the carpal tunnel: A randomized prospective multicenter study. J Hand Surg Am. 1992;17:987–995. doi: 10.1016/s0363-5023(09)91044-9. [DOI] [PubMed] [Google Scholar]
- 6.Boya H., Ozcan O., Oztekin H.H. Long-term complications of open carpal tunnel release. Muscle Nerve. 2008;38:1443–1446. doi: 10.1002/mus.21068. [DOI] [PubMed] [Google Scholar]
- 7.Kluge W., Simpson R.G., Nicol A.C. Late complications after open carpal tunnel decompression. J Hand Surg Br. 1996;21:205–207. doi: 10.1016/s0266-7681(96)80098-2. [DOI] [PubMed] [Google Scholar]
- 8.Engineer N.J., Hazani R., Mowlavi A., Neumeister M.W., Lee W.P., Wilhelmi B.J. Variations in the anatomy of the third common digital nerve and landmarks to avoid injury to the third common digital nerve with carpal tunnel release. Eplasty. 2008;8:e51. [PMC free article] [PubMed] [Google Scholar]
- 9.Neuhaus V., Christoforou D., Cheriyan T., Mudgal C.S. Evaluation and treatment of failed carpal tunnel release. Orthop Clin North Am. 2012;43:439–447. doi: 10.1016/j.ocl.2012.07.013. [DOI] [PubMed] [Google Scholar]
- 10.Herrera J.T., Ceja B.C., Hernández J.M., Sesma R.V., Gargollo C. Carpal tunnel release with minimal incisions. Evaluation of the technique in fresh cadaver models. Acta Ortop Mex. 2013;27:260–264. [in Spanish] [PubMed] [Google Scholar]
- 11.Didailler P., Ragois P., Morales P. Pseudoaneurysm of the superficial palmar arch, following endoscopic carpal tunnel release. A case report. Chir Main. 2011;30:73–75. doi: 10.1016/j.main.2010.09.002. [in French] [DOI] [PubMed] [Google Scholar]
- 12.Bilgin S.S., Kose K.C., Demirtas A.M., Adiyaman S. Necessity of inspection of superficial palmar arch by blunt dissection from exit portal in endoscopic carpal tunnel release. Plast Reconstr Surg. 2004;114:602–603. doi: 10.1097/01.prs.0000128492.17782.ec. [DOI] [PubMed] [Google Scholar]
- 13.Chow J.C., Hantes M. Endoscopic carpal tunnel release: Thirteen years' experience with the Chow technique. J Hand Surg Am. 2002;27:1011–1018. doi: 10.1053/jhsu.2002.35884. [DOI] [PubMed] [Google Scholar]
- 14.Lecoq B., Hanouz N., Vielpeau C., Marcelli C. Ultrasound-guided percutaneous surgery for carpal tunnel syndrome: A cadaver study. Joint Bone Spine. 2011;78:516–518. doi: 10.1016/j.jbspin.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 15.McShane J.M., Slaff S., Gold J.E., Nazarian L.N. Sonographically guided percutaneous needle release of the carpal tunnel for treatment of carpal tunnel syndrome: Preliminary report. J Ultrasound Med. 2012;31:1341–1349. doi: 10.7863/jum.2012.31.9.1341. [DOI] [PubMed] [Google Scholar]
- 16.Karabay N., Toros T., Çetinkol E., Ada S. Correlations between ultrasonography findings and surgical findings in patients with refractory symptoms after primary surgical release for carpal tunnel syndrome. Acta Orthop Traumatol Turc. 2015;49:126–132. doi: 10.3944/AOTT.2015.14.0198. [DOI] [PubMed] [Google Scholar]
- 17.Yoshii Y., Ishii T., Tung W.L. Ultrasound assessment of the effectiveness of carpal tunnel release on median nerve deformation. J Orthop Res. 2015;33:726–730. doi: 10.1002/jor.22843. [DOI] [PubMed] [Google Scholar]
- 18.Chern T.C., Wu K.C., Huang L.W. A cadaveric and preliminary clinical study of ultrasonographically assisted percutaneous carpal tunnel release. Ultrasound Med Biol. 2014;40:1819–1826. doi: 10.1016/j.ultrasmedbio.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 19.Ohuchi H., Ichikawa K., Shinga K., Hattori S., Yamada S., Takahashi K. Ultrasound-assisted endoscopic partial plantar fascia release. Arthrosc Tech. 2013;2:e227–e230. doi: 10.1016/j.eats.2013.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Key principles and technical pearls of ultrasound-assisted endoscopic carpal tunnel release. The proximal portal is made using ultrasound to confirm that the incision is not directly above but lies just ulnar to the median nerve and that it is proximal enough to allow easy access to the undersurface of the transverse carpal ligament without compressing the flexor tendons deep to the ligament. The distal portal is made using ultrasound to confirm that it is distal enough to release the compressed median nerve completely and to minimize the risk of damage to the superficial palmar arch. Under an endoscopic view, the transverse carpal ligament is identified, and after confirmation that there are no intervening structures, the release is performed using arthroscopic knives. After irrigation and suturing of the portals, ultrasound is used to confirm successful release of the nerve.