Abstract
The exclusive autograft choice for medial collateral ligament (MCL) reconstruction that has been described until today is the semitendinosus tendon. However, this has some potential disadvantages in a knee with combined MCL–anterior cruciate ligament (ACL) injury, including weakening of the hamstring's anterior restraining action in an already ACL-injured knee and nonanatomic distal MCL graft insertion when leaving the semitendinosus insertion intact at the pes anserinus during reconstruction. Moreover, because some surgeons prefer to use the hamstring for autologous ACL reconstruction, the contralateral uninjured knee hamstring needs to be harvested as a graft source for the MCL reconstruction if autografts and not allografts are the surgeons' preference. We describe a technique for performing combined reconstruction of the MCL and ACL using ipsilateral quadriceps tendon–bone and bone–patellar tendon–bone autografts. This technique of MCL reconstruction spares the hamstring tendons and benefits from the advantage provided by bone-to-bone healing on the femur with distal and proximal MCL tibial fixation that closely reproduces the native MCL tibia insertion.
Combined medial collateral ligament (MCL) and anterior cruciate ligament (ACL) instability that requires reconstruction of both ligaments is uncommon. This is because most MCL lesions tend to heal satisfactorily without surgery within 8 to 12 weeks after the injury with coronal-plane protective bracing.1 However, in rare cases, symptomatic medial and anterior instabilities coexist in the chronic setting, which may then require combined reconstruction of both ligaments. Multiple surgical techniques to reconstruct the MCL in combined ligament injuries have been described using allografts.2, 3, 4 When autograft was used for MCL reconstruction, the semitendinosus was the exclusive autologous graft choice described.5, 6, 7 The disadvantages of using allografts for reconstructing the knee ligaments relate to financial costs,8 concerns regarding tissue quality with slower biological incorporation,9 disease transmission,10 and some evidence of higher failure rates and inferior functional outcomes in young active adults, at least for the ACL.11 The potential disadvantages of using autologous hamstring for reconstructing the MCL in the ACL-deficient knee include weakening of the hamstring's anterior restraining action.12 Moreover, nonanatomic (i.e., too anterior) distal MCL graft insertion when leaving the semitendinosus insertion intact at the pes anserinus during reconstruction may lead to inadequate posteromedial restraint and therefore the need to reconstruct an additional posteromedial graft limb to overcome the “too anterior” distal MCL graft attachment at the pes anserinus.6, 7 We describe a technique for performing combined reconstruction of the MCL and ACL using ipsilateral quadriceps tendon–bone and bone–patellar tendon–bone (BPTB) autografts. It yields excellent biological incorporation of autografts, spares the hamstring in the MCL-ACL–deficient knee, and closely reproduces the anatomic insertions of the MCL graft on the femur and tibia.
Surgical Technique
In the operating room and before the surgical procedure begins, the following steps are performed (Video 1):
-
1.
The patient is placed in the supine position. A tourniquet cuff (Zimmer, Dover, OH) is placed around the proximal thigh but not inflated yet. A lateral thigh post (Maquet, Rastatt, Germany) and a 3-L arthroscopic irrigation bag are strapped distally onto the operating table and used as a foot bolster, positioning and supporting the knee at 90° of flexion, as well as mobilizing it freely from flexion toward extension during the operation as needed.
-
2.
The knee is examined with the patient under anesthesia with emphasis on range of motion and ligament laxity, including the ACL, posterior cruciate ligament, MCL, fibular collateral ligament, and corners. In this case, positive findings of the left knee included grade 2+ Lachman, grade 2+ pivot shift, grade 2+ MCL laxity in the extended knee, and grade 3+ MCL laxity in 20° of flexion.
The surgical steps for combined MCL-ACL reconstruction are then performed as follows:
-
1.
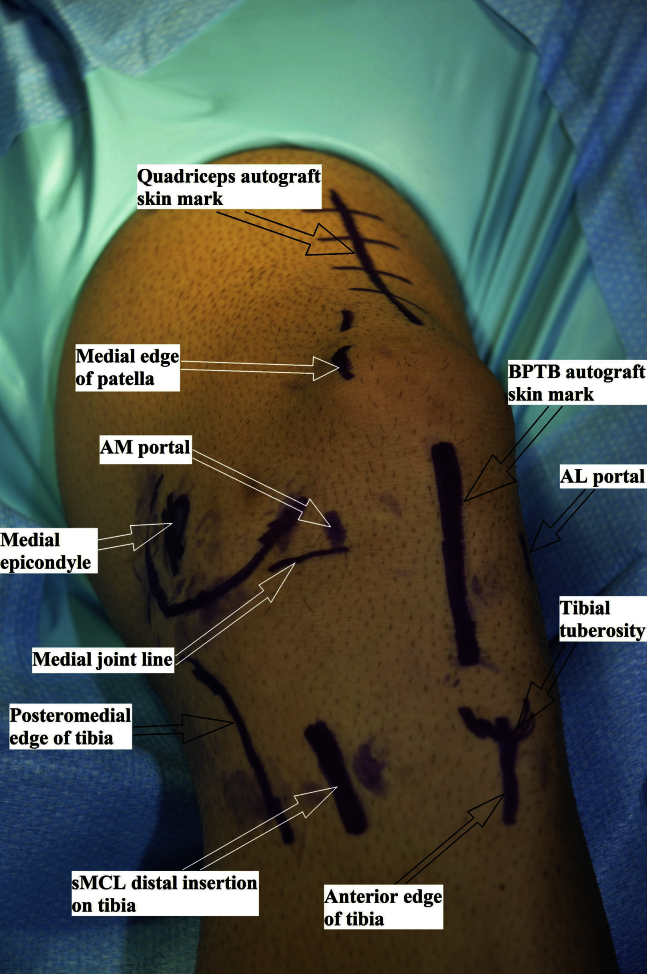
All relevant skin markings are drawn, including the proximal posteromedial tibial ridge, medial femoral epicondyle, approximate distal tibial insertion of the superficial MCL 6 cm distal to the joint line, tibial tuberosity, quadriceps and patellar tendons, medial joint line, and locations for anterolateral and anteromedial arthroscopic portals (Fig 1).
-
2.
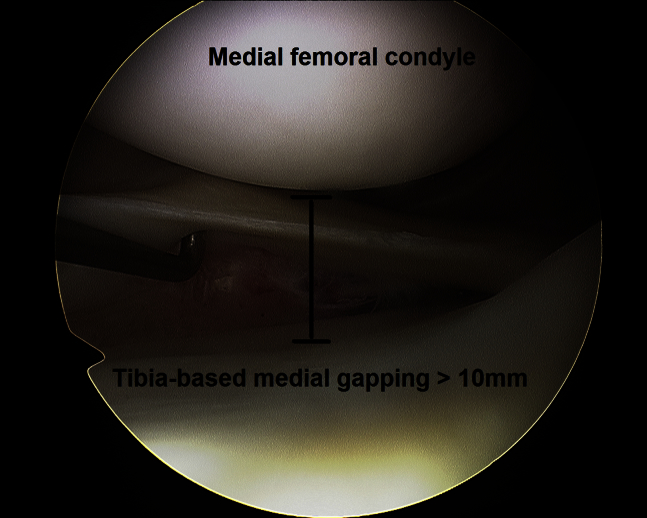
Systematic arthroscopic evaluation of all knee compartments is performed with a 30° arthroscope (Olympus, Center Valley, PA) using standard anterolateral and anteromedial portals. Any unstable chondral lesion or meniscus tear is debrided or repaired as needed. In this case, a lateral meniscus posterior horn flap tear was resected using a medium–bite width meniscal punch (Arthrex, Naples, FL). Grade I to II lateral-compartment impaction and fissuring chondral lesions were left alone. In this case, ACL probing confirmed a high-grade intrasubstance tear resulting in a loose ligament. Medial- and lateral-compartment tibiofemoral gapping is then evaluated. In the case presented in Video 1, medial-compartment gapping at 20° of flexion under a valgus load showed over 1 cm of tibia-based gapping, supportive of grade 3+ MCL insufficiency (Fig 2). Lateral-compartment gapping under varus stress at a figure-of-4 position was normal.
-
3.
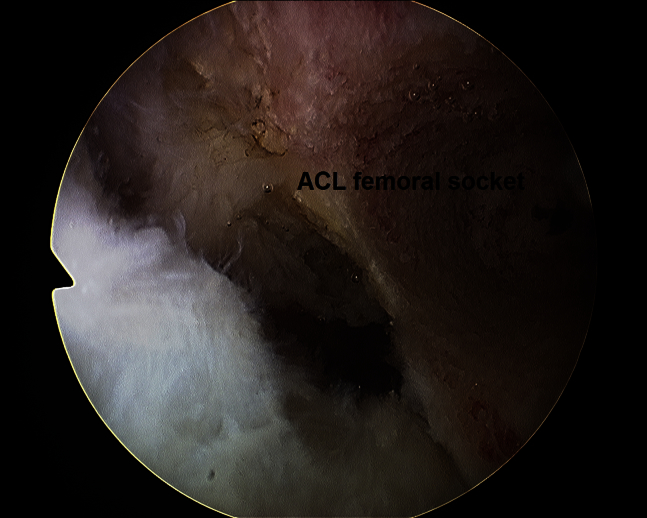
After torn ACL tissue is debrided using a 5.0-mm full-radius resector shaver (Stryker, San Jose, CA), with the knee at 110° of flexion, a 7-mm over-the-top femoral offset guide (Arthrex) is inserted through the anteromedial portal, and a 2.4-mm guidewire (Arthrex) through this offset guide is centered at the femoral ACL footprint. By use of a 10-mm-diameter low-profile reamer (Arthrex), a 10-mm-diameter × 20-mm-long femoral socket for the BPTB graft is then reamed over the guidewire (Fig 3).
-
4.
The thigh tourniquet cuff is now inflated to a pressure of 250 mm Hg, and graft harvest begins.
-
5.
The central third of the patellar tendon is incised with a 10-mm-wide double cutter (Arthrex). The tibial tuberosity bone plug is harvested using a Micro 100 sagittal saw (Hall, Charlottesville, VA) and measures 10 mm wide × 20 mm long.
-
6.
At this point, it is essential to measure and precisely mark a 10-mm-wide × 15-mm-long distal patellar bone plug (Fig 4). This length of 15 mm will allow a 10-mm bone bridge to be eventually maintained at the center of the patella between the proximal and distal patellar bone plugs.
-
7.
The quadriceps tendon–bone graft is then harvested. After skin and subcutaneous layers are incised longitudinally from the proximal patellar pole and extending proximally, the quadriceps tendon is identified. The width of the graft is 10 mm, and the length of the tendinous part of the graft should be at least 10 cm to later allow sufficient graft length from the proximal femoral MCL insertion to the distal tibial MCL insertion (Fig 5). During this step, the superficial rectus femoris layer is separated from the deeper vastus intermedius layer proximally, thus eventually creating a partial-thickness quadriceps tendon graft.
-
8.
At the proximal patella, a 15-mm-long × 10-mm-wide bone plug is needed, with the surgeon ensuring that an intact patellar bone bridge measuring at least 10 mm remains between the proximal and distal patellar bone plugs (Fig 6). The quadriceps harvest site is irrigated, and the soft-tissue layers are closed.
-
9.
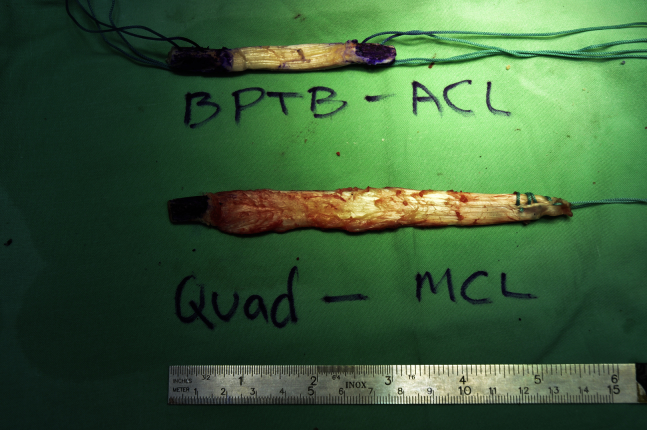
On a side table, the partial-thickness quadriceps tendon graft is whipstitched at the tip with No. 5 Ethibond suture (Ethicon, Somerville, NJ). The bone plug is gently tapered with a rongeur (Aesculap, Center Valley, PA) to a diameter of 9 mm and length of 15 mm. The BPTB ACL graft is prepared as well, with gentle tapering of both patellar plugs with the rongeur to fit a diameter of 10 mm. Two No. 5 Ethibond sutures are passed through two 1.5-mm drill holes made in each of the 2 patellar tendon bone plugs (Fig 7).
-
10.
At this point, the 30° arthroscope is reinserted into the knee through the anterolateral portal and a tibial tunnel of 10 mm in diameter is reamed over a 2.4-mm guidewire (Arthrex) centered at the tibial ACL footprint (Fig 8).
-
11.
The BPTB ACL graft is passed into the knee through the tibial tunnel (Fig 9) and fixed in the femoral socket with a 7-mm × 20-mm titanium interference screw (Arthrex) (Fig 10).
-
12.
The operation now continues on the extra-articular side.
-
13.
A 3-cm longitudinal incision is made over the medial epicondyle, and a 2.4-mm guidewire (Arthrex) is inserted 3 to 5 mm proximal and posterior to the tip of the medial epicondyle and horizontally relative to the joint line. The location of the guidewire is confirmed with fluoroscopy (Fig 11).
-
14.
A socket of 9 mm in diameter and 18 mm in depth is reamed over the guidewire, and remnants of soft tissue at the edges of the socket are debrided to ensure better visualization of the bony margins of this socket.
-
15.
The bone plug of the quadriceps tendon–bone graft is docked in the femoral socket and fixed with a 7-mm × 20-mm titanium interference screw (Arthrex) (Fig 12).
-
16.
A 3- to 5-cm longitudinal incision is made 6 cm distal to the joint line and posterior to the pes anserinus at the approximated anatomic distal tibial superficial MCL insertion (Fig 13).
-
17.
The superficial fascial layer (i.e., layer 1) is incised, and a soft-tissue tunnel is created bluntly with Metzenbaum scissors (Aesculap) for future MCL graft passage, which is overlying the native superficial MCL layer from the distal MCL insertion point to the femoral MCL fixation point.
-
18.
A nitinol guidewire (Arthrex) is inserted temporarily into the femoral MCL fixation screw, and a suture loop is passed around the wire and brought under the skin to the approximated distal MCL insertion point. The knee is cycled while the suture loop is held tight against the approximated distal MCL tibial insertion until the isometric point is identified on the tibia. This point is marked with a Bovie device on the tibia for future distal graft fixation.
-
19.
A 21-gauge needle (Henke-Sass Wolf, Tuttlingen, Germany) is used to identify the area 5 to 10 mm distal to the medial joint line. After its location is confirmed with fluoroscopy as reproducing the proximal tibial soft-tissue MCL insertion area (Fig 14), a 2- to 3-cm longitudinal skin incision is made in this area. Layer 1 is incised, and care is taken to avoid injury to any saphenous nerve branches, if present.
-
20.
The quadriceps tendon graft is now passed under layer 1 from proximal to distal (Fig 15).
-
21.
The knee is cycled, and the ACL BPTB graft is fixed in the tibial tunnel with a 9-mm × 20-mm titanium interference screw (Arthrex) when the knee is in extension.
-
22.
A 2-cm longitudinal slit is made in the quadriceps tendon graft over the area previously marked with a Bovie device for distal tibial insertion of the MCL graft. Soft tissue is gently debrided with a rongeur at the planned insertion site on the tibia to promote graft-bone healing.
-
23.
The knee is cycled, tension is applied to the quadriceps tendon graft, and the graft is fixed at the distal insertion point (previously marked with a Bovie device) with a 4.5-mm titanium screw (Arthrex) and 18-mm titanium spiked washer (Arthrex) while the knee is at 20° of flexion and under slight varus stress (Fig 16).
-
24.
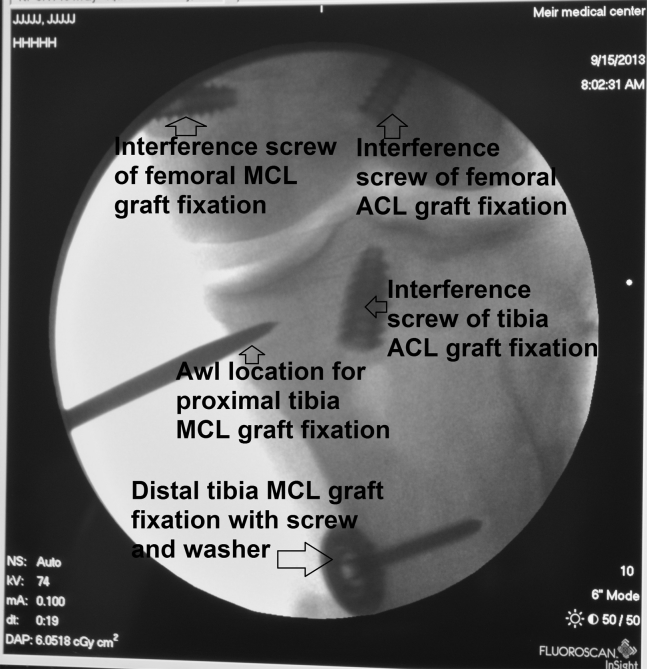
A 5.5-mm double-loaded Bio-Corkscrew FT anchor is finally added for reproducing proximal tibial soft-tissue MCL graft fixation (Fig 17). The anchor is placed just at the posterior edge of the quadriceps graft, 5 to 10 mm distal to the joint line, and the location is confirmed with fluoroscopy (Fig 18).
-
25.
The distal quadriceps MCL graft remnant is resected, and the soft-tissue layers are closed.
Fig 1.
All relevant skin markings are drawn on a left knee, including the proximal posteromedial tibial ridge, medial femoral epicondyle, approximate distal tibial insertion of the superficial medial collateral ligament (sMCL) 6 cm distal to the joint line, tibial tuberosity, quadriceps and patellar tendons, medial joint line, and locations for anterolateral (AL) and anteromedial (AM) arthroscopic portals. (BPTB, bone–patellar tendon–bone.)
Fig 2.
A left knee viewed using a 30° arthroscope through the anterolateral portal. The knee is held at 20° of flexion and under a valgus load. Medial-compartment tibia-based gapping of over 1 cm is supportive of grade 3+ medial collateral ligament insufficiency.
Fig 3.
A left knee viewed using a 30° arthroscope through the anterolateral portal. A 10-mm-diameter × 20-mm-long femoral socket was prepared at the center of the femoral anterior cruciate ligament (ACL) footprint for a bone–patellar tendon–bone graft.
Fig 4.
A 15-mm-long distal patellar bone plug is planned and precisely measured before patellar bone plug harvest as part of the anterior cruciate ligament bone–patellar tendon–bone graft preparation, as shown in a left knee.
Fig 5.
As shown in a left knee, during quadriceps tendon graft harvest, the superficial rectus femoris layer is separated from the deeper vastus intermedius layer proximally, thus eventually creating a partial-thickness quadriceps tendon graft. The width of the graft is 10 mm, and the length of the tendinous part of the graft should be at least 10 cm to later allow sufficient graft length from the proximal femoral medial collateral ligament insertion to the distal tibial medial collateral ligament insertion.
Fig 6.
As shown in a left knee, to complete partial-thickness quadriceps tendon–bone graft harvest, at the proximal patella, a 15-mm-long × 10-mm-wide bone plug is precisely measured and harvested. A 10-mm intact patellar bone bridge should remain between the proximal and distal patellar bone plugs.
Fig 7.
On a side table, the partial-thickness quadriceps (Quad) tendon graft is whipstitched at the tip with No. 5 Ethibond suture. The bone plug is gently tapered with a rongeur to a diameter of 9 mm and length of 15 mm. The bone–patellar tendon–bone (BPTB) anterior cruciate ligament (ACL) graft is prepared as well, with gentle tapering of both patellar plugs with a rongeur to fit a diameter of 10 mm. Two No. 5 Ethibond sutures are passed through two 1.5-mm drill holes made in each of the 2 patellar tendon bone plugs. (MCL, medial collateral ligament.)
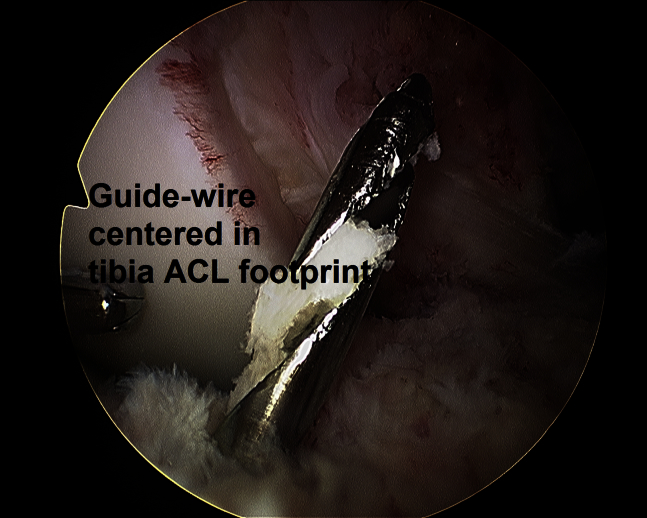
Fig 8.
A left knee viewed using a 30° arthroscope through the anterolateral portal. A 2.4-mm guidewire is centered at the tibial anterior cruciate ligament (ACL) footprint, over which a tibial tunnel of 10 mm in diameter is reamed next.
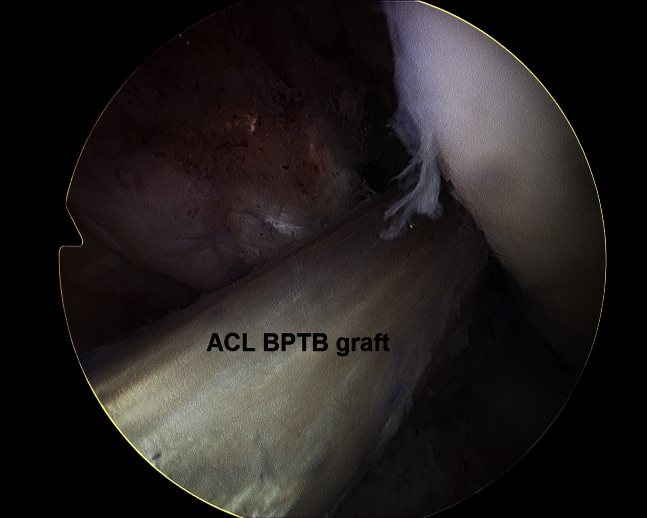
Fig 9.
A left knee viewed using a 30° arthroscope through the anterolateral portal. The bone–patellar tendon–bone (BPTB) anterior cruciate ligament (ACL) graft is passed into the knee through the tibial tunnel and located in the desired position.
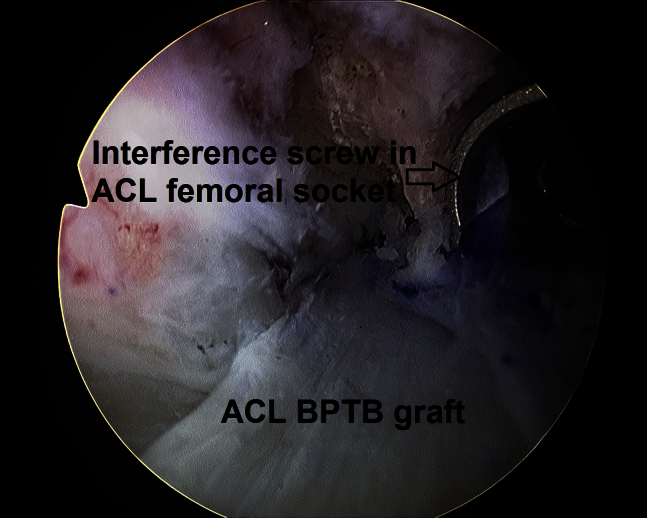
Fig 10.
A left knee viewed using a 30° arthroscope through the anteromedial portal showing the femoral socket with 7-mm × 20-mm titanium interference screw fixation of the anterior cruciate ligament (ACL) bone–patellar tendon–bone (BPTB) graft.
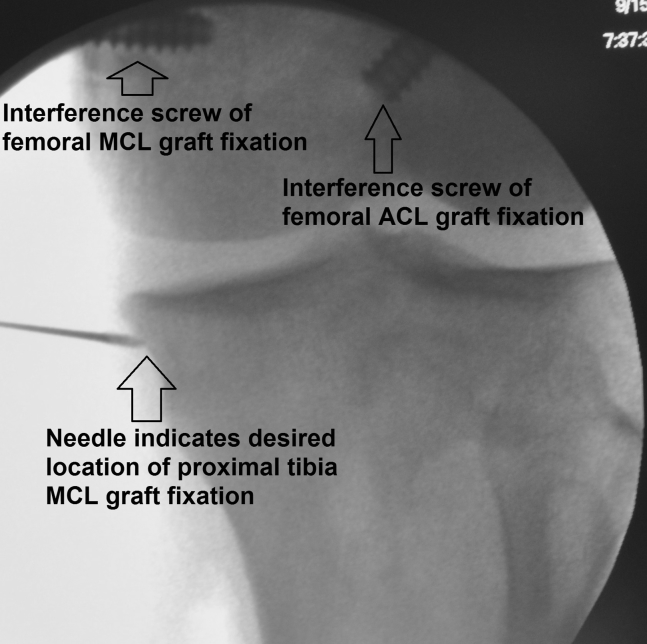
Fig 11.
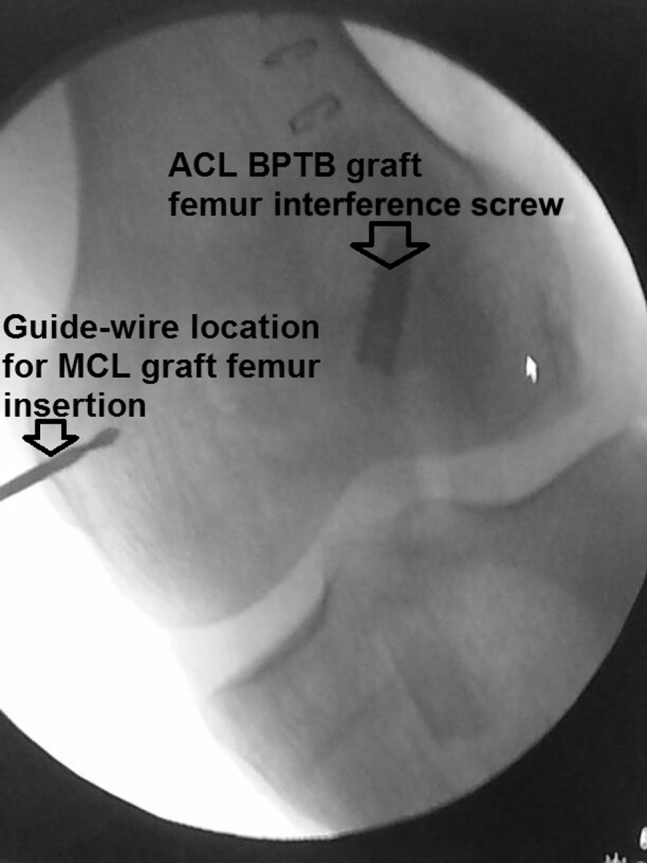
Fluoroscopy confirms the desired location of a 2.4-mm guidewire for future femoral medial collateral ligament (MCL) graft insertion just proximal to the tip of the medial epicondyle and horizontally relative to the joint line, as shown in a left knee. (ACL, anterior cruciate ligament; BPTB, bone–patellar tendon–bone.)
Fig 12.
As shown in a left knee viewed from the medial side, the bone plug of the quadriceps tendon–bone graft is docked in the femoral socket and fixed with a 7-mm × 20-mm titanium interference screw. (MCL, medial collateral ligament.)
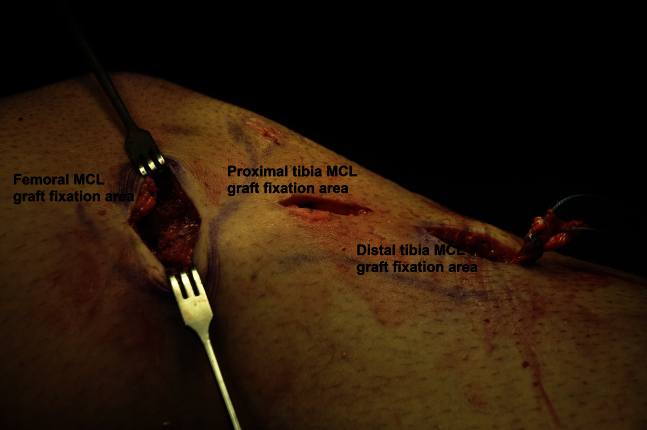
Fig 13.
As shown in a left knee viewed from the medial side, a 3- to 5-cm longitudinal incision is made 6 cm distal to the joint line and posterior to the pes anserinus at the approximated anatomic distal tibial superficial medial collateral ligament (MCL) insertion.
Fig 14.
Fluoroscopy in a left knee confirms the location of a 21-gauge needle, which is used to identify the area 5 to 10 mm distal to the medial joint line for later reproducing the proximal tibial soft-tissue medial collateral ligament (MCL) insertion area. A 2- to 3-cm longitudinal skin incision is then made in this area, and layer 1 is incised, with care taken to avoid any saphenous nerve branches, if present. (ACL, anterior cruciate ligament.)
Fig 15.
As shown in a left knee viewed from the medial side, the quadriceps tendon graft was passed under layer 1 from the femoral medial collateral ligament (MCL) graft insertion to the distal MCL graft insertion area.
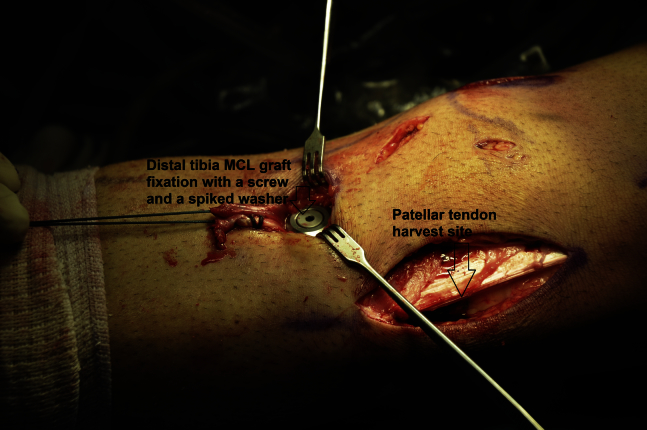
Fig 16.
As shown in a left knee viewed from the anteromedial side, a 4.5-mm titanium screw and 18-mm titanium spiked washer are used to fix the quadriceps tendon medial collateral ligament (MCL) graft at the distal tibial MCL insertion point while the knee is held at 20° of flexion and under slight varus stress.
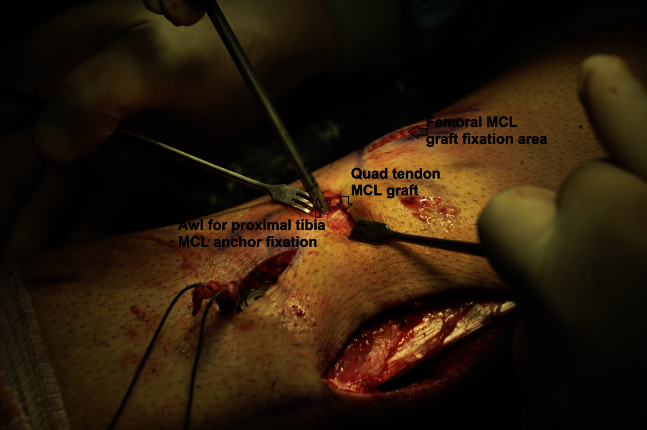
Fig 17.
As shown in a left knee viewed from the anteromedial side, an awl from a 5.5-mm double-loaded Bio-Corkscrew FT anchor is added at the posterior edge of the quadriceps (Quad) tendon for reproducing proximal tibial soft-tissue medial collateral ligament (MCL) graft fixation.
Fig 18.
As shown in a left knee, fluoroscopy confirms the awl location 5 to 10 mm distal to the joint line. (ACL, anterior cruciate ligament; MCL, medial collateral ligament.)
Postoperative Management
The postoperative protocol includes wearing a T-Scope knee brace (Breg, Carlsbad, CA) with range of motion from 0° to 30° during the first 2 weeks, 0° to 60° during the third and fourth weeks, and 0° to 90° during the fifth and sixth weeks. Thereafter, unrestricted range of motion is encouraged. Weight bearing is avoided for 6 weeks. Use of the knee brace is recommended for 12 weeks during walking to ensure MCL graft protection during soft tissue–to–bone incorporation at the tibial MCL graft insertion. Crutches are used until the gait pattern is normalized. Closed kinetic chain exercises are encouraged during rehabilitation with open chain exercises avoided throughout the first 3 months after the operation to decrease potential anterior translation shearing forces.
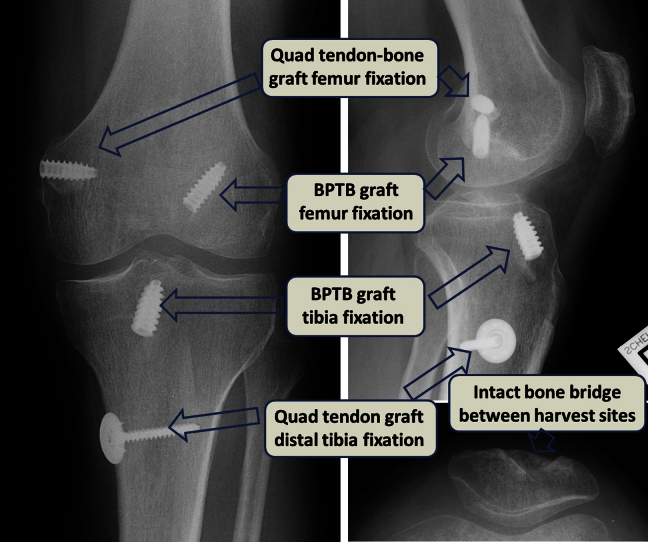
At the first postoperative visit, 1 to 2 weeks after the operation, anteroposterior, lateral, and patellar sky-view images are obtained (Fig 19). This is aimed particularly to confirm proper hardware locations, intact bone plugs, and an intact patella (except for the expected harvest-site bone defect). Table 1 summarizes tips and pearls for performing the described operation.
Fig 19.
Anteroposterior (left image), lateral (upper right image), and sky-view (lower right image) radiographs of left knee after combined reconstruction of medial collateral ligament and anterior cruciate ligament using ipsilateral quadriceps (Quad) tendon–bone and bone–patellar tendon–bone (BPTB) autografts.
Table 1.
Tips and Pitfalls During Combined Reconstruction of MCL and ACL Using Ipsilateral Quadriceps Tendon–Bone and BPTB Autografts
| Tips |
| A C-arm fluoroscopy machine is placed in the operating room. |
| A lateral post is preferred over a fixed thigh holder because mobilization of the knee from flexion to extension is needed during the operation. |
| A thigh tourniquet cuff is placed but not inflated until graft harvesting to save tourniquet time. The cuff is placed as proximally as possible to allow sterile dressing proximal to the quadriceps tendon harvest cut. |
| All skin markings are drawn before the operation is started, including estimated anatomic MCL insertions. |
| Medial gapping is measured during the initial arthroscopic assessment with the knee at 20° of flexion and under mild valgus stress. This is performed with the tip of the arthroscopic probe measured outside the knee and used as a reference. Over 10 mm of gapping supports grade 3+ MCL injury and may justify reconstruction. |
| Creating the femoral socket for the ACL at this time will save time later. |
| The thigh tourniquet is inflated only now at the beginning of graft harvesting. |
| The distal patellar bone plug for the patellar tendon graft and the proximal patellar bone plug for the quadriceps tendon–bone graft should be 15 mm long each. A bone bridge of about 10 mm should remain between the 2 bone plugs. |
| The partial-thickness quadriceps tendon length should be 10 cm or more. |
| Care is taken not to detach the partial-thickness quadriceps tendon at the patellar insertion, so that an intact tendon-bone junction remains during harvesting. |
| Fluoroscopy is used to confirm the correct location of the guidewire for the femoral socket of the MCL graft. |
| The saphenous nerve branches are carefully avoided, if present, at the area of the proximal tibia anchor insertion for the MCL graft, 5 to 10 mm distal to the medial joint line. |
| The quadriceps tendon graft is passed under layer 1 and overlies the native superficial MCL layer. |
| Pitfalls |
| Harvesting a patellar bone plug longer than 15 mm for the BPTB graft may result in inadequate remaining intact patella to later allow a second patellar bone plug harvest during quadriceps bone plug preparation. |
| Detachment of the partial-thickness quadriceps tendon at the tendon-patella junction may result from misinterpreting the gross anatomy at this junctional area. |
| Overzealous dissection at the proximal tibial MCL insertion area during anchor placement and during knot tying through the quadriceps tendon graft may harm the saphenous nerve branches. |
ACL, anterior cruciate ligament; BPTB, bone–patellar tendon–bone; MCL, medial collateral ligament.
Discussion
The presented technique using ipsilateral quadriceps tendon–bone and BPTB autografts to perform combined reconstruction of the MCL and ACL poses the following principal advantages: (1) excellent biological incorporation potential of autograft tissue of both ligaments, including bone-to-bone healing of the MCL graft in the femoral socket; (2) anatomic placement and fixation points of the MCL graft on the femur and tibia; and (3) sparing of the hamstring tendons as anterior and medial restraints in the situation of an anteriorly and medially unstable knee. Moreover, this technique spares the need for using allografts, which are associated with increased financial costs8; concerns of low tissue quality, particularly with irradiated grafts; slower biological incorporation9 and graft remodeling13; disease transmission10; and some evidence of higher failure rates and inferior functional outcomes in young active adults, at least for the ACL.11 Furthermore, using quadriceps tendon–bone autograft for reconstructing the MCL can also be applied to other scenarios as well, such as in rare cases of chronic isolated MCL instability or by surgeons who prefer to reconstruct the ACL with autologous hamstring tendons and wish to use autograft also for their MCL reconstruction in the combined MCL-ACL–deficient knee. The surgical risks of using our technique include an inadequate remaining bone bridge between the proximal and distal patellar bone plugs, which could potentially increase the risk of patellar fracture; inadvertent detachment of the partial-thickness quadriceps tendon graft from the proximal patellar pole during harvest; and saphenous nerve injury during proximal tibia exposure just distal to the joint line when inserting an anchor in this area. Moreover, harvesting both BPTB and quadriceps tendon–bone autografts adds operative time compared with using allografts and could potentially require a longer period of rehabilitation until full recovery of the extensor mechanism occurs.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Examination with the patient under anesthesia showed grade 2+ Lachman, grade 2+ pivot shift, and grade 2 to 3+ medial collateral ligament (MCL) laxity. Before the operation is started, all relevant skin markings are drawn. Arthroscopic evaluation using a 30° arthroscope (Olympus) is then performed. Anterior cruciate ligament (ACL) probing in this case confirmed a high-grade intrasubstance tear. Medial-compartment gapping at 20° of flexion with a valgus load showed over 1 cm of tibia-based gapping, supportive of grade 3+ MCL insufficiency. A 10-mm-diameter × 20-mm-long femoral socket for a bone–patellar tendon–bone (BPTB) graft is prepared. The thigh tourniquet is now inflated, and grafts harvest begins. The tibial tuberosity bone plug of the patellar tendon graft measures 10 mm wide × 20 mm long, whereas the distal patellar bone plug measures 10 mm wide × 15 mm long. This allows a bone bridge to be maintained at the center of the patella between the proximal and distal patellar bone plugs. A partial-thickness quadriceps tendon–bone graft is harvested next. A soft-tissue graft that is at least 10 cm long should be harvested. At the proximal patella, a 15-mm-long bone plug is needed, with the surgeon making sure that a central patellar bone bridge remains between the proximal and distal patellar bone plugs. The partial-thickness quadriceps tendon graft is whipstitched. The bone plug is tapered to a diameter of 9 mm and length of 15 mm. The arthroscope is reinserted into the knee, and a tibial tunnel of 10 mm in diameter is reamed for the ACL graft. The BPTB ACL graft is fixed in the femoral socket with a 7-mm × 20-mm titanium interference screw (Arthrex). The operation now continues on the extra-articular side. A 3-cm longitudinal incision is made over the medial epicondyle, and a guidewire is inserted horizontally 3 to 5 mm proximal and posterior to the tip of the medial epicondyle. A socket of 9 mm in diameter and 18 mm in depth is reamed over the guidewire. The bone plug of the quadriceps tendon–bone graft is docked in the femoral socket and fixed with a 7-mm × 20-mm titanium interference screw (Arthrex). A 3- to 5-cm longitudinal incision is made 6 cm distal to the joint line and posterior to the pes anserinus at the approximated anatomic distal tibial superficial MCL insertion. The superficial fascial layer (i.e., layer 1) is incised, and a soft-tissue tunnel is created bluntly, overlying the native superficial MCL layer from the distal MCL insertion point to the femoral MCL fixation point. The isometric point for the MCL graft is then identified on the tibia with a suture loop and marked with a Bovie device. A 2- to 3-cm longitudinal incision is made 5 to 10 mm distal and horizontal to the medial joint line. Layer 1 is incised. The quadriceps tendon graft is passed under layer 1 from proximal to distal. The ACL BPTB graft is fixed in the tibial tunnel with a 9-mm × 20-mm titanium interference screw (Arthrex) with the knee in extension. A 2-cm longitudinal slit is prepared in the quadriceps tendon over the area marked with a Bovie device for distal tibial insertion of the MCL graft. The knee is cycled, and the graft is fixed at the distal insertion point with a 4.5-mm titanium screw (Arthrex) and 18-mm titanium spiked washer (Arthrex) while the knee is at 20° of flexion and under slight varus stress. A 5.5-mm double-loaded Bio-Corkscrew FT anchor is finally added for reproducing proximal tibial soft-tissue MCL graft fixation just at the posterior edge of the quadriceps graft, 5 to 10 mm distal to the joint line. The location is confirmed fluoroscopically. The distal quadriceps MCL graft remnant is resected, and the combined reconstruction is complete.
References
- 1.Indelicato P.A. Non-operative treatment of complete tears of the medial collateral ligament of the knee. J Bone Joint Surg Am. 1983;65:323–329. [PubMed] [Google Scholar]
- 2.Zhang H., Sun Y., Han X. Simultaneous reconstruction of the anterior cruciate ligament and medial collateral ligament in patients with chronic ACL-MCL lesions: A minimum 2-year follow-up study. Am J Sports Med. 2014;42:1675–1681. doi: 10.1177/0363546514531394. [DOI] [PubMed] [Google Scholar]
- 3.Marx R.G., Hetsroni I. Surgical technique: Medial collateral ligament reconstruction using Achilles allograft for combined knee ligament injury. Clin Orthop Relat Res. 2012;470:798–805. doi: 10.1007/s11999-011-1941-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Delong J.M., Waterman B.R. Surgical techniques for the reconstruction of medial collateral ligament and posteromedial corner injuries of the knee: A systematic review. Arthroscopy. 2015;31:2258–2272. doi: 10.1016/j.arthro.2015.05.011. [DOI] [PubMed] [Google Scholar]
- 5.Bosworth D.M. Transplantation of the semitendinosus for repair of laceration of medial collateral ligament of the knee. J Bone Joint Surg Am. 1952;34:196–202. [PubMed] [Google Scholar]
- 6.Kim S.J., Lee D.H., Kim T.E., Choi N.H. Concomitant reconstruction of the medial collateral and posterior oblique ligaments for medial instability of the knee. J Bone Joint Surg Br. 2008;90:1323–1327. doi: 10.1302/0301-620X.90B10.20781. [DOI] [PubMed] [Google Scholar]
- 7.Lind M., Jakobsen B.W., Lund B., Hansen M.S., Abdallah O., Christiansen S.E. Anatomical reconstruction of the medial collateral ligament and posteromedial corner of the knee in patients with chronic medial collateral ligament instability. Am J Sports Med. 2009;37:1116–1122. doi: 10.1177/0363546509332498. [DOI] [PubMed] [Google Scholar]
- 8.Nagda S.H., Altobelli G.G., Bowdry K.A., Brewster C.E., Lombardo S.J. Cost analysis of outpatient anterior cruciate ligament reconstruction: Autograft versus allograft. Clin Orthop Relat Res. 2010;468:1418–1422. doi: 10.1007/s11999-009-1178-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tom J.A., Rodeo S.A. Soft tissue allografts for knee reconstruction in sports medicine. Clin Orthop Relat Res. 2002;402:135–156. doi: 10.1097/00003086-200209000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Mroz T.E., Joyce M.J., Steinmetz M.P., Lieberman I.H., Wang J.C. Musculoskeletal allograft risks and recalls in the United States. J Am Acad Orthop Surg. 2008;16:559–565. doi: 10.5435/00124635-200810000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Mascarenhas R., Erickson B.J., Sayegh E.T. Is there a higher failure rate of allografts compared with autografts in anterior cruciate ligament reconstruction: A systematic review of overlapping meta-analysis. Arthroscopy. 2015;31:364–372. doi: 10.1016/j.arthro.2014.07.011. [DOI] [PubMed] [Google Scholar]
- 12.More R.C., Karras B.T., Neiman R., Fritschy D., Woo S.L., Daniel D.M. Hamstrings—An anterior cruciate ligament protagonist. An in vitro study. Am J Sports Med. 1993;21:231–237. doi: 10.1177/036354659302100212. [DOI] [PubMed] [Google Scholar]
- 13.Bhatia S., Bell R., Frank R.M. Bony incorporation of soft tissue anterior cruciate ligament grafts in an animal model: Autograft versus allograft with low-dose gamma irradiation. Am J Sports Med. 2012;40:1789–1798. doi: 10.1177/0363546511435637. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Examination with the patient under anesthesia showed grade 2+ Lachman, grade 2+ pivot shift, and grade 2 to 3+ medial collateral ligament (MCL) laxity. Before the operation is started, all relevant skin markings are drawn. Arthroscopic evaluation using a 30° arthroscope (Olympus) is then performed. Anterior cruciate ligament (ACL) probing in this case confirmed a high-grade intrasubstance tear. Medial-compartment gapping at 20° of flexion with a valgus load showed over 1 cm of tibia-based gapping, supportive of grade 3+ MCL insufficiency. A 10-mm-diameter × 20-mm-long femoral socket for a bone–patellar tendon–bone (BPTB) graft is prepared. The thigh tourniquet is now inflated, and grafts harvest begins. The tibial tuberosity bone plug of the patellar tendon graft measures 10 mm wide × 20 mm long, whereas the distal patellar bone plug measures 10 mm wide × 15 mm long. This allows a bone bridge to be maintained at the center of the patella between the proximal and distal patellar bone plugs. A partial-thickness quadriceps tendon–bone graft is harvested next. A soft-tissue graft that is at least 10 cm long should be harvested. At the proximal patella, a 15-mm-long bone plug is needed, with the surgeon making sure that a central patellar bone bridge remains between the proximal and distal patellar bone plugs. The partial-thickness quadriceps tendon graft is whipstitched. The bone plug is tapered to a diameter of 9 mm and length of 15 mm. The arthroscope is reinserted into the knee, and a tibial tunnel of 10 mm in diameter is reamed for the ACL graft. The BPTB ACL graft is fixed in the femoral socket with a 7-mm × 20-mm titanium interference screw (Arthrex). The operation now continues on the extra-articular side. A 3-cm longitudinal incision is made over the medial epicondyle, and a guidewire is inserted horizontally 3 to 5 mm proximal and posterior to the tip of the medial epicondyle. A socket of 9 mm in diameter and 18 mm in depth is reamed over the guidewire. The bone plug of the quadriceps tendon–bone graft is docked in the femoral socket and fixed with a 7-mm × 20-mm titanium interference screw (Arthrex). A 3- to 5-cm longitudinal incision is made 6 cm distal to the joint line and posterior to the pes anserinus at the approximated anatomic distal tibial superficial MCL insertion. The superficial fascial layer (i.e., layer 1) is incised, and a soft-tissue tunnel is created bluntly, overlying the native superficial MCL layer from the distal MCL insertion point to the femoral MCL fixation point. The isometric point for the MCL graft is then identified on the tibia with a suture loop and marked with a Bovie device. A 2- to 3-cm longitudinal incision is made 5 to 10 mm distal and horizontal to the medial joint line. Layer 1 is incised. The quadriceps tendon graft is passed under layer 1 from proximal to distal. The ACL BPTB graft is fixed in the tibial tunnel with a 9-mm × 20-mm titanium interference screw (Arthrex) with the knee in extension. A 2-cm longitudinal slit is prepared in the quadriceps tendon over the area marked with a Bovie device for distal tibial insertion of the MCL graft. The knee is cycled, and the graft is fixed at the distal insertion point with a 4.5-mm titanium screw (Arthrex) and 18-mm titanium spiked washer (Arthrex) while the knee is at 20° of flexion and under slight varus stress. A 5.5-mm double-loaded Bio-Corkscrew FT anchor is finally added for reproducing proximal tibial soft-tissue MCL graft fixation just at the posterior edge of the quadriceps graft, 5 to 10 mm distal to the joint line. The location is confirmed fluoroscopically. The distal quadriceps MCL graft remnant is resected, and the combined reconstruction is complete.