Abstract
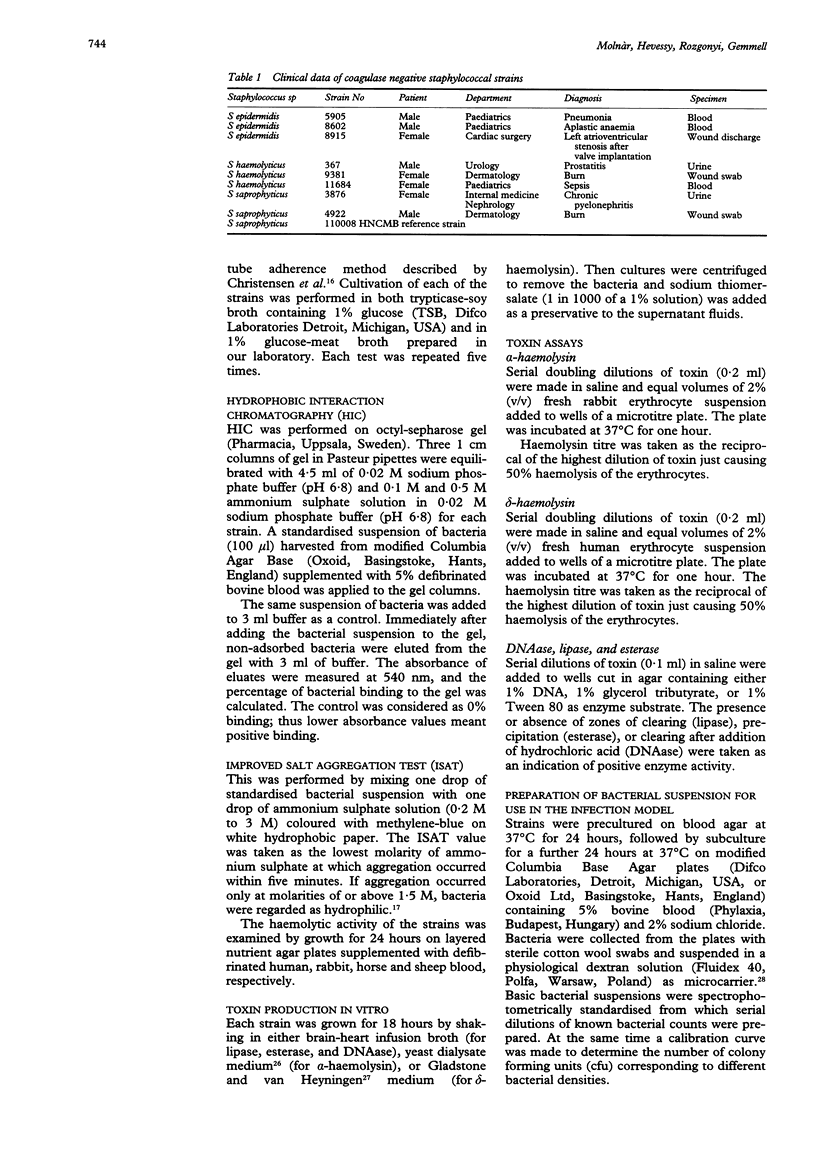
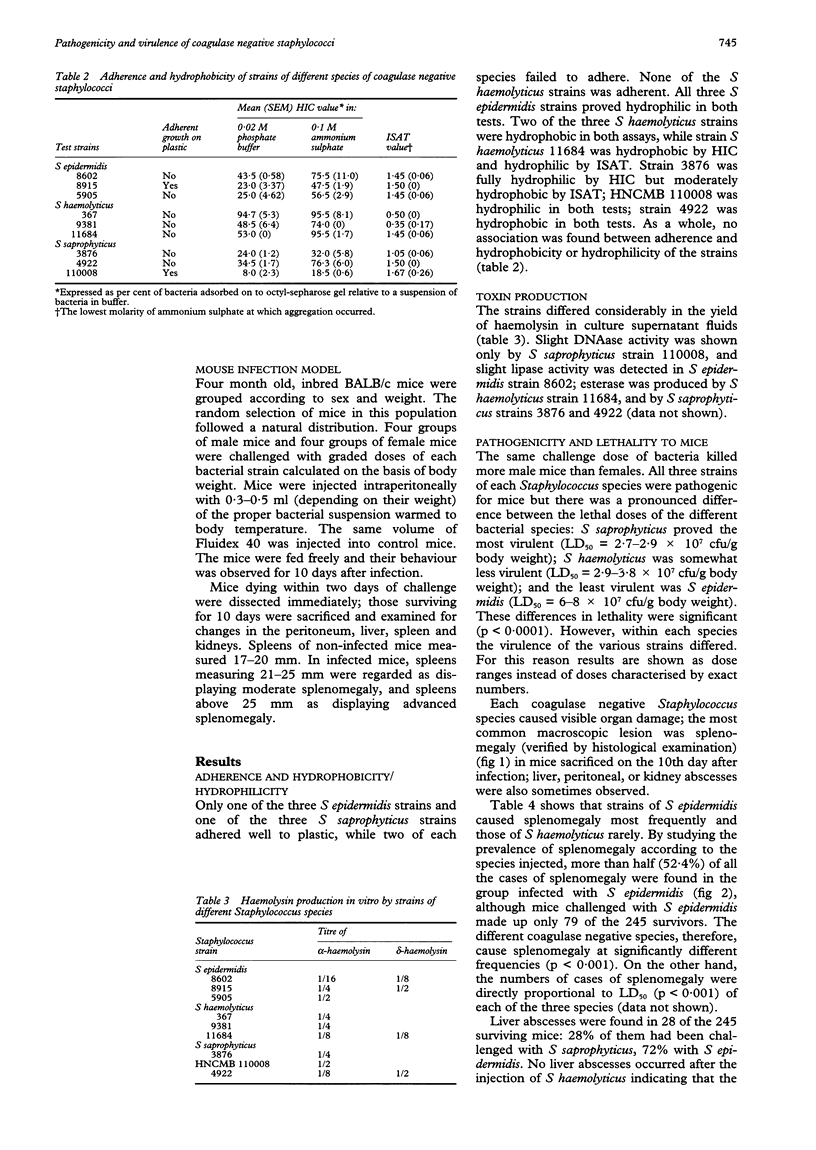
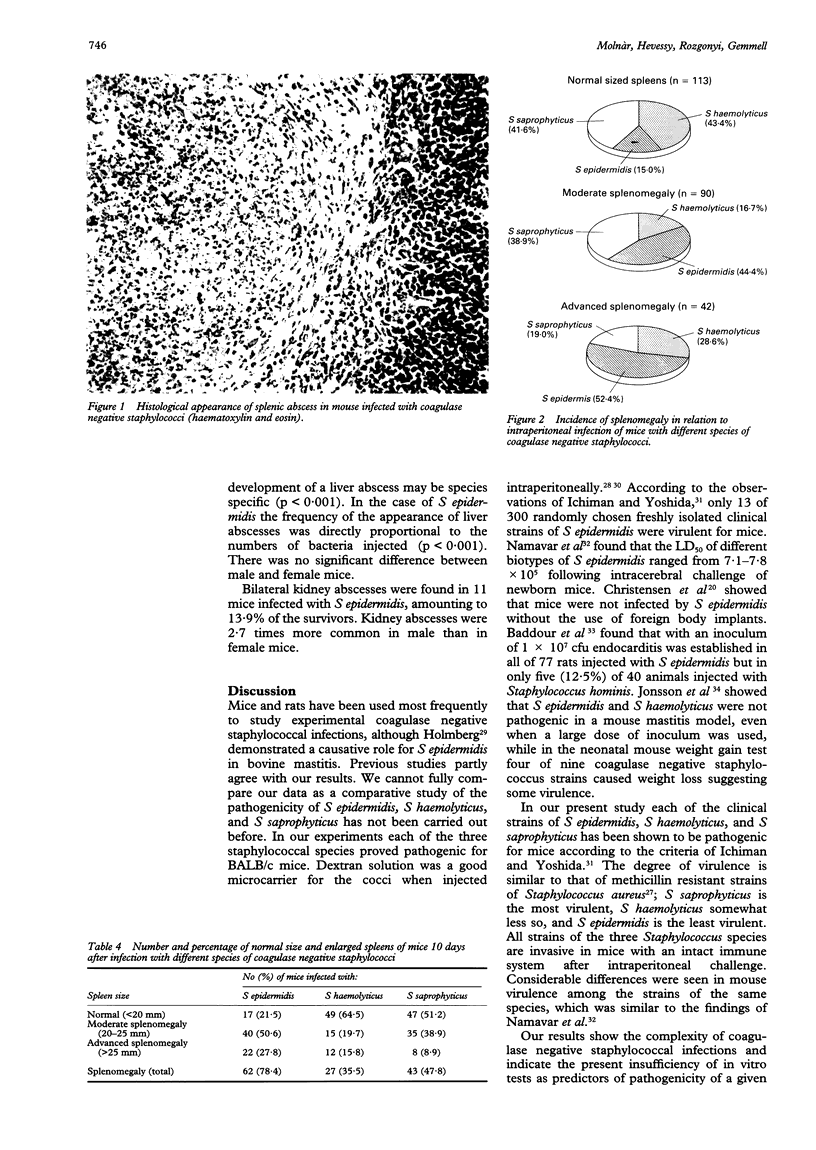
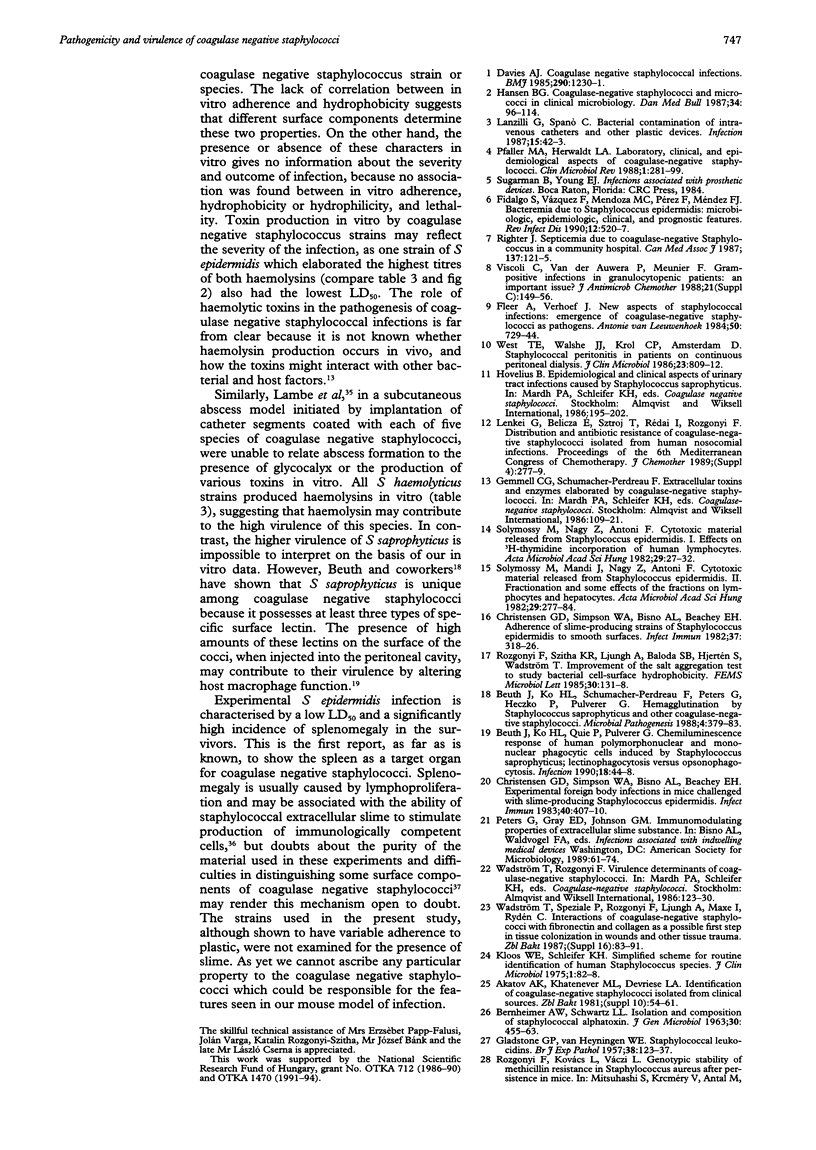
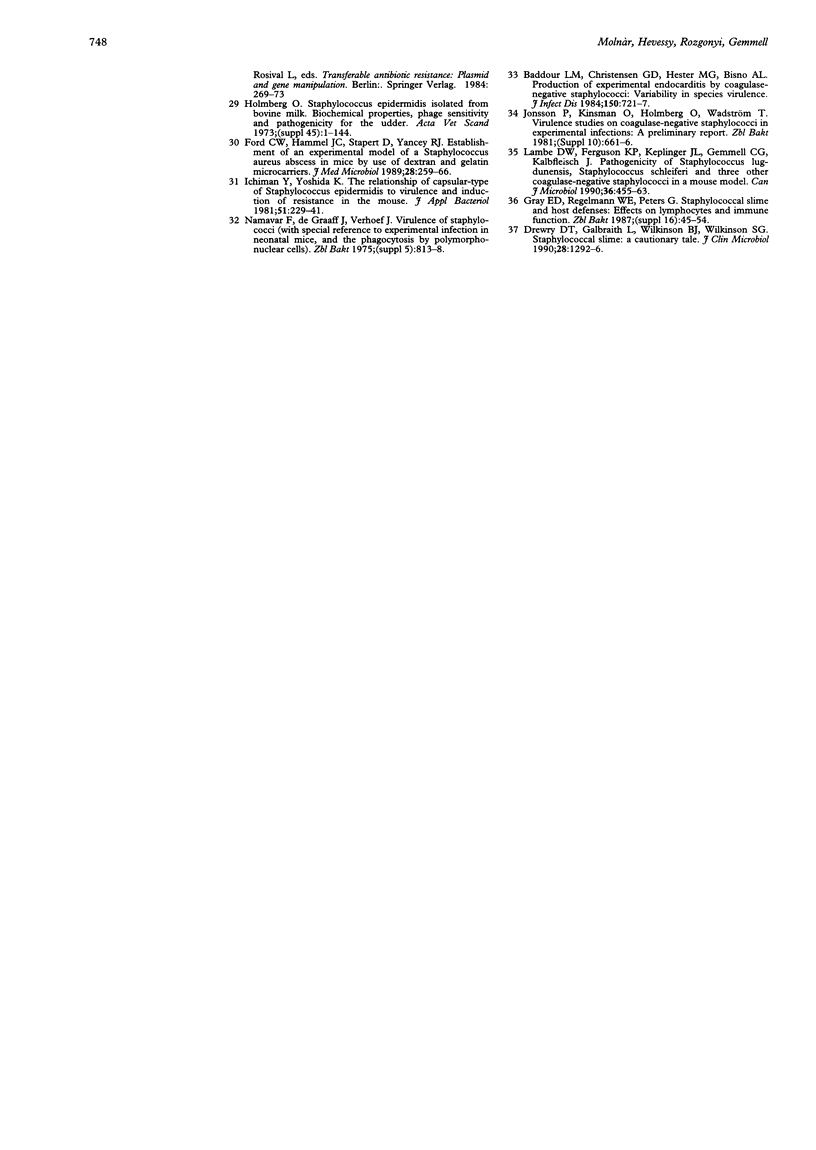
AIMS--To study the pathogenicity and virulence characteristics of Staphylococcus epidermidis, Staphylococcus haemolyticus, and Staphylococcus sapro-phyticus. METHODS--BALB/c mice were challenged intraperitoneally with graded doses of three strains belonging to each species. LD50s were measured for each strain. Haemolysin (alpha- and delta-) and enzyme (DNAase, lipase, and esterase) production in vitro were measured qualitatively and quantitatively. Adhesion to plastic was measured and related to cell surface hydrophobicity among the strains. RESULTS--S saprophyticus proved the most virulent (LD50 = 2.7-2.9 x 10(7) cfu/g body weight) while S epidermidis was the least virulent (LD50 = 6-8 x 10(7) cfu/g body weight). An enlarged spleen was the most common macroscopic pathological feature. Kidney, liver, and more rarely peritoneal abscesses were also seen in the infected animals. No direct correlation was found between adherence in vitro, cell surface hydrophobicity, or toxin/enzyme biosynthesis and virulence in mice. CONCLUSION--The results show that coagulase negative staphylococci are pathogenic in BALB/c mice. It is clear that these bacteria can cause invasive disease. However, the in vitro characteristics of coagulase negative staphylococci are not related to the pathogenicity of the organisms in mice.
Full text
PDF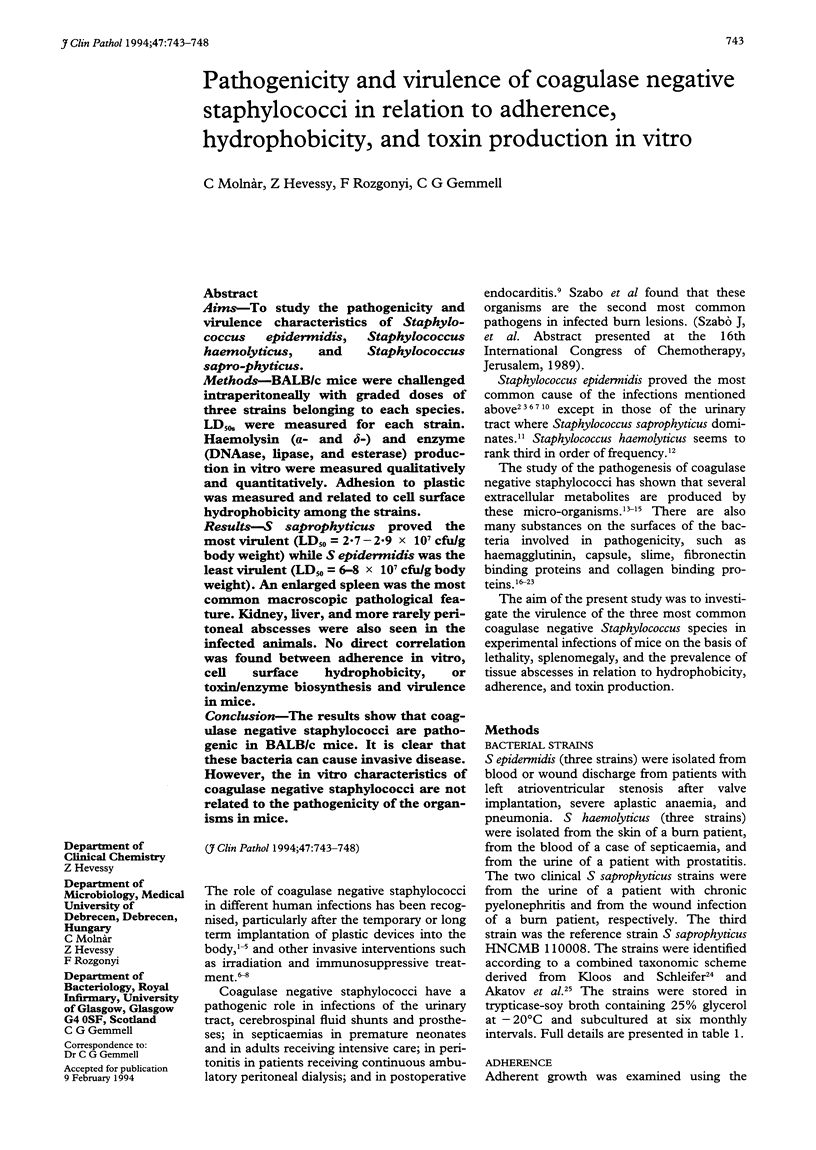
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BERNHEIMER A. W., SCHWARTZ L. L. Isolation and composition of staphylococcal alpha toxin. J Gen Microbiol. 1963 Mar;30:455–468. doi: 10.1099/00221287-30-3-455. [DOI] [PubMed] [Google Scholar]
- Baddour L. M., Christensen G. D., Hester M. G., Bisno A. L. Production of experimental endocarditis by coagulase-negative staphylococci: variability in species virulence. J Infect Dis. 1984 Nov;150(5):721–727. doi: 10.1093/infdis/150.5.721. [DOI] [PubMed] [Google Scholar]
- Beuth J., Ko H. L., Schumacher-Perdreau F., Peters G., Heczko P., Pulverer G. Hemagglutination by Staphylococcus saprophyticus and other coagulase-negative staphylococci. Microb Pathog. 1988 May;4(5):379–383. doi: 10.1016/0882-4010(88)90065-4. [DOI] [PubMed] [Google Scholar]
- Christensen G. D., Simpson W. A., Bisno A. L., Beachey E. H. Adherence of slime-producing strains of Staphylococcus epidermidis to smooth surfaces. Infect Immun. 1982 Jul;37(1):318–326. doi: 10.1128/iai.37.1.318-326.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen G. D., Simpson W. A., Bisno A. L., Beachey E. H. Experimental foreign body infections in mice challenged with slime-producing Staphylococcus epidermidis. Infect Immun. 1983 Apr;40(1):407–410. doi: 10.1128/iai.40.1.407-410.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies A. J. Coagulase negative staphylococcal infections. Br Med J (Clin Res Ed) 1985 Apr 27;290(6477):1230–1231. doi: 10.1136/bmj.290.6477.1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewry D. T., Galbraith L., Wilkinson B. J., Wilkinson S. G. Staphylococcal slime: a cautionary tale. J Clin Microbiol. 1990 Jun;28(6):1292–1296. doi: 10.1128/jcm.28.6.1292-1296.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fidalgo S., Vázquez F., Mendoza M. C., Pérez F., Méndez F. J. Bacteremia due to Staphylococcus epidermidis: microbiologic, epidemiologic, clinical, and prognostic features. Rev Infect Dis. 1990 May-Jun;12(3):520–528. doi: 10.1093/clinids/12.3.520. [DOI] [PubMed] [Google Scholar]
- Fleer A., Verhoef J. New aspects of staphylococcal infections: emergence of coagulase-negative staphylococci as pathogens. Antonie Van Leeuwenhoek. 1984;50(5-6):729–744. doi: 10.1007/BF02386237. [DOI] [PubMed] [Google Scholar]
- Ford C. W., Hamel J. C., Stapert D., Yancey R. J. Establishment of an experimental model of a Staphylococcus aureus abscess in mice by use of dextran and gelatin microcarriers. J Med Microbiol. 1989 Apr;28(4):259–266. doi: 10.1099/00222615-28-4-259. [DOI] [PubMed] [Google Scholar]
- GLADSTONE G. P., VAN HEYNINGEN W. E. Staphylococcal leucocidins. Br J Exp Pathol. 1957 Apr;38(2):123–137. [PMC free article] [PubMed] [Google Scholar]
- Gahrn-Hansen B. Coagulase-negative staphylococci and micrococci in clinical microbiology. Dan Med Bull. 1987 Apr;34(2):96–114. [PubMed] [Google Scholar]
- Holmberg O. Staphylococcus epidermidis isolated from bovine milk. Biochemical properties, phage sensitivity and pathogenicity for the udder. Acta Vet Scand Suppl. 1973:1–144. [PubMed] [Google Scholar]
- Ichiman Y., Yoshida K. The relationship of capsular-type of Staphylococcus epidermidis to virulence and induction of resistance in the mouse. J Appl Bacteriol. 1981 Oct;51(2):229–241. doi: 10.1111/j.1365-2672.1981.tb01237.x. [DOI] [PubMed] [Google Scholar]
- Kloos W. E., Schleifer K. H. Simplified scheme for routine identification of human Staphylococcus species. J Clin Microbiol. 1975 Jan;1(1):82–88. doi: 10.1128/jcm.1.1.82-88.1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambe D. W., Jr, Ferguson K. P., Keplinger J. L., Gemmell C. G., Kalbfleisch J. H. Pathogenicity of Staphylococcus lugdunensis, Staphylococcus schleiferi, and three other coagulase-negative staphylococci in a mouse model and possible virulence factors. Can J Microbiol. 1990 Jul;36(7):455–463. doi: 10.1139/m90-080. [DOI] [PubMed] [Google Scholar]
- Lanzilli G., Spanò C. Bacterial contamination of intravenous catheters and other plastic devices. Infection. 1987 Jan-Feb;15(1):42–43. doi: 10.1007/BF01646118. [DOI] [PubMed] [Google Scholar]
- Lenkei G., Belicza E., Sztroj T., Rédai I., Rozgonyi F. Distribution and antibiotic resistance of coagulase-negative staphylococci isolated from human nosocomial infections. J Chemother. 1989 Jul;1(4 Suppl):277–279. [PubMed] [Google Scholar]
- Pfaller M. A., Herwaldt L. A. Laboratory, clinical, and epidemiological aspects of coagulase-negative staphylococci. Clin Microbiol Rev. 1988 Jul;1(3):281–299. doi: 10.1128/cmr.1.3.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Righter J. Septicemia due to coagulase-negative Staphylococcus in a community hospital. CMAJ. 1987 Jul 15;137(2):121–125. [PMC free article] [PubMed] [Google Scholar]
- Solymossy M., Mandl J., Nagy Z., Antoni F. Cytotoxic material released from Staphylococcus epidermidis. II. Fractionation and some effects of the fractions on lymphocytes and hepatocytes. Acta Microbiol Acad Sci Hung. 1982;29(4):277–284. [PubMed] [Google Scholar]
- Solymossy M., Nagy Z., Antoni F. Cytotoxic material released from Staphylococcus epidermidis. I. Effects on [3H]thymidine incorporation of human lymphocytes. Acta Microbiol Acad Sci Hung. 1982;29(1):27–32. [PubMed] [Google Scholar]
- Viscoli C., Van der Auwera P., Meunier F. Gram-positive infections in granulocytopenic patients: an important issue? J Antimicrob Chemother. 1988 Apr;21 (Suppl 100):149–156. doi: 10.1093/jac/21.suppl_c.149. [DOI] [PubMed] [Google Scholar]
- West T. E., Walshe J. J., Krol C. P., Amsterdam D. Staphylococcal peritonitis in patients on continuous peritoneal dialysis. J Clin Microbiol. 1986 May;23(5):809–812. doi: 10.1128/jcm.23.5.809-812.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]