ABSTRACT
The only licensed live attenuated influenza A virus vaccines (LAIVs) in the United States (FluMist) are created using internal protein-coding gene segments from the cold-adapted temperature-sensitive master donor virus A/Ann Arbor/6/1960 and HA/NA gene segments from circulating viruses. During serial passage of A/Ann Arbor/6/1960 at low temperatures to select the desired attenuating phenotypes, multiple cold-adaptive mutations and temperature-sensitive mutations arose. A substantial amount of scientific and clinical evidence has proven that FluMist is safe and effective. Nevertheless, no study has been conducted specifically to determine if the attenuating temperature-sensitive phenotype can revert and, if so, the types of substitutions that will emerge (i.e., compensatory substitutions versus reversion of existing attenuating mutations). Serial passage of the monovalent FluMist 2009 H1N1 pandemic vaccine at increasing temperatures in vitro generated a variant that replicated efficiently at higher temperatures. Sequencing of the variant identified seven nonsynonymous mutations, PB1-E51K, PB1-I171V, PA-N350K, PA-L366I, NP-N125Y, NP-V186I, and NS2-G63E. None occurred at positions previously reported to affect the temperature sensitivity of influenza A viruses. Synthetic genomics technology was used to synthesize the whole genome of the virus, and the roles of individual mutations were characterized by assessing their effects on RNA polymerase activity and virus replication kinetics at various temperatures. The revertant also regained virulence and caused significant disease in mice, with severity comparable to that caused by a wild-type 2009 H1N1 pandemic virus.
IMPORTANCE The live attenuated influenza vaccine FluMist has been proven safe and effective and is widely used in the United States. The phenotype and genotype of the vaccine virus are believed to be very stable, and mutants that cause disease in animals or humans have never been reported. By propagating the virus under well-controlled laboratory conditions, we found that the FluMist vaccine backbone could regain virulence to cause severe disease in mice. The identification of the responsible substitutions and elucidation of the underlying mechanisms provide unique insights into the attenuation of influenza virus, which is important to basic research on vaccines, attenuation reversion, and replication. In addition, this study suggests that the safety of LAIVs should be closely monitored after mass vaccination and that novel strategies to continue to improve LAIV vaccine safety should be investigated.
INTRODUCTION
Annual influenza epidemics are caused by influenza A (H1N1 and H3N2) and influenza B viruses that infect 5% to 10% of adults and 20% to 30% of children (1). Disease outcomes range from subclinical infections to severe infections that result in very high mortality. The estimated 3 to 5 million cases of severe illness and 250,000 to 500,000 deaths each year, as well as significant socioeconomic losses, warrant continuous improvements in influenza prevention, diagnosis, and treatment.
Vaccination is the most effective way to prevent influenza virus infections and alleviate disease severity. During the 2012-2013 influenza season in the United States, in spite of a less than 45% vaccination rate in people older than 6 months, vaccination still prevented an estimated 6.6 million influenza virus-associated illnesses, 3.2 million medically attended illnesses, and 79,000 hospitalizations (2). Both inactivated and live attenuated vaccines are available for influenza immunization, with the former more widely used than the latter. Inactivated influenza vaccines have been used for more than 70 years with proven safety and moderate effectiveness (3). Live attenuated influenza vaccines (LAIVs) have been used in the former Soviet Union and Russia for several decades, but they were not used in other countries until the licensure of FluMist in the United States in 2003. Comparative studies in humans have demonstrated that LAIVs have the potential to provide better protection than the split inactivated vaccines in children and adolescents 2 to 17 years of age (4–12), which may have resulted partly from the disputable superiority of LAIVs in eliciting IgA mucosal immunity and cellular immunity (13–19).
Influenza A viruses are encoded by eight segments of negative-sense RNA (viral RNA [vRNA]), and FluMist LAIVs are reassortant viruses that contain the HA and NA surface glycoprotein vRNAs from contemporary strains and the remaining six backbone vRNA segments (PB2, PB1, PA, NP, M, and NS) from a cold-adapted master donor virus (20, 21). HA and NA are the major antigenic determinants of FluMist and are from strains biannually predicted by a WHO vaccine strain recommendation committee to provide the best antigenic match to the strains circulating in humans. The master donor backbone (i.e., ca A/Ann Arbor/6/1960 [caAA60]) imparts the cold-adapted (ca), temperature-sensitive (ts), and attenuated (att) phenotypes to the FluMist vaccines. The caAA60 virus was originally generated by H. F. Maassab in the 1960s through serial passage of the wild-type AA60 virus at successively lower temperatures (22). At temperatures close to or a few degrees lower than the human core body temperature (33°C to 37°C), the caAA60 virus still replicates as efficiently as the wild-type virus does. However, at higher temperatures (e.g., 39°C) that are still permissive to the wild-type virus, the caAA60 virus has lost the ability to replicate and has thus become temperature sensitive (ts); in contrast, at lower temperatures (e.g., 25°C) that are too low for the wild-type virus to replicate, the caAA60 virus replicates efficiently and thus is cold adapted. Largely due to their temperature-sensitive feature, the caAA60 virus and vaccine reassortants are attenuated in the hosts, with their replication severely restricted in the warmer lower respiratory tract of animals and absence of symptoms of lower respiratory tract disease in humans administered the vaccine. A substantial amount of scientific and clinical evidence has proven the caAA60-based LAIVs (e.g., FluMist) safe and protective in animals and humans (reviewed in reference 21).
To determine what vRNA segments are responsible for the ca, ts, and att phenotypes of caAA60, early studies relied heavily on using classic gene reassortment between caAA60 and other viruses. Although the different gene constellations of the reassortants often confounded the results, the studies suggested that the PB2 and PB1 segments contributed to the ts phenotype; the PA segment contributed to the ca phenotype; and the PB2, PB1, PA, NP, and M segments contributed to the att phenotype (23–25). Sequence comparison between the complete genomes of caAA60 and wild-type AA60 identified multiple synonymous and nonsynonymous changes in each of the six backbone vRNAs (26), further supporting the notion that there is a network of mutations that confer the ca, ts, and att phenotypes independently and interdependently. More recently, reverse genetics irrefutably confirmed that PB1-K391E/E581G/A661T, PB2-N265S, and NP-D34G are the major loci responsible for the ts phenotype of caAA60 and that they are sufficient to confer the ts phenotype on the A/PR/8/34 strain (27, 28).
Although the ts phenotype of many experimental ts influenza viruses is unstable in vitro or in vivo (29–39), the ts phenotype of the caAA60-based vaccines has been very stable following replication in animals and humans (21). Nevertheless, recent studies on the genetic stability of FluMist reported that mutations can occur in the manufacturing process and in the replication of the virus in vaccinated children (40, 41). As FluMist is shed from children and adults postvaccination (42–44), the potential of the mutations for enhanced transmission and increased virulence should not be neglected. Consequently, we sought to evaluate the phenotypic and genetic stability of FluMist by investigating the following questions. (i) Is it possible for the caAA60 backbone to lose its ts phenotype? (ii) What substitutions will emerge, and are they compensatory changes or reversion of existing mutations to the original wild-type residues? (iii) Will the reversion of the ts phenotype in vitro result in the reversion of the att phenotype in vivo?
MATERIALS AND METHODS
Biosafety and ethics statement.
All experiments with infectious virus were performed in a biosafety level 2 laboratory using procedures and facilities that met the requirements set forth by the U.S. Department of Health and Human Services for propagation of influenza A viruses. In vivo experiments were carried out in strict accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health. Mouse studies were conducted under animal care and use protocols approved by St. Jude Children's Research Hospital's Institutional Animal Care and Use Committee (IACUC protocol 512). No survival surgery was performed, and all efforts were made to minimize suffering.
Cells.
Human embryonic kidney 293T (HEK-293T) cells were maintained in Dulbecco's modified Eagle's medium (DMEM) supplemented with 10% fetal bovine serum (FBS). Madin-Darby canine kidney (MDCK) cells were maintained in minimum essential medium (MEM) supplemented with 5% FBS.
Virus and serial passage.
An aliquot of surplus 2009 pandemic H1N1 live attenuated vaccine (FluMist; monovalent) was provided by the New York State Department of Health and used as a control in our previous vaccine study (45). Residual virus (5 μl) left over from that aliquot was inoculated into an MDCK monolayer in a 35-mm petri dish and cultured at 30°C for 3 days. Since cytopathic effect (CPE) was not evident, all the supernatant from the petri dish (passage 1 [P1]) was transferred to a fresh MDCK monolayer in a T-75 flask; 3 days later, CPE became evident, and all the supernatant (P2) was collected and aliquoted. The P2 virus stock (FluMist/pH1N1-P2) was further passaged in MDCK cells at gradually elevated temperatures, as illustrated in Fig. 1A. The last passage (P20) was done at 37°C under the assumption that the adapted virus might still replicate to higher titers at 37°C than at 39°C, so we could obtain a high titer of P20 stock.
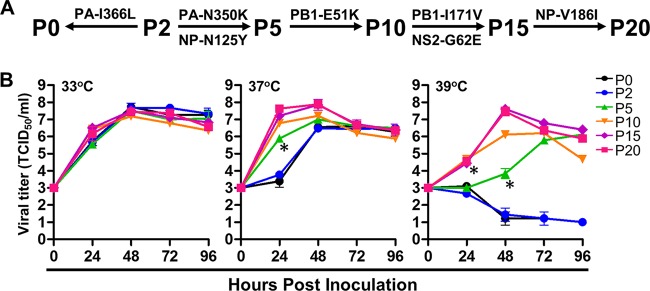
FIG 1.
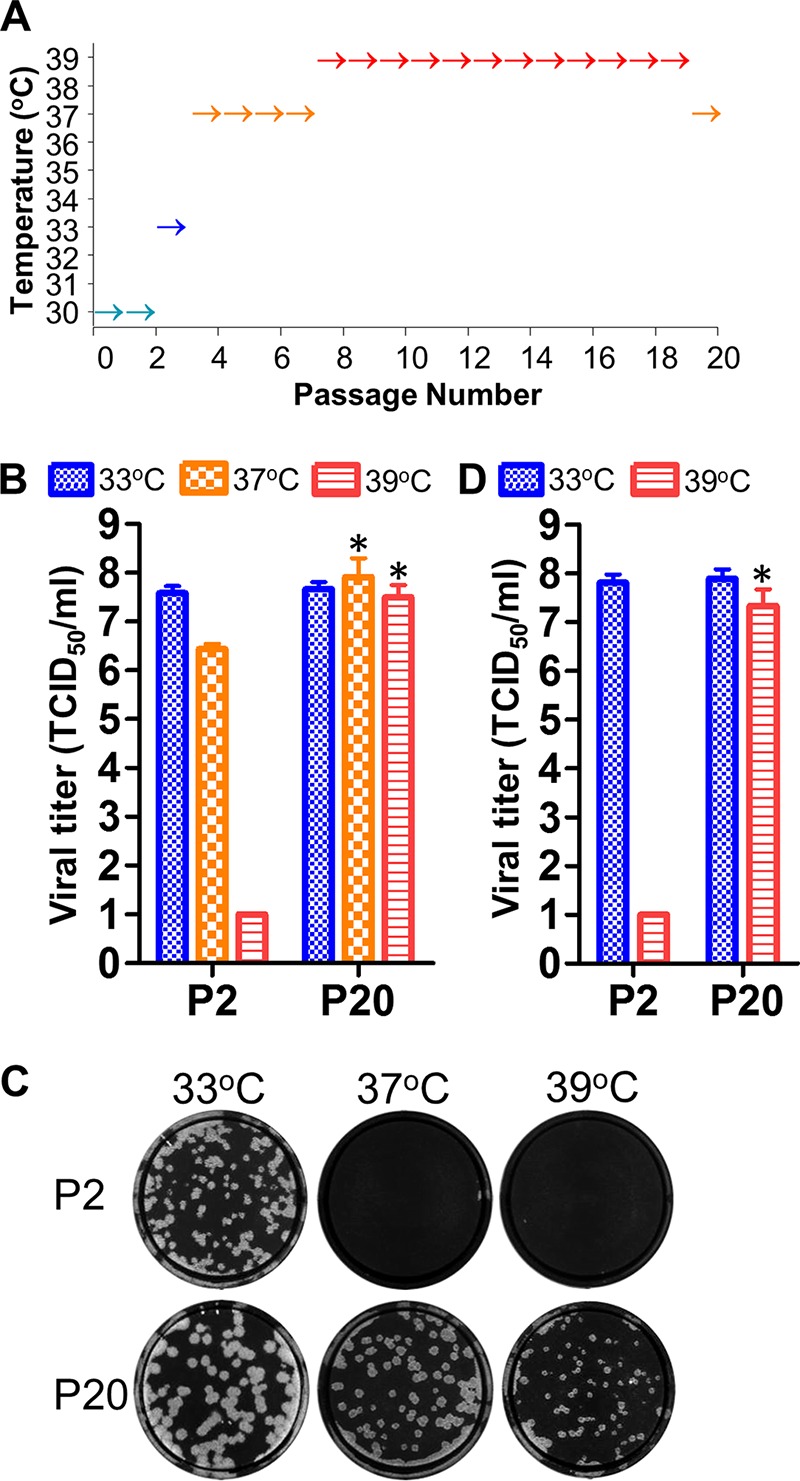
Generation of a FluMist/pH1N1 variant capable of replication at nonpermissive temperatures. (A) The FluMist/pH1N1 virus was passaged at gradually elevated temperatures. (B) Maximal viral titers of FluMist/pH1N1-P2 and FluMist/pH1N1-P20 in MDCK cells (MOI = 0.002 TCID50/cell) at 33°C, 37°C, and 39°C (maximal titers were achieved at 2 dpi at all temperatures). (C) Plaque sizes of FluMist/pH1N1-P2 and FluMist/pH1N1-P20 in MDCK cells at 33°C, 37°C, and 39°C. (D) Maximal viral titers of FluMist/pH1N1-P2 and FluMist/pH1N1-P20 in embryonated chicken eggs (1,000 TCID50/egg) at 33°C and 39°C (maximal titers were achieved at 2 dpi at both temperatures). *, P < 0.05 for FluMist/pH1N1-P20 compared to FluMist/pH1N1-P2 at corresponding temperatures. The error bars represent SD.
Sequencing and analysis.
Since the FluMist/pH1N1-P0 and -P1 viruses were exhausted in passage, we chose FluMist/pH1N1-P2, -P5, -P10, -P15, and -P20 for deep sequencing to determine the presence of nucleotide substitutions. The genomes of the viruses were amplified using the multisegment reverse transcription-PCR method (46) and sequenced using the Illumina MiSeq platform, as described previously (47). The sequence reads were sorted by sample index, trimmed, and mapped to the caAA60 reference genome retrieved from GenBank (PB2, M23970; PB1, M23972; PA, M23974; NP, M23976; M, M23978; NS, M23968) using the CLC Genomics Workbench program. The average sequencing depth for each viral segment varied from a few hundred to 2,000 times coverage. At each nucleotide position, if a variant represented more than 10% of the population, it was described as a substitution or single nucleotide variant.
Genome synthesis and mutagenesis.
cDNAs encoding the six backbone vRNAs (PB2, PB1, PA, NP, M, and NS) of caAA/60 were synthesized by enzymatic assembly of oligonucleotides approximately 60 bases in length using protocols described previously in the syntheses of H7N9 and bat influenza virus genomes (48, 49). The synthetic genes were cloned into the modified bidirectional influenza virus reverse-genetics vectors pBZ61A18 (PB2, PB1, and PA) and pBZ61A15 (NP, M, and NS) using a recombination-based method (50) and transformed into Stella competent Escherichia coli cells (Clontech). Colonies were selected and sequenced. The appropriate clones for each segment were propagated for plasmid preparation and verified by sequencing. The resultant plasmids were pKMS1A1 (PB2), pBZ170A7 (PB1), pWW58A1 (PA), pKMS2A2 (NP), pKMS3A1 (M), and pBZ172A1 (NS). The plasmids containing mutations were generated by site-directed mutagenesis, and the resultant plasmids were pWW43A1 (PB1-E51K), pWW44A1 (PB1-I171V), pWW39A1 (PB1-E51K/I171V, or PB1P20), pWW46A1 (PA-N350K), pWW59A1 (PA-L366I), pWW40A2 (PA-N350K/L366I, or PAP20), pWW61A8 (NP-N125Y), pWW62A6 (NP-V186I), pWW41A2 (NP-N125Y/V186I, or NPP20), and pWW42A1 (NS2-G63E, or NSP20).
Minigenome replication assay.
The luciferase-mediated minigenome replication assay was performed as previously described, using a PolI-driven firefly luciferase reporter plasmid and pDZ-based PB2, PB1, PA, and NP bidirectional expression plasmids (51). Briefly, HEK-293T cells in 24-well plates were cotransfected with 0.2 μg each of pPolI-NS-Luc plasmid (pBZ81A36) and caAA60 PB2, PB1, PA, and NP plasmids or mutant plasmids. As a control of transfection efficiency, 0.02 μg of the Renilla luciferase plasmid pRL-TK (Promega, Madison, WI) was also cotransfected. Cells were incubated at 33°C, 37°C, and 39°C for 12 h, and then luciferase production was assayed using the dual-luciferase reporter assay system (Promega) according to the manufacturer's instructions. Firefly luciferase expression was normalized to Renilla luciferase expression (relative activity). At each temperature, the relative activity of caAA60 polymerase was set at 100%, and the activities of the various mutants were determined relative to that. All the results shown are the averages from triplicate transfections with standard deviations (SD).
Recombinant virus rescue.
Recombinant caAA60 and various mutant viruses were generated by cotransfection of eight reverse-genetics plasmids carrying the cDNA of each gene segment into a 293T-MDCK coculture monolayer as previously described (52). Briefly, 0.6 μg of each plasmid was mixed and incubated with 15 μl of TransIt-LT1 transfection reagent (Mirus Bio, Madison, WI) at 20°C for 20 min and then added to 80% confluent 293T-MDCK cocultures in 6-well plates. The transfection plates were incubated at 33°C with 5% CO2 for 12 to 24 h before the culture supernatant was replaced with 3 ml of Opti-MEM I medium (Life Technologies) supplemented with 0.3% bovine serum albumin (BSA) fraction V (Life Technologies), 3 μg/ml tosylsulfonyl phenylalanyl chloromethyl ketone (TPCK)-trypsin (Worthington, Lakewood, NJ), and 1% antibiotic-antimycotic (Life Technologies). Three days posttransfection, the supernatant was collected and virus was propagated in MDCK cells at 33°C. All the virus stocks used for in vitro and in vivo studies were sequenced to confirm the absence of any unintended mutations.
Replication kinetics in vitro.
MDCK cell monolayers in 12-well plates were washed twice with MEM, and then, 1 ml of virus growth medium (MEM supplemented with 0.15% BSA fraction V, 2 μg/ml TPCK-trypsin, and 1% antibiotic-antimycotic) was added to each well. The cells were inoculated with the indicated viruses at a multiplicity of infection (MOI) of ∼0.002 50% tissue culture infective dose (TCID50)/cell. The cells were incubated at three different temperatures (33°C, 37°C, and 39°C) after inoculation. The supernatants were collected at the indicated time points (hours postinoculation [hpi]). For comparison of the reverse-genetics-rescued recombinant viruses rFluMist/pH1N1-P0, -P2, -P5, -P10, -P15, and -P20, there were 5 × 105 cells in each well (in 12-well plates), and we diluted each of the 6 virus stocks to 104 TCID50/ml and added at 100 μl/well to 36 wells in three 12-well plates (MOI = 0.002 TCID50/ml) and then added 900 μl infection medium/well. For each virus, we subjected 1 of the 12-well plates to 33°C, 37°C, or 39°C. On each day (24, 48, 72, and 96 hpi), we collected supernatants from 3 wells at each temperature for virus titration. The inocula were back titrated. Comparisons of the other recombinant viruses were done similarly, with additional sample collections at 0 and 2 hpi. For comparison of FluMist/pH1N1-P2 and FluMist/pH1N1-P20 in 10-day-old embryonated chicken eggs, 1,000 TCID50 of virus was used for each egg. All virus titers were determined by TCID50 assay using MDCK cells.
Mouse experiments.
Six-week-old female BALB/cJ mice (Jackson Laboratory, Bar Harbor, ME) were anesthetized with isoflurane and inoculated intranasally with 25 μl MEM diluent containing 106 TCID50 of rFluMist/pH1N1-P0, rFluMist/pH1N1-P20, rFluMist/pH1N1-P20_PA-I366L, rFluMist/pH1N1-P20_NS2-E63G, or a pH1N1 virus or mock inoculated (15 mice/virus group). The rFluMist/pH1N1-P20_PA-I366L virus is the same as the rFluMist/pH1N1-P20 virus, except that it does not contain the PA-L366I mutation; the rFluMist/pH1N1-P20_NS2-E63G virus is the same as the rFluMist/pH1N1-P20 virus, except that it does not contain the NS2-G63E mutation; the pH1N1 virus is a recombinant 2009 H1N1 pandemic strain, A/New York/1682/2009, whose HA and NA are replaced with those from the FluMist vaccine used in this study (A/CA/07/2009 with mutations [53]). For each group, the body weights of 5 mice were measured daily for 10 days, and clinical observations were recorded. At 2 and 4 days postinfection (dpi), 5 mice from each group were euthanized, and nasal washes were collected in 1 ml medium. Lungs (n = 4) were homogenized in 1 ml medium and clarified by centrifugation. Nasal wash and lung viral titers were determined by TCID50 assay. Immunohistochemical (IHC) staining for influenza virus NP (antibody 05G; United States Biological, Salem, MA) was performed on 3-μm lung sections by the St. Jude Children's Research Hospital Veterinary Pathology Core Facility.
Structural analysis.
Temperature-sensitive mutations in the caAA60 virus and temperature-permissive mutations in the FluMist revertant from this study were mapped to the bat influenza virus polymerase X-ray structure (Protein Data Bank [PDB] ID 4WSB) and the A/WSN/33 NP structure (PDB ID 3RO5). The mapped structures were visualized and generated in PyMOL.
Statistics.
Luciferase activity, virus titers, and mouse weights were analyzed by using Student's t test or analysis of variance (ANOVA) in GraphPad Prism version 5.0 (GraphPad Software Inc., La Jolla, CA). The standard deviation (SD) for each of the procedures is shown.
Accession number(s).
The GenBank accession numbers for the assembled consensus genome sequences of FluMist/pH1N1-P2, -P5, -P10, -P15, and -P20 are KT383437 to KT383466.
RESULTS
FluMist/pH1N1 overcame temperature restriction.
To test if the licensed live attenuated influenza vaccine FluMist backbone could maintain a stable phenotype under the experimental conditions, the monovalent FluMist vaccine for the 2009 H1N1 pandemic (FluMist/pH1N1) was passaged at gradually elevated temperatures from 30°C to 39°C for 20 passages in MDCK cells (Fig. 1A). In contrast to the parental stock virus, which underwent two passages postmanufacture at 30°C (FluMist/pH1N1-P2), the virus that underwent 20 passages at higher temperatures (FluMist/pH1N1-P20) overcame the replication restriction imposed by higher temperatures (e.g., 39°C), replicated to high titers (107.5 TCID50/ml), and formed obvious plaques at the restrictive temperature (39°C for FluMist/pH1N1) (Fig. 1B and C). This FluMist/pH1N1-P20 also replicated to high titers (107.3 TCID50/ml) in 10-day-old embryonated chicken eggs at 39°C (Fig. 1D), indicating that the robust replication of FluMist/pH1N1-P20 in MDCK cells at 39°C was not due to host-specific adaptation, but rather, it was a real reversion of the temperature-sensitive phenotype of FluMist/pH1N1.
Multiple compensatory mutations enhanced virus replication.
To determine the genetic basis of the phenotypic reversion, we analyzed the whole genomes of FluMist/pH1N1-P2, -P5, -P10, -P15, and -P20 viruses using a next-generation-sequencing (NGS) approach. Multiple mutations emerged gradually in the FluMist/pH1N1 genome in the course of serial passages compared to the caAA60 reference genome in GenBank (Table 1). Interestingly, none of the new substitutions were reversions of the existing mutations that are potentially responsible for the temperature-sensitive phenotype of caAA60, including PB2-N265S; PB1-K391E, -E457D, -E581G, and -A661T; PA-K613E and -L715P; NP-T23N and -D34G; M2-A86S; and NS1-A153T (26, 27).
TABLE 1.
Mutations detected at different passages of FluMist
| Reference genea | Mutationb |
Frequencyc (%) |
|||||
|---|---|---|---|---|---|---|---|
| Nucleotide | Amino acid | P2 | P5 | P10 | P15 | P20 | |
| PB1 | G175A | E51K | 98.9 | 98.5 | 99.4 | ||
| PB1 | A535G | I171V | 98.9 | 99.4 | |||
| PA | A618G | Synonymous | 98.1 | 99.0 | |||
| PA | T1074G | N350K | 49.7 | 98.9 | 98.8 | 98.1 | |
| PA | C1120A | L366I | 99.7 | 99.4 | 99.5 | 99.3 | 99.5 |
| NP | A418T | N125Y | 93.2 | 99.7 | 99.5 | 99.6 | |
| NP | G601A | V186I | 74.5 | ||||
| NS | G686A | G63E(NS2) | 99.3 | 98.7 | |||
The FluMist reference genome sequences used for comparison were as follows: PB2, M23970; PB1, M23972; PA, M23974; NP, M23976; M, M23978; and NS, M23968. Only the 6 FluMist backbone genes (PB2, PB1, PA, NP, M, and NS genes) were analyzed.
Nonsynonymous mutations present in >10% of the viral population (frequency) are listed; multiple synonymous mutations were also detected as early as P2, but only the synonymous mutations absent in P2 are listed. The synonymous mutations detected in P2 could be a result of the different caA/AA/60 master strains used by the vaccine manufacturer and by the sequence depositor. We assumed they were irrelevant to the reversion of the ts phenotype, since P2 was passaged only at 30°C.
Frequency, the percentage of the viral population containing a specific mutation.
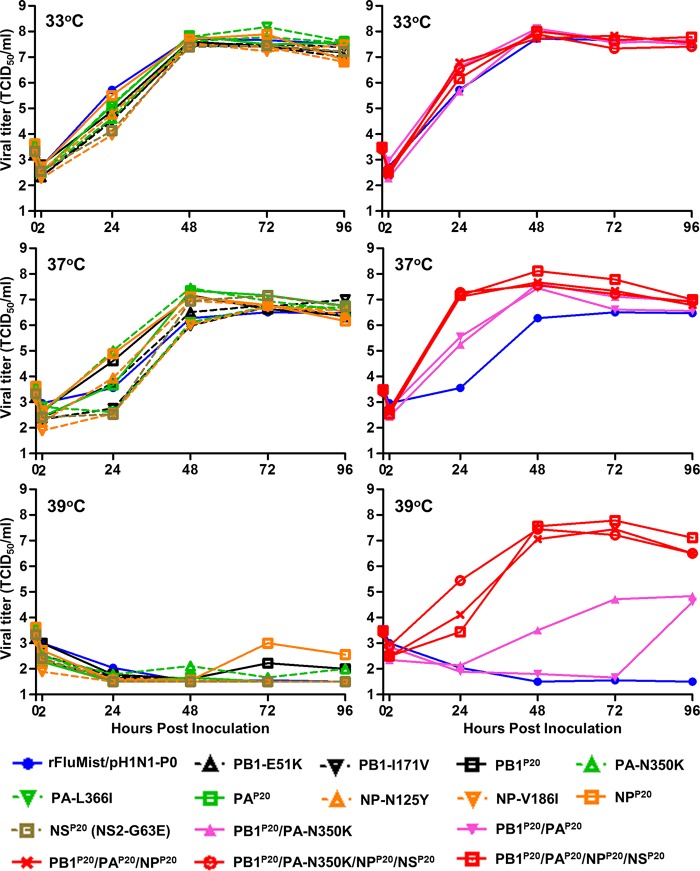
We then synthesized the complete genome of FluMist/pH1N1-P2 using a rapid gene synthesis technology described previously (48, 49, 54), cloned it into the bidirectional reverse-genetics vectors pBZ61A15 and pBZ61A18 (46, 50), and rescued the recombinant virus rFluMist/pH1N1-P2. Based on the sequence analysis (Table 1), we assumed that rFluMist/pH1N1-P0 had a leucine at PA residue 366, as shown in the GenBank reference sequence, so we reintroduced PA-I366L into rFluMist/pH1N1-P2 and rescued the rFluMist/pH1N1-P0 virus. PA-N350K and NP-N125Y were introduced into rFluMist/pH1N1-P2 to rescue rFluMist/pH1N1-P5. PB1-E51K was introduced into rFluMist/pH1N1-P5 to rescue rFluMist/pH1N1-P10. PB1-I171V and NS2-G63E were introduced into rFluMist/pH1N1-P10 to rescue rFluMist/pH1N1-P15. Finally, NP-V186I was introduced into rFluMist/pH1N1-P15 to rescue rFluMist/pH1N1-P20 (Fig. 2A). The replication kinetics of the six rFluMist/pH1N1 viruses were compared at different temperatures. At 33°C, all the viruses showed similar replication kinetics, whereas the results from 37°C and 39°C suggested a gradually increased ability of the viruses to replicate at restrictive temperatures: P0 and P2 < P5 < P10 < P15 and P20 (Fig. 2B). Therefore, the ts phenotypic reversion of FluMist/pH1N1 was accomplished by sequential selection of compensatory mutations at restrictive temperatures.
FIG 2.
Generation of recombinant FluMist/pH1N1 and revertants and their replication kinetics. (A) Reverse-genetics generation of rFluMist/pH1N1-P0, -P2, -P5, -P10, -P15, and -P20. The genome of rFluMist/pH1N1-P2 was synthesized entirely from oligonucleotides, and specific mutations were introduced into the synthetic genome to generate the genomes for rFluMist-P0, -P5, -P10, -P15, and -P20. (B) Replication kinetics of recombinant rFluMist/pH1N1 variants at 33°C, 37°C, and 39°C. MDCK cells were infected at an MOI of 0.002 TCID50/cell, and the culture supernatants were collected at 24 h, 48 h, 72 h, and 96 h postinfection. The 0-h titer shown is the back titer of the dilution used to inoculate all replicates for each virus. Viral titers were determined by TCID50 assay at 33°C. Significant differences (*, P < 0.05) in viral titers compared to rFluMist-P0 are shown at select time points for select viruses. The error bars represent SD.
Phenotypic reversion was multimechanistic, with both additive and synergistic effects.
Since most of the mutations were in the PB2, PB1, PA, and NP genes, we were able to use a minigenome replication assay to sensitively assess the effects of specific mutations on polymerase activity at various temperatures (45). In transfected 293T cells, PB1-E51K, PB1-I171V, and PA-N350K dramatically increased the polymerase activity at 39°C, whereas the effects were less pronounced at 33°C and 37°C (Fig. 3). At all temperatures, NP-N125Y and NP-V186I had minimal effects on polymerase activity, and surprisingly, PA-L366I inhibited polymerase activity (Fig. 3).
FIG 3.
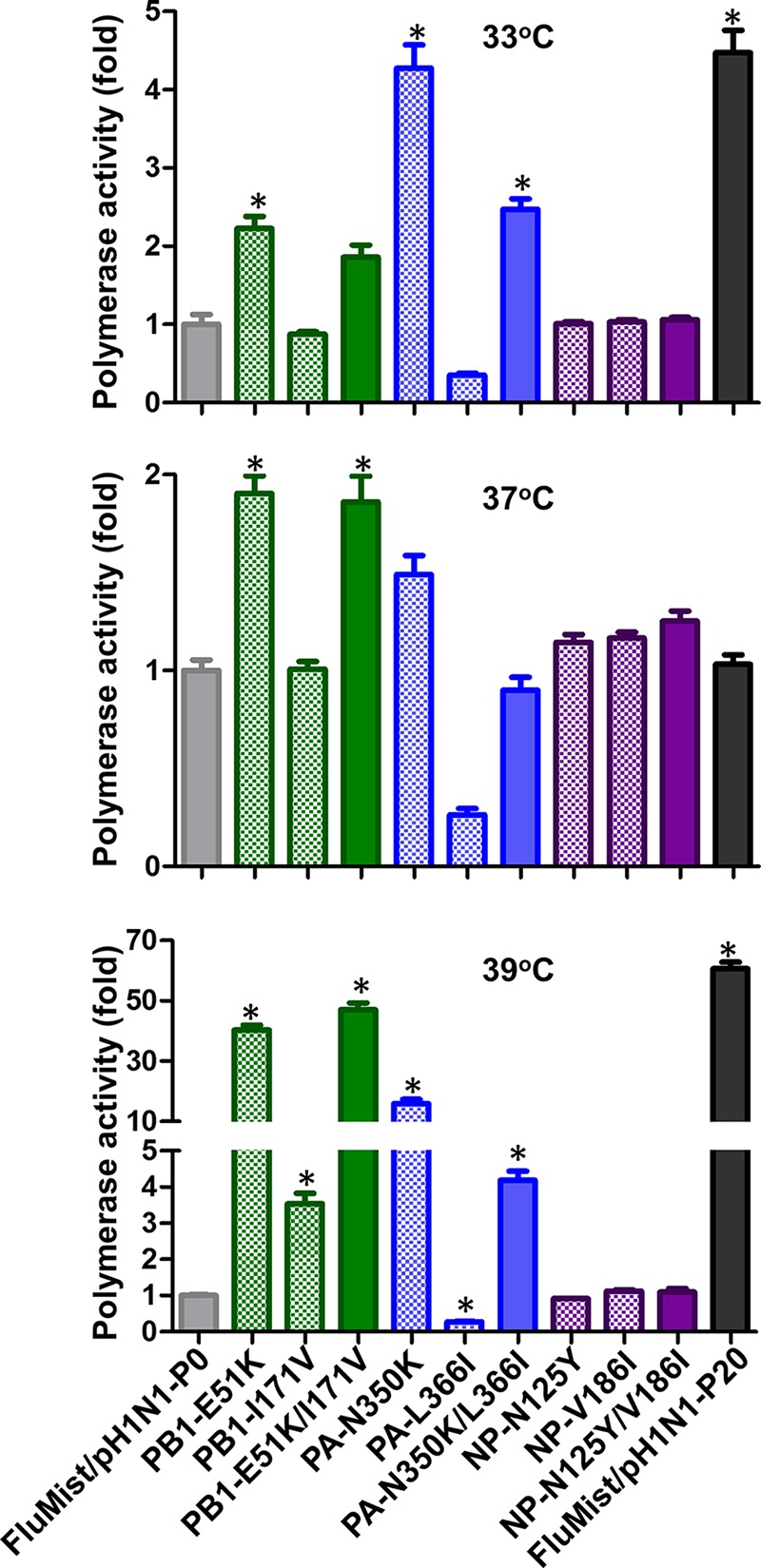
Effects of mutations on FluMist polymerase activity at 33°C, 37°C, and 39°C. A minigenome replication assay was performed by cotransfection of luciferase reporter plasmids and wild-type or mutant PB2, PB1, PA, and NP plasmids into 293T cells and incubation at the indicated temperatures. The luciferase activities were determined after 12 h, and the activities of mutants were expressed relative to the activity of the wild-type FluMist/pH1N1-P0 (1-fold). *, P < 0.001 compared to the polymerase activity of FluMist/pH1N1-P0. The error bars represent SD.
We then rescued rFluMist/pH1N1 viruses with various amino acid substitutions to determine the changes (Table 1) responsible for the phenotypic reversion. Interestingly, although PB1-E51K, PB1-I171V, and PA-N350K dramatically increased the polymerase activity at restrictive temperatures (Fig. 3), none of these substitutions alone had any detectable effects on the generation of progeny virus (Fig. 4). Even the combination of the PB1-E51K-I171V and PA-N350K substitutions was not sufficient to substantially overcome the ts phenotype at 39°C (Fig. 4). However, when NP-N125Y and NP-V186I were also added to the PB1 and PA substitutions, the recombinant virus was no longer ts (Fig. 4). The NP reversion substitutions (NP-N125Y and NP-V186I) in the absence of other substitutions did not show an effect on the ts phenotype (Fig. 4). This result clearly indicates a synergistic effect between the polymerase and the NP genes (e.g., Fig. 4, compare the replication of NPP20, PB1P20/PAP20, and PB1P20/PAP20/NPP20 viruses at 39°C). Taken together, the data indicate that the ts phenotypic reversion substitutions are both additive and synergistic and that viral replication at higher temperatures is accomplished by both the increased viral RNA polymerase activity (e.g., PB1 mutations) and mechanisms unrelated to polymerase activity (e.g., NP mutations).
FIG 4.
Effects of mutations on the replication of recombinant rFluMist/pH1N1 variants at 33°C, 37°C, and 39°C. MDCK cells were infected at an MOI of 0.002 TCID50/cell, and the culture supernatants were collected at 0, 2, 24, 48, 72, and 96 h postinoculation. Viral titers were determined by TCID50 assay at 33°C. The superscript P20 indicates the mutations found in P20. For instance, PB1P20 designates the virus that contains the PB1-E51K and PB1-I171V double mutation with all the other genes the same as in rFluMist/pH1N1-P0. PB1P20/PA-N350K/NPP20/NSP20 designates the virus that is the same as rFluMist/pH1N1-P0 except that it also contains PB1-E51K, PB1-I171V, PA-N350K, NP-N125Y, NP-V186I, and NS2-G63E mutations. All the replication kinetics assays were performed in one experiment so that the titers could be compared to each other directly. The viruses were separated into two groups at each temperature for clarity of the graphs.
Revertant viruses obtained increased virulence.
To determine whether the ts phenotypic reversion in vitro results in the reversion of the attenuation phenotype of FluMist/pH1N1 in vivo, the pathogenicities of selected recombinant caAA60 viruses were compared in 6-week-old BALB/cJ mice. While the two viruses had similar replication efficiencies in mouse nasal washes, rFluMist/pH1N1-P20 replicated to significantly higher titers than the parental rFluMist/pH1N1-P0 virus in mouse lungs, where the temperature is higher (Fig. 5A and B). Additionally, rFluMist/pH1N1-P20-infected mice had increased NP staining in their lungs compared to mice infected with the parental virus (Fig. 5C). In addition to increased viral replication in the lungs, rFluMist/pH1N1-P20-infected mice also showed significant weight loss (Fig. 5D). The disease severity (based on replication and weight loss) caused by rFluMist/pH1N1-P20 was similar to that caused by pH1N1 expressing the same HA and NA (Fig. 5).
FIG 5.
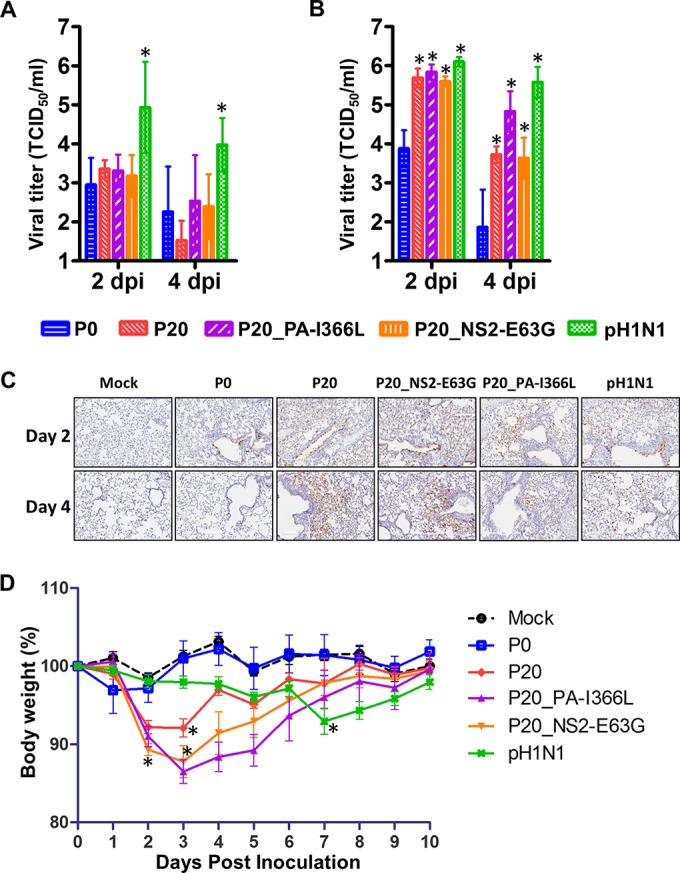
Replication and pathogenicity of rFluMist/pH1N1 and variants in mice. Six-week-old BALB/cJ mice were intranasally inoculated with 106 TCID50 of the indicated viruses. (A and B) Nasal washes (A) and lungs (B) were collected at 2 and 4 dpi, and viral titers were determined by TCID50 assay at 33°C. (C) IHC assays were performed on mouse lungs. (D) Mouse weights were recorded daily through 10 dpi. The weights on each day were expressed as percentages of the weights at 0 dpi (100%). P0, rFluMist/pH1N1-P0; P20, rFluMist/pH1N1-P20. P20_PA-I366L is the same as P20 except that it does not contain the PA-L366I mutation; P20_NS2-E63G is the same as P20, except that it does not contain the NS2-G63E mutation; pH1N1 is a recombinant 2009 H1N1 pandemic strain A/New York/1682/2009 whose HA and NA are replaced with those from the FluMist vaccine used in this study (A/CA/07/2009 with mutations). Significant differences (*, P < 0.05) in viral titers compared to rFluMist/pH1N1-P0 are shown in panels A and B, and the first day showing a significant difference (*, P < 0.05) in weight loss compared to rFluMist/pH1N1-P0 is shown in panel D. The error bars represent SD.
The PA-L366I mutation exists in the FluMist/pH1N1-P2 population but does not exist in the caAA60 GenBank reference sequence. It inhibited polymerase activity (Fig. 3) and reduced virus replication (Fig. 4). To examine the influence of PA-L366I on the attenuation of FluMist/pH1N1 in vivo, we introduced the PA-I366L substitution into the rFluMist/pH1N1-P20 virus, and the resultant virus (rFluMist/pH1N1-P20_PA-I366L) replicated more efficiently in mouse lungs and caused greater weight loss than rFluMist/pH1N1-P20 (Fig. 5). In total, these results suggest that the PA-L366I mutation may be an inhibitory mutation at higher temperatures and is unlikely to contribute to the phenotypic reversion demonstrated by FluMist/pH1N1-P20.
The mouse model also allowed us to determine that the NS2-G63E mutation does not contribute to the increased virulence of rFluMist/pH1N1-P20. When we introduced NS2-E63G into the rFluMist/pH1N1-P20 virus, the resultant rFluMist/pH1N1-P20_NS2-E63G virus showed a level of virulence similar to that of the rFluMist/pH1N1-P20 virus (Fig. 5).
DISCUSSION
Although many preclinical and clinical studies have proven that the caAA60 backbone of FluMist influenza A vaccines is phenotypically very stable, our study demonstrated that the caAA60 vRNA backbone can still undergo phenotypic reversion to generate a virus that can replicate at high temperature and is no longer attenuated in mice. To understand the molecular mechanisms of the reversion, we used NGS to analyze different passages of FluMist/pH1N1, which illustrated the dynamics of the emergence of mutations and characterized the roles specific substitutions play in the phenotypic reversion of the caAA60 backbone of FluMist influenza A virus vaccines. Many interesting questions arise from this study, and more in-depth analyses of other FluMist vaccine strains and their revertants in future studies are likely to provide more insights into the basic mechanisms of virus attenuation and reversion.
Multiple mutations emerged in the cold adaptation of wild-type AA60 to caAA60 (26), and therefore, it is not surprising that multiple mutations also emerged during the reversion of the ts phenotype of FluMist/pH1N1 (Table 1). What is surprising is that none of the new substitutions are genetic reversions that occur at the preexisting caAA60 mutation loci, illustrating the large genetic flexibility and various strategies that influenza viruses use to adapt to a new environment.
Previous studies suggested that the ca, ts, and att phenotypes are determined by sets of different but overlapping amino acid substitutions. Our study shows that the mutations responsible for the reversion of ts phenotype are also sufficient to revert the att phenotype of FluMist/pH1N1 in mice, resulting in lung viral titers and body weight loss similar to that caused by a pandemic H1N1 virus expressing the same HA and NA (Fig. 5). Interestingly, unlike most of the ts mutations that increased polymerase activity at elevated temperatures, the two residue changes in NP did not affect the viral RNA polymerase activity at any of the temperatures tested (Fig. 3), suggesting that multiple genes with different mechanisms relevant to polymerase activity (e.g., PB1 mutations) or irrelevant to polymerase activity (e.g., NP mutations) acted additively and synergistically to revert the ts and att phenotype of FluMist/pH1N1 to that of a wild-type virus. For example, the FluMist-P5 virus with the PA-N350K and NP-N125Y mutations replicated to moderate titers at 39°C (Fig. 2), but the rFluMist/pH1N1 viruses with only one of the mutations were completely inhibited at 39°C (Fig. 4, viruses PA-N350K and NP-N125Y). In addition, we speculate that both the NP-N125Y and -V186I changes are beneficial to the ts and att phenotypic reversion, because rFluMist/pH1N1 expressing both changes replicated a little better than viruses with individual NP changes (Fig. 4, compare NP-N125Y, NP-V186I, and NPP20).
The FluMist/pH1N1 P0 stock was not available for sequencing, so we compared the P2 sequence to the caAA60 sequences retrieved from GenBank and detected the PA-L366I mutation. We originally assumed the PA-L366I mutation emerged in the P0 to P2 passages. However, the PA-L366I mutation appears to be inhibitory to the virus at all temperatures in vitro (Fig. 3) and restrictive to the virus in vivo (Fig. 5B and D). Although the effect is not significant in a comparison of P0 and P2, both of which are severely ts and att, it is more obvious in viruses that have already reverted the ts phenotype (e.g., Fig. 4, compare PB1P20/PA-N350K/NPP20/NSP20 and PB1P20/PAP20/NPP20/NSP20 at 39°C). Therefore, we speculated that PA-L366I may also exist in the FluMist/pH1N1 aliquot (P0) distributed for vaccination. To confirm this, we used Illumina MiSeq to sequence an unpassaged trivalent FluMist vaccine of the 2010-2011 influenza season, in which the H1N1 vaccine strain is the same as the pH1N1 monovalent vaccine used for the current study (A/California/7/2009). Interestingly, PA-L366 (44%) and PA-I366 (56%) coexisted in that stock. The PA-L366I substitution seen in the 2009-2010 and 2010-2011 FluMist vaccines may have existed in the master donor strain plasmids used for generation of the reassortment seed virus or may have occurred in the manufacturing process (40). In any case, five amino acid substitutions (PB1-E51K, PB1-I171V, PA-N350K, NP-N125Y, and/or NP-V186I) are sufficient to revert the ts and att phenotypes of FluMist/pH1N1.
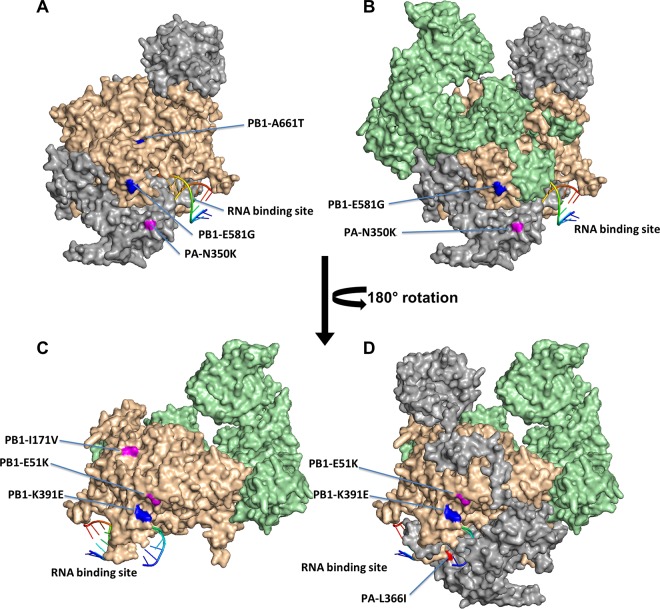
We mapped polymerase mutations onto the PDB ID 4WSB crystal structure (Fig. 6) and NP substitutions onto PDB ID 3RO5 (not shown). All of the amino acid substitutions from the FluMist revertant, except for NP-I186, are on the surfaces of the protein subunits (PB1-K51 and -V171, PA-K350 and -I366, and NP-Y125). Intriguingly, PB1-171V is in the interface between the PB1 and PA subunits, and this position may have a role in intermolecular interaction and/or polymerase activity. The original temperature-sensitive mutation PB1-A661T appears to be in a region where PB1 and PB2 interact. While the temperature-sensitive PB1-K391E substitution and the temperature-permissive PB1-E51K are far apart in the linear sequence, they appear to be proximal in the protein structure (Fig. 6). Furthermore, there is a basic (K) to an acidic (E) residue change in the original ts virus, whereas the revertant displays an acidic (E)-to-basic (K) substitution in this region, which suggests that the region may be involved in interactions with other viral or host proteins. The potential roles of these reversion substitutions are elusive, and their discovery is further complicated by the lack of high-resolution structures depicting the interactions between the polymerase and NP proteins. For instance, the PA-N350K and NP-N125Y mutations are the two earliest mutations that emerged in the adaptation (Table 1, P5), and they may interact directly or indirectly to affect the polymerase activity and virus replication.
FIG 6.
Locations of temperature-sensitive and permissive mutations in the polymerase structure. Selected temperature-sensitive mutations in the caAA60 virus (blue residues) and the temperature-permissive mutations in the FluMist revertant from this study (magenta residues) were mapped to the structure PDB ID 4WSB. The polymerase subunit PA is shown in gray, PB1 in light brown, and PB2 in light green. (A) PA and PB1. (B) PA, PB1, and PB2. (C) PB1 and PB2. (D) PA, PB1, and PB2 rotated 180o compared to the structure in panel B. The mapped structures were visualized and generated in PyMOL.
In conclusion, this study proved that the widely used live attenuated influenza A virus vaccine backbone in FluMist has the potential to become a virulent virus under specific conditions. Although under current recommendations infants and immunocompromised individuals should not take the vaccine, it may be administered to immunocompromised individuals who have not yet been diagnosed. In such an unusual scenario, the caAA60 backbone in FluMist could undergo prolonged replication in the individual to accumulate substitutions leading to increased replication and shedding (55, 56), which could lead to transmission to another person and further selection. Therefore, the phenotypic and genetic stability of LAIVs during and after massive vaccination should be closely monitored to ensure vaccine safety. Meanwhile, there are many strategies to further improve the safety of LAIVs, and research on this front is very important. For instance, additional ts mutations identified in other studies can be incorporated into the LAIVs (45); non-ts but att mutations, such as NS1 truncations (actually, PA-L366I may also fall into this category), can also be combined with the ts mutations to create additional layers of safety.
ACKNOWLEDGMENTS
We thank James Stevens for mapping the mutations to the crystal structures and helping in interpretation of the data.
The opinions expressed in this article are our own and do not reflect the views of the Centers for Disease Control and Prevention, the Department of Health and Human Services, or the United States government.
Funding Statement
The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
REFERENCES
- 1.WHO. 2009. World Health Organization: Influenza (seasonal) fact sheet 211. http://www.who.int/mediacentre/factsheets/fs211/en/.
- 2.Centers for Disease Control and Prevention. 2013. Estimated influenza illnesses and hospitalizations averted by influenza vaccination—United States, 2012-13 influenza season. MMWR Morb Mortal Wkly Rep 62:997–1000. [PMC free article] [PubMed] [Google Scholar]
- 3.Hannoun C. 2013. The evolving history of influenza viruses and influenza vaccines. Expert Rev Vaccines 12:1085–1094. doi: 10.1586/14760584.2013.824709. [DOI] [PubMed] [Google Scholar]
- 4.Clements ML, Betts RF, Murphy BR. 1984. Advantage of live attenuated cold-adapted influenza A virus over inactivated vaccine for A/Washington/80 (H3N2) wild-type virus infection. Lancet i:705–708. [DOI] [PubMed] [Google Scholar]
- 5.Rhorer J, Ambrose CS, Dickinson S, Hamilton H, Oleka NA, Malinoski FJ, Wittes J. 2009. Efficacy of live attenuated influenza vaccine in children: a meta-analysis of nine randomized clinical trials. Vaccine 27:1101–1110. doi: 10.1016/j.vaccine.2008.11.093. [DOI] [PubMed] [Google Scholar]
- 6.Ashkenazi S, Vertruyen A, Aristegui J, Esposito S, McKeith DD, Klemola T, Biolek J, Kuhr J, Bujnowski T, Desgrandchamps D, Cheng SM, Skinner J, Gruber WC, Forrest BD, CAIV-T Study Group. 2006. Superior relative efficacy of live attenuated influenza vaccine compared with inactivated influenza vaccine in young children with recurrent respiratory tract infections. Pediatr Infect Dis J 25:870–879. doi: 10.1097/01.inf.0000237829.66310.85. [DOI] [PubMed] [Google Scholar]
- 7.Belshe RB, Edwards KM, Vesikari T, Black SV, Walker RE, Hultquist M, Kemble G, Connor EM, CAIV-T Comparative Efficacy Study Group. 2007. Live attenuated versus inactivated influenza vaccine in infants and young children. N Engl J Med 356:685–696. doi: 10.1056/NEJMoa065368. [DOI] [PubMed] [Google Scholar]
- 8.Luce BR, Nichol KL, Belshe RB, Frick KD, Li SX, Boscoe A, Rousculp MD, Mahadevia PJ. 2008. Cost-effectiveness of live attenuated influenza vaccine versus inactivated influenza vaccine among children aged 24-59 months in the United States. Vaccine 26:2841–2848. doi: 10.1016/j.vaccine.2008.03.046. [DOI] [PubMed] [Google Scholar]
- 9.Ambrose CS, Levin MJ, Belshe RB. 2011. The relative efficacy of trivalent live attenuated and inactivated influenza vaccines in children and adults. Influenza Other Respir Viruses 5:67–75. doi: 10.1111/j.1750-2659.2010.00183.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Falkenhorst G, Harder T, Remschmidt C, Terhardt M, Zepp F, Ledig T, Wicker S, Keller-Stanislawski B, Mertens T. 2013. Background paper to the recommendation for the preferential use of live-attenuated influenza vaccine in children aged 2-6 years in Germany. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 56:1557–1564. doi: 10.1007/s00103-013-1844-9. [DOI] [PubMed] [Google Scholar]
- 11.Carter NJ, Curran MP. 2011. Live attenuated influenza vaccine (FluMist(R); Fluenz): a review of its use in the prevention of seasonal influenza in children and adults. Drugs 71:1591–1622. doi: 10.2165/11206860-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 12.Ambrose CS, Wu X, Knuf M, Wutzler P. 2012. The efficacy of intranasal live attenuated influenza vaccine in children 2 through 17 years of age: a meta-analysis of 8 randomized controlled studies. Vaccine 30:886–892. doi: 10.1016/j.vaccine.2011.11.104. [DOI] [PubMed] [Google Scholar]
- 13.Hoft DF, Babusis E, Worku S, Spencer CT, Lottenbach K, Truscott SM, Abate G, Sakala IG, Edwards KM, Creech CB, Gerber MA, Bernstein DI, Newman F, Graham I, Anderson EL, Belshe RB. 2011. Live and inactivated influenza vaccines induce similar humoral responses, but only live vaccines induce diverse T-cell responses in young children. J Infect Dis 204:845–853. doi: 10.1093/infdis/jir436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cox RJ, Brokstad KA, Ogra P. 2004. Influenza virus: immunity and vaccination strategies. Comparison of the immune response to inactivated and live, attenuated influenza vaccines. Scand J Immunol 59:1–15. [DOI] [PubMed] [Google Scholar]
- 15.Zhu W, Higgs BW, Morehouse C, Streicher K, Ambrose CS, Woo J, Kemble GW, Jallal B, Yao Y. 2010. A whole genome transcriptional analysis of the early immune response induced by live attenuated and inactivated influenza vaccines in young children. Vaccine 28:2865–2876. doi: 10.1016/j.vaccine.2010.01.060. [DOI] [PubMed] [Google Scholar]
- 16.Johnson PR Jr, Feldman S, Thompson JM, Mahoney JD, Wright PF. 1985. Comparison of long-term systemic and secretory antibody responses in children given live, attenuated, or inactivated influenza A vaccine. J Med Virol 17:325–335. doi: 10.1002/jmv.1890170405. [DOI] [PubMed] [Google Scholar]
- 17.Sasaki S, He XS, Holmes TH, Dekker CL, Kemble GW, Arvin AM, Greenberg HB. 2008. Influence of prior influenza vaccination on antibody and B-cell responses. PLoS One 3:e2975. doi: 10.1371/journal.pone.0002975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gorse GJ, Belshe RB. 1990. Enhancement of anti-influenza A virus cytotoxicity following influenza A virus vaccination in older, chronically ill adults. J Clin Microbiol 28:2539–2550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cheng X, Zengel JR, Suguitan AL Jr, Xu Q, Wang W, Lin J, Jin H. 2013. Evaluation of the humoral and cellular immune responses elicited by the live attenuated and inactivated influenza vaccines and their roles in heterologous protection in ferrets. J Infect Dis 208:594–602. doi: 10.1093/infdis/jit207. [DOI] [PubMed] [Google Scholar]
- 20.Maassab HF, Bryant ML. 1999. The development of live attenuated cold-adapted influenza virus vaccine for humans. Rev Med Virol 9:237–244. doi:. [DOI] [PubMed] [Google Scholar]
- 21.Murphy BR, Coelingh K. 2002. Principles underlying the development and use of live attenuated cold-adapted influenza A and B virus vaccines. Viral Immunol 15:295–323. doi: 10.1089/08828240260066242. [DOI] [PubMed] [Google Scholar]
- 22.Maassab HF. 1967. Adaptation and growth characteristics of influenza virus at 25°C. Nature 213:612–614. doi: 10.1038/213612a0. [DOI] [PubMed] [Google Scholar]
- 23.Snyder MH, Clements ML, De Borde D, Maassab HF, Murphy BR. 1985. Attenuation of wild-type human influenza A virus by acquisition of the PA polymerase and matrix protein genes of influenza A/Ann Arbor/6/60 cold-adapted donor virus. J Clin Microbiol 22:719–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Snyder MH, Betts RF, DeBorde D, Tierney EL, Clements ML, Herrington D, Sears SD, Dolin R, Maassab HF, Murphy BR. 1988. Four viral genes independently contribute to attenuation of live influenza A/Ann Arbor/6/60 (H2N2) cold-adapted reassortant virus vaccines. J Virol 62:488–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Subbarao EK, Perkins M, Treanor JJ, Murphy BR. 1992. The attenuation phenotype conferred by the M gene of the influenza A/Ann Arbor/6/60 cold-adapted virus (H2N2) on the A/Korea/82 (H3N2) reassortant virus results from a gene constellation effect. Virus Res 25:37–50. doi: 10.1016/0168-1702(92)90098-T. [DOI] [PubMed] [Google Scholar]
- 26.Cox NJ, Kitame F, Kendal AP, Maassab HF, Naeve C. 1988. Identification of sequence changes in the cold-adapted, live attenuated influenza vaccine strain, A/Ann Arbor/6/60 (H2N2). Virology 167:554–567. [PubMed] [Google Scholar]
- 27.Jin H, Lu B, Zhou H, Ma C, Zhao J, Yang CF, Kemble G, Greenberg H. 2003. Multiple amino acid residues confer temperature sensitivity to human influenza virus vaccine strains (FluMist) derived from cold-adapted A/Ann Arbor/6/60. Virology 306:18–24. doi: 10.1016/S0042-6822(02)00035-1. [DOI] [PubMed] [Google Scholar]
- 28.Jin H, Zhou H, Lu B, Kemble G. 2004. Imparting temperature sensitivity and attenuation in ferrets to A/Puerto Rico/8/34 influenza virus by transferring the genetic signature for temperature sensitivity from cold-adapted A/Ann Arbor/6/60. J Virol 78:995–998. doi: 10.1128/JVI.78.2.995-998.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mostow SR, Hopkins JA, Wright PF. 1979. Behavior of vaccine revertants of temperature-sensitive mutants of influenza virus in ferret tracheal organ culture. Infect Immun 26:193–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Murphy BR, Markoff LJ, Hosier NT, Massicot JG, Chanock RM. 1982. Production and level of genetic stability of an influenza A virus temperature-sensitive mutant containing two genes with ts mutations. Infect Immun 37:235–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tolpin MD, Clements ML, Levine MM, Black RE, Saah AJ, Anthony WC, Cisneros L, Chanock RM, Murphy BR. 1982. Evaluation of a phenotypic revertant of the A/Alaska/77-ts-1A2 reassortant virus in hamsters and in seronegative adult volunteers: further evidence that the temperature-sensitive phenotype is responsible for attenuation of ts-1A2 reassortant viruses. Infect Immun 36:645–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Scholtissek C, Rott R. 1984. Correlation between loss of the temperature-sensitive phenotype and pathogenicity of fowl plague virus mutants in the chicken. Virus Res 1:117–131. doi: 10.1016/0168-1702(84)90068-6. [DOI] [PubMed] [Google Scholar]
- 33.Donabedian AM, DeBorde DC, Cook S, Smitka CW, Maassab HF. 1988. A mutation in the PA protein gene of cold-adapted B/Ann Arbor/1/66 influenza virus associated with reversion of temperature sensitivity and attenuated virulence. Virology 163:444–451. doi: 10.1016/0042-6822(88)90285-1. [DOI] [PubMed] [Google Scholar]
- 34.Mandler J, Muller K, Scholtissek C. 1991. Mutants and revertants of an avian influenza A virus with temperature-sensitive defects in the nucleoprotein and PB2. Virology 181:512–519. doi: 10.1016/0042-6822(91)90883-D. [DOI] [PubMed] [Google Scholar]
- 35.Treanor JJ, Buja R, Murphy BR. 1991. Intragenic suppression of a deletion mutation of the nonstructural gene of an influenza A virus. J Virol 65:4204–4210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Treanor J, Perkins M, Battaglia R, Murphy BR. 1994. Evaluation of the genetic stability of the temperature-sensitive PB2 gene mutation of the influenza A/Ann Arbor/6/60 cold-adapted vaccine virus. J Virol 68:7684–7688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Murphy BR, Park EJ, Gottlieb P, Subbarao K. 1997. An influenza A live attenuated reassortant virus possessing three temperature-sensitive mutations in the PB2 polymerase gene rapidly loses temperature sensitivity following replication in hamsters. Vaccine 15:1372–1378. doi: 10.1016/S0264-410X(97)00031-5. [DOI] [PubMed] [Google Scholar]
- 38.Parkin NT, Chiu P, Coelingh K. 1997. Genetically engineered live attenuated influenza A virus vaccine candidates. J Virol 71:2772–2778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Da Costa B, Sausset A, Munier S, Ghounaris A, Naffakh N, Le Goffic R, Delmas B. 2015. Temperature-sensitive mutants in the influenza A virus RNA polymerase: alterations in the PA linker reduce nuclear targeting of the PB1-PA dimer and result in viral attenuation. J Virol 89:6376–6390. doi: 10.1128/JVI.00589-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Buonagurio DA, Bechert TM, Yang CF, Shutyak L, D'Arco GA, Kazachkov Y, Wang HP, Rojas EA, O'Neill RE, Spaete RR, Coelingh KL, Zamb TJ, Sidhu MS, Udem SA. 2006. Genetic stability of live, cold-adapted influenza virus components of the FluMist/CAIV-T vaccine throughout the manufacturing process. Vaccine 24:2151–2160. doi: 10.1016/j.vaccine.2005.11.007. [DOI] [PubMed] [Google Scholar]
- 41.Buonagurio DA, O'Neill RE, Shutyak L, D'Arco GA, Bechert TM, Kazachkov Y, Wang HP, DeStefano J, Coelingh KL, August M, Parks CL, Zamb TJ, Sidhu MS, Udem SA. 2006. Genetic and phenotypic stability of cold-adapted influenza viruses in a trivalent vaccine administered to children in a day care setting. Virology 347:296–306. doi: 10.1016/j.virol.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 42.Block SL, Yogev R, Hayden FG, Ambrose CS, Zeng W, Walker RE. 2008. Shedding and immunogenicity of live attenuated influenza vaccine virus in subjects 5-49 years of age. Vaccine 26:4940–4946. doi: 10.1016/j.vaccine.2008.07.013. [DOI] [PubMed] [Google Scholar]
- 43.Hammitt LL, Bartlett JP, Li S, Rahkola J, Lang N, Janoff EN, Levin MJ, Weinberg A. 2009. Kinetics of viral shedding and immune responses in adults following administration of cold-adapted influenza vaccine. Vaccine 27:7359–7366. doi: 10.1016/j.vaccine.2009.09.041. [DOI] [PubMed] [Google Scholar]
- 44.Mallory RM, Yi T, Ambrose CS. 2011. Shedding of Ann Arbor strain live attenuated influenza vaccine virus in children 6-59 months of age. Vaccine 29:4322–4327. doi: 10.1016/j.vaccine.2011.04.022. [DOI] [PubMed] [Google Scholar]
- 45.Zhou B, Li Y, Speer SD, Subba A, Lin X, Wentworth DE. 2012. Engineering temperature sensitive live attenuated influenza vaccines from emerging viruses. Vaccine 30:3691–3702. doi: 10.1016/j.vaccine.2012.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhou B, Donnelly ME, Scholes DT, St George K, Hatta M, Kawaoka Y, Wentworth DE. 2009. Single-reaction genomic amplification accelerates sequencing and vaccine production for classical and swine origin human influenza A viruses. J Virol 83:10309–10313. doi: 10.1128/JVI.01109-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhou B, Lin X, Wang W, Halpin RA, Bera J, Stockwell TB, Barr IG, Wentworth DE. 2014. Universal influenza B virus genomic amplification facilitates sequencing, diagnostics, and reverse genetics. J Clin Microbiol 52:1330–1337. doi: 10.1128/JCM.03265-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Liu Q, Zhou B, Ma W, Bawa B, Ma J, Wang W, Lang Y, Lyoo Y, Halpin RA, Lin X, Stockwell TB, Webby R, Wentworth DE, Richt JA. 2014. Analysis of recombinant H7N9 wild-type and mutant viruses in pigs shows that the Q226L mutation in HA is important for transmission. J Virol 88:8153–8165. doi: 10.1128/JVI.00894-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhou B, Ma J, Liu Q, Bawa B, Wang W, Shabman RS, Duff M, Lee J, Lang Y, Cao N, Nagy A, Lin X, Stockwell TB, Richt JA, Wentworth DE, Ma W. 2014. Characterization of uncultivable bat influenza virus using a replicative synthetic Virus. PLoS Pathog 10:e1004420. doi: 10.1371/journal.ppat.1004420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhou B, Wentworth DE. 2012. Influenza A virus molecular virology techniques. Methods Mol Biol 865:175–192. doi: 10.1007/978-1-61779-621-0_11. [DOI] [PubMed] [Google Scholar]
- 51.Zhou B, Li Y, Halpin R, Hine E, Spiro DJ, Wentworth DE. 2011. PB2 residue 158 is a pathogenic determinant of pandemic H1N1 and H5 influenza A viruses in mice. J Virol 85:357–365. doi: 10.1128/JVI.01694-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhou B, Li Y, Belser JA, Pearce MB, Schmolke M, Subba AX, Shi Z, Zaki SR, Blau DM, Garcia-Sastre A, Tumpey TM, Wentworth DE. 2010. NS-based live attenuated H1N1 pandemic vaccines protect mice and ferrets. Vaccine 28:8015–8025. doi: 10.1016/j.vaccine.2010.08.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chen Z, Wang W, Zhou H, Suguitan AL Jr, Shambaugh C, Kim L, Zhao J, Kemble G, Jin H. 2010. Generation of live attenuated novel influenza virus A/California/7/09 (H1N1) vaccines with high yield in embryonated chicken eggs. J Virol 84:44–51. doi: 10.1128/JVI.02106-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dormitzer PR, Suphaphiphat P, Gibson DG, Wentworth DE, Stockwell TB, Algire MA, Alperovich N, Barro M, Brown DM, Craig S, Dattilo BM, Denisova EA, De Souza I, Eickmann M, Dugan VG, Ferrari A, Gomila RC, Han L, Judge C, Mane S, Matrosovich M, Merryman C, Palladino G, Palmer GA, Spencer T, Strecker T, Trusheim H, Uhlendorff J, Wen Y, Yee AC, Zaveri J, Zhou B, Becker S, Donabedian A, Mason PW, Glass JI, Rappuoli R, Venter JC. 2013. Synthetic generation of influenza vaccine viruses for rapid response to pandemics. Sci Transl Med 5:185ra68. doi: 10.1126/scitranslmed.3006368. [DOI] [PubMed] [Google Scholar]
- 55.Memoli MJ, Hrabal RJ, Hassantoufighi A, Jagger BW, Sheng ZM, Eichelberger MC, Taubenberger JK. 2010. Rapid selection of a transmissible multidrug-resistant influenza A/H3N2 virus in an immunocompromised host. J Infect Dis 201:1397–1403. doi: 10.1086/651610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ghedin E, Laplante J, DePasse J, Wentworth DE, Santos RP, Lepow ML, Porter J, Stellrecht K, Lin X, Operario D, Griesemer S, Fitch A, Halpin RA, Stockwell TB, Spiro DJ, Holmes EC, St George K. 2011. Deep sequencing reveals mixed infection with 2009 pandemic influenza A (H1N1) virus strains and the emergence of oseltamivir resistance. J Infect Dis 203:168–174. doi: 10.1093/infdis/jiq040. [DOI] [PMC free article] [PubMed] [Google Scholar]