Abstract
Both unicameral bone cysts and intraosseous lipoma of the calcaneus are rare entities that are mostly diagnosed because of unspecific heel pain, pathologic fracture, or as incidental finding. Minimally invasive ossoscopy with endoscopic resection of the tumor followed by grafting can potentially minimize risks of open surgery and speed up convalescence. We present our modifications to previously described techniques of endoscopic curettage with a particular focus on intraosseous lipoma and allogenic grafting. The key point for grafting is the use of a funnel-shaped ear speculum facilitating the plombage with allogenic cancellous bone chips. Compared with its alternatives, grafting with allogenic cancellous bone might prove favorable in this localization for several reasons: osteointegration, handling, availability, and costs. The objective of this technical note is to present a simple, safe, and cost-effective surgical technique for endoscopic surgical treatment of benign osteolytic lesions of the calcaneus.
We define the term “ossoscopy” as a minimally invasive procedure to visualize and treat pre-existing or iatrogenically created bone cavities with the help of an arthroscope or endoscope. Examples for ossoscopy include retrograde core drilling for osteochondral defects (iatrogenically created bone cavity) and minimally invasive treatment of benign osteolytic bone lesions such as calcaneal cysts (pre-existing bone cavity). Intraosseous lipoma (IOL) and simple bone cyst are the 2 entities most often responsible for benign osteolytic lesions of the calcaneus. Lipoma of bone is a benign neoplasm of adipocytes that typically arises within the medullary cavity of bone. IOL is rare and accounts for less than 0.1% of primary bone tumors; their actual incidence is not known. Considering that only a few cases of lipoma of bone have been published and often seem to be accidental findings, reliable data regarding age distribution are not available.1 Besides the proximal, metaphyseal femur, the calcaneus is a common predilection site.2 Intramedullary lipoma may be asymptomatic (30%) or produce aching pain or swelling (70%); rarely it presents as a pathologic fracture.2, 3 The typical appearance of a calcaneal lipoma consists of a well-defined lytic mass surrounded by a thin rim of sclerosis located in the ventral triangular area between the major trabecular groups (Diard's area 6).4, 5 The lesion often contains central dystrophic calcifications, commonly described as nidus or sequestrum.
Unicameral (simple) bone cyst (UBC) is a common tumor-like lesion of the bone. There is a strong predilection for the long bones of the proximal humerus and proximal femur, accounting for up to 85% of all cases.6 Calcaneal localization is less frequent. Localized at the lower extremities, UBC can cause persevering pain and thus justify surgical therapy.7 The main indication for treatment is pain and prevention of pathologic fracture. Pogoda et al. proposed that cysts reaching 100% of the cross-sectional diameter in the coronal plane and 30% in the sagittal plane were at risk for a pathological fracture.8, 9 Regarding localization and presentation on plain radiographs, calcaneal lipoma can be identical to UBC of the heel bone. These findings strictly have to be differentiated from physiological diminution of the calcaneal bone structure in the very same area.10, 11 If a lytic bone lesion of the calcaneus is seen on plain radiographs, magnetic resonance imaging (MRI) is mandatory for further clarification of relevant differential diagnoses.5
Treatment recommendations for asymptomatic calcaneal lipoma and unicameral bone cysts are still being discussed controversially. However, surgery is indicated in the presence of pain resistant to conservative treatment methods and impending or pathological fractures.12 Standard surgical procedures such as open curettage and autologous bone grafting can entail non-negligible risks and complications. Conventional open curettage and plombage of a benign lytic calcaneal bone lesion is usually performed through a lateral surgical approach with a longitudinal or L-shaped skin incision and a fenestration of the lateral cortical wall of the calcaneus.13 Prolonged wound healing and iatrogenic damage of the sural nerve are well-known complications for this localization. Furthermore, a large fenestration can weaken the cortical structures of the calcaneus additionally. Advantages of minimally invasive surgery include less pain, less scarring, and better aesthetical results as only a small incision and limited dissection is necessary.9, 14 Endoscopic curettage of solitary calcaneal cysts with different forms of grafting has been reported before with good results.9, 15 To the best of our knowledge, endoscopic treatment for IOL of the calcaneus has only been reported as a case report so far.16, 17 Compared with autografts, allogenic bone is easily available and almost unlimited in supply. Compared with injectable bone substitute, percutaneous grafting with allogenic cancellous bone chips can be exhausting and time-consuming though. Costs and osteintegration might still favor the use of allografts.
Technique
Preoperative Setup
Plain radiography and MRI are mandatory for an accurate preoperative planning; computed tomography scans are regarded as optional. The exact localization and expansion of the bone cavity is analyzed. Under general anesthesia, the patient is put in a stable lateral position on a radiolucent table, the lateral aspect of the affected rearfoot facing upward on the operation table. The dimensions of the bone lesion are marked under fluoroscopic control on the skin of the lateral rearfoot with a sterile pen.
Portal Placement
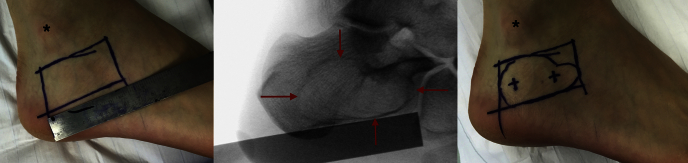
Depending on the size of the cystic bone lesion, the 2 portals for ossoscopy are marked accordingly over the lateral aspect of the calcaneus (Fig 1). After skin incision and blunt dissection of the underlying soft tissue, the thinned-out cortex can be penetrated with a semisharp obturator (Arthrex, Naples, FL) before the sheath for an arthroscope is introduced into the cavity. Depending on the size of the bone lesions, an arthroscope ranging from 2.7 to 4.0 mm in diameter can be used (Arthrex). One of the portals will need a diameter of 4 mm for percutaneous allogenic grafting. During blunt dissection to the lateral wall of the calcaneal bone, care must be taken not to harm the sural nerve and the peroneal tendons.
Fig 1.
With fluoroscopic control, the margins of the bone lesions and the 2 portals for ossoscopy are marked on the skin over the right lateral calcaneus. The patient is in a stable left lateral position. The black asterisk marks the lateral malleolus; the planta pedis is seen at the lower border of the figure. The red arrows mark the sclerotic borders of the bone lesion as seen through fluoroscopy (middle).
Ossoscopic Tumor Resection and Cleaning of the Bone Cavity
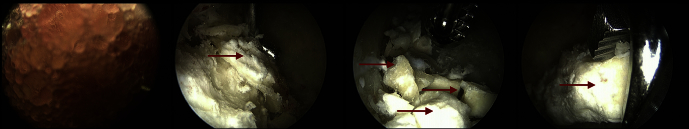
Contrary to ossoscopy of the calcaneal bone for unicameral bone cyst, in cases of IOL clear vision of the bone cavity can only be achieved after a second portal has been established and thorough endoscopic irrigation is performed. By this, loose lipomatous tissue is washed out and the typical calcified areas of IOL become visible. Calcifications are cleaned out with an arthroscopic shaver (3.0-mm Dissector, Arthrex); larger pieces can be grasped with an arthroscopic punch or grapser (Arthrex) (Fig 2). Often, a tennis net-like pseudomembrane covers the walls of the cavity. This membrane is common for UBC but can also be present in calcaneal lipoma. The membrane is resected and sent for histopathological analysis (Video 1).
Fig 2.
After introduction of the arthroscope into the bone cavity, vision is often impaired by fat tissue in case of intraosseous lipoma (left picture). After irrigation and endoscopic removal of the fat tissue, residual calcifications can be identified (red arrows). The term “ossifying lipoma” is sometimes used synonymously. The viewing portal (anterior) is on the same line in the anterior-posterior direction as the working portal (posterior). In this figure, all instruments (probe, shaver, and grasper) are introduced over the posterior portal.
After endoscopic resection of IOL, histopathological confirmation of the diagnosis can prove to be difficult though. Continuous irrigation is needed to obtain clear vision of the cavity and all lipomatous tissue will be washed out promptly. Where present, dystrophic calcifications can be extracted and sent for histopathological analysis. Alternatively, specimen of lipomatous intraosseous tissue can be saved for further analysis once the first portal for ossoscopy has been established. Without endoscopic vision and irrigation a percutaneous biopsy can produce enough representative tissue for a precise histopathological diagnosis in most cases. For UBC, the inner lining of the bone cavity will not be washed out by endoscopic irrigation and samples can easily be saved for further diagnosis by ossoscopic resection.
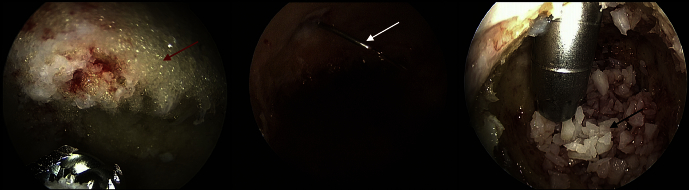
Before allogenic grafting, the cavity is rinsed with 95% ethanol (20-mL Ampulla, Braun, Melsungen, Germany) as a local adjuvant therapy ensuring denaturization of remaining cyst membranes (Fig 3). The application time for the ethanol should not exceed 2 to 3 minutes, and after intermittent thorough irrigation with sterile saline solution, this procedure is repeated 2 to 3 times. The ethanol should not get in contact with any soft tissue to avoid damage to sensible structures like the sural nerve.
Fig 3.
Left to right: resection of the remaining fat tissue (red arrow) of intraosseous lipoma with an arthroscopic shaver, percutaneous irrigation with 95% ethanol through a cannula (white arrow), and grafting with allogenic cancellous bone under ossoscopic control. In this older case, a hollow bone punch originally used for bone biopsies was used to facilitate the process of plombage (black arrow). Again, all instruments in this figure are introduced over the posterior portal, whereas ossoscopy is performed over the anterior portal enabling an excellent overview.
Bone Plombage
For grafting, allogenic cancellous bone (Cancellous Bone Chips <1 cm, DIZG, Berlin, Germany) is our preferred choice for plombage of the cavity. The bone chips are further morselized with a Luer plier to simplify handling (Table 1). Compared with autologous bone or bone substitute, allogenic bone is easily available, affordable, and can offer good osteoinductive and osteoconductive properties.18 The major advantage is to avoid sacrificing host tissue.19 For easy application of the morselized allogenic cancellous bone chips, a small 3-mm Boucheron ear speculum (Aesculap, Tuttlingen, Germany) is introduced through one of the ossoscopy portals. To our experience, this device has proved to be easier to handle compared with previously used instruments like a pedicle filler (borrowed from spine surgery) or a hollow bone punch, originally used for biopsies. Under endoscopic vision through the second portal, impaction of the bone graft is performed intermittently (Figs 4 and 5). After final fluroscopic control, both portals can be sealed with an absorbable haemostatic gelatin sponge (Spongostan, Ethicon, Norderstedt, Germany) to avoid accidental leakage of the bone graft.
Table 1.
Pearls and Pitfalls of Calcaneal Ossoscopy With Allogenic Bone Grafting
| 1. The amount of allogenic cancellous bone needed for plombage can be estimated either by accurate preoperative planning on cross-sectional imaging or by injection of a defined volume of sterile saline solution during the surgical procedure. |
| 2. In case of intraosseous lipoma, ossoscopic visibility can be impaired by lipomatous tissue at first and clear vision can often only be established after irrigation through a second portal. |
| 3. During the process of resection of the tumor and cleaning of the bone cavity, the allogenic cancellous bone chips are soaked in sterile saline solution and morselized by an assistant for easy handling. |
| 4. In case of intraosseous lipoma, histopathological biopsies should be performed before irrigation starts—otherwise all lipomatous loose tissue will be washed out promptly. |
| 5. In small cysts with a diameter of 3 cm or less, both instruments for ossoscopy might interfere with each other and complicate handling. |
| 6. In small cysts, the portal of a standard arthroscope (4.0 mm) and the portal for grafting (4.0 mm) can prove to be oversized and cause unintentional damage to the egg shell-like calcaneal cortex. |
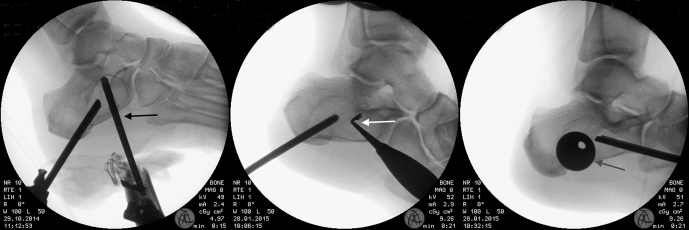
Fig 4.
Minimally invasive bone grafting made easy through an ear speculum (left, black arrow). Impaction of the cancellous bone chips with a curved bone tamp (right, white arrow). The patient is in a left lateral position, with the affected right rearfoot facing upward on the operation table. The black asterisk (*) marks the lateral malleolus.
Fig 5.
Lateral view of a right rearfoot with fluroscopic documentation of ossoscopic shaving (left, black arrow), curettage with a sharp spoon (middle, white arrow), and introduction of the ear speculum for plombage of the bone cavity (right, gray arrow).
Postoperative Care
After wound closure, the foot is immobilized in a semirigid lower leg orthosis. Partial weight bearing is advised for 6 weeks and impact sports should be avoided for a minimum of 3 months postop. A radiologic follow-up is performed 6 and 12 weeks and 12 months postop with plain radiography. Repeated MRI after complete resection of lipoma of bone is usually not required as recurrence is very rare.3
Tips and Tricks
Tables 1 and 2 present pearls and pitfalls as well as advantages and risks of our technique.
Table 2.
Advantages and Limitations of Calcaneal Ossoscopy With Allogenic Bone Grafting
| 1. Minimally invasive procedure: less soft-tissue dissection, lower risk of iatrogenic sural nerve damage. |
| 2. Compared with injectable bone substitutes, allogenic cancellous bone is mostly less expensive and might prove favorable regarding osteointegration. |
| 3. Compared with injectable bone substitutes, grafting with allogenic cancellous bone is more time-consuming. |
| 4. Compared with traditional open surgery for calcaneal bone cyst and intraosseous lipoma, calcaneal ossoscopy is a more demanding surgical procedure requiring experience in arthroscopic techniques, foot and ankle surgery, and tumor orthopedics. |
Discussion
Musculoskeletal tumors and tumor-like lesions of the calcaneus are rare but have to be taken into consideration for chronic heel pain.20 To avoid pathological fracture, large lesions are recommended for prophylactic surgical therapy, even if the patient is free of symptoms.8 Traditionally, symptomatic cases of IOL or UBC were treated with open curettage and bone grafting. As an advantage to open curettage with a longitudinal incision parallel to the planta pedis or a classic L-shaped incision, minimally invasive ossoscopy can diminish the risk of impaired wound healing and speed up superficial wound healing.9 Several studies demonstrated that minimally invasive ossoscopy can offer a safe alternative to open surgical procedures.9, 14, 15, 16 Compared with endoscopic resection and filling with injectable bone substitute, allogenic bone grafting is both less expensive21 and might prove biologically superior. As a modification of previously reported procedures, the use of an ear speculum, as described in our technique, can considerably facilitate the process of grafting with cancellous bone chips. This proved advantageous over previously used instruments for percutaneous grafting. We experienced that meticulous ossoscopic curettage of IOL with resection of dystrophic calcifications was more time-consuming than in UBC. Operation time of our procedure might be additionally cut down by the use of injectable bone substitute, but, in our experience, osteointegration is inferior to allogenic bone, adverse effects have been reported,22 and, last but not least, cost-effectiveness is mostly disadvantageous.21 Limitations for this procedure include that in our experience bone lesions smaller than 3 cm in diameter in the sagittal plane are not suitable for ossoscopy with a standard 4.0-mm arthroscope as both portals can brake out and form one large opening because of their close proximity to each other. Alternatively to a mini-open surgery, ossoscopy with a small-joint arthroscope of 2.7 mm and percutaneous injection of a bioresorbable bone substitute can be discussed.
Footnotes
The authors report the following potential conflict of interest or source of funding: A.T. is an instructor for Arthrex Foot and Ankle Surgery Courses.
Supplementary Data
Calcaneal ossoscopy performed with a standard 4-mm arthroscope. The patient is in a stable lateral position under general anesthesia; the lateral aspect of the rearfoot faces upward on the operation table. Only after a second portal has been established, lipotamous tissue can be washed out. Calcifications are removed with an arthroscopic shaver and grasper. The inner lining of the bone cavity is sent for histopathological analysis. Rinsing with 95% ethanol reduces risk of recurrence before grafting with allogenic cancellous bone is performed through an ear speculum.
References
- 1.Pappas A.J., Haffner K.E., Mendicino S.S. An intraosseous lipoma of the calcaneus: A case report. J Foot Ankle Surg. 2014;53:638–642. doi: 10.1053/j.jfas.2014.03.007. [DOI] [PubMed] [Google Scholar]
- 2.Freyschmidt J.O., Ostertag H., Jundt G. Springer; Berlin: 2010. Knochenutmoren mit Kiefertumoren: Klinik-Radiologie-Pathologie. [Google Scholar]
- 3.Fletcher C., Bridge J.A., Hogendoorn P.C.W., Mertens F. WHO; Lyon, France: 2013. World Health Organization classification of tumours. [Google Scholar]
- 4.Diard F., Hauger O., Moinard M., Brunot S., Marcet B. Pseudo-cysts, lipomas, infarcts and simple cysts of the calcaneus: Are there different or related lesions? JBR-BTR. 2007;90:315–324. [PubMed] [Google Scholar]
- 5.Weger C., Frings A., Friesenbichler J. Osteolytic lesions of the calcaneus: Results from a multicentre study. Int Orthop. 2013;37:1851–1856. doi: 10.1007/s00264-013-2042-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Takada J., Hoshi M., Oebisu N. A comparative study of clinicopathological features between simple bone cysts of the calcaneus and the long bone. Foot Ankle Int. 2014;35:374–382. doi: 10.1177/1071100713519600. [DOI] [PubMed] [Google Scholar]
- 7.Sung A.D., Anderson M.E., Zurakowski D., Hornicek F.J., Gebhardt M.C. Unicameral bone cyst: A retrospective study of three surgical treatments. Clin Orthop Relat Res. 2008;466:2519–2526. doi: 10.1007/s11999-008-0407-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pogoda P., Priemel M., Linhart W. Clinical relevance of calcaneal bone cysts: A study of 50 cysts in 47 patients. Clin Orthop Relat Res. 2004:202–210. doi: 10.1097/01.blo.0000128297.66784.12. [DOI] [PubMed] [Google Scholar]
- 9.Yildirim C., Akmaz I., Sahin O., Keklikci K. Simple calcaneal bone cysts: A pilot study comparing open versus endoscopic curettage and grafting. J Bone Joint Surg Br. 2011;93:1626–1631. doi: 10.1302/0301-620X.93B12.27315. [DOI] [PubMed] [Google Scholar]
- 10.De Wilde V., De Maeseneer M., Lenchik L., Van Roy P., Beeckman P., Osteaux M. Normal osseous variants presenting as cystic or lucent areas on radiography and CT imaging: A pictorial overview. Eur J Radiol. 2004;51:77–84. doi: 10.1016/S0720-048X(03)00180-3. [DOI] [PubMed] [Google Scholar]
- 11.Sirry A. The pseudo-cystic triangle in the normal os calcis. Acta Radiol. 1951;36:516–520. doi: 10.3109/00016925109177004. [DOI] [PubMed] [Google Scholar]
- 12.Ulucay C., Altintas F., Ozkan N.K., Inan M., Ugutmen E. Surgical treatment for calcaneal intraosseous lipomas. Foot. 2009;19:93–97. doi: 10.1016/j.foot.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 13.Levy D.M., Gross C.E., Garras D.N. Treatment of unicameral bone cysts of the calcaneus: A systematic review. J Foot Ankle Surg. 2015;54:652–656. doi: 10.1053/j.jfas.2014.10.014. [DOI] [PubMed] [Google Scholar]
- 14.Mainard D., Galois L. Treatment of a solitary calcaneal cyst with endoscopic curettage and percutaneous injection of calcium phosphate cement. J Foot Ankle Surg. 2006;45:436–440. doi: 10.1053/j.jfas.2006.09.014. [DOI] [PubMed] [Google Scholar]
- 15.Innami K., Takao M., Miyamoto W., Abe S., Nishi H., Matsushita T. Endoscopic surgery for young athletes with symptomatic unicameral bone cyst of the calcaneus. Am J Sports Med. 2011;39:575–581. doi: 10.1177/0363546510388932. [DOI] [PubMed] [Google Scholar]
- 16.Futani H., Fukunaga S., Nishio S., Yagi M., Yoshiya S. Successful treatment of bilateral calcaneal intraosseous lipomas using endoscopically assisted tumor resection. Anticancer Res. 2007;27:4311–4314. [PubMed] [Google Scholar]
- 17.Muramatsu K., Tominaga Y., Hashimoto T., Taguchi T. Symptomatic intraosseous lipoma in the calcaneus. Anticancer Res. 2014;34:963–966. [PubMed] [Google Scholar]
- 18.Oryan A., Alidadi S., Moshiri A., Maffulli N. Bone regenerative medicine: Classic options, novel strategies, and future directions. J Orthop Surg Res. 2014;9:18. doi: 10.1186/1749-799X-9-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Greenwald A.S., Boden S.D., Goldberg V.M. Bone-graft substitutes: Facts, fictions, and applications. J Bone Joint Surg Am. 2001;83-A(suppl 2, pt 2):98–103. doi: 10.2106/00004623-200100022-00007. [DOI] [PubMed] [Google Scholar]
- 20.Lenze U., Stolberg-Stolberg J., Pohlig F. Unicameral bone cyst in the calcaneus of mirror image twins. J Foot Ankle Surg. 2015;54:754–757. doi: 10.1053/j.jfas.2014.09.017. [DOI] [PubMed] [Google Scholar]
- 21.Kurien T., Pearson R.G., Scammell B.E. Bone graft substitutes currently available in orthopaedic practice: The evidence for their use. Bone Joint J. 2013;95-B:583–597. doi: 10.1302/0301-620X.95B5.30286. [DOI] [PubMed] [Google Scholar]
- 22.Lee G.H., Khoury J.G., Bell J.E., Buckwalter J.A. Adverse reactions to OsteoSet bone graft substitute, the incidence in a consecutive series. Iowa Orthop J. 2002;22:35–38. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Calcaneal ossoscopy performed with a standard 4-mm arthroscope. The patient is in a stable lateral position under general anesthesia; the lateral aspect of the rearfoot faces upward on the operation table. Only after a second portal has been established, lipotamous tissue can be washed out. Calcifications are removed with an arthroscopic shaver and grasper. The inner lining of the bone cavity is sent for histopathological analysis. Rinsing with 95% ethanol reduces risk of recurrence before grafting with allogenic cancellous bone is performed through an ear speculum.