Abstract
The arthroscopic remplissage procedure has gained popularity in recent years and is gaining acceptance as an excellent and safe procedure to perform in patients with large engaging Hill-Sachs lesions. The procedure was introduced as an arthroscopic procedure, but surgeons not familiar with the procedure often encounter many problems, which makes the procedure difficult and frustrating to perform. A technique for this procedure using a commercially available PASTA (partial articular supraspinatus tendon avulsion) repair kit is presented.
Arthroscopic shoulder stabilization surgery is well established and has become one of the most commonly performed arthroscopic procedures in the shoulder. In the presence of bone defects, a simple Bankart repair results in unacceptably high rates of recurrent dislocations.1, 2
The Hill-Sachs remplissage procedure has, in recent years, gained popularity. Most studies have reported good to excellent outcomes with little to no loss in range of movement and recurrence rates comparable with those of arthroscopic Bankart repairs performed in patients with clinically insignificant Hill-Sachs lesions. Most notably, complication rates associated with remplissage have been low.3
The remplissage procedure can be challenging and frustrating for surgeons without prior experience. Problems potentially faced include inadequate visualization, difficulty placing cannulas through the rotator cuff, inaccurate anchor placement, inability to locate the hole through the rotator cuff created by insertion of the awl (if no cannula is used), difficulty retrieving sutures from the subacromial space, inadvertent damage to the sutures while clearing tissue in the subacromial space, and difficulty completing the Bankart repair after the remplissage because of reduced glenohumeral space.
A remplissage technique that makes use of a commercially available PASTA (partial articular supraspinatus tendon avulsion) repair kit is presented (Video 1). The described technique uses the Healix Transtend Implant System (DePuy Synthes, Warsaw, IN).
Equipment
To successfully perform our arthroscopic technique for the Hill-Sachs remplissage procedure, the following items are required:
-
•
Standard shoulder arthroscopy equipment including a 30° standard 4.0-mm arthroscope (Stryker, Kalamazoo, MI)—a 70° arthroscope may be required if visualizing through a low anterior portal
-
•
Arthroscopic rasp or ring curette (DePuy Mitek, Raynham, MA)
-
•
PASTA repair kit (we use the Healix Transtend Implant System with 2 double-loaded 3.4-mm anchors)
-
•
Arthroscopic knot pusher (DePuy Mitek)
-
•
Arthroscopic suture cutter (DePuy Mitek)
It must be noted that the use of the PASTA repair kit described in this report is an off-label use. A standard PASTA kit comprises a sharp guidewire, an obturator that fits snugly within a cannula, and an awl that also fits through the cannula. The anchor is designed to just pass through the cannula. This ensures that the hole made in the rotator cuff is just large enough to allow passage of the cannula, thereby minimizing damage to the rotator cuff.
Technique
Step 1: Setup and Patient Positioning
The procedure can be performed with the patient in the beach-chair or lateral decubitus position. However, in our experience, the procedure is less difficult to complete with the patient in the lateral decubitus position because the humeral head is pulled anteriorly and inferiorly, hence increasing the amount of space between the Hill-Sachs lesion and the overlying capsule and infraspinatus tendon (Fig 1 A and B). If the beach-chair position is used, the surgeon should ensure that the monitor is positioned directly opposite himself or herself (across the patient) rather than at the foot of the patient. Alternatively, the surgeon should have 2 monitors—one at the foot and another at the head of the patient. Otherwise, the surgeon will find himself or herself having to look over his or her shoulder while performing the remplissage procedure, which will be uncomfortable and disorienting. The surgeon should also consider using a mechanical or hydraulic arm holder (Trimano Arm Holder [Maquet, Rastatt, Germany] or Spider Limb Positioner [Smith & Nephew, London, England]), which will allow him or her to apply sustained traction to, and control rotation of, the arm while he or she performs the remplissage.
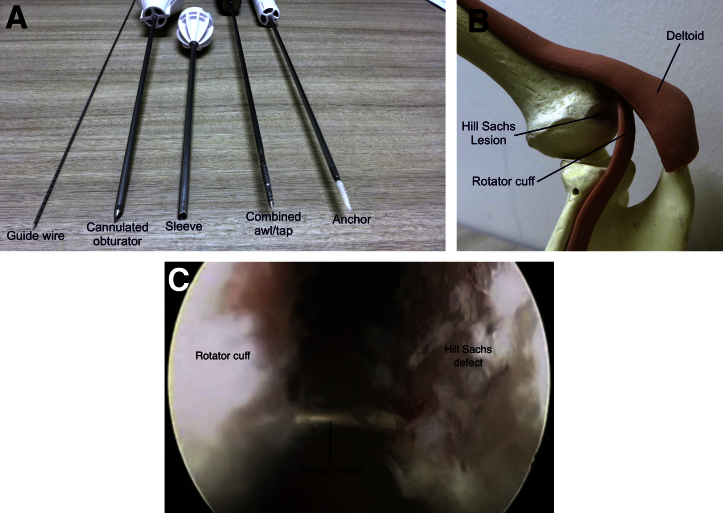
Fig 1.
(A) Standard PASTA (partial articular supraspinatus tendon avulsion) repair kit. (B) Illustrated technique. A Sawbones model (Pacific Research Laboratories, Vashon, WA) is set up as pictured. The rotator cuff muscle and tendon with the overlying deltoid muscle are added. They have been deliberately left anatomically inaccurate to allow adequate visualization of the Hill-Sachs lesion. (C) A spinal needle is percutaneously placed into the joint, through the deltoid muscle and infraspinatus tendon. The surgeon should visualize that he or she is able to easily change the angle of the instruments and eventually insert an anchor on either side of the spinal needle.
Step 2: Portal Placement
The classically described posterior viewing portal is 2 cm inferior and 2 cm medial to the posterolateral corner of the acromion. If a Hill-Sachs remplissage procedure is anticipated, a slightly lateral and superior4 posterior portal is implemented. This modified posterior portal allows the same portal, first established for access to the glenohumeral joint, to be used as the working portal for the eventual remplissage procedure as well. However, in our experience, the use of this modified portal often results in a suboptimal angle with respect to the bed of the Hill-Sachs lesion. As such, the use of this modified portal is not recommended. A single additional portal (after the optimal placement of this portal has been verified arthroscopically) should be routinely made. After the glenohumeral joint is accessed through the posterior portal, a diagnostic arthroscopy of the shoulder is performed and the need for Hill-Sachs remplissage confirmed. The surgeon then proceeds with the establishment of an anterior working portal and anterosuperior accessory portal.
Step 3: Preparation for Bankart Repair
Mobilization of the anteroinferior labrum and freshening of the anterior glenoid as per a standard Bankart repair are performed.
Step 4: Preparation of Hill-Sachs Lesion
The camera should be switched to the anterosuperior accessory portal. An excellent view of the entire Hill-Sachs lesion can be obtained using a 30° arthroscope. An adequate view can also be obtained from the anterior working portal (placed just superior to the subscapularis tendon), although a 70° arthroscope is required. The bed of the Hill-Sachs lesion, which is usually covered with thin membranous scar tissue, is abraded with a curette or rasp introduced through the posterior portal.
Step 5: Creation of Accessory Portal for Insertion of Anchors
A spinal needle (Quincke; B. Braun Medical, Bethlehem, PA) placed either percutaneously or through the modified posterior portal is used to ensure that the anchors can be optimally placed in the superior and inferior extent of the Hill-Sachs lesion (Fig 1C). The spinal needle is then replaced with the guidewire of the PASTA kit, which is gently tapped into the cancellous bone of the humeral head (Fig 2A).
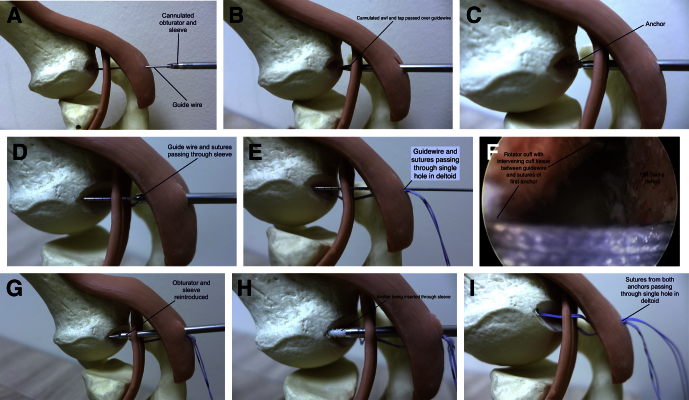
Fig 2.
(A) Once the position of the needle is satisfactory, it is removed. A 0.5-cm nick is made in the skin, and the 1.1-mm guidewire is inserted in the same direction as the spinal needle and tapped into the Hill-Sachs defect. (B) A 4-mm cannula with a sharp obturator is passed over the wire and into the joint. The guidewire and obturator are then removed. (C) A hole for the anchor is created with an awl or drill (depending on the system being used). The anchor is then inserted and its introducer removed. (D) The tip of the cannula is carefully withdrawn. It is important to visualize this step arthroscopically. Once the cannula has been withdrawn beyond the rotator cuff tendon, it must not be withdrawn any further. The guidewire is inserted, the cannula (containing the guidewire and the sutures from the first anchor) is redirected, and the guidewire is used to pierce the rotator cuff tendon again, leaving a sufficient bridge of infraspinatus tendon between the exiting sutures and the guidewire. (E) The cannula must now be completely withdrawn while the surgeon ensures the guidewire stays in place. This is done so that the sutures from the first anchor can be extricated from the cannula. (F) Arthroscopic view showing a generous sleeve of rotator cuff tissue between the sutures from the first anchor and the guidewire, which will guide the insertion of the second anchor. (G) The sharp obturator together with the cannula can now be advanced over the guidewire, through the infraspinatus tendon, and into the joint. (H) A hole is created using the awl, and another anchor is inserted. (I) The surgeon now has 2 anchors inserted into the Hill-Sachs lesion with their respective sutures piercing the infraspinatus tendon at separate points (leaving a bridge of intervening tendon). The sutures exit the deltoid muscle and skin through a single portal.
Step 6: Insertion of Cannula and First Anchor
The obturator and cannula of the PASTA repair system are passed over the guidewire and advanced into the joint through the infraspinatus tendon (Fig 2B). Once the cannula is within the joint, the surgeon can remove the guidewire and the obturator and proceed with the usual steps for placing the anchor (Fig 2C). It is important to be mindful of the direction in which the anchor is placed to avoid inadvertent penetration of the articular surface by the awl or anchor.
Step 7: Insertion of Second Anchor
The cannula is withdrawn under direct vision until just beyond the hole in the infraspinatus tendon. The guidewire is then inserted through the cannula and used to pierce the infraspinatus tendon a sufficient distance away from the initial hole, creating an intervening bridge of infraspinatus tendon (Fig 2D). Once a satisfactory position for the next anchor is obtained, the guidewire is again tapped into the cancellous bone (Fig 2 E and F). The anchors are placed as far apart within the bed of the Hill-Sachs lesion as possible, ensuring as maximum coverage of the lesion and as large a sleeve of intervening rotator cuff and capsule as possible.
The cannula should now contain the strands of sutures from the first suture anchor and the guidewire. However, it is not possible to pass the obturator or the second anchor through the cannula because of the bulk of the sutures. Hence, the cannula must be fully withdrawn over the guidewire and the sutures extracted from the cannula. The obturator can now be inserted into the cannula and passed over the guidewire, through the infraspinatus, and into the joint (Fig 2G). The same process for inserting the first anchor is repeated, after which the cannula can be withdrawn (Fig 2H). The result at this stage is 4 strands of sutures (2 from each anchor) separated by a bridge of infraspinatus, exiting from the same portal traversing the skin, subcutaneous tissue, and deltoid muscle (Fig 2I).
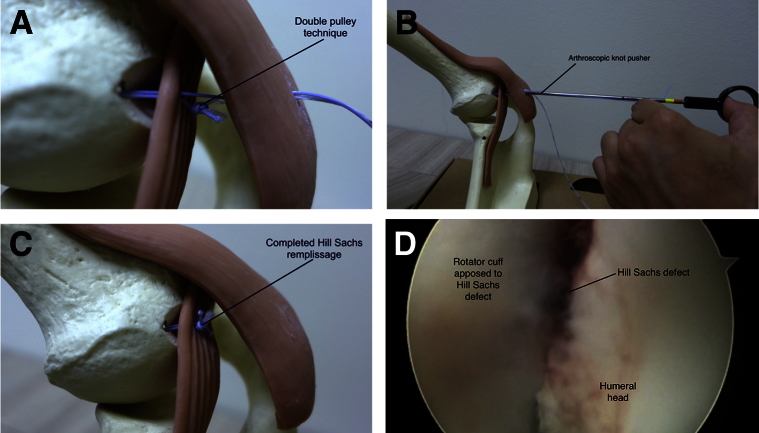
Step 8: Completion of Bankart Repair and Remplissage Procedure
The surgeon may now proceed with the Bankart repair, after which the remplissage procedure can be completed by the double-pulley technique5 (Fig 3). There is no need to enter the subacromial space to retrieve the sutures before tying the sutures to complete the remplissage procedure. This technique ensures there is no deltoid muscle caught in the sutures bridging the anchors as long as the cannula is withdrawn under direct vision until just beyond the cannula hole in the infraspinatus. Patients who have undergone remplissage with this technique have full range of movement, as reported by other authors.5, 6
Fig 3.
(A) The double-pulley technique is performed, and remplissage is completed. (B) The surgeon must be comfortable with arthroscopic knot tying, and he or she should be sufficiently proficient to be able to tie static arthroscopic knots blindly (i.e., tying arthroscopic knots without direct visualization of the knots). (C) Completed Hill-Sachs remplissage. (D) Completed remplissage showing excellent apposition of the overlying rotator cuff to the bed of the Hill-Sachs defect.
Discussion
The Hill-Sachs lesion has been recognized since 1940,7 but its role in contributing to recurrent shoulder instability was not fully appreciated until Palmer and Widen8 described the “engaging Hill Sachs” lesion. The Hill-Sachs lesion has been identified in up to 80% of shoulder instability cases.6 Many authors have shown that the presence of bony lesions on either the glenoid or the humeral head results in higher rates of recurrent instability if only a Bankart repair is carried out.1, 9
Various surgical techniques have been described for the management of a significantly sized Hill-Sachs lesion. These include rotational humeral osteotomy,10 filling of the defect with osteochondral allograft,11 transfer of the infraspinatus into the defect,12 humeroplasty,13 and resurfacing arthroplasty.14 These procedures, however, can be technically challenging, often cannot be accomplished arthroscopically, and are associated with potentially serious complications.3
In the original technique described by Wolf and colleagues,4 they placed suture anchors into the humeral head through the Hill-Sachs defect and retrieved one limb of the sutures using a sharp penetrating grasper with a 1-cm bridge of infraspinatus tendon. They repeated this process with another anchor before moving to the subacromial space, retrieving the sutures from the subacromial space, and finally, tying the sutures under direct arthroscopic vision. Koo et al.5 subsequently published a modification of the original technique, coined the “double-pulley technique,” postulating that a larger footprint of fixation can be achieved with their technique. They reported good results in their series of over 20 patients, with all but 1 having excellent range of movement and strength. A recently published biomechanical study performed in cadavers by Tan et al.15 confirmed that the double-pulley technique is effective at preventing engaging of a Hill-Sachs defect.
Although conceptually straightforward, the arthroscopic remplissage procedure can be difficult for the arthroscopic surgeon attempting it for the first time. Difficulties he or she may encounter, along with useful pearls, are listed in Table 1. The described technique has several advantages, as listed in Table 2.
Table 1.
Pitfalls and Pearls
| Pitfalls | Pearls |
|---|---|
| Poor visualization of the Hill-Sachs defect | The surgeon should use a high anterior viewing portal or a 70° arthroscope. |
| Limited working space posteriorly | The surgeon should apply slight traction to the arm and increase pump pressure temporarily. |
| Difficulty placing a cannula through the thick rotator cuff tendon and capsule | The Transtend system alleviates this problem. |
| Cannula slipping out once placed | The Transtend system alleviates this problem. |
| Poor placement of the anchor with possible penetration of the articular surface of the humeral head | The surgeon should establish an accessory posterolateral portal using a spinal needle to guide him or her. |
| Disorientation when viewing from the anterior portal, resulting in frustration | If operating with the patient in the beach-chair position, the surgeon should ensure that the screen is placed directly opposite himself or herself. |
| Difficulty accurately retrieving the separate limbs of the sutures intra-articularly if using the sharp tissue penetrator (technique described by Wolf and colleagues4) | Our technique does not require this step. |
| Difficulty locating the limbs of the suture from the subacromial space | Our technique does not require this step. |
| Encountering bleeding vessels in the subacromial space (because the sutures are place posteriorly, in an extra-bursal manner) | Our technique does not require this step. |
| Inadvertent damage to or debridement of the sutures limbs while attempting to locate the sutures in the subacromial space | Our technique does not require this step. |
Table 2.
Advantages of Hill-Sachs Remplissage Using PASTA Kit
| The guidewire with the cannulated obturator and the cannula system allow easy penetration of the rotator cuff. |
| The small diameter of the cannula is designed to just allow passage of the anchor; hence, the hole made in the rotator cuff is small. |
| There is no need to enter the subacromial space to retrieve the ends of the sutures, hence eliminating the risk of inadvertent damage to the sutures. |
| Because the surgeon does not have to enter the subacromial space, frustration from being unable to locate the sutures and encountering bleeding vessels is eliminated. |
| The immediate effect of the Hill-Sachs remplissage can be seen intra-articularly when the sutures are tied blind—the capsule and rotator cuff can be seen approximating the Hill-Sachs defect. |
Our technique has several potential problems and limitations. Because both anchors are placed within the Hill-Sachs defect through a single stab incision, utmost care must be taken to ensure that the incision allows for optimal direction and placement of both anchors. This is achieved by using a long spinal needle inserted percutaneously and viewed arthroscopically, before the skin incision is made. In addition, because a double-pulley technique is used, if one of the suture limbs ruptures or if any of the knots slip, the procedure will fail. Hence, double-loaded anchors, which allow for 2 double-pulley systems to be tied, are used. Moreover, our technique uses the Transtend PASTA repair kit and hence only can be performed if this kit is available, unless other kits are used with some improvisation. In addition, the anchors used are 3.4-mm anchors, which some surgeons may believe are too small. Finally, to use this technique, the surgeon must first be comfortable with “blind” arthroscopic knot tying.
Footnotes
The authors report the following potential conflict of interest or source of funding: B.H.M.T. has attended courses and a surgeon visitation was paid for by various implant companies (Arthrex and Johnson & Johnson), but these activities were unrelated to the submitted work.
Supplementary Data
Technique performed on the left shoulder of a patient in the lateral decubitus position with 10 lb of traction, viewed from a standard posterior portal. An engaging Hill-Sachs lesion is shown arthroscopically. A high anterior portal is then created and used as the viewing portal, and the posterior portal is now used to prepare the bed of the Hill-Sachs lesion. A needle is used to identify the optimal position of the accessory posterolateral portal, which is used to complete the remplissage procedure.
References
- 1.Burkhart S.S., De Beer J.F. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: Significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16:677–694. doi: 10.1053/jars.2000.17715. [DOI] [PubMed] [Google Scholar]
- 2.Boileau P., Villalba M., Héry J.Y., Balg F., Ahrens P., Neyton L. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am. 2006;88:1755–1763. doi: 10.2106/JBJS.E.00817. [DOI] [PubMed] [Google Scholar]
- 3.Buza J.A., III, Iyengar J.J., Anakwenze O.A., Ahmad C.S., Levine W.N. Arthroscopic Hill-Sachs remplissage: A systematic review. J Bone Joint Surg Am. 2014;96:549–555. doi: 10.2106/JBJS.L.01760. [DOI] [PubMed] [Google Scholar]
- 4.Purchase R.J., Wolf E.M., Hobgood E.R., Pollock M.E., Smalley C.C. Hill-Sachs “remplissage”: An arthroscopic solution for the engaging Hill-Sachs lesion. Arthroscopy. 2008;24:723–726. doi: 10.1016/j.arthro.2008.03.015. [DOI] [PubMed] [Google Scholar]
- 5.Koo S.S., Burkhart S.S., Ochoa E. Arthroscopic double-pulley remplissage technique for engaging Hill-Sachs lesions in anterior shoulder instability repairs. Arthroscopy. 2009;25:1343–1348. doi: 10.1016/j.arthro.2009.06.011. [DOI] [PubMed] [Google Scholar]
- 6.Zhu Y.-M., Lu Y., Zhang J., Shen J.-W., Jiang C.-Y. Arthroscopic Bankart repair combined with remplissage technique for the treatment of anterior shoulder instability with engaging Hill-Sachs lesion: A report of 49 cases with a minimum 2-year follow-up. Am J Sports Med. 2011;39:1640–1647. doi: 10.1177/0363546511400018. [DOI] [PubMed] [Google Scholar]
- 7.Hill H., Sachs M. The grooved defect of the humeral head: A frequently unrecognized complication of dislocations of the shoulder joint. Radiology. 1940;35:690–700. [Google Scholar]
- 8.Palmer I., Widen A. The bone block method for recurrent dislocation of the shoulder joint. J Bone Joint Surg Br. 1948;30:53–58. [PubMed] [Google Scholar]
- 9.Voos J.E., Livermore R.W., Feeley B.T. Prospective evaluation of arthroscopic Bankart repairs for anterior instability. Am J Sports Med. 2010;38:302–307. doi: 10.1177/0363546509348049. [DOI] [PubMed] [Google Scholar]
- 10.Weber B., Simpson L., Hardegger F. Rotational humeral osteotomy for recurrent anterior dislocation of the shoulder associated with a large Hill-Sachs lesion. J Bone Joint Surg Am. 1984;66:1443–1450. [PubMed] [Google Scholar]
- 11.Chapovsky F., Kelly J.D., IV Osteochondral allograft transplantation for treatment of glenohumeral instability. Arthroscopy. 2005;21:1007. doi: 10.1016/j.arthro.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 12.Connolly J. Humeral head defects associated with shoulder dislocation—their diagnostic and surgical significance. Instr Course Lect. 1972;21:42–54. [Google Scholar]
- 13.Kazel M.D., Sekiya J.K., Greene J.A., Bruker C.T. Percutaneous correction (humeroplasty) of humeral head defects (Hill-Sachs) associated with anterior shoulder instability: A cadaveric study. Arthroscopy. 2005;21:1473–1478. doi: 10.1016/j.arthro.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 14.Armitage M.S., Faber K.J., Drosdowech D.S., Litchfield R.B., Athwal G.S. Humeral head bone defects: Remplissage, allograft, and arthroplasty. Orthop Clin North Am. 2010;41:417–425. doi: 10.1016/j.ocl.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 15.Tan C.H.J., Saier T., von Deimling C. Effect of three remplissage techniques on tendon coverage and shoulder kinematics: A navigated robotic biomechanical study. BMC Musculoskelet Disord. 2016;17:1. doi: 10.1186/s12891-015-0856-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Technique performed on the left shoulder of a patient in the lateral decubitus position with 10 lb of traction, viewed from a standard posterior portal. An engaging Hill-Sachs lesion is shown arthroscopically. A high anterior portal is then created and used as the viewing portal, and the posterior portal is now used to prepare the bed of the Hill-Sachs lesion. A needle is used to identify the optimal position of the accessory posterolateral portal, which is used to complete the remplissage procedure.