Abstract
This article aims to describe a simple and reliable technique that helps in positioning the cannulated percutaneous screws during fixation of depression-type tibial plateau fractures. After fracture reduction under arthroscopic control, an outside-in anterior cruciate ligament femoral guide is introduced through the tibial cortical metaphyseal window and positioned under endoscopic control just underneath the elevated fragment. When proper height is achieved, a guide pin is drilled from lateral to medial through the sleeve, 1 to 2 cm distal to the articular surface of the depressed fragment. The cannulated screw can then be introduced under endoscopic control, without fluoroscopic assistance, just under the previously elevated joint surface. This technique ensures optimal placement of the cannulated screw in the middle of the bony tunnel to obtain optimal subchondral bone support during fixation of the depressed tibial plateau fracture.
Tibial plateau fractures are associated with high morbidity. The main goal of treatment is to achieve accurate reduction of the articular lesion, which can be technically demanding. First described by Caspari et al.1 and Jennings,2 arthroscopically assisted techniques, when compared with traditional open reduction and internal fixation, are less invasive; allow full evaluation of intra-articular lesions; ensure optimal anatomic reduction through Schatzker type 1, 2, and 3 fractures; and are associated with decreased morbidity rates.3 Such techniques are based on percutaneous articular reduction under arthroscopic control followed by stable fixation. The most common fixation method is by a subchondrally placed cannulated cancellous screw. Traditionally, screw and guide pin placement is performed under fluoroscopic guidance.3 Assessment of guide pin and screw positioning under fluoroscopic control to obtain optimal support of the subchondral bone after elevation of the depressed fragment is technically challenging and time-consuming. A specific automatic pinning system has already been described to ease screw placement but is not easily available.4 We describe an original, simple and reliable technique that allows accurate positioning of the guidewire and the cannulated screw percutaneously underneath the elevated fragment without the use of a C-arm intraoperatively (Fig 1, Table 1).
Fig 1.
Our simple trick allows the surgeon to avoid the use of fluoroscopy intraoperatively to position the cannulated screw for fixation of a depression lateral tibial plateau fracture. After reduction of the fragment, an outside-in anterior cruciate ligament femoral guide, set at maximum amplitude with a 115° to 120° aiming device, is introduced through the tibial cortical metaphyseal window and positioned under endoscopic control just underneath the elevated fragment. This ensures optimal placement of the screw in the middle of the bony tunnel just underneath the elevated fragment to obtain an optimal rafter effect.
Table 1.
Advantages and Disadvantages
| Advantages |
| Optimal positioning of the subchondral screw that supports the elevated fragment |
| Decreased total radiation dose (fluoroscopy-free technique) |
| Avoidance of expensive and customized equipment (normal common ACL guide instrumentation) |
| Less fracture manipulation during surgery |
| Disadvantages |
| Need for an adjustable ACL reconstruction outside-in femoral guide |
ACL, anterior cruciate ligament.
Surgical Technique
Patient Position and Setup
The patient is placed in the supine position on a standard table (Video 1). Arthroscopy of the knee joint is performed using standard arthroscopic portals after inflation of a tourniquet. All the arthroscopic procedures are carried out with a continuous flow of physiological saline solution under gravity pressure. This acts as a checkrein to reduce the occurrence of compartment syndrome.
Hematoma Evacuation and Fracture Visualization
We irrigate the joint and evacuate all blood clots. Possible associated intra-articular lesions are evaluated under direct arthroscopic view.
Position of Guide Pin and Preparation of Cortical Window
A 2- to 3-cm incision is made on the tibia, approximately 10 cm distal to the joint line. A tibia-specific jig (Tibial Plateau Fracture Management System [AR-6010]; Arthrex, Naples, FL) is positioned arthroscopically through the anteromedial portal (Fig 2 A and B). Under arthroscopic control, the jig is oriented toward the depressed fragment; when satisfactory orientation is achieved, a guide pin is drilled toward the deepest point of the fracture. This step is followed by overdrilling the tibial cortex with a 10-mm cannulated reamer (Arthrex), thereby creating a window on the anteromedial cortex of the tibia (Table 2).
Fig 2.
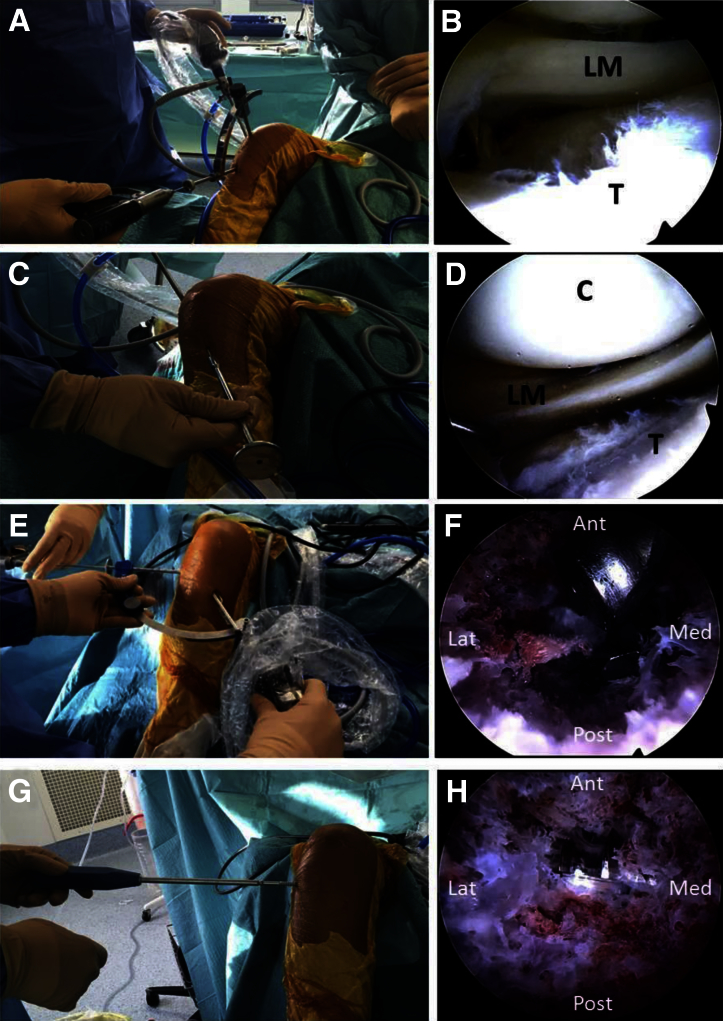
Surgical technique. (A, B) The patient is placed in the supine position on a standard table. A tibia-specific jig (Tibial Plateau Fracture Management System) is positioned arthroscopically, through the anteromedial portal. When satisfactory orientation is achieved, a guide pin is drilled toward the deepest point of the fracture. (C, D) A cannulated tamp (Arthrex) is introduced through the tibial cortical window, and under arthroscopic guidance, the depressed fragment is carefully elevated until satisfactory reduction is achieved. (E, F) An outside-in anterior cruciate ligament femoral guide (Arthrex), set at maximum amplitude with a 115° to 120° aiming device, is introduced through the tibial cortical metaphyseal window and positioned under endoscopic control just underneath the elevated fragment. (G, H) A 7-mm cannulated cancellous screw with an 16- or 32-mm thread length is then introduced over the guide pin, after drilling and tapping (Magna-FX cannulated screw system), under endoscopic control. (Ant, anterior; C, condyle; Lat, lateral; LM, lateral meniscus; Med, medial; Post, posterior; T, tibia.)
Table 2.
Pearls and Pitfalls
| Pearls | Pitfalls | |
|---|---|---|
| Tibial bone hole | The surgeon should overdrill only the tibial cortex. | Aggressive drilling may lead to further metaphyseal bone loss or even damage to the articular surface. |
| Screw placement | Setting the ACL femoral guide at 115° to 120° will help position the guide pin parallel to the articular surface. | Improper ACL jig angulation will result in suboptimal screw placement, resulting in the loss of the “rafter” effect. |
| Arthroscopic inspection after guidewire positioning is advised. | Doing so will prevent inadvertent intra-articular positioning of the screw. | |
| Fracture evaluation | The surgeon should evaluate the cortical bone envelope integrity on a computed tomography scan. | Poor bone quality or excessive metaphyseal impaction will result in a weak construct. |
| The coronary ligament between the capsule and meniscus may be divided to mobilize the meniscus and visualize the full extent of the fracture. | Inappropriate visualization may underestimate the full fracture extent. | |
| Bone graft | Bone graft placed through the tibial cortical window will help support the articular cartilage reduction. | Graft-site morbidity (autologous graft) and/or increased cost to the patient (allograft) can occur. |
ACL, anterior cruciate ligament.
Fracture Reduction
A cannulated tamp (Tibial Plateau Fracture Management System) is introduced through the tibial cortical window, and under arthroscopic guidance, the depressed fragment is carefully elevated until satisfactory reduction is achieved (Fig 2 C and D). Temporary fixation can be achieved with subchondrally placed 3.2-mm K-wires (Magna-FX cannulated screw system; Zimmer, Warsaw, IN) to prevent loss of reduction. In addition, if mediolateral compression is required, stab incisions are made appropriately and a reduction clamp (Tibial Plateau Fracture Management System) is placed to hold reduction.
Cannulated Screw Fixation
An outside-in anterior cruciate ligament femoral guide (Arthrex), set at maximum amplitude with a 115° to 120° aiming device, is introduced through the tibial cortical metaphyseal window and positioned under endoscopic control just underneath the elevated fragment (Fig 2 E and F). Care must be taken with the management of both instruments in the tibial bone tunnel because they can increase the metaphyseal bone hole and further weaken the subchondral bone. When proper height is achieved, a 3.2-mm guide pin (Magna-FX cannulated screw system) is then drilled from lateral to medial through the sleeve, 1 to 2 cm distal to the articular surface of the depressed fragment. Arthroscopic control can ensure the guidewire is optimally positioned: in the middle of the bony tunnel, with no articular breach, without the need for C-arm fluoroscopy assistance. A 7-mm cannulated screw (Magna-FX cannulated screw system) is introduced over the guide pin, after drilling and tapping, under endoscopic control (Fig 2 G and H).
The cortical window can then be filled with either autologous or synthetic bone graft to create a solid tunnel. The subchondrally placed screw acts as a rafter supporting the cortical surface.
Postoperative Protocol
The leg is palpated for any firmness, and periodic monitoring for compartment syndrome is carried out in the immediate postoperative period. Deep vein thrombosis prophylaxis is administered postoperatively and continued for 6 weeks. The patient is kept non–weight bearing for 6 weeks after surgery. Static quadriceps and knee range-of-motion exercises are started immediately after surgery as per pain tolerance. Partial weight bearing is started with a walking aid as tolerated by the patient after 6 weeks, with a gradual increase to full weight bearing by 10 weeks.
Discussion
Arthroscopy-assisted percutaneous fixation can be the treatment of choice in Schatzker type 2 and 3 fractures because it ensures optimal reduction and stable fixation.5 Screw position is usually evaluated on intraoperative anteroposterior and lateral fluoroscopy views.6 However, a depressed fracture may not be fully appreciated with C-arm fluoroscopy intraoperatively.7 Cross-sectional imaging is needed to clearly evaluate it. Moreover, with the use of fluoroscopy, it is difficult to intraoperatively assess the bone core position after elevating the depressed fragments and to understand the cannulated screw positioning underneath the subchondral bone to obtain optimal support. Correct positioning of the cannulated screws is required because the joint surface congruity achieved during surgery must be maintained during the healing period by the cannulated screw support (Fig 3). Therefore, inaccurate screw placement may lead to a superior toggling of the screws with articular penetration or an inferior toggling of the screws, causing loss of reduction and eventually leading to articular incongruity.3
Fig 3.
Preoperative and postoperative radiographs of 2 cases of Schatzker type 3 depressed lateral tibial plateau fracture. (A, C) Tibial plateau fractures (arrows) occasionally are difficult to appreciate with standard radiographs. The preferred examination consists of radiographs in multiple obliquities of the knee. (B, D) Postoperative anteroposterior views after 7-mm cannulated screws (Magna-FX cannulated screw system) were used as a rafter to support the articular surface.
Our technique is a modification of the fluoroscopy-free technique with custom-made instruments for tibial fracture treatment described by Suganuma and Akutsu.4 However, such custom-made guides are not ordinarily available. Rather than using custom-made instruments to obtain articular reduction through impaction and optimal screw placement, we present a simplified practical approach, using a routine outside-in anterior cruciate ligament guide to obtain a fluoroscopy-free, accurate fracture reduction and optimal subchondral screw positioning. Whereas avoiding fluoroscopy during the procedure decreases the total radiation dose, arthroscopically assisted reduction throughout guided screw placement may reduce the surgical time, ease the articular reduction, and ensure optimal support provided from subchondral screws. This simple technical trick avoids the need for customized equipment, reduces manipulation during surgery, and ensures an anatomic fracture reduction.
Footnotes
The authors report the following potential conflict of interest or source of funding: M.T. receives support from Arthrex. B.S-C. receives support from Arthrex. J.M.F. receives support from Arthrex.
Supplementary Data
Two cases of Schatzker type 3 depressed lateral tibial plateau fracture are presented. Both fractures are reduced under arthroscopic control, using specific instrumentation (Tibial Plateau Fracture Management System). After fracture reduction under arthroscopic control, an outside-in anterior cruciate ligament femoral guide (Arthrex) is introduced through the tibial cortical metaphyseal window and positioned under endoscopic control just underneath the elevated fragment. When proper height is achieved, a guide pin (Magna-FX cannulated screw system) is then drilled from lateral to medial through the sleeve, 1 to 2 cm distal to the articular surface of the depressed fragment. The cannulated screw (Magna-FX cannulated screw system) can then be introduced under endoscopic control, without fluoroscopic assistance, just under the previously elevated joint surface. This technique ensures optimal placement of the cannulated screw in the middle of the bony tunnel to obtain optimal subchondral bone support during fixation of the depressed tibial plateau fracture.
References
- 1.Caspari R.B., Hutton P.M., Whipple T.L., Meyers J.F. The role of arthroscopy in the management of tibial plateau fractures. Arthroscopy. 1985;1:76–82. doi: 10.1016/s0749-8063(85)80035-9. [DOI] [PubMed] [Google Scholar]
- 2.Jennings J.E. Arthroscopic management of tibial plateau fractures. Arthroscopy. 1985;1:160–168. doi: 10.1016/s0749-8063(85)80003-7. [DOI] [PubMed] [Google Scholar]
- 3.Burdin G. Arthroscopic management of tibial plateau fractures: Surgical technique. Orthop Traumatol Surg Res. 2013;99(suppl):S208–S218. doi: 10.1016/j.otsr.2012.11.011. [DOI] [PubMed] [Google Scholar]
- 4.Suganuma J., Akutsu S. Arthroscopically assisted treatment of tibial plateau fractures. Arthroscopy. 2004;20:1084–1089. doi: 10.1016/j.arthro.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 5.Lubowitz J.H., Elson W.S., Guttmann D. Part I: Arthroscopic management of tibial plateau fractures. Arthroscopy. 2004;20:1063–1070. doi: 10.1016/j.arthro.2004.09.001. [DOI] [PubMed] [Google Scholar]
- 6.Hartigan D.E., McCarthy M.A., Krych A.J., Levy B.A. Arthroscopic-assisted reduction and percutaneous fixation of tibial plateau fractures. Arthrosc Tech. 2015;4:e51–e55. doi: 10.1016/j.eats.2014.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haller J.M., O'Toole R., Graves M. How much articular displacement can be detected using fluoroscopy for tibial plateau fractures? Injury. 2015;46:2243–2247. doi: 10.1016/j.injury.2015.06.043. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Two cases of Schatzker type 3 depressed lateral tibial plateau fracture are presented. Both fractures are reduced under arthroscopic control, using specific instrumentation (Tibial Plateau Fracture Management System). After fracture reduction under arthroscopic control, an outside-in anterior cruciate ligament femoral guide (Arthrex) is introduced through the tibial cortical metaphyseal window and positioned under endoscopic control just underneath the elevated fragment. When proper height is achieved, a guide pin (Magna-FX cannulated screw system) is then drilled from lateral to medial through the sleeve, 1 to 2 cm distal to the articular surface of the depressed fragment. The cannulated screw (Magna-FX cannulated screw system) can then be introduced under endoscopic control, without fluoroscopic assistance, just under the previously elevated joint surface. This technique ensures optimal placement of the cannulated screw in the middle of the bony tunnel to obtain optimal subchondral bone support during fixation of the depressed tibial plateau fracture.