Abstract
Objective
The purpose of this randomized trial was to investigate the efficacy of two behavioral treatments focusing on different change mechanisms in ameliorating a borderline personality disorder constellation of behaviors and substance use in adolescents referred by juvenile diversion programs.
Methods
Forty adolescents 14 to 17 years of age and meeting DSM IV criteria for borderline personality disorder and substance use disorders were randomized to Integrative Borderline Personality Disorder-Oriented Adolescent Family Therapy (I-BAFT) or Individual Drug Counseling (IDC). This design allowed a comparison of two manualized interventions, one family-based and one individually-oriented. Profiles of clinical change were used to detect impact and to estimate treatment effect sizes.
Results
Primary analyses showed that both interventions had a clinically significant impact on borderline personality disorder behaviors 12 months after baseline but with no differential treatment effects. The impact on substance use was more complex. Subgroup analyses revealed that adolescents with depression had significantly more severe profiles of borderline personality disorder and substance use. These youth were the only group to show reductions in substance use, but only if they received the I-BAFT intervention. Study data also documented the high dosage of intensive residential treatment needed by this population.
Conclusions and Implications for Practice
Results highlight the intensive treatment needs of juvenile justice involved youth with co-occurring substance use and borderline personality disorder including depression, the hybrid outpatient and residential treatment often required by this population, and the promise of a family oriented approach particularly for youth with severe symptoms and co-occurring depression.
Many adolescents in the juvenile justice system need specialized mental health and substance abuse treatments, which are often offered via diversion programs (Cocozza, Veysey, Chapin, Dembo, Walters, & Farina, 2005). Entry into the juvenile justice system may be triggered by mental disorders, court mandated assessment at a Juvenile Addiction Receiving Facility, or by an offense not formally linked to a mental or substance use disorder. Regardless of the point of entry, youth in the juvenile justice system often display an array of mental health problems, many masked by unlawful activity and problem behaviors. Family-based and multisystemic treatments have been used successfully with court-involved adolescents (Henggeler & Sheidow, 2012) although continued research is needed to understand the challenges that emerge when treating adolescents and young adults presenting with both substance use disorders and severe co-occurring psychiatric disorders or personality disorders (Farrand, Booth, Gilbert, & Lankshear, 2009).
One body of research that has consistently focused on adolescents with severe symptom clusters is found in the literature on adolescent Borderline Personality Disorders (Miller, Rathus, DuBose, Dexter-Mazza, & Goldklang, 2007). In a recent study, adolescent borderline personality disorder symptoms predicted lower social functioning, worse academic and occupational attainment, greater general impairment, and increased use of health care services even 20 years later (Winograd, Cohen, & Chen, 2008). Bernstein (1997) found that adolescents with borderline personality disorder were 13 times more likely than youth without borderline personality disorder to maintain the symptoms and receive a borderline personality disorder diagnosis two years later. While there is not always agreement on whether adolescents should be diagnosed with borderline personality disorder, these studies have shown that it is possible to identify adolescents displaying a profile of co-occurring substance use, impulsivity, and self-harm behaviors that often require multiple residential/inpatient hospitalizations and that endure over time if not properly treated. The handful of available randomized trials with adolescents with sub-syndromal or full-syndromal borderline personality disorder have reported mixed results suggesting reduced borderline personality disorder symptoms but few differential treatment effects (Chanen et al., 2008; Schuppert et al., 2009).
Comorbid depression has emerged as a particularly interesting and impactful condition. A meta-analysis by Newton-Howes, Tyrer, & Johnson (2006) found that individuals with co-occurring personality disorder and depression were about twice as likely to have worse treatment outcomes. Less evidence exists for adolescents, but Warden and colleagues (2012) showed that adolescents in treatment for drug use with co-occurring depression reported more drug use at baseline and higher use throughout the course of treatment. Interestingly, there is some evidence that family-based treatments may be particularly useful for adolescents with the most severe profiles of substance use and psychiatric co-morbidity (Henderson, Dakof, Greenbaum, & Liddle, 2010).
The comparison of interventions based on different frameworks can be useful in identifying the best possible treatment for substance abuse in adolescents. Because of the likelihood that borderline behavior and substance use can easily trigger each other, we sought to develop a treatment that would combine one of the most effective interventions for adolescent substance abuse (i.e., family therapy) with components of one of the most effective interventions for Borderline Personality Disorder (i.e., DBT skills). The newly developed intervention sought to address both problems simultaneously through individual and family focused work (Integrative BPD-oriented Adolescent Family Therapy; I-BAFT; Santisteban, Muir, et al., 2003). An alternative treatment approach is to focus squarely on the primary symptom of substance use. Individual Drug Counseling is a manualized intervention originally designed for adults but used with adolescents with opioid dependence in a National Institute on Drug Abuse study (Subramaniam, et al., 2011). IDC is based on the 12-step philosophy that conceptualizes addiction as a complex problem that damages the substance using individual physically, mentally, and spiritually (Mercer & Woody, 1999). The IDC treatment can address depression and other relevant emotions that emerge as triggers to use but it is not specifically designed to do so.
The purpose of this randomized trial was to investigate the efficacy of two behavioral treatments for adolescents with borderline personality disorder and substance abuse. We compared two bona fide manualized treatments with equivalent dosage, but with different targets for intervention (family-based and focused on co-occurring psychiatric disorders vs. individually-based and focused almost exclusively on drug use). All of the participants met criteria for substance abuse and borderline personality disorder but only a third (38%) had comorbid depression. This profile allowed us to investigate how depression might impact all of our variables of interest. The research objectives of this study were to investigate: 1) the clinical and drug use profile of our sample, 2) the feasibility/acceptability (therapeutic alliance and outpatient sessions received) of individual and family treatments in this sample, 3) whether I-BAFT was more effective at changing borderline behaviors and substance use than IDC, and 4) the amount of intensive/emergency residential treatment needed, in addition to outpatient sessions, to address the severe clinical profile of this sample. In addition, for each of the research questions above, we also investigated the effect of co-morbid depression.
Method
Participants
Forty adolescentsages14 to 17 years who met DSM-IV criteria for Substance Abuse and borderline personality disorder were included in the study. It should be noted that an adolescent could meet the eligibility criteria for Substance Use Disorder based on the last 12 months, even if there was no documented use in the past 30 days. This sample size of 15–30 cases per condition is consistent with guidelines for the early stage testing of new innovative treatments (Rounsaville, Carroll, & Onken, 2001). The adolescents and at least one caregiver in each family participated in assessments and treatment at a university center in South Florida. Table 1 shows characteristics of adolescents and primary caregivers. Sixty-five percent of the youth reported being arrested or detained at a police station during the past year. About two-thirds of youth were referred from the juvenile justice system: 38% Miami-Dade Juvenile Services Department (JSD), and 32% Juvenile Addictions Receiving Facility (JARF) (30% were referred by school counselors or the community in general).
Table 1.
Baseline characteristics of Adolescents and Primary Caregivers.
| Variable | I-BAFT | IDC |
|---|---|---|
| Adolescents | ||
| Age, years, M (SD) | 16.0 (0.8) | 15.6 (0.8) |
| Male, N (%) | 12 (60) | 13 (65) |
| Hispanic, N (%) | 16 (80) | 18 (90) |
| Primary Caregivers | ||
| Age, years, M (SD) | 46.58 (6.5) | 43.85 (6.4) |
| Hispanic, N (%) | 16 (84.2) | 17 (85.0) |
| Married, N (%) | 6 (32) | 8 (40) |
| Separated, N (%) | 5 (26) | 0 (0) |
| Single, N (%) | 1 (5) | 5 (25) |
| Divorced, N (%) | 6 (32) | 7 (35) |
| Widowed, N (%) | 1 (5) | 0 (0) |
| Less than High School, N (%) | 4 (21) | 7 (35) |
| High School Degree, N (%) | 6 (32) | 5 (25) |
| Technical Degree, N (%) | 1 (5) | 1 (5) |
| 2 Year Degree, N (%) | 5 (26) | 4 (20) |
| 4 Year Degree, N (%) | 1 (5) | 3 (15) |
| Master’s Degree, N (%) | 2 (11) | 0 (0) |
Note. No differences between intervention conditions at p < .05.
Participants referred through JSD were in diversion programs that focused on youth who had committed a minor first-time misdemeanor offense. Although not formally arrested, the youth from JSD were assigned a case worker and were evaluated to determine their individual needs. Adolescents also comply with specific program mandates including completing community service hours, attending school or being legally employed, and receiving treatment for mental health and/or substance abuse issues when appropriate. Youth were monitored by a JSD case worker for approximately four months.
The Juvenile Addiction Receiving Facility is a secure, locked facility that provides assessment and referral to youth who are using alcohol and drugs. Youth enter the JARF either voluntarily or involuntarily (Court order through the Florida Marchman Act, JSD), are in crisis due to substance abuse, and remain at the JARF for 3–5 days. Through a comprehensive assessment, the JARF determines the youth’s treatment needs and assists with placement in appropriate intervention programs prior to discharge. Youth who are involuntarily placed there are required to comply with the JARF assessment and to receive the assigned treatment. The court may impose legal consequences for lack of compliance.
Procedures
The study was approved by the university IRB and all participating family members provided written consent or assent. It is important to note that although the participants referred from JSD and the JARF were legally required to receive treatment, our program was voluntary. All participants were informed that they had the right to refuse to participate in research and could be offered treatment outside of a research study. This was also spelled out in the informed consent document, which parents and youth signed prior to enrollment.
All procedures and treatments were offered in English or Spanish. After completing the intake assessment participants were assigned to one of two conditions using permuted block randomization: Integrative borderline personality disorder-oriented Adolescent Family Therapy (I-BAFT) or Individual Drug Counseling (IDC). Randomization was stratified by gender, race/ethnicity, and drug use severity in the past 30 days. Data were collected at baseline, four-months, eight-months, and 12-months post baseline at the university center (See CONSORT Figure 1).
Figure 1.
CONSORT participant flow diagram. Analysis of clinically significant change used multiple imputation for cases with data missing at the 12-month follow-up.
Measures
Measures were selected that had strong psychometric properties and were available in Spanish and English. Bachelors-level assessors with several years of experience and who were fluent in Spanish and English completed all interviews with participants. Assessors were not blind to the intervention.
Borderline Personality Disorder Diagnosis
Borderline personality disorder diagnosis was determined at baseline using the Revised Diagnostic Interview for Borderlines (DIB-R; Kolb & Gunderson, 1980) a semi-structured interview that assesses five functional areas: social adaptation, impulse/action patterns, affect, psychosis, and interpersonal relations.
Therapeutic Alliance
Therapeutic alliance between the therapist and the adolescent was measured using adolescent and therapist reports from the Working Alliance Inventory (Horvath & Greenberg, 1989) which was collected on a monthly basis during the intervention. This instrument measures the level of collaboration, agreement, and emotional connection between therapist and client. Items were rated on a 1 (never) to 7 (always) point Likert scale and were averaged into a single total score separately for therapists and adolescents. The reliability for the total score used in this study ranged from .95 – .98 for client reports and .91 – .96 for therapist reports. To correct for extreme negative skew in the alliance scores, both therapist and client reports were transformed into two separate categorical variables.
Outpatient Sessions
Outpatient sessions were defined as the number of planned sessions received as part of either intervention condition during the treatment phase. In I-BAFT, sessions could be family, individual, or skills building sessions. In IDC, all but a few sessions were individual sessions. Any services that were received outside of this study were not included in this count.
Borderline Personality Disorder behaviors
A dimensional score of the borderline personality disorder constellation was obtained using the adolescent report on the Borderline Personality scale from the Millon Adolescent Clinical Inventory (MACI; Millon, 1993). The Base Rate was calculated using gender and age norms. In this sample, reliability was good at all assessments (αs range .78 – .88). For analysis, a dichotomous variable was created: borderline personality disorder behavior was coded as not functional (Base Rate > 60) vs. functional (Base Rate ≤ 60).
Depression
Depression was measured with the Diagnostic Interview Schedule for Children-Predictive scales (DPS; Lucas et al., 2001), a brief screening instrument was administered at baseline and matched to DSM-IV diagnoses a child would “likely” receive if given a full diagnostic interview. Adolescents and caregivers were interviewed separately using the structured interview and adolescents were categorized as having depression at baseline if they met criteria on either caregiver or adolescent reports, i.e., the participant was given the diagnosis if either the parent or adolescent endorsed the number of symptoms for each disorder. For this study, the DPS covered 30 days before baseline.
Substance use
Substance use was measured using the Timeline Follow back (TLFB; Sobell et al., 2003) and urine toxicology. The TLFB obtains retrospective adolescent reports of daily substance use with a 30-day calendar to stimulate recall and gathers information on specific substances used and days used, and has been used with juvenile justice populations (Haliday-Boykins, Schaeffer, Henggeler, Chapman, Cunningham, Randall, & Shapiro, 2010). A urine sample was collected from each participant up to twice monthly (after a treatment session chosen randomly) and at each of the main assessment time-points. Urine samples were sent to a certified laboratory for analyses to identify amphetamine, marijuana, cocaine, opiate, phencyclidine (PCP), methamphetamine, barbiturate, and benzodiazepine use. For certain analysis the TLFB and urine toxicology were combined into a single dichotomous variable: substance use was coded as positive for a single time-point if any of the samples were positive for use or there was any self-reported use and negative if all of the samples were negative for use and there was no self-reported use.
Residential Days of Treatment
Data on several types of services were collected at baseline and every two months post-baseline to investigate the types of emergency services typically needed by this population. Hospitalization for psychiatric problems and residential treatment for deteriorating drug problems were combined into a single Residential Treatment category. This category includes residential treatment received during two periods: during the treatment and follow-up phases.
Interventions
Integrative borderline personality disorder-oriented Adolescent Family Therapy (I-BAFT)
I-BAFT is a manualized treatment that adapted individual interventions and skills training modules from Dialectic Behavior Therapy (DBT; Linehan, 1993) and family interventions from Structural Family Therapy (Minuchin & Fishman, 1981). I-BAFT targets factors that directly contribute to adolescent drug abuse and other self-harm behaviors such as emotion dysregulation and impulsivity, failure to establish life goals and ineffective life skills, unstable family attachment, and maladaptive family interactions (Santisteban, Muir, Mena, & Mitrani, 2003). I-BAFT delivered weekly family therapy, individual therapy, and skills building interventions in a two session per week format over a seven-month period. One family session and either a skills training or an individual session with the adolescent were scheduled weekly. Separate therapists and skills trainers were used as recommended for DBT (Linehan, 1993). In this study each I-BAFT therapist was the primary therapist (family and individual) for half of the participating families and the skills trainer for the other half. Therapists were trained by I-BAFT’s developer.
Individual Drug Counseling (IDC)
IDC was an active and bona fide comparison condition in this study. IDC is a manualized individually oriented substance abuse intervention that has been used with both adults and adolescents (Subramaniam, et al., 2011). The foundation of IDC is the 12-step philosophy which seeks to address addiction from the physical, mental, and spiritual perspectives (Mercer & Woody, 1999). An experienced trainer from the team that developed the IDC intervention conducted the training for the IDC clinicians in the study. IDC was administered in a two session per week format implemented over a seven-month period that matched the dosage in I-BAFT. All sessions were conducted as individual sessions with the adolescent except for a monthly family meeting with caregivers. Goals of the IDC manual included: 1) identifying signs and symptoms of addiction and triggers to use; 2) recognizing and re-channeling urges to use drugs; 3) increasing motivation to achieve and sustain abstinence; 4) becoming accountable for episodes of use; 5) developing new and more effective problem-solving strategies; 6) connecting with the 12-step philosophy and participating in NA, AA, and/or CA; and 7) improving self-esteem by practicing newly acquired coping skills and problem-solving strategies at home and in the community (Mercer & Woody, 1999).
Therapists
Therapists for the two conditions were eight masters-level and doctoral-level therapists with substantial experience in the treatment of substance abusing adolescents. Each therapist was trained by an expert in their respective conditions and met weekly with a supervisor and fellow therapists to view videotaped therapy sessions and to discuss the implementation of the manualized interventions with a high degree of adherence and fidelity. Therapists were nested in conditions with four therapists delivering IDC and four therapists delivering IBAFT.
Results
Participant’s Clinical Profiles at Baseline
Preliminary analyses focused on the characteristics of adolescents and their caregivers at baseline, and also tested for any pre-treatment differences between participants in the two intervention conditions. Due to the small sample size of this study, analyses relied on clinical change and effect sizes to detect promising treatment patterns worthy of further research. Baseline profiles of adolescent substance use and borderline personality disorder behaviors are found in Table 2. Substance use was fairly even across the two conditions, although there was a non-significant trend for differences between conditions (likely due to more daily users in I-BAFT). All participants reported that they had used marijuana and alcohol in their lifetime; over half reported lifetime cocaine use. Recent (past 30 days) marijuana use was reported by 85% of the sample; 56% reported recent alcohol use. Youth reported severe symptoms; eleven (28%) adolescents had been in residential treatment in the year prior to the study, with an average stay of 37.27 (SD = 37.89) days, but clearly symptoms persisted.
Table 2.
Baseline Clinical Profiles of Participants in Each Intervention Condition.
| I-BAFT (n = 20) | IDC (n = 20) | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| Baseline Clinical Status | n | % | n | % | χ2 | p |
| Depression | 7 | 35% | 8 | 40% | 0.11 | .744 |
| Non-Functional BPD Behavior | 13 | 65% | 12 | 60% | 0.11 | .744 |
| Any Alcohol Use (past 30 days)a | 11 | 59% | 11 | 55% | 0.03 | .855 |
| Any Marijuana Use (past 30 days)a | 15 | 79% | 18 | 90% | 0.91 | .339 |
| Substance Usea | 7.35 | .062 | ||||
| Abstainer | 3 | 16% | 1 | 5% | ||
| Weekly | 8 | 42% | 12 | 60% | ||
| Frequent | 2 | 11% | 6 | 30% | ||
| Daily | 6 | 32% | 1 | 5% | ||
Note. IDC = Individual Drug Counseling; I-BAFT = Integrative BPD-oriented Adolescent Family Therapy.
One participant in I-BAFT refused to report level of substance use at baseline.
Subgroups based on comorbid depression
We conducted subgroup analyses with the sample divided into adolescents with and without co-morbid depression. Adolescents with depression had significantly greater self-reported substance use, B = 1.00, SE = 0.34, p = .004, 95%CI [0.32, 1.69], non-functional borderline behavior, B = 2.93, SE = 1.12, p = .009, 95%CI [0.73, 5.12], OR = 18.63, and twice the odds (OR = 2.00) of having a positive urine results, although this difference was not significant, B = 0.69, SE = 0.72, p = .335, 95%CI [−0.72, 2.11].
Feasibility and Acceptability
Therapeutic Alliance
We tested for differences in the therapeutic alliance (as reported by adolescents and therapists) between the two intervention conditions. Generalized Estimating Equations was used to account for repeated measures across time when analyzing differences in therapeutic alliance scores. Most (91%) therapists and adolescents (84%) reported high alliance throughout therapy in both conditions. There was no difference between conditions in adolescent-reported alliance, B = −1.08, SE = 0.80, p = .174, 95%CI [−2.65, 0.48], or therapist-reported alliance, B = −1.21, SE = 0.72, p = .095, 95%CI [−2.63, 0.21], although there was a trend for better therapist-reported alliance in IDC.
Subgroup Analysis
There were no differences between youth with co-morbid depression and those without co-morbid depression in adolescent-reported alliance, B =0.49, SE = 0.96, p= .615, 95% CI [−1.41, 2.38], or therapist-reported alliance, B =0.61, SE = 0.68, p = .371, 95% CI [−0.73, 1.94]. There was no intervention condition x comorbidity interaction on adolescent-reported alliance, B = −0.01, SE = 1.33, p= .997, 95% CI [−2.61, 2.62], or therapist-reported alliance, B = −1.66, SE = 1.44, p= .250, 95% CI [−4.50, 1.17].
IDC/BAFT Outpatient Sessions Received
Participants in both conditions attended a considerable number of outpatient sessions (IDC: M = 20.90, SD=12.07; I-BAFT: M = 27.15, SD=14.76). The distribution of types of sessions (individual, family, and skills focused) was consistent with the parameters of the distinct interventions and the research design. That is, participants in IDC received significantly more individual sessions, and significantly fewer family sessions and skills sessions than did the I-BAFT participants. ANOVA were used to examine differences in the number of outpatient sessions each adolescent and/or family received. The total number of sessions was not different between the two conditions, F(1, 38) = 2.15, p = .151.
Subgroup analysis
Co-morbid depression was not related to the number of sessions, F(1, 36) = 3.18, p = .325. Comorbid depression did not significantly interact with intervention condition, F(1, 36) = 0.60, p = .445. However, in IDC there was a large-size difference in outpatient sessions between adolescents without co-morbid depression (M = 24.67, SD = 8.19) and those with co-morbid depression (M = 15.25, SD = 15.14, F(1, 18) = 3.27, p = .087, Cohen’s d = .77). In I-BAFT, there was only a small difference in outpatient sessions between adolescents without co-morbid depression (M = 28.08, SD = 15.37) and those with co-morbid depression (M = 25.43, SD = 14.57, F(1, 18) = 0.14, p = .713, Cohen’s d = .18). Figure 2 shows the number of outpatient sessions (left side) for participants in each intervention condition, divided by co-morbid depression profile.
Figure 2.

Estimated number of outpatient sessions and residential sessions during the treatment and follow-up phases. (N=40)
Profiles of Clinical Change
Differential treatment effects were investigated using an analysis of the profile of clinical change in substance use and analysis of clinically significant change (Jacobson & Truax, 1991) in borderline personality disorder behavior from baseline to the 12 month follow-up. Our substance use measure did not allow for the formal steps recommended by Jacobson and Truax (1991) but we replicated a strategy used successfully in similar adolescent drug treatment trials (e.g., Santisteban, Coatsworth, et al., 2003). Each analysis was conducted first using the overall sample and then separately for the depressed and non-depressed groups. The formal analysis of clinical significance involved two steps: (1) determining whether participants have statistically reliable change; and (2) categorizing participants according to clinical cut-points. Different definitions of change, i.e., different cut-points, were used for substance use and borderline personality disorder behaviors.
Definition of Change in borderline personality disorder Behavior
Using the more formal criteria for clinically significant change for borderline personality disorder behavior, participants were categorized as follows: 1) recovered–participants with scores in the clinical range at intake, with statistically reliable reductions in scores and MACI base rates less than 60 at the 12-month follow-up; 2) improved–participants with statistically reliable reduction in scores, but with scores in the clinical range at follow-up; 3) unchanged, non-clinical– participants who did not show statistically reliable change in scores but were not in the clinical range at follow-up; 4) unchanged, clinical– participants who did not show statistically reliable change in scores and remained in the clinical range at follow-up; and 5) deteriorated–participants with statistically reliable increases in scores at follow-up.
Definition of Change in Substance Use
For substance use, participants were first categorized into four levels of drug use that have been previously used in the substance use treatment literature (Brook, et al., 1998; Santisteban, Coatsworth, et al., 2003). The categories were based on adolescent-reported substance use at baseline and the 12-month follow-up. They are as follows: abstinence (no substance use); weekly use (1 to 8 days of use); frequent use (9 to 16 days of use); and daily use (17 or more days of use). These categories, along with urine toxicology, were then used to calculate clinical change. The more formal test of clinically significant change was not possible due to the absence of normative and reliability information for self-reported substance use. For our change profile, participants were categorized as follows: 1)recovered– participants reporting decreased use (moving to a category representing less use) and negative urine screen and self-reported abstinence at the last follow-up; 2) improved– participants with decreased use, but not abstinence at follow-up; 3) unchanged, – clean participants who showed no sign of use at intake or follow-up; 4) unchanged, dirty – participants showing no change in use category and signs of use at both baseline and follow-up; and 5) deteriorated – participants with increased use at the last follow-up. An examination of TLFB and UDS data from intake, show high levels of agreement between the two measures: 8% were negative on both; 59% were positive on both. However, both measures detected use when the other did not: 5% of the cases that self-reported no use had positive UDS; 28% of cases that had a negative UDS self-reported use.
Missing Data Strategy
About a third of cases had missing data (33% self-reported substance use, 38% urine samples, and 33% borderline personality disorder behavior) at the 12 month assessment due in large part to hospitalizations/residential stays. Any assessments collected in these settings would have supplied misleading data on drug use and other symptoms. Before performing the analyses of clinically significant change, we used multiple imputation to recapture the missing variability (Enders, 2010; Graham, 2009). Multiple imputation has been recommended as a “state of the art” technique to account for missing data (Schafer & Graham, 2002) because it requires fewer assumptions about the missing data mechanism. Simulation studies have shown that it typically produces more accurate estimates than other techniques (e.g., listwise deletion, mean substitution). Using simulation studies, Graham & Schafer (1999) showed that multiple imputation is effective with sample sizes comparable to this study with as much as 50% missing data from most variables, even in complex models. Previous psychological and legal studies have successfully used multiple imputation with samples of comparable size to the current study (e.g., Wimberly, Carver, Laurenceau, Harris, & Antoni, 2005; Maguire, 2009). Multiple imputation uses a regression-based procedure to generate multiple copies of the data set, each with different estimates of the missing values. We used Norm 2.03 (Schafer, 1997) to generate 100 imputed datasets for substance use and 100 for borderline personality disorder behavior. These were imputed separately due to the ratio of variables to be imputed to sample size. Exploratory analyses suggested that the datasets be separated by 925 iterations for substance use and 196 iterations for borderline personality disorder behavior. The imputation model included important information including residential hospitalization at 12 months, baseline depression, adolescent gender, intervention condition, and the number of outpatient sessions received, in addition to the outcome variables at all four time-points.
After creating the imputed datasets, we estimated relationships for each of the 100 datasets, and then combined parameter estimates and standard errors into a single set of results using Rubin’s (1987) formula. One of the strengths of this approach is that there is variation between datasets, which allows for better estimates. This variation also results in cases falling into different categories across the different datasets, so the estimated numbers in each category were not necessarily integers. Some percentages do not sum to 100 due to rounding. We calculated effect sizes (OR) for recovered and improved vs. unchanged and deteriorated. We tested for differences by intervention condition, psychiatric severity group, and an intervention condition x psychiatric severity group interaction with ordinal regression pooled over the 100 datasets.
Borderline personality disorder behavior
For the full sample, intervention condition was not related to borderline personality disorder behavior, B = 2.86, SE = 6.98, p = .683, 95%CI [−10.98, 16.69]. We estimated that 62% of the adolescents in IDC and 76% in I-BAFT improved/recovered.
Subgroup Analysis
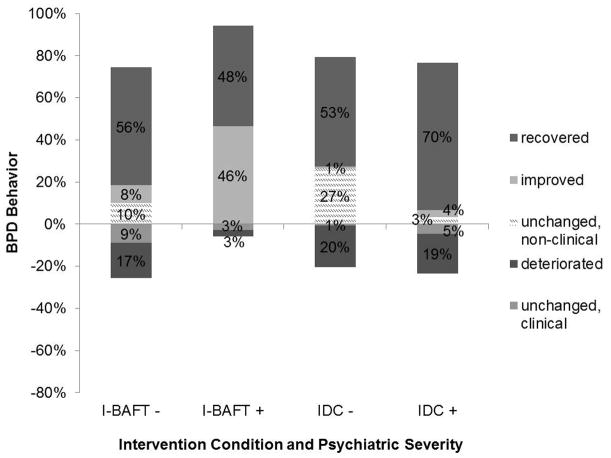
There was no difference between youth with co-morbid depression and those without borderline personality disorder behavior, B = −0.28, SE = 1.00, p = .796, 95%CI [−2.21, 1.70]. There was no intervention condition x depression interaction, B = −3.05, SE = 7.02, p = .665, 95%CI [−16.97, 16.97, 10.88]. Figure 3 shows change in borderline personality disorder behavior for each intervention condition divided by comorbid depression. In the non-depressed group, for I-BAFT (n = 13) we estimated 7.3 (56%) recovered, 1.1 (8%) improved, 1.3 (10%) unchanged, non-clinical, 1.2 (9%) unchanged, clinical, and 2.2 (17%) deteriorated; in IDC (n = 12) we estimated 6.3 (53%) recovered, 0.1 (1%) improved, 3.2 (27%) unchanged, non-clinical, 0.1 (1%) unchanged, clinical, and 2.4 (20%) deteriorated. Low-severity adolescents in I-BAFT had greater odds (OR = 1.58) of recovering/improving compared to IDC.
Figure 3.
Estimated proportions of cases with clinically significant change in borderline behavior. Recovered = clinically significant improvement in behavior from baseline to 12 months and, functioning in the “normal” range at 12 months. Improved = clinically significant improvement in behavior from baseline to 12 months and, but functioning in the “impaired” range at 12 months. Unchanged, non-clinical = no statistically reliable change in behavior from baseline and 12 months, and scores in non-clinical range at 12 months. Unchanged, clinical = no statistically reliable change in behavior from baseline and 12 months, and scores in clinical range at 12 months. Deterioration = clinically significant worsening in behavior from baseline to 12 months. I-BAFT − = adolescents without co-morbid depression in I-BAFT. I-BAFT + = adolescents with co-morbid depression in I-BAFT. IDC − = adolescents without co-morbid depression in IDC. IDC + = adolescents with co-morbid depression in IDC. (N=40)
In the depressed group, I-BAFT (n = 7) we estimated 3.4 (48%) recovered, 3.3 (46%) improved, none were unchanged, non-clinical, 0.2 (3%) unchanged, clinical, and 0.2 (3%) deteriorated; and in IDC (n = 8) we estimated 5.6 (70%) recovered, 0.3 (4%) improved, 0.3 (3%) were unchanged, non-clinical, 0.4 (5%) unchanged, clinical, and 1.5 (19%) deteriorated. High-severity adolescents in I-BAFT had greater odds (OR = 5.72) of recovering/improving compared to IDC.
Substance Use
For the full sample intervention condition was not related to substance use, B = −2.28, SE = 1.44, p = .115, 95%CI [−5.12, 0.56]. We estimated that 23% of the adolescents in IDC and 38% in I-BAFT improved/recovered.
Subgroup Analysis
There was a significant difference in substance use between youth with co-morbid depression and those without, B = −2.78, SE = 1.16, p = .018, 95%CI [−5.02, −0.02]. There was non-significant trend for an intervention condition x depression interaction, B = 2.96, SE = 1.69, p = .080, 95%CI [−0.36, 6.27]. Figure 4 shows change in substance for each intervention group divided by comorbidity. In the non-depressed group I-BAFT participants (n= 13) we estimated 1.3 (10%) recovered, 1.0 (8%) improved, 1.1 (8%) were unchanged, clean, 2.1 (16%) were unchanged, dirty, and 7.5 (58%) deteriorated; and in IDC (n= 12) we estimated 2.5 (21%) recovered, 0.1 (1%) improved, none were unchanged, clean, 5.2 (43%) were unchanged, dirty, and 3.2 (35%) deteriorated. Low-severity adolescents in I-BAFT had smaller odds (OR = 0.78) of recovering/improving compared to IDC.
Figure 4.

Estimated proportions of cases with clinically significant change in substance use. Recovered = reduced use from baseline to 12 months and abstinence at 12 months. Improved = reduced use from baseline to 12 months, but not abstinent at 12 months. Unchanged, clean = no use at either baseline and 12 months. Unchanged, dirty = same level of use at baseline and 12 months. Deterioration = increased use from baseline to 12 months. I-BAFT − = adolescents without co-morbid depression in I-BAFT. I-BAFT + = adolescents with co-morbid depression in I-BAFT. IDC− = adolescents without co-morbid depression in IDC. IDC + = adolescents with co-morbid depression in IDC. (N=40)
In the group with comorbid depression, in I-BAFT (n = 7) we estimated 4.2 (60%) recovered, 1.0 (14%) improved, none unchanged, clean, 1.4 (20%) unchanged, dirty, and 0.4 (6%) deteriorated; and in IDC (n = 8) we estimated 0.9 (11%) recovered, 0.7 (9%) improved, none unchanged, clean, 3.3(41%) unchanged, dirty, and 3.2 (40%) deteriorated. Adolescents with comorbid depression in I-BAFT had greater odds (OR = 11.38) of recovering/improving compared to IDC.
Unplanned Residential Services
The number of residential days was positively skewed with over dispersion, so a negative binomial regression analysis in Mplus was used. Residential days was not related to intervention condition, B = 0.25, SE = 0.34, p = .473, 95%CI [−0.42, 0.91].
Subgroup Analysis
Adolescents in the depressed group were hospitalized significantly more, B = 1.03, SE = 0.36, p = .004, 95%CI [0.34, 1.73], than those in the non-depressed group. Intervention condition interacted significantly with comorbid depression, B = −2.13, SE = 0.72, p = .003, 95%CI [−3.55, −0.71]. In the I-BAFT condition there was a small difference (Cohen’s d = .14) in residential days between non-depressed (M = 20.50, SD = 64.68) and depressed youth (M = 28.00, SD = 41.16). Conversely, in IDC there was a large difference (Cohen’s d = .75) in the residential days between the non-depressed (M = 3.54, SD = 10.21) and the depressed adolescents (M = 40.71, SD = 69.55). Figure 2 shows residential services (right side) for youth in each intervention condition, divided based on comorbid depression.
Discussion
This study was designed to shed light on a group of adolescents with severe psychiatric symptoms who often require intensive treatment including considerable residential treatment. This group of adolescents is often involved in the juvenile justice system and it is important to highlight their treatment needs and the complexity of that treatment. The results of this study add to a limited literature by reporting the results of a small randomized clinical trial of two manualized behavioral interventions for adolescents with borderline personality disorder and co-occurring substance use disorder. Although neither the I-BAFT nor the IDC interventions were specifically tailored for juvenile justice populations, both interventions sought to identify and modify triggers for substance abuse and for engagement in associated criminal behaviors. The severity of the symptoms and overlap of multiple problems is evident in the fact that almost two-thirds of adolescents were involved in the juvenile justice system, 28% had been hospitalized or in residential treatment in the year preceding the trial, and 65% had been arrested or detained in a police station in the year prior to baseline, all of which are relatively rare in adolescents in the general population. The sample size of this study is small, but consistent with the early stage research of new innovative treatments (Rounsaville, et al., 2001). This study relied on the analysis of feasibility and acceptability, as well as on the analysis of effect sizes and trends to detect promising treatment patterns worthy of further study.
The strong baseline relationship of co-occurring depression, substance use, and borderline personality disorder behavior is consistent with recent research with adolescents (e.g., Warden et al., 2012) showing a subgroup with high psychiatric severity that included internalizing problems. A difficult question to answer is whether depression preceded and contributed to the increased drug use and borderline personality disorder behavior, or whether either greater substance use or dysfunctional borderline personality disorder behaviors may have led to a greater risk for depression. Another possibility is that these three conditions result from a single underlying genetic predisposition. Our data did not permit us to investigate the causal links between symptoms, but it is an important question for future research. What we do know is that the distinction between those adolescents with depression and those without turned out to be a clinically meaningful distinction. Over the course of the trial, we saw an association between depression and more severe symptoms, differential impact on emergency residential treatment, and an interaction with the effects of the treatment conditions.
Feasibility and acceptability required looking at both within-intervention and outside-intervention indicators. Therapeutic alliance and overall dosage of therapy (i.e., the number of outpatient sessions that adolescents attended) suggested that there was a high level of feasibility and acceptability for both I-BAFT and IDC. Further, there were no differences in alliance from the adolescent’s perspective between an individually-oriented and a family oriented approach. However, this interpretation must be qualified by the fact that the participants required a substantial amount of unplanned residential treatment on average. That youth had outside hospitalizations was not a surprising finding given that more than a quarter of the sample had received residential services in the year prior to entering our outpatient study. The high volume of treatment received underlines the complex treatment needs of this population. Interestingly, there was a very clear pattern in which IDC youth with comorbid depression attended a lower number of planned outpatient sessions compared to the other 3 subgroups, and also attended higher number of treatment/follow-up residential days of treatment. The individually-oriented 12 step-based treatment condition may have been too focused on substance use to meet treatment needs in other areas, such as depression. I-BAFT’s use of DBT-derived skills training tools for managing depression focus on how substance use and depression could trigger each other, and focus on teaching parents how to better support their adolescents around issues of depression, may have contributed to all family members being highly involved in the outpatient treatment, particularly when depression was present.
Previous pilot work with a slightly less severe sample led us to expect some concurrent residential treatment. We incorporated treatment manual guidelines on establishing close collaboration between outpatient and residential/inpatient treatment teams. The substantial number of days of residential treatment documented in both intervention conditions in this study reinforced the importance of this collaboration even more clearly and suggested that this type of collaboration is particularly worthwhile for youth with comorbid depression. When symptom severity is high as in this sample, the actual treatment received will likely be a combination of outpatient and residential/inpatient treatment. I-BAFT included a plan for collaboration with hospital and residential agencies, but even more specificity and collaborative planning will be needed to maximize the benefit of treatment in future iterations. One must also wonder whether an IBAFT-based residential treatment would be efficacious, as long as it includes frequent trips home to solidify gains from family therapy.
The analysis of clinical change and clinical significance suggested that the only subgroup with substantial improvement on indicators of substance use were adolescents with comorbid depression (borderline personality disorder + substance use + depression) who received the I-BAFT intervention. This finding is consistent with findings reported by Henderson and colleagues (2010) who showed that family-based treatment was particularly effective with high severity cases. Unlike the IDC condition which focused almost exclusively on substance use triggers and abstinence strategies, I-BAFT was designed to address: 1) co-occurring psychiatric symptoms and emotion dysregulation that is prominent in borderline personality disorder and may be exacerbated by depression, and 2) family mechanisms that help the adolescents recover from substance use and depression disorders. A holistic family-based intervention may be particularly well-suited to intervening with youth who have complex, inter-related symptoms and to overcome the difficulty adolescents with depression have in reducing substance use during treatment.
Interestingly the I-BAFT condition was not particularly helpful with adolescents who did not have depression. In fact, these participants continued to deteriorate with respect to substance use. The IDC condition also did not lead to improved substance use in adolescents with depression, even though they received a substantial number of days of intensive residential (inpatient) treatment. Our clinical team experienced that when residential stays were not planned for and conceptualized with the parents as a natural extension/enhancement of the outpatient treatment, then each day in the residential/inpatient setting was interpreted as a failure of treatment, causing adolescents and parents alike to lose hope in treatment.
Unlike substance use, borderline personality disorder behaviors appeared to improve more evenly in the two conditions and for most adolescents regardless of the existence or absence of comorbid depression. This finding suggests that some of these behaviors may be more amenable to change in adolescents with substance abuse problems, than is the substance use. It is important to note that the substance use measures incorporated both self-reports of use and urine samples, but the measure of borderline personality disorder behavior was only self-reported. There is as yet no direct analog to laboratory toxicology for borderline personality disorder behavior, but future studies should include additional measures of these behavior. Results, though not conclusive, challenge any notion that borderline personality disorder improves as a consequence of substance use reduction, or that improvement in borderline behaviors inevitably lead to substance use reductions.
This study highlighted the complexity of conducting research on outpatient behavioral treatments with adolescents with severe co-occurring symptoms, but also showed benefits of rigorous research. It is important to document the crises and outside services received. Further, clinicians should expect the “true” treatment that adolescents with borderline personality disorder receive is likely a hybrid of outpatient and residential/inpatient treatment. Any outpatient treatment should have a well-designed strategy for working with residential service providers and parents in preparation for the adolescents return to the family. Just as family members of adolescents with borderline personality disorder may experience hopelessness, therapists may become discouraged by uneven progress and unexpected hospitalizations. Recommendations (Linehan, 1993) that a support mechanism be in place for therapists working with individuals with borderline personality disorder was reinforced by our experience.
Our most recent work on the development and testing of an adaptive methodology/strategy that can be used to systematically tailor our work with adolescents and families to their unique clinical and cultural profiles (Santisteban, Mena, & Abalo, 2013) may be a key component of future work with adolescents with borderline personality disorder and substance abuse. The adaptive strategy can be integrated into I-BAFT so that it can better address the unique circumstances (e.g., criminal activities and symptom severity that requires hospitalization/residential services) with which some but not all adolescents enter treatment. The selection of psycho-educational modules that may be best suited for subsets of the sample, may help I-BAFT to address each adolescent’s/family’s unique needs in a more focused manner and enhances its overall efficacy.
This study had several limitations. The small sample limited statistical power and the types of analyses that could be used. For example, there were differences in the dosage of residential treatment received by the youth in the study, however in the analyses we were not able to control for this due to the small sample size. The process of data collection was difficult due to the high level of substance use and psychiatric symptoms, which resulted in multiple hospital and residential treatment placements – some during the treatment period and immediately preceding the final assessment point. The analysis of clinical and clinically significant change used multiple imputation to deal with the resulting missing data. This strategy provided the best possible estimates, but ideal data sets would have no missing data. We considered assessments at the residential sites, but family functioning and substance use data collected in a restricted environment over a long period of time would have not be comparable to data collected outside of a restricted environment.
Acknowledgments
Work funded primarily by the National Institute on Drug Abuse Grant #s R01 DA019057to Daniel Santisteban (PI). This work was also supported in part by National Institute on Drug Abuse Grant #RO1 DA027920 to Daniel Santisteban (PI). The authors would like to thank Dr. Marsha Linehan for her generosity in giving of her time and expertise to our clinical researchers who were new to this area of work.
Contributor Information
Daniel A. Santisteban, Email: dsantist@miami.edu.
Maite P. Mena, Email: mmena@miami.edu.
Joan Muir, Email: jmuir@med.miami.edu.
Brian E. McCabe, Email: bmccabe@miami.edu.
Clara Abalo, Email: c.abalo@miami.edu.
Amanda M. Cummings, Email: amandacummings@gmail.com.
References
- Bernstein DP. Adolescent personality disorders: Just a passing phase? The Journal of the California Alliance for the Mentally Ill. 1997;8:56–57. [Google Scholar]
- Brook JS, Brook DW, de la Rosa M, Duque LF, Rodriguez E, Montoya ID, Whiteman M. Pathways to marijuana use among adolescents: Cultural/ecological, family, peer, and personality influences. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37(7):759–766. [PubMed] [Google Scholar]
- Chanen AM, Jackson HJ, McCutcheon LK, Jovev M, Dudgeon P, Yuen H, … McGorry PD. Early intervention for adolescents with borderline personality disorder using cognitive analytic therapy: Randomized controlled trial. British Journal of Psychiatry. 2008;193(6):477–484. doi: 10.1192/bjp.bp.107.048934. [DOI] [PubMed] [Google Scholar]
- Cocozza J, Veysey BM, Chapin DA, Dembo R, Walters W, Farina S. Diversion from the juvenile justice system: The Miami-Dade juvenile assessment center post-arrest diversion program. Substance Use & Misuse. 2005;40:935–951. doi: 10.1081/JA-200058853. [DOI] [PubMed] [Google Scholar]
- Cornelius JR, Bukstein OG, Salloum IM, Kelly TM, Wood DS, Clark DB. Fluoxetine in depressed AUD adolescents: A 1-year follow-up evaluation. Journal of Child and Adolescent Psychopharmacology. 2004;14:33–38. doi: 10.1089/104454604773840463. [DOI] [PubMed] [Google Scholar]
- Enders CK. Applied Missing Data Analysis. New York: Guilford Press; 2010. [Google Scholar]
- Farrand P, Booth N, Gilbert T, Lankshear G. Engagement and early termination of contact with a community-based early intervention service for personality disorder in young adults. Early Intervention in Psychiatry. 2009;3:204–212. doi: 10.1111/j.1751-7893.2009.00134.x. [DOI] [PubMed] [Google Scholar]
- Graham JW. Missing data analysis: making it work in the real world. Annual Review of Psychology. 2009;60:549–576. doi: 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- Graham JW, Schafer JL. On the performance of multiple imputation for multivariate data with small sample size. In: Hoyle R, editor. Statistical strategies for small sample research. Thousand Oaks, CA: Sage; 1999. pp. 1–29. [Google Scholar]
- Halliday-Boykins CA, Schaeffer CM, Henggeler SW, Chapman JE, Cunningham PB, Randall J, Shapiro SB. Predicting non-response to juvenile drug court interventions. Journal of Substance Abuse Treatment. 2010;39(4):318–328. doi: 10.1016/j.jsat.2010.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin D, Nunes E, Meydan J. Comorbidity of alcohol, drug and psychiatric disorders: Epidemiology. In: Kranzler HR, Tinsley JA, editors. Dual diagnosis and psychiatric treatment: Substance abuse and comorbid disorders. Vol. 1. New York: Marcle Dekker, Inc; 2004. pp. 1–34. [Google Scholar]
- Henderson CE, Dakof GA, Greenbaum PE, Liddle HA. Effectiveness of multidimensional family therapy with higher severity substance-abusing adolescents: Report from two randomized controlled trials. Journal of Consulting and Clinical Psychology. 2010 Dec;78(6):885–897. doi: 10.1037/a0020620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henggeler SW, Sheidow AJ. Empirically supported family-based treatments for conduct disorder and delinquency in adolescents. Journal of Marital and Family Therapy. 2012;38(1):30–58. doi: 10.1111/j.1752-0606.2011.00244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horvath AO, Greenberg LS. The development and validation of the working alliance inventory. Journal of Counseling Psychology. 1989;36:223–23. [Google Scholar]
- Jacobson A, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting & Clinical Psychology. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Kolb JE, Gunderson JG. Diagnosing borderline patients with a semi-structured interview. Archives of General Psychiatry. 1980;37(1):37–41. doi: 10.1001/archpsyc.1980.01780140039004. [DOI] [PubMed] [Google Scholar]
- Linehan M. Cognitive behavioral treatment of borderline personality disorder. New York: Guilford Press; 1993. [Google Scholar]
- Lucas CP, Zhang H, Fisher PW, Shaffer D, Regier DA, Narrow WE, … Friman P. The DISC predictive scales (DPS): Efficiently screening for diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40(4):443–449. doi: 10.1097/00004583-200104000-00013. [DOI] [PubMed] [Google Scholar]
- Maquire ER. Police organizational structure and child sexual abuse case attrition. Policing: An International Journal of Police Strategies & Management. 2009;32:157–179. [Google Scholar]
- Mercer DE, Woody GE. Individual Drug Counseling, “a manual”. Rockville, MD: National Institute on Drug Abuse; 1999. NIH Publication Number 99–4380. [Google Scholar]
- Miller AL, Rathus JH, DuBose AP, Dexter-Mazza ET, Goldklang AR. Dialectical behavior therapy for Adolescents. In: Dimeff LA, Koerner K, editors. Dialectical behavior therapy in clinical practice: Applications across disorders and settings. New York, NY: Guilford Press; 2007. [Google Scholar]
- Millon T. MACI Manual, Millon Adolescent Clinical Inventory. Minneapolis, MN: National Computer Systems, Inc; 1993. [Google Scholar]
- Minuchin S, Fishman CH. Family Therapy Techniques. Cambridge, MA: Harvard University Press; 1981. [Google Scholar]
- Newton-Howes G, Tyrer P, Johnson T. Personality disorder and the outcome of depression: Meta-analysis of published studies. The British Journal of Psychiatry. 2006;188:13–20. doi: 10.1192/bjp.188.1.13. [DOI] [PubMed] [Google Scholar]
- Rathus JH, Miller AL. Dialectical behavior therapy adapted for suicidal adolescents. Suicide and Life-Threatening Behavior. 2002;32(2):146–157. doi: 10.1521/suli.32.2.146.24399. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, Carroll KM, Onken LS. A stage model of behavioral therapies research: Getting started and moving on from Stage I. Clinical Psychology: Science & Practice. 2001;8(2):133–142. [Google Scholar]
- Rowe CL, Liddle HA, Greenbaum PE, Henderson CE. Impact of psychiatric comorbidity on treatment of adolescent drug abusers. Journal of Substance Abuse Treatment. 2004;26:129–140. doi: 10.1016/S0740-5472(03)00166-1. [DOI] [PubMed] [Google Scholar]
- Rubin DB. Multiple imputation for nonresponse in surveys. New York: Wiley; 1987. [Google Scholar]
- Santisteban DA, Coatsworth D, Perez-Vidal A, Kurtines WM, Schwartz SJ, LaPerriere A, Szapocznik J. The efficacy of brief strategic/structural family therapy in modifying behavior problems and an exploration of the mediating role that family functioning plays in behavior change. Journal of Family Psychology. 2003;17(1):121–133. doi: 10.1037/0893-3200.17.1.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santisteban DA, Mena MP, Abalo C. Bridging Diversity and Family Systems: Culturally Informed and Flexible Family-Based Treatment for Hisapnic Adolescents. Couple and Family Psychology. 2013;2(4):246–263. doi: 10.1037/cfp0000013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santisteban DA, Muir JA, Mena MP, Mitrani VB. Integrative Borderline Adolescent Family Therapy: Meeting the Challenges of Treating Borderline Adolescents. Psychotherapy: Theory/Research/Practice/Training. 2003;40(4):251–264. doi: 10.1037/0033-3204.40.4.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer JL. Analysis of Incomplete Multivariate Data. London: Chapman & Hall; 1997. [Google Scholar]
- Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychological Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Schuppert HM, Giesen-Bloo J, van Gemert TG, Wiersema HM, Minderaa RB, Emmelkamp PMG, Nauta MH. Effectiveness of an emotion regulation group training for adolescents- A randomized controlled pilot study. Clinical Psychology and Psychotherapy. 2009;16:467–478. doi: 10.1002/cpp.637. [DOI] [PubMed] [Google Scholar]
- Schwarz G. Estimating the dimension of a model. Annals of Statistics. 1978;6:461–464. [Google Scholar]
- Sobell LC, Agrawal S, Sobell M, Leo G, Young L, Cunningham JA, Simco ER. Comparison of a Quick Drinking Screen with the Timeline Follow back for Individuals with Alcohol Problems. Journal of Studies on Alcohol. 2003;64(6):858–861. doi: 10.15288/jsa.2003.64.858. [DOI] [PubMed] [Google Scholar]
- Subramaniam GA, Warden D, Minhajuddin A, Fishman MJ, Stitzer ML, Adinoff B, … Woody GE. Predictors of abstinence: national institute of drug abuse multisite buprenorphine/naloxone treatment trial in opiod-dependent youth. Journal of the Academy of Child and Adolescent Psychiatry. 2011;50:1120–1128. doi: 10.1016/j.jaac.2011.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warden D, Riggs PD, Min SJ, Mikulich-Gilbertson SK, Tamm L, Trello-Rishel K, Winhusen T. Major depression and treatment response in adolescents with ADHD and substance use disorder. Drug and Alcohol Dependence. 2012 Jan 1;120(1–3):214–219. doi: 10.1016/j.drugalcdep.2011.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winograd G, Cohen P, Chen H. Adolescent borderline symptoms in the community: Prognosis for functioning over 20 years. Journal of Child Psychology and Psychiatry. 2008;49(9):933–941. doi: 10.1111/j.1469-7610.2008.01930.x. [DOI] [PubMed] [Google Scholar]
- Wimberly SR, Carver CS, Laurenceau JP, Harris SD, Antoni MH. Perceived partner reactions to diagnosis and treatment of breast cancer: impact on psychosocial and psychosexual adjustment. Journal of Consulting and Clinical Psychology. 2005;73:300–311. doi: 10.1037/0022-006X.73.2.300. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Gunderson JG, Frankenburg FR, Chauncey DL. The revised Diagnostic Interview for Borderlines: Discriminating BPD from other Axis II disorders. Journal Of Personality Disorders. 1989;3(1):10–18. doi: 10.1521/pedi.1989.3.1.10. [DOI] [Google Scholar]